Abstract
Background
Depression with diverse etiologies is exacerbated by chronic diseases, such as chronic kidney disease (CKD), coronary artery disease (CAD), cancer, diabetes mellitus, and hypertension. This study aimed to analyse depression, its associations, and predictors among patients attending the kidney clinic of a teaching hospital.
Methods
Data were collected from 01 August 2017 to 30 September 2017 via face-to-face interviews and examination of the medical records of a convenience sample of 314 patients. The patients were categorised broadly as stages I and II with an estimated glomerular filtration rate (eGFR) > 60 mls/min/1.73 m2, and with stages III, IV, and V or GFR ≤ 60 mls/ min/1.73 m2 (or CKD). The Patient Health Questionnaire (PHQ)-9 was the data collection instrument for depression-related data.
Results
Participants were predominantly male (n = 179; 57.0%), aged over 60 years (n = 211; 67.2%), Indo-Trinbagonian (n = 237; 75.5%), and with stages III, IV, and V CKD. The two leading comorbid conditions were hypertension (83.4%) and diabetes mellitus (56.1%). Of the 261 (83.1%) patients with recorded eGFR, 113 (43.3%) had Stage III CKD. The mean depression (PHQ-9) score was 13.0/27 (\(\pm\)9.15), with 306 (97.5%) patients diagnosed as having depression with the following severities: mild (n = 116; 37.9%), moderate (n = 138, 45.1%), moderately severe (n = 38; 12.4%), and severe (n = 14; 4.6%). Depression was independent of sex. Nine sociodemographic variables were associated with depression; however, ‘level of education’, was the only predictor of depression with greater severity associated with lower levels of education. eGFR was negatively correlated with the PHQ-9 scores (Pearson’s correlation, r = -0.144, p = 0.022). At least 78.3% of the patients who self-reported no depression had clinical depression (moderate, moderately severe, or severe) PHQ-9 scores ≥ 10.
Conclusion
Depression was a significant comorbidity among patients with CKD, with the majority displaying clinical depression. “Level of education” was the only predictor of depression. Self-reported depression is an unreliable method for evaluating clinical depression.
Similar content being viewed by others
Background
Chronic kidney disease (CKD) is irreversible damage to the kidney lasting > 3 months. Worldwide, CKD is quite prevalent, impacting more than 10% of people [1]. It affects people physically [2], mentally [3], and socially [4], leading to “poorer health outcomes, increased hospitalisation, and lower quality of life” [5]; anxiety whose prevalence among patients with CKD was 19%, and anxiety symptoms whose occurrence was 43% [6]. Depression, a common mental disorder, according to the World Health Organization, “is characterised by sadness, loss of interest or pleasure, feelings of guilt or low self-worth, disturbed sleep or appetite, feelings of tiredness, and poor concentration” [7]. Approximately 280 million people have depression worldwide [8]. The global depression levels are an estimated 3.8% of the population, including 5.0% of adults and 5.7% of adults aged > 60 years [8]. The overall depression levels in Trinidad and Tobago are unavailable. However, the levels vary from 25.3% ± 2.37% among adolescents [9] to 40% among stable cardiac clinic attendees [10]. Depression among patients with kidney diseases accounts for 20–25% of the adult population globally [11]. The prevalence of clinical depression (Patient Health Questionnaire, PHQ > 9) among patients with CKD is 39% [12] and 46% [13] in the USA and the UK, respectively. Research by Agarwal et al. revealed the prevalence of depression among haemodialysis patients to be 78%, 65%, and 51% using PHQ-9, HAD-17, and ICD-10, respectively. [14].
Risk factors for depression include “female sex, financial difficulties/low socioeconomic status, stressful life events, lack of social support, serious or chronic illness, and a history of eating disorders” [15], many of which are common in our population.
Predictors of depression vary with socio-cultural and economic contexts. Tannor et al. identified predictors of CKD with diabetes mellitus and hypertension as increasing age, low educational status, increased duration of hypertension, and use of herbal preparations [16]. According to Yang Meng et al., independent predictors of depression in haemodialysis patients were lower monthly family income, more comorbidities, and a higher degree of pruritus. [17].
This study aimed to determine depression levels among patients with CKD and its associations and predictors.
Methods
This cross-sectional study comprised patients with kidney diseases attending CKD clinics at a public health institute. The institute is a 325-bed hospital providing a multitude of services, including both peritoneal and haemodialysis, emergency, and follow-up care in two kidney clinics, each of which attends to approximately 40 to 50 patients per clinic day [18] conducted once per week. The patients are referred to the clinic primarily because of elevated serum creatinine (a marker of CKD), apart from leg swelling and proteinuria. CKD was defined as a decrease in the renal creatinine filtration rate (estimated glomerular filtration rate - eGFR < 60 mL/min/1.73 m2) [19] lasting more than 90 days. [20] eGFR is used to determine the presence of CKD (CKD stages 3–5) [20]. eGFR [21] can be classified into 5 stages: Stage 1 CKD: mild kidney damage, estimated GFR (eGFR) ≥ 90 mL/1.73 m2; Stage 2 CKD: mild loss of kidney function, eGFR ranging from 60 mL/1.73m2 to 89 mL/1.73m2; Stage 3a and 3b CKD: mild to severe loss of kidney function, eGFR ranging from 30 mL/1.73m2 to 59 mL/1.73 m2; Stage 4 CKD: severe loss of kidney function, eGFR ranging from 15 mL/ 1.73m2 to 29 mL/1.73m2; and Stage 5 CKD: Kidney failure or end-stage renal failure, eGFR < 15 mL/ 1.73 m2 [22].
Participants were selected by convenience sampling because of the challenges of obtaining a random sample. Furthermore, a sample size could not be determined primarily because of the absence of a formula to compute sample size from a non-random sample. The questionnaire was piloted among kidney and non-kidney patients and edited based on feedback from interviewees and the Ethics Committee. Submission of the results was delayed beyond the intended date due mainly to unforeseen administrative issues. There were no missing data except for one participant whose PHQ-9 score could not be computed because of missing information. The inclusion criteria were as follows: age > 18 years and being enrolled in the clinic for at least 12 months. Patients who were uremic, confused, or unable to communicate coherently were excluded from the study. Patients who visited the kidney clinic were briefed on the nature of the study and invited to participate. They were assured of the confidentiality, anonymity, and privacy of data. All participants gave their informed consent to participate in the study .
Data were collected from 01 August 2017 to 30 September 2017 using a pre-tested questionnaire. The data collection instrument was a 24-item questionnaire consisting of sociodemographic variables (12), medical diagnosis/history (2), cardiovascular history (1), and the nine-item PHQ-9 for depressive symptoms. Depression is ideally best diagnosed using the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) [23]. However, PHQ-9 was used because of its brevity and simplicity, and according to Kroenke et al., it is also “a reliable and valid measure of depression severity” [24]. PHQ-9 (comprising nine questions) has a reported sensitivity of 54% and specificity of 90% for scores ≥ 10 [25].
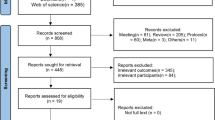
PHQ-9 data were collected via face-to-face interviews after obtaining verbal consent, whereas other relevant data were extracted from the patient records. Overall, 350 patients were selected for participation; 36 (10.3%) were excluded, resulting in a convenience sample of 314 participants. Figure 1.
Each PHQ-9 question was scored from 0 (not at all) to 3 (every day), and the individual scores were added to obtain a total PHQ-9 score (range 0–27) for each participant, with higher scores signifying worse depression. These scores were used to classify the participants according to the level of depression using the ranges provided with the data entry codes (Table 1).
The following definitions were used to facilitate data collection: Obesity and Hypercholesterolaemia (self-reported), Hypertensive if previously diagnosed, and currently under antihypertensive medications, in accordance with the American College of Cardiology Guidelines [27]. Cardiovascular disease (coronary artery disease and/or stroke) was determined by a “history of coronary heart disease (angina, myocardial infarction) verified through medical records of a prior episode and confirmed by work-up including electrocardiography, echocardiography, and exercise treadmill test” [28]. Physical inactivity was defined as not performing moderate to vigorous activity for at least 150 min per week; participants classified into this group were categorised as “physically inactive” [29]. Clinical depression was defined as a total PHQ-9 score ≥ 10 for all nine questionnaire items [24]. Because of the challenges in applying the definition of smokers, i.e., someone who has smoked more than 100 cigarettes in their lifetime and has smoked in the last 28 days [30], we identified smokers as persons who self-reported smoking up to the time of presentation in the clinic.
Database and data analysis
We used Microsoft EXCEL version 10 to create a database, which was imported into SPSS, Version 21, to develop the SPSS database that was used for descriptive and inferential analyses.
Only the researchers and research assistants could access these databases. The descriptive data analysis methods included frequency, percentage distribution tables, graphs and/or charts, sample proportions or percentages for qualitative variables, and the measures of central tendency (minimum, median, maximum, mean and standard deviation) for quantitative variables. The inferential methods included 95% confidence intervals (CI), hypothesis testing (Z-tests for the equality of two proportions, t-test for the equality of two means, analysis of variance (ANOVA), chi-square tests of association, binary, ordinal, and logistic regression to identify the predictors of depression. All hypotheses were assessed at a 5% level of significance.
Ethical approval was obtained from the Ethics Committee of the South West Regional Authority.
Results
All 314 patients completed the full face-to-face interview; however, data needed to determine depression status (PHQ 9 -score), 7 (2.2%) patients were either incomplete; or missing altogether from their respective files. Cronbach’s alpha, the measure of the PHQ-9 questionnaire reliability, was 0.745, which is indicative of good internal consistency of the responses.
Demographics
The majority (n = 160; 51.0%) of study participants were referred by the Medical Department (Fig. 2).
They were predominantly male, over 60 years of age, of Indo-Trinbagonian ethnicity had family support and/or social support and were on government assistance (Table 2).
High creatinine (n = 146; 46.5%) was the most common reason for kidney clinic referral (Fig. 3).
Hypertension was most common comorbidity (83.8%; n = 263), and obesity was the least prevalent comorbidity (4.8%; n = 15) (Fig. 4). The minimum number of conditions was 0 (n = 33; 10.5%), whereas the maximum was 5 (n = 4; 1.3%), with a mode, median, and mean of 2 (n = 138; 43.9%), 2, and 1.8 ± 1.06, respectively.
eGFR and creatinine values
The eGFR values ranged from 4.0 mls/min/1.73 m2 to 130.0 mls/min/1.73 m2, with a median, mode, and mean value of 31, 36 (n = 11), and 33.7 (± 21.85), respectively. The mean, minimum, maximum, median, and mode values for creatinine were 3.2 (± 2.96), 0.6, 22.0, 2.1, and 1.4, respectively.
eGFR values were documented in 261 (83.1%) patients according to the CKD stage.
(Fig. 5). The prevalence of Stage 1 and Stage 5 was 2.7% (n = 7) and 17.1% (n = 45), respectively, with Stage 3 being the most prevalent (43.3%; n = 114).
Depressive symptoms/total PHQ scores and distribution by socio-demographic variables
The mean responses for PHQ-9 questions ranged from 1.00 (thoughts that you would be better off dead or of hurting yourself in some way) to 1.74 (feeling tired or having little energy). In other words, each participant either experienced at least one of the nine symptoms or enddured them for several days, but less than half of the days. The overall mean of the nine items was 1.34 ± 0.249, and the minimum score was 0, similar to the median and modal scores.
Depression scores
Total PHQ-9 scores ranged from 9 (n = 116; 37.6%) to 27 (n = 1; 0.3%). The means and standard deviations (SD) according to socio-demographic variables and the p-values obtained from using ANOVA to test for equality of within-category means are shown in Table 3.
Patients with no family support had a significantly higher mean depression score than did patients with family support (p = 0.014). However, patients who lived with spouses had a significantly lower mean PHQ-9 score than patients who lived with their children (p = 0.030) and patients who lived with their children and spouse (p = 0.002). Furthermore, patients with CKD for 10 years or more had a higher mean score than patients with CKD for less than 1 year (p = 0.042), patients with CKD for 1 to 5 years (p = 0.010), and patients with CKD for 6 to 10 years (p = 0.011).
Depression severity: associated factors and predictors
None of the PHQ-9 scores ranged from 0 to 4, i.e., none of the patients had none to minimal depression. The majority of patients had moderate depression (non-symptomatic) (n = 138; 45.1%), and the smallest percentage had severe depression (clinical; symptomatic) (n = 14; 4.6%) depression (Fig. 6).
Pearson’s Chi-square tests of Association (Table 4) showed that, except for gender, each of the qualitative variables measured was associated with depression severity. Furthermore, Ordinal Logistic Regression showed that of the nine associated variables, ‘Level of Education’, was the only predictor of depression severity. Respective Adjusted odds ratios (AOR) with corresponding 95% CI are shown in Table 5.
Specifically, patents with Primary School education only were thirty-three times more likely to experience some level of depression compared to those with a tertiary level education. Patients with A Secondary School education were equally as likely as those with a tertiary education to experience some degree of depression.
Depression severity according to the CKD stage
Figure 7 shows the percentage distribution of depression levels among the 153 (48.7%) patients with Stage 3 (n = 65), Stage 4 (n = 56), and Stage 5 (n = 32) CKD.
Chi-square analysis showed no association between the two variables (Chi-square: 4.248, df = 8, and p = 0.834).
Finally, the Mc Nemar-Bowker test of equality of paired proportions showed significant discordance between self-reported depression level and PHQ-9 depression classification (p ≤ 0.001). In total, 78.3% of the patients who self-reported no depression had PHQ-9 scores ≥ 10 (moderate to severe depression). Table 6 shows that of the 225 (87.2%) patients who self-reported having no depression, 202 (89.8%) were designated as having Moderate to Severe depression by PHQ-9 assessment. Table 6.
Discussion
The study population comprised principally of referrals with CKD or stages 3, 4, and 5 (90.8%), with over one-third (n = 120; 38.2%) having an age range of 61–70 years. Participants were predominantly male (57.0%), Indo-Trinidadian (75.5%), and with cardiovascular risks factors, including hypertension (83.8%) and diabetes (57%). These characteristics differ from overall population characteristics. The age-standardised global prevalence of CKD, stages 3–5 in adults aged ≥ 20 years was 4.7% in men and 5.8% in women [31]. According to the center for disease control, CKD stages 3–4 prevalence among patients with diabetes in the United States (US) was 24.5% from 2011 to 2014, and among adults with hypertension in the US adults was 35.8% from 2011 to 2014 [32].
Clinical depression.
Each participant had experienced at least one of the nine depressive symptoms or experienced them for several days but less than half of the days. More than half of the patients (62.1%) were classified as those with clinical depression: moderate (n = 138; 45.1%), moderate to severe (n = 40; 12.4%), and severe depression (n = 14; 4.6%). These findings are similar to those of a study by Gardia et al. among patients with CKD on haemodialysis which revealed an overall depression of 66% (n = 100): 28.8% had moderate depression, and 13.6% had severe depression [33]. Gardia et al. also found that depression was more prevalent in female patients (86%) as compared to male patients (57%). (P = 0.005).
Our study revealed that chi-square tests of association demonstrated that gender, education level, monthly income, persons “lived with”, family support, financial support, employment status, CKD duration, and age group were associated with clinical depression. These findings corroborated with other studies that revealed an association between depression and sociodemographic variables, such as income [33], employment [34], social status [35], and social support [36]. A study by Duan et al., analyzing other variables revealed “negative illness perception, low self-esteem and severe pain interference” were associated with depression among CKD patients not on dialysis. [37].
According to Pevrol et al. there is a similar associaltion between lower level of education and major depression. [38]. Patients with lower level education were significantly more likely to have major depression than those with higher education. This association of lower educational level with more depression was reported by Timmermans IAL and Widdershoven J [39]. Because depressed people with lower education may have less access to screening and treatment. [40].
Furthermore, in our study, ordinal logistic regression revealed that “level of education”, was the only predictor of depression severity with greater severity associated with lower levels of education. Other predictors of major depression in CKD, identified by Tezel and Turkistani were family support [41, 42]. Support is a major contributor to patient security [43], quality of life [44, 45], and life expectancy. The lack of patient support hinders transport support services and supplementation of treatment; thus, there is a risk of worsening depression with complications and early death [46]. Most patients in this study received financial support, followed by help from the family. These findings differ from those of Silva et al. [46] and Bapat et al. [47]. Depression can lead to poorer health outcomes [48], increased hospitalisation [49], and lower quality of life [50]. Additionally, it was discovered that medication nonadherence is linked to worsening of CKD [51].According to Meng et al., depression and worsening CKD together increase the risk of both cardiovascular and all-cause death. [52].
The difference between the prevalence of depression was insignificant among women and men (63.9% vs. 60.5%) (p = 0.637). However, Sqalli-Houssaini et al. [53] and Chiang et al. [54] demonstrated a significant association. Our findings revealed no significant association between depression severity and ethnicity (p = 0.776). Similarly, Mosleh et al. demonstrated that age was the only variable associated with depression among patients with CKD undergoing dialysis and was the only predictor of depression (OR: 1.040; 95% CI: 1.004–1.076; p = 0.027) [55]. Factors associated with depression in other populations studied include satisfaction with care [56], social support [57], and associated comorbid conditions [58]. Furthermore, researchers have reported “a higher prevalence of depression among patients with CKD without religious beliefs, no regular exercise regimen, sleep disorders, and diagnosed with stage III or higher CKD” [54].
At each stage of CKD, moderate to moderate severity of depression remained relatively the same (between 65 and 75%) except for severe depression, which seems to increase with worsening CKD – stages III to V). The chi-square analysis did not reveal an association between these variables (Chi-square: 4.248, df = 8, p = 0.834). Tsai et al., Lee et al., and Danielle et al. reported clinical depression levels of 37% [59], 47.1% [60], and 40% [61], respectively, for CKD Stages III, IV, and V. Generally, patients with CKD (Stage V) displayed the highest prevalence of clinical depression [55]; however, this finding was inconsistent. Dziubek et al. revealed a 53% prevalence of depression among patients with Stage V renal failure [62]. In this study, high levels of depression were not surprising because of the lack of quality support (financial, social, and medical), also reported by Hettiarachchi and Abeysena [63].
Further, a significant number (78.3%) of patients who self-reported no depression had at least moderate to severe depression (PHQ-9 scores ≥ 10). Self-reported depression among patients with CKD was reported to be less accurate, especially among patients with kidney failure. [64].
Limitations
The study sample was relatively small because of resource constraints. Moreover, it was not randomised but a convenience sample. The patients had to rely on recall, which could be challenging. Apart from hypertension and diabetes, the medical history of the respondents was not appropriately documented. Further, clinical depression evaluation based on the PHQ 9 score is subjective and may underestimate or overestimate symptoms. The use of PHQ 9 is a major limitation of diagnosisng depression which requires use of the DSM-5 criterion. The PHQ 9, however has shown merits as a major screening tool. Patients with at least moderate to severe depression should have been referred for further psychiatric evaluation and treatment. Although the data is not current since a few years have lapsed since data collection, the results of this study is very relevant today since the type of patients and modus operandi of clinics remain the same.
Conclusions
Depression and depressive symptoms are major comorbidities in patients with CKD. Furthermore, the lack of social support is a predictor of depression. There is marked discordance in the high levels of depression reported using depression tools and low levels identified from self-reporting. Self-reported evaluation can underdiagnose depression and depression severity. Scientific evaluation of depression can avoid underdiagnosis, delayed diagnosis, delayed psychiatric referrals, and definitive treatment. Routine screening for depression with adequate systems in place for management should be mandatory. Greater work is required to determine psycho-social and medical determinants of depression and quality of life among patients with CKD.
Data Availability
The data supporting the findings of this study shall be made available from the corresponding author upon reasonable request.
Change history
24 October 2023
The figures were incorrectly positioned in the original publication. The article has been updated to rectify theerrors.
27 November 2023
A Correction to this paper has been published: https://doi.org/10.1186/s12888-023-05383-7
Abbreviations
- PHQ-9:
-
Patient Health Questionnaire-9
- KDIGO:
-
Kidney Disease Improving Global Outcomes
- CKD:
-
Chronic kidney disease
- GFR:
-
Glomerular filtration rate
- eGFR:
-
Estimated glomerular filtration rate
- ESRD:
-
End-stage renal disease
- AOR:
-
adjusted odds ratios
- ANOVA:
-
Analysis of variance
References
Kovesdy CP. Epidemiology of chronic kidney disease: an update 2022. Kidney Int Suppl (2011). 2022;12:7–11. https://doi.org/10.1016/j.kisu.2021.11.003.
Whitsel LP, Arena R, Kaminsky LA, Berrigan D, Katzmarzyk PT, Calitz C, et al. Assessing physical activity, sedentary behavior, and Cardiorespiratory Fitness in Worksite Health Promotion. Am J Health Promot. 2019;33:318–26. https://journals.sagepub.com/doi/10.1177/0890117118816750e.
Simões e Silva AC, Miranda AS, Rocha NP, Teixeira AL. Neuropsychiatric Disorders in chronic kidney disease. Front Pharmacol. 2019;10:932. https://doi.org/10.3389/fphar.2019.00932/full;10:932. Published 2019 Aug 16. https://www.frontiersin.org/articles/.
Babatsikou FP, Georgianni SK. Social aspects of chronic renal failure in patients undergoing haemodialysis. Int J Caring Sci. 2014;7:740–5. http://www.internationaljournalofcaringsciences.org/docs/6.%20Gerogianni%20%20SPECIAL.pdf.
Staff AKF. Depression in people living with kidney disease [Internet]. Am Kidney Fund. 2018 [cited 2022Jun3]. https://www.kidneyfund.org/kidney-today/depression-in-kidney-disease-patients.html.
Huang CW, Wee PH, Low LL, Koong YLA, Htay H, Fan Q, et al. Prevalence and risk factors for elevated anxiety symptoms and anxiety disorders in chronic kidney disease: a systematic review and meta-analysis. Gen Hosp Psychiatry. 2021;69:27–40. https://doi.org/10.1016/j.genhosppsych.2020.12.003.
World Health Organization. Depression: Definition [Internet]. World Health Organization. ; 2022. https://www.euro.who.int/en/health-topics/noncommunicable-diseases/pages/news/news/2012/10/depression-in-europe/depression-definition. Accessed 18 March 2022.
World Health Organization. Depression [Internet]. World Health Organization. World Health Organization; 2021. common%20illness,world%20have%20depression%20. https://www.who.int/news-room/fact-sheets/detail/depression#:~:text=Depression%20is%20a%20.
Maharaj RG, Alli F, Cumberbatch K, Laloo P, Mohammed S, Ramesar A, et al. Depression among adolescents, aged 13–19 years, attending secondary schools in Trinidad: prevalence and associated factors. West Indian Med J. 2008;57:352–9. https://pubmed.ncbi.nlm.nih.gov/19566015/.
Bahall M, Khan K. Quality of life of patients with first-time AMI: a descriptive study. Health Qual Life Outcomes. 2018;16:32. https://doi.org/10.1186/s12955-018-0860-8.
Shirazian S. Depression in CKD: understanding the mechanisms of disease. Kidney Int Rep. 2019;4:189–90. https://doi.org/10.1016/j.ekir.2018.11.013.
Palmer S, Vecchio M, Craig JC, Tonelli M, Johnson DW, Nicolucci A, et al. Prevalence of depression in chronic kidney disease: systematic review and meta-analysis of observational studies. Kidney Int. 2013;84:179–91. https://doi.org/10.1038/ki.2013.77.
Chilcot J, Wellsted D, Da Silva-Gane M, Farrington K. Depression on dialysis. Nephron Clin Pract. 2008;108:c256–64. https://doi.org/10.1159/000124749.
Agrawaal KK, Chhetri PK, Singh PM, Manandhar DN, Poudel P, Chhetri A. Prevalence of Depression in patients with chronic kidney Disease Stage 5 on Hemodialysis at a Tertiary Care Center. JNMA J Nepal Med Assoc. 2019;57:172–5. https://doi.org/10.31729/jnma.4408.
Razzak HA, Harbi A, Ahli S. Depression: Prevalence and Associated Risk factors in the United Arab Emirates. Oman Med J. 2019;34:274–82. https://doi.org/10.5001/omj.2019.56.
Tannor EK, Sarfo FS, Mobula LM, Sarfo-Kantanka O, Adu-Gyamfi R, Plange-Rhule J. Prevalence and predictors of chronic kidney disease among ghanaian patients with hypertension and diabetes mellitus: a multicenter cross sectional study. J Clin Hypertens. 2019;21:1542–50.
Meng Y, Wu HT, Niu JL, Zhang Y, Qin H, Huang LL, et al. Prevalence of depression and anxiety and their predictors among patients undergoing maintenance hemodialysis in Northern China: a cross-sectional study. Ren Fail. 2022;44:933–44. https://doi.org/10.1080/0886022X.2022.2077761.
Utilisation Report of the Medical Records Department. Trinidad: South West Regional Health Authority, Ministry of Health; 2017.
Clase C. Renal failure (chronic). BMJ Clin Evid. 2011;2011:2004. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3217810/?report=classic2011.
Levey AS, Eckardt KU, Dorman NM, Christiansen SL, Cheung M, Jadoul M et al. Nomenclature for kidney function and disease-executive summary and glossary from a Kidney Disease: Improving Global Outcomes (KDIGO) consensus conference. Eur Heart J. 2020;41:4592-8. https://doi.org/10.1093/eurheartj/ehaa650.
Levey AS, Stevens LA, Estimating GFR, Using the CKD Epidemiology Collaboration (CKD-EPI). Creatinine equation: more accurate GFR estimates, lower CKD prevalence estimates, and better risk predictions. Am J Kidney Dis. 2010;55:622–7. https://doi.org/10.1053/j.ajkd.2010.02.337.
American kidney fund. Stages of kidney disease [Internet]. Am Kidney Fund. 2022 [cited 2022Jun3]. https://www.kidneyfund.org/all-about-kidneys/stages-kidney-disease.
Truschel J. Depression Definition and DSM-5 Diagnostic Criteria [Internet]. Psycom.net. Psycom; 2022. Available from: https://www.psycom.net/depression/major-depressive-disorder/dsm-5-depression-criteria.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
Hamo CE, Heitner JF, Pfeffer MA, Kim HY, Kenwood CT, Assmann SF, et al. Baseline distribution of participants with depression and impaired quality of life in the treatment of preserved cardiac function heart failure with an Aldosterone Antagonist Trial. Circ Heart Fail. 2015;8:268–77. https://doi.org/10.1161/CIRCHEARTFAILURE.114.001838.
Hall-Flavin DK. Severe, persistent depression [Internet]. Mayo Clinic Publications. Mayo Foundation for Medical Education and Research; 2017 [cited 2022Jul4]. https://www.mayoclinic.org/diseases-conditions/depression/expert-answers/clinical-depression/faq-20057770.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH et al. /ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13-e115. https://doi.org/10.1161/HYP.0000000000000065.
World Health Organization. Cardiovascular disease [Internet]. World Health Organization. [cited 2022Jun3]. https://www.who.int/cardiovascular_diseases/about_cvd/en/.
Bull F. Defining physical inactivity. Lancet. 2003;361:258–9. https://doi.org/10.1016/S0140-6736(03)12290-8.
Ministry of Health NZ. Definitions of smoking status [Internet]. Ministry of, Health N. 2021 [cited 2022Jun3]. https://www.health.govt.nz/our-work/preventative-health-wellness/tobacco-control/tobacco-control-information-practitioners/definitions-smoking-status.
Mills KT, Xu Y, Zhang W, Bundy JD, Chen CS, Kelly TN, et al. A systematic analysis of worldwide population-based data on the global burden of chronic kidney disease in 2010. Kidney Int. 2015;88:950–7.
Centers for Disease Control and Prevention Chronic kidney disease (CKD) surveillance system. : 2021. https://nccd.cdc.gov/ckd/default.aspx Accessed September 30, 2021.
Gadia P, Awasthi A, Jain S, Koolwal GD. Depression and anxiety in patients of chronic kidney disease undergoing haemodialysis: a study from western Rajasthan. J Family Med Prim Care. 2020;9:4282–6. https://doi.org/10.4103/jfmpc.jfmpc_840_20.
Kutner NG, Zhang R, Huang Y, Johansen KL. Depressed mood, usual activity level, and continued employment after starting dialysis. Clin J Am Soc Nephrol. 2010;5:2040–5. https://doi.org/10.2215/CJN.03980510.
Shin SJ, Lee JH. Hemodialysis as a life-sustaining treatment at the end of life. Kidney Res Clin Pract. 2018;37:112–8. https://doi.org/10.23876/j.krcp.2018.37.2.112.
Mıstık S, Ünalan D, Tokgöz B. The effect of depression and perceived social support systems on quality of life in dialysis patients. Turk Nephr Dial Transpl Turkish J Nephrol. 2017;26:23–8.
Duan D, Yang L, Zhang M, Song X, Ren W. Depression and associated factors in Chinese patients with chronic kidney disease without dialysis: A cross-sectional study. Front Public Health [Internet]. 2021;9. https://doi.org/10.3389/fpubh.2021.605651.
Peyrot WJ, Lee SH, Milaneschi Y, Abdellaoui A, Byrne EM, Esko T, et al. The association between lower educational attainment and depression owing to shared genetic effects? Results in ~ 25,000 subjects. Mol Psychiatry. 2015;6:735–43. https://doi.org/10.1038/mp.2015.50. - DOI - PMC - PubMed.
Timmermans IAL, Widdershoven J. Educational level as a predictor for anxiety and depression in ICD-patients [Internet]. Uvt.nl. 2016 [cited 2023 Sep 13]. Available from: http://arno.uvt.nl/show.cgi?fid=141103#:~:text=Educational%20level%20is%20an%.
Taple BJ, Chapman R, Schalet BD, Brower R, Griffith JW. The impact of education on Depression Assessment: Differential Item Functioning Analysis. Assessment. 2022;29(2):272–84. https://doi.org/10.1177/1073191120971357.
Tezel A, Karabulutlu E, Sahin O. Depression and perceived social support from family in turkish patients with chronic renal failure treated by hemodialysis. J Res Med Sci. 2011;16:666–73. https://pubmed.ncbi.nlm.nih.gov/22091290/.
Turkistani I, Nuqali A, Badawi M, Taibah O, Alserihy O, Morad M, et al. The prevalence of anxiety and depression among end-stage renal disease patients on hemodialysis in Saudi Arabia. Ren Fail. 2014;36:1510–5. https://doi.org/10.3109/0886022X.2014.949761.
Tavares JM, Lisboa MT, Ferreira MA, Valadares GV, Silva FV. Peritoneal dialysis: family care for chronic kidney disease patients in home-based treatment. Rev Bras Enferm. 2016;69:1172–8. https://doi.org/10.1590/0034-7167-2016-0262. Portuguese, English.
Zhang JP, Liu HR. [Family support and quality of life among hemodialysis patients] Hunan Yi Ke Da Xue Xue Bao. 2001;26:359–62. Chinese. https://pubmed.ncbi.nlm.nih.gov/12536737/.
Rambod M, Rafii F. Perceived social support and quality of life in iranian hemodialysis patients. J Nurs Scholarsh. 2010;42:242–9. https://doi.org/10.1111/j.1547-5069.2010.01353.x.
Silva da SM, Braido NF, Ottaviani AC, Gesualdo GD, Zazzetta MS, Orlandi Fde S. Social support of adults and elderly with chronic kidney disease on dialysis. Rev Lat Am Enfermagem. 2016;24:e2752. https://doi.org/10.1590/1518-8345.0411.2752.
Bapat U, Nayak SG, Kedleya PG, Gokulnath. Demographics and social factors associated with acceptance of treatment in patients with chronic kidney disease. Saudi J Kidney Dis Transpl. 2008;19:132–6.
Shirazian S, Grant CD, Aina O, Mattana J, Khorassani F, Ricardo AC. Depression in chronic kidney disease and end-stage renal disease: similarities and differences in diagnosis, epidemiology, and management. Kidney Int Rep. 2016;2:94–107. https://doi.org/10.1016/j.ekir.2016.09.005.
Virani A, Shah RP, Haneef G, Khan AT, Dias CC, Pereira KN, et al. Depression impairs level of functioning in chronic kidney disease inpatients: a case-control study. Cureus. 2021;13:e16017. https://doi.org/10.7759/cureus.16017.
Odden MC, Whooley MA, Shlipak MG. Depression, stress, and quality of life in persons with chronic kidney disease: the heart and soul study. Nephron Clin Pract. 2006;103:c1–7. https://doi.org/10.1159/000090112.
Seng JJB, Tan JY, Yeam CT, Htay H, Foo WYM. Factors affecting medication adherence among pre-dialysis chronic kidney disease patients: a systematic review and meta-analysis of literature. Int Urol Nephrol. 2020;52(5):903–16. https://doi.org/10.1007/s11255-020-02452-8.
Meng F, Qi Y, Chen X, et al. The synergistic effect of depression and moderate chronic kidney disease on the all-cause and cardiovascular disease mortality among adults: a retrospective cohort study. BMC Nephrol. 2022;23:330. https://doi.org/10.1186/s12882-022-02957-7.
Sqalli-Houssaini T, Ramouz I, Fahi Z, Tahiri A, Sekkat FZ, Ouzeddoun N et al. Effects of anxiety and depression on haemodialysis adequacy. Nephrol Ther. 2005;1:31 – 7. French. https://doi.org/10.1016/j.nephro.2005.01.007.
Chiang HH, Livneh H, Yen ML, Li TC, Tsai TY. Prevalence and correlates of depression among chronic kidney disease patients in Taiwan. BMC Nephrol. 2013;14:78. https://doi.org/10.1186/1471-2369-14-78.
Mosleh H, Alenezi M, Johani SA, Alsani A, Fairaq G, Bedaiwi R. Prevalence and factors of anxiety and depression in chronic kidney disease patients undergoing hemodialysis: a cross-sectional single-center study in Saudi Arabia. Cureus. 2020;12:e6668. https://doi.org/10.7759/cureus.6668.
Kavalnienė R, Deksnyte A, Kasiulevičius V, Šapoka V, Aranauskas R, Aranauskas L. Patient satisfaction with primary healthcare services: are there any links with patients’ symptoms of anxiety and depression? BMC Fam Pract. 2018;19:90. https://doi.org/10.1186/s12875-018-0780-z.
Lilympaki I, Makri A, Vlantousi K, Koutelekos I, Babatsikou F, Polikandrioti M. Effect of perceived social support on the levels of anxiety and depression of hemodialysis patients. Mater Sociomed. 2016;28:361–5. https://doi.org/10.5455/msm.2016.28.361-365.
Christensen AJ, Van Liew JR, Kellerman QD, O’Hara MW. Depression in chronic kidney disease [Internet]. Oxford Handbooks Online. The Oxford Handbook of Depression and Comorbidity; 2014 [cited 2022Jul4]. Richards CS, editor. https://www.oxfordhandbooks.com/view/https://doi.org/10.1093/oxfordhb/9780199797004.001.0001/oxfordhb-9780199797004-e-013.
Tsai YC, Chiu YW, Hung CC, Hwang SJ, Tsai JC, Wang SL, et al. Association of symptoms of depression with progression of CKD. Am J Kidney Dis. 2012;60:54–61. https://doi.org/10.1053/j.ajkd.2012.02.325.
Lee YJ, Kim MS, Cho S, Kim SR. Association of depression and anxiety with reduced quality of life in patients with predialysis chronic kidney disease. Int J Clin Pract. 2013;67:363–8. https://doi.org/10.1111/ijcp.12020.
Danielle FMH, Mahamat M, Victorine N, Vincent N, Fernande TOA, Marie-Patrice H, et al. Epidemiology profile and associated factors of depression in chronic kidney disease stage 3–5 and chronic haemodialysis patients in Cameroon. Arch Nephrol Urol. 2020;3:108–20.
Dziubek W, Pawlaczyk W, Rogowski L, Stefanska M, Golebiowski T, Mazanowska O, et al. Assessment of Depression and anxiety in patients with chronic kidney Disease and after kidney Transplantation-A comparative analysis. Int J Environ Res Public Health. 2021;18:10517. https://doi.org/10.3390/ijerph181910517.
Hettiarachchi R, Abeysena C. Association of poor social support and financial insecurity with psychological distress of chronic kidney disease patients attending National Nephrology Unit in Sri Lanka. Int J Nephrol. 2018;2018:5678781. https://doi.org/10.1155/2018/5678781.
Shirazian S, Grant CD, Aina O, Mattana J, Khorassani F, Ricardo AC. Depression in Chronic Kidney Disease and End-Stage Renal Disease. Similarities and differences in diagnosis, epidemiology, and management. Kidney Int Rep. 2016;2:94–107. https://doi.org/10.1016/j.ekir.2016.09.005.
Acknowledgements
I wish to acknowledge the patients who provided their time to participate, the medical students who assisted with data collection, and the staff from the renal clinic of SFGH who helped with the research.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Author’s contributionsMB conceptualized, designed, conducted, and reviewed the study and wrote and revised the manuscript; GL performed the statistical analysis and edited the manuscript. CL assisted in editing the manuscript and designing the questionnaire.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the Southwest Regional Health Authority, Trinidad and Tobago. We confirm that all methods were performed in accordance with their relevant guidelines and regulations. All participants gave their verbal informed consent to participate in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: the caption of Figure 5 has been updated.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bahall, M., Legall, G. & Lalla, C. Depression among patients with chronic kidney disease, associated factors, and predictors: a cross-sectional study. BMC Psychiatry 23, 733 (2023). https://doi.org/10.1186/s12888-023-05249-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-023-05249-y