Abstract
Background
Loneliness and social isolation are increasingly recognised as prevalent among people with mental health problems, and as potential targets for interventions to improve quality of life and outcomes, as well as for preventive strategies. Understanding the relationship between quality and quantity of social relationships and a range of mental health conditions is a helpful step towards development of such interventions.
Purpose
Our aim was to give an overview of associations between constructs related to social relationships (including loneliness and social isolation) and diagnosed mental conditions and mental health symptoms, as reported in systematic reviews of observational studies.
Methods
For this umbrella review (systematic review of systematic reviews) we searched five databases (PsycINFO, MEDLINE, EMBASE, CINAHL, Web of Science) and relevant online resources (PROSPERO, Campbell Collaboration, Joanna Briggs Institute Evidence Synthesis Journal). We included systematic reviews of studies of associations between constructs related to social relationships and mental health diagnoses or psychiatric symptom severity, in clinical or general population samples. We also included reviews of general population studies investigating the relationship between loneliness and risk of onset of mental health problems.
Results
We identified 53 relevant systematic reviews, including them in a narrative synthesis. We found evidence regarding associations between (i) loneliness, social isolation, social support, social network size and composition, and individual-level social capital and (ii) diagnoses of mental health conditions and severity of various mental health symptoms. Depression (including post-natal) and psychosis were most often reported on, with few systematic reviews on eating disorders or post-traumatic stress disorder (PTSD), and only four related to anxiety. Social support was the most commonly included social construct. Our findings were limited by low quality of reviews and their inclusion of mainly cross-sectional evidence.
Conclusion
Good quality evidence is needed on a wider range of social constructs, on conditions other than depression, and on longitudinal relationships between social constructs and mental health symptoms and conditions.
Similar content being viewed by others
Introduction
Evidence is accumulating on the effects of social relationships, or of the lack of them, on physical and mental health. Loneliness and social isolation have been associated with increased mortality rates in two meta-analytic reviews, with comparable effect sizes to those observed for smoking, obesity, and physical inactivity as risk behaviors [1, 2]. Loneliness and social isolation are longitudinally associated with the development of cardiovascular disease [3], elevated blood pressure [4, 5], and increased fatigue and pain [6]. Among people with mental health problems, loneliness and social isolation are more prevalent than in the general population [7, 8]. Associations with loneliness and social isolation have been reported for depressive disorders [9, 10] and symptoms [11], self-harm [12], psychosis [13, 14], being diagnosed with a “personality disorder” [15], cognitive decline [16, 17], mild cognitive impairment, and dementia [18]. In a rapidly expanding research field, an up-to-date synthesis is needed of evidence on whether, and in what ways, loneliness, social isolation, and related constructs are associated with the incidence and prevalence of a range of mental health conditions, and with their outcomes.
Several other social constructs are related to loneliness and social isolation, including social support, social networks, individual social capital, confiding relationships, connectedness and alienation. Wang et al. [19] have proposed a conceptual model to incorporate these constructs related to social relationships at the individual level in mental health research. According to this model, these constructs can be grouped as: (i) perceived or subjective experiences of social relationships (such as loneliness, perceived social isolation, social support, confiding relationships or individual-level social capital); (ii) objective aspects of social isolation (such as the number of social contacts and social network size), or (iii) constructs that combine measures of both quality and quantity of social relationships (such as social support from members of an individual’s social network).
Several systematic reviews have been published regarding associations between constructs related to social relationships and aspects of mental health, e.g. [10, 20,21,22,23]. However, these reviews have typically focused on specific mental health outcomes in particular populations, so that they do not provide a holistic stock-take of the overall state of evidence in this field, its implications for research, policy and practice, and the gaps still to be addressed.
Umbrella reviews, which are systematic reviews of the systematic review evidence [24], can inform policy, practice and further research by providing a systematic overview of current evidence and its gaps. One recent umbrella review explored the associations between loneliness and outcome measures related to mental health [25]. This concluded that loneliness has a range of adverse impacts on mental and physical health outcomes, but it did not include other related constructs such as social isolation, or reviews of associations between loneliness and social isolation and mental health diagnoses. To our knowledge, there is no umbrella review that synthesises the evidence for associations between a comprehensive set of constructs related to social relationships and specific mental health problems. Such a review has potential value in allowing policy makers, clinicians and researchers to identify areas in which there is a robust and actionable body of evidence regarding connections between mental health conditions and social relationships, and those in which there is a pressing need for more evidence.
This umbrella review addresses this gap by providing an updated and comprehensive overview of the evidence on the associations between a full range of social constructs at the individual level (Table 1) and mental health diagnoses and symptoms in both clinical and population-based samples. The constructs we used to encapsulate important aspects of social relationships including loneliness and isolation are those identified by Wang et al. [19] in their conceptual review. We aimed to address the following linked research questions:
-
1.
What is the evidence from systematic reviews regarding associations in general population samples between constructs related to social relationships, and presence of mental health conditions and symptoms?
-
2.
What evidence is there from systematic reviews regarding associations between constructs related to social relationships and severity of psychiatric symptoms among people diagnosed with mental health conditions?
-
3.
What evidence is there from systematic reviews of longitudinal relationships between constructs related to social relationships and risk of onset of mental health conditions in the general population?
Methods
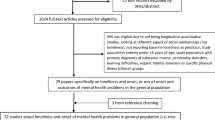
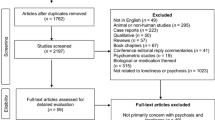
We followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Fig. 1). The protocol for this review was pre-registered with the international Prospective Register of Systematic Reviews.
(PROSPERO: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020192509).

From: Page MJ, McKenzie JE, Boosuvt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. Doi:1136/bmj.n71For more information, visit: http://www.prisma-statement.org/
Prisma diagram identification of studies via databases and registers
Inclusion and exclusion criteria
Included exposures: measures related to social relationships
We included the subjective aspects of social relationships and objective measures of social network size and structure identified in the conceptual review by Wang et al. [19] to encapsulate the main dimensions of social relationships assessed in mental health research. Table 1 summarises and defines the included domains of measurement. We excluded dimensions of social relationships beyond the individual level, such as ecological social capital or social exclusion, following Wang et al. [19].
Included outcomes: mental health measures
We considered a full range of mental health diagnoses and psychiatric symptoms, but we excluded neurodegenerative diagnoses (e.g., dementia), neurodevelopmental disorders (e.g., intellectual disabilities), general wellbeing outcomes and suicide-related outcomes, as well as cohorts of people selected on the basis of a primary physical health diagnosis.
Included methods
We included reviews of quantitative studies (cross-sectional and longitudinal) of associations between constructs related to social relationships (exposures; see above) and mental health diagnoses or psychiatric symptom severity (outcomes) in clinical and general population samples. We included meta-analyses, narrative systematic reviews and any other literature reviews that followed systematic methods. Included reviews varied in whether they reported adjusted and/or unadjusted associations. We excluded individual empirical studies and reviews that were not systematic. We did not apply any restrictions by publication date, language or age to our search.
Search strategy
We searched PsycINFO, MEDLINE, EMBASE, CINAHL, and Web of Science databases. We also searched online repositories of systematic reviews: PROSPERO, Campbell Collaboration, and the Joanna Briggs Institute Evidence Synthesis Journal.
The following search terms related to social isolation and loneliness were used following the conceptual review by Wang et al. [19]: social isolation OR loneliness OR social network* OR social support OR confiding OR confide OR social contact* OR social relation* OR social capital.
The above terms were combined with the following search terms for mental health problems and symptoms:
(mental OR psychiatr* OR schizo* OR psychosis OR psychotic OR depress* OR mania* OR manic OR bipolar near/5 (disorder or disease or illness) OR anxiety) OR (Eating Disorder* OR Anorexia Nervosa OR Bulimia Nervosa OR Binge Eating Disorder) OR personality disorder* OR borderline personality OR emotionally unstable personality OR histrionic personality or narcissistic personality OR antisocial personality OR paranoid personality OR schizoid personality OR schizotypal personality OR avoidant personality OR dependent personality OR obsessive compulsive personality).
The search strategy for Medline appears in full in Supplementary Table S1; this was adapted to other search engines. The results of all searches were imported into EndNote. The initial search was run in August 2019 with updates in July 2020 and January 2022. Following removal of duplicate citations, a reviewer (MB or YN) screened the abstracts and titles of all articles against the inclusion criteria, and second reviewers (EP, MT) randomly screened 10% of included abstracts to check agreement. MB, EP, YN and MT screened the full texts of selected articles, with all full texts screened by a second reviewer. AP and EP discussed any disagreements and clarified criteria to achieve good consistency. Data were extracted from included reviews independently by nine reviewers (MB, EP, JY, EC, AS, LKC and MC, YN and MT): senior researchers MB and EP supervised the other reviewers to ensure consistency and checked extracted data.
For included studies, we developed and piloted a pro forma that allowed extraction of data on setting(s), objectives of the review, type of review, inclusion criteria, number of included studies, publication date range for included studies, type of analysis, and outcomes reported relating to mental health and to loneliness, social isolation and related constructs.
Quality assessment
Seven reviewers (JY, EC, AS, LKC, MC, MT and YN) independently assessed the methodological quality of included studies under the supervision of MB and EP, using a modified version of AMSTAR (A Measurement Tool to Assess Systematic Reviews) (Supplementary Table S2). One reviewer (MT) independently quality rated all included reviews to ensure consistency, and two further reviewers (YD, MH) then checked these again. The AMSTAR-2 tool has 16 items in total and enables appraisal of systematic reviews. Item 7, which assesses adequacy of explanations for excluding studies from reviews at the full text stage was modified (reviews were rated as a “no” but not as critically flawed if they included some explanations for exclusion but not a full list, and as critically flawed if no explanation was given) and Items 3, 10 and 16 (on interventions, funding and conflict of interest) were excluded because of limited relevance or feasibility. We included rapid systematic reviews and scoping reviews if the searches and data extraction were systematic.
Data synthesis
We conducted a narrative synthesis: we grouped reviews according to disorder or symptom type, and within these categories we separated them by different social constructs. Social constructs were grouped following Wang et al’s typology. Reviews may appear in more than one section of the narrative synthesis if they included multiple social constructs e.g. both loneliness and social support. Most reviews focused on broad groups of mental health conditions, such as depressive illnesses, conditions related to anxiety, perinatal conditions and psychosis: we were able to categorise the reviews straightforwardly by grouping together those reporting that they focused on the same, or similar mental health conditions. In our narrative, we distinguish reviews that report results from meta-analysis, and those that are longitudinal rather than reporting on cross-sectional associations. Where possible, we distinguished evidence on symptom severity versus diagnosis.
Results
In total, 53 systematic reviews were included in the final umbrella review (Tables 2 and 3; Fig. 1), which together included 1,657 studies, of which 340 (21%) were longitudinal (Supplementary Table S3, showing study methodologies). Supplementary Table S4 provides details of the 147 studies that were included in more than one review: thus fewer than 10% of primary studies were included in more than one review. Of the 53 included reviews, 31 used narrative synthesis, 17 included meta-analyses, and five conducted both meta-analysis and narrative synthesis. Locations of studies included within the systematic reviews encompassed Europe, Asia, Africa, North and Central America and Australasia, although there were very few studies from lower income countries. Reviews were published between 2005 and 2021, with only three published prior to 2013. No deviations from the PROSPERO protocol were identified.
Twenty-one studies focused on depression, of which 16 related solely to depression and the other four to depression in conjunction with other disorders such as anxiety, obsessive compulsive disorder (OCD), or psychosis. Ten reviews investigated peri- or post-natal depression; seven psychosis; six Post-Traumatic Stress Disorder (PTSD); four mental health in general (i.e. not differentiating conditions); one anxiety and a further two anxiety in conjunction with other disorders. Three reviews focused specifically on mental health and loneliness during the COVID-19 pandemic.
Five different social constructs featured as the analysed exposures across the reviews: 29 reviews focused on social support; 11 on loneliness, sometimes together with measures of social isolation, and 2 on social capital. Eleven reviews investigated a combination of these constructs alongside social networks. Clear differentiations were not always made between constructs such as loneliness and social isolation, so that sometimes we report on these together below. See Table 2 for more detail.
The quality of reviews according to AMSTAR ratings tended to be low (Supplementary Table S2): 27 reviews were assessed as critically low in quality, 14 as low quality, and 12 as of moderate quality. Common critical flaws were failure to establish clear review methods pre-publication, such as via PROSPERO pre-registration, and insufficient discussion by review authors of the risk of bias when interpreting results. Of note only two reviews included evidence from randomised controlled trials (RCTs): one review included three RCTs alongside other study designs but could only summarise findings in its narrative review as they were not eligible for inclusion in their meta-analysis [26], whilst one other review included one RCT alongside other study designs [27].
Methodological and statistical heterogeneity across reviews prevented useful meta-analyses so we undertook a narrative synthesis. Headings below reflect topics on which there is evidence to report: we do not include sections for combinations of social constructs and mental health outcomes for which we found no relevant reviews.
Depression
Twenty-one reviews focused on links between depression and a range of constructs, sometimes including more than one social outcome in each review.
Loneliness and depression
Four reviews focused on older adults [28,29,30,31], one on adults in the general population [32], one on adults experiencing mental illness [33], and two on adolescents [10, 34]. Reviews varied in operationalisations of “depression” (clinical diagnosis versus symptoms), but findings appeared similar regardless of the approach to measurement.
For example, a recent narrative systematic review reported that both cross-sectional and longitudinal studies found statistically significant associations between loneliness and/or social isolation and depressive symptoms in children and adolescents, with longitudinal effects found several years later, and cross-sectional effect sizes being moderate to large [10]. An earlier meta-analysis also found a significant positive relationship between loneliness and depression across 30 studies in adolescents and young people aged 11–23 years [34]. A meta-analysis of mostly cross-sectional studies across the adult age range reported that loneliness was moderately positively correlated with depression, including in distinct models for carers, the elderly, students and service users [32]. The only systematic review focusing solely on longitudinal studies among adults with mental health conditions found only a single study investigating the longitudinal relationship between loneliness and outcomes for people with depression, which reported loneliness to be a predictor of worse depression outcomes [33].
Loneliness was also found to be positively associated with depressive symptoms in older adults. Three reviews of primarily cross-sectional studies reported links between loneliness and perceived social support, and loneliness and depressive symptoms in most included studies [28, 29, 31]. A scoping review using systematic methods included cross-sectional and longitudinal studies, and reported that the overall evidence ‘clearly showed’ a link between loneliness and depression [30].
Social support and depression
Eighteen reviews investigated depression and social support (Tables 2 and 3). Seven focused on older adults [28, 30, 31, 35,36,37,38], four on adults of all ages [39,40,41,42], and five on children and adolescents [10, 43,44,45,46], including one on LGBQ young people [45]. Wang et al. [33] investigated the relationship between perceived social support and outcome in people with depression, and Edwards et al. [47] reviewed literature on social support and depression among Christian clergymen, a group at high risk of depression.
Three reviews included meta-analyses, all reporting inverse relationships between social support and depressive symptom severity and/or diagnosis. A review including cross-sectional and longitudinal studies found associations between more social support and fewer depressive symptoms for children and adolescents, adults, and older adults [40]. A meta-analysis of studies investigating social support and depression among children and adolescents also found a moderate effect, which held across different sources of support [44]. A meta-analysis of cross-sectional studies in older adults in China reached a similar conclusion [38].
Results varied in other more population-specific reviews. For example, in a narrative synthesis investigating depression amongst adults experiencing traumatic bereavement [41], there was some evidence that social support was associated with depression diagnosis or symptom outcome, but no such evidence in the only included longitudinal study. A systematic review of longitudinal studies in adults experiencing mental illness found that for people with depression, lower perceived social support at baseline was predictive of worse symptoms in 11/13 studies, reduced recovery in 6/7 studies and poorer functioning outcomes in 2/5 studies at subsequent follow-up assessments [33].
In the general population, less perceived social support was associated with depression in a review focused on adolescents [44], and another focused on adults [39]. Likewise, three reviews based primarily on cross-sectional studies examined the relationship between satisfaction with social support and depressive symptom severity and/or risk of developing depression and found an inverse relationship [27, 35, 37].
Most reviews did not differentiate between sources of social support. However, for children and young people, one review found that social support from peers was especially important for children and younger adolescents [44]. A second review of mainly cross-sectional studies [40] found that support from parents was more strongly associated with depression risk than support from friends, particularly for girls. There were inconsistent findings for adults regarding which sources of support are most significant in terms of associations with depression [39, 40]. Among older adults, spousal support had the strongest association with lower levels of depression, followed by support from friends, with less evidence for support from children [40].
Social networks and depression
Six reviews explored associations between social network size and depression onset, diagnosis and/or symptom severity. Four focused on older adults [31, 35,36,37], one on adults in the general population [39] and one on adults with chronic depression [48].
In one review of moderate quality, large social networks were found in most studies to be protective against the onset of depression in the general population (9/13 studies, including five prospective studies of high quality) whereas four studies (two prospective) found no statistically significant association [39]. For people already experiencing chronic depression, social networks appeared to be smaller than those of healthy individuals, or of patients with non-chronic major depression and other disorders [48].
Findings on the association between social network size and depressive symptoms were mixed, with reviews identifying some studies suggesting a protective effect of large social networks and others finding no relationship [36, 37].
Two reviews reported on associations with social network composition in older adults, with one reporting a social network composed mainly of family rather than friends to be associated with lower rates of depression in older adults [37], while a second review reported fewer depressive symptoms among those with a larger and more diverse network [35].
Peri-natal Conditions
Social Support and peri-natal depression
Ten reviews looked at peri- or post-natal depression and its relationship to social support in countries including China, the USA, Australia and Ethiopia [22, 27, 49,50,51,52,53,54,55,56].
Peri-natal findings were consistent in suggesting that lower social support was associated with elevated odds of developing depression. In a meta-analysis of 45 studies, 26 of which were cross-sectional, 37 found a significant negative relationship between social support and developing depression. The narrative element of the paper, which drew on 15 studies, reported similar findings [55]. Two earlier systematic reviews drew similar conclusions. A review of 10 cross-sectional, 14 longitudinal and one RCT studies found lower social support was related to higher scores for both peri- and post-natal depressive symptoms [27]. The review also suggested that social support may play a mediating role between peri- and post-natal symptoms. In a meta-analysis of 10 cross-sectional studies focusing on Chinese women [50], the conclusions were similar to those above, although the economic status of women tended to matter more than social support. In a review of risk factors for paternal peri-natal depression, five out of seventeen studies (three cross sectional, two longitudinal) identified lower social support as a risk factor alongside age, economic status and ethnicity [56] (Tarsuslu et al. 2020).
Social support and peri-natal anxiety
Two reviews investigated peri-natal anxiety [22, 55]. All nine studies included in a meta-analysis reported a significant negative relationship between social support and developing peri-natal anxiety [55]. A second review similarly reported lower levels of social support to be a risk factor for ante-natal anxiety in most included studies [22].
Anxiety
Five reviews investigated social constructs and anxiety: three related to loneliness [10, 34, 57] and two to social support [33, 58].
Loneliness and anxiety
Three reviews investigated loneliness and anxiety, all focused on children and adolescents. A rapid systematic review on children and adolescents in the general population found small to moderate associations between loneliness and social anxiety in cross-sectional studies, while three out of four longitudinal studies found that loneliness was associated with greater subsequent rates of anxiety [10]. An earlier meta-analysis, also focused on adolescents, found mostly significant positive associations between loneliness and social anxiety with a moderate effect size [34].
A recent rapid systematic review [57] regarding children and adolescents with established mental health conditions (including depression, anxiety, and neurodevelopmental disorders) also identified associations between loneliness and anxiety (especially social anxiety) in most included studies, including among autistic participants.
Social support and anxiety
The reviews investigating social support and anxiety focused on the adult population. A recent review [58] reported mixed evidence as to whether social support was a protective factor against severity of anxiety and, on balance, concluded it was not. A systematic review including only longitudinal studies of people with mental health conditions at baseline found significant associations between perceived social support and subsequent anxiety outcomes [33].
Psychosis
Seven systematic reviews investigated social relationship constructs and psychosis. Four focused on loneliness and/or perceived social support [13, 14, 23, 33], and three on social network size and composition [26, 59, 60].
Loneliness and/or perceived social support and psychosis
The only review focusing solely on longitudinal studies found no relevant studies on loneliness in relation to psychosis outcomes. It did report preliminary evidence from two studies for positive associations between perceived social support, and life satisfaction and social functioning [33].
Most of the studies included in the three other reviews were cross-sectional (Table 3). Two included meta-analyses indicating moderate positive associations between loneliness and psychotic symptom severity [13, 23]. Chau et al. [23] distinguished different types of psychosis symptoms and found associations between loneliness and both positive symptoms (30 studies, only three of which were longitudinal), and negative symptoms (15 cross-sectional studies).
The third systematic review that focused on loneliness in psychosis included perceived social isolation in the search terms and reported inconsistent findings, with some studies reporting associations between loneliness and psychosis symptoms and others finding none [14].
Social networks and psychosis
Three systematic reviews investigated social networks among people with diagnosed psychotic disorders [26, 59, 60].
Degnan et al. [26] conducted a meta-analysis of cross-sectional data and found that smaller social network size was moderately associated with more severe overall psychiatric symptoms and negative symptoms, but not positive symptoms. Most of the studies had samples of participants with a diagnosis of schizophrenia. In one narrative review, participants with first episode psychosis were found to have smaller social networks and reported less satisfactory social support compared to general population controls [60]. In the same review, scores on measures related to psychosis or schizotypy were found to be negatively related to social network size and social support in samples from the general population who reported psychotic experiences or had high levels of schizotypy traits [60].
Another narrative review found evidence that a larger proportion of the social networks of people with psychosis are family members rather than friends, although lack of general population control groups and inconsistent methods for measuring social networks limited conclusions [59].
PTSD
Social support and PTSD
Seven reviews examined the relationship between PTSD and social support. Two of these focused on children [61, 62], two reported on the adult population in general [42, 63], and three on specific adult populations including military veterans [64]; betrayal trauma survivors [65]; and adults bereaved by sudden or violent death [41]. All papers focused on symptom severity and most included studies were cross-sectional.
In a series of meta-analyses by the same group of authors [63,64,65], the association between social support and symptom severity was investigated across three different populations: military veterans, adults in the general population, and adult betrayal survivors. In each population, a moderate association was found between greater social support, perceived or enacted, and less severe PTSD symptoms.
All six studies in the review on bereaved adults found that greater social support was associated with lower likelihood of meeting the threshold for PTSD and/or less severe PTSD symptoms [41], including one longitudinal study.
Two meta-analyses investigated PTSD and social support in children and adolescents [61, 62]. A meta-analysis of four cross-sectional studies found a significant positive association between low social support and PTSD with a medium-to-large effect size [62]. A more recent meta-analysis found only a small effect size between social support and PTSD symptoms, with considerable heterogeneity across results [61].
Bipolar disorder and constructs related to social relationships
Three systematic reviews examined relationships between social support and bipolar disorder [21, 33, 66]. Overall, the reviews found that people with bipolar disorder have lower levels of social support than the general population [21, 66]. Longitudinal data from one review did not support a clear association between social support and bipolar episode relapse (either manic or depressive) [21]. However, the other two reviews did find evidence to suggest that people with bipolar disorder who have greater social support have fewer recurrences overall and fewer depressive episodes [33, 66]. One review including solely longitudinal studies found that lower perceived support was a significant predictor of greater depressive symptom severity and a longer time to recovery in people diagnosed with bipolar disorder [33].
Eating disorders and constructs related to social relationships
Two systematic reviews investigated eating disorders and a social relationships construct. One looked at social isolation during the Covid-19 pandemic [67] (see COVID-19 section below). Another review focused on social support in relation to anorexia nervosa and bulimia nervosa: all four included studies were cross-sectional [20]. People with eating disorders were found to report receiving less emotional and/or practical social support than general population controls.
General mental health
Five reviews included studies not focused on specific diagnoses, including two examining relationships between social support and mental health in general [68, 69], and a third at social support in relation to all mental health disorders, including groups with a mixture of diagnoses [33]. A further two reviews looked at individual-level social capital in relation to common mental health disorders [70, 71].
Social support and mental ill-health
A systematic review on adults caring for children with HIV reported mixed findings from cross-sectional studies on the relationship between social support and mental ill-health [68]. A second review investigated the mental health of older people in Middle Eastern countries and found that higher levels of social support, especially perceived social support, were associated with better mental health outcomes in eight out of nine studies. In their review of studies investigating the longitudinal relationships between mental health problems and both loneliness and perceived social support, Wang et al. [33] reported on two studies with samples of people with a mixture of mental health conditions. One study found that loneliness at baseline predicted subsequent depression and the other that greater perceived social support predicted higher subsequent quality of life.
Social capital and mental health
Two narrative systematic reviews using largely cross-sectional data (Table 3) found an inverse association between individual-level cognitive social capital and common mental disorders [70, 71], apparent in both cross-sectional and longitudinal studies in the latter review. Individual-level cognitive social capital was defined by the authors as quality of social interactions, measured by asking about participation in social relationships and perceptions of the quality of those relationships. Findings regarding structural social capital (which aims to measure the quantity of social interactions) and common psychiatric conditions were a mixture of positive associations, negative associations and no associations. See Table 3 for details.
COVID-19 pandemic
There were three reviews investigating the association between social constructs and mental ill health during the COVID-19 pandemic. One focused on loneliness [67], one on social support [49] and another on both loneliness and social support [42].
A review focusing on loneliness and eating disorder symptom severity [67] reported mixed and low-quality evidence as to whether social isolation policies during the pandemic were associated with greater eating disorder symptoms, with no clear overall conclusions about the impact of home confinement during the pandemic on eating disorder symptoms. A review focusing on loneliness in relation to PTSD during the pandemic [42] found loneliness to be the strongest psychological predictor of PTSD, with the authors noting both the prevalence and distressing nature of loneliness related to social distancing and isolation measures during Covid-19. In the same review, there was consistent evidence in six cross sectional studies suggesting people with adequate social support were less likely to have PTSD. In one of those studies, the type of social support was important: family support, but not support from friends or partners, was associated with lower PTSD prevalence.
A systematic-review of cross-sectional studies focused on pregnant women’s experiences during the Covid-19 pandemic concluded that women who received more social support were less likely to develop depression or anxiety [49], although associations with socio-economic variables were stronger.
Discussion
Main findings
This umbrella review summarises a body of evidence linking various social constructs relevant to social relationships with a range of mental health diagnoses, with depression and psychosis the conditions most commonly investigated. Our review includes all the constructs identified as related to subjective and objective aspects of social relationships in an influential conceptual review [19] and all major mental health conditions, offering a broad stock-take of the current state of evidence in this field as reflected by systematic reviews.
Regarding what is known so far, much more literature has focused on depression than on any other condition. However, even for this condition, much of the literature reported in reviews is cross-sectional and limited in shedding light on mechanisms or the role of particular forms of social support and social relationships. Regarding cross-sectional findings, most measures of constructs related to loneliness and social isolation appear associated with depression in the expected directions. Some systematic reviews on social support and social network size identify some longitudinal evidence suggesting a protective effect against depression onset or against more severe symptoms. A systematic review focused on adolescents found that loneliness predicts onset of depression and of anxiety.
Regarding other conditions, various reviews report cross-sectional associations between poorer social support and onset and/or severity of symptoms in anxiety (including perinatal anxiety) and PTSD, with some longitudinal evidence for relationships between social support and onset or severity of anxiety. For the relationship between psychosis and loneliness, the two reviews that include a meta-analysis of cross-sectional data both concluded that there is an association between loneliness and psychosis symptoms. However, another review concluded the evidence was of insufficient quality for such a conclusion to be firmly drawn and did not attempt a meta-analysis. A psychosis diagnosis was also found to be cross-sectionally associated with more limited social network size. Some reviews of the longitudinal relationship between social indicators and bipolar disorder reported social support as protective against relapse. Finally, a single review regarding the relationship between eating disorders and social support found cross-sectional evidence for less social support among people with eating disorders.
Many gaps emerged from this overview of reviews. Even for depression, which has yielded the largest amount of literature, reviews report only a limited body of longitudinal evidence to allow clear conclusions to be reached about temporal relationships and potential causality. Most reviews pool studies across countries and cultures, even though relevant social indicators and their impacts might be expected to vary cross-culturally. Likewise, whether patterns vary by gender, demographic group and other socio-demographic factors cannot generally be extrapolated from the reviews. Most measures of social constructs were relatively lacking in nuance: global indicators of loneliness tended to be reported rather than differentiating sub-types, although some studies made distinctions between different types of social support (for example from friends versus family). Evidence on support from peers with relevant personal experience of mental health problems was also generally not reported in the syntheses but has considerable potential practical relevance.
Reviews of literature on anxiety, bipolar and eating disorders identified relatively few studies, most cross-sectional. While a somewhat greater number of primary studies was retrieved in the reviews on psychosis (including schizophrenia), high quality longitudinal studies from which an understanding of causality can be achieved were not retrieved. No review reporting on associations with “personality disorder” diagnosis was found, despite the centrality of social relationships to the difficulties many people with such a diagnosis face, nor were reviews found regarding specific anxiety-related conditions such as obsessive compulsive disorder and social anxiety. Social support was the most commonly assessed social construct in reviews and there were no reviews looking at relationships between individual-level social capital and specific mental health disorders. Where reviews were found, they tended to be of low or critically low quality, confirming significant further potential for conducting high quality reviews in this sphere.
Strengths and Limitations
The main strength of this review was the aggregation of evidence regarding the relationships between multiple constructs related to social connection/relations and a range of mental health conditions in both clinical and general population samples. We followed PRISMA guidelines, pre-registered the protocol and used independent screening to improve the rigor of the review process. Grouping of studies was informed by clinician team members’ views as to what would be more clinically meaningful.
The main limitation of this umbrella review was the generally low quality of included reviews, according to our team’s quality appraisals. Most meta-analyses and reviews included in this umbrella review used cross-sectional data so causality could not be inferred. Because we aggregated the findings of systematic reviews rather than primary studies, details of primary studies not reported in specific systematic reviews will have been lost. Publication dates varied, and primary studies published since review searches will not have been captured in this review of reviews. Some reviews were also included in multiple systematic reviews, although this applied to fewer than 10% of included primary studies. Further limitations of our approach, reflecting the wide scope of our review, were that we double screened all studies only at full text stage, and did not search grey literature (we anticipated yield in terms of good quality unpublished systematic reviews would be low), consult experts to seek further references or carry out hand-searching of reference lists. Our search strategy was reviewed by multiple experienced reviewers within our team (BLE, AP, SJ), but not subject to external peer review. We screened five databases, including both comprehensive and subject-specific ones, as well as repositories of systematic reviews, but we did not include Google Scholar, CENTRAL, or SCOPUS, databases which are included in recent Cochrane Collaboration guidance on designing comprehensive searches for individual studies [72], and which might have retrieved additional systematic reviews. We also did not search for grey literature: this is not recommended in guidance on umbrella reviews that we followed [24] or in the Cochrane Collaboration recommendations for an Overview of Systematic Reviews [73]: however, it may have resulted in the omission of systematic reviews not published in peer-reviewed sources, for example if produced by policy bodies.
The broad scope of our view across many mental health conditions and constructs related to social relationships, and variations in how these were measured, mean that it is challenging to make direct comparisons between findings of different reviews, and a metasynthesis was not feasible. Thus while we can summarise conclusions from a substantial number of reviews, we cannot present statistically robust summary findings for main research questions, nor was grading of overall strength of evidence feasible. Even though we included a wide range of mental health conditions and symptoms, a significant limitation is that in the interests of feasibility, we did not include well-being or positive conceptualisations of mental health, advocated as important for holistic and recovery-focused understanding of mental health [74].
Clinical, research and policy implications
Some of the many gaps in the evidence as reported by systematic reviews have already been identified above, especially in relation to conditions other than depression, to longitudinal studies, and to better quality reviews. However, there is consistent evidence to support associations between certain social constructs and specific psychiatric conditions, particularly depression, post-natal mental health conditions and psychosis, and thus a clear rationale for conducting further longitudinal studies to understand outcomes and the mechanisms underpinning associations. Hypotheses to drive mechanistic studies can be derived not only from cross-sectional studies but also from qualitative research (e.g., Birken et al. [75]) and from relevant lived experience.
Established associations between social constructs and mental health conditions suggest potential benefits in raising clinician awareness of these potential influences on mental health. Work to embed measurement of loneliness and other constructs related to social isolation in routine clinical examinations might yield benefits in raising clinicians’ awareness of their influence on mental health and the potential scope for helpful social interventions. Documenting repeated measures of loneliness could also facilitate longitudinal analyses of anonymised data from electronic health records, advancing understanding of prevalence and potential mechanisms and identifying potential targets for intervention. The UK government recommends using the 3-item UCLA Loneliness Scale and a single item direct measure of loneliness [76]. This presents a low question burden for clinicians and patients as well as being a valid and reliable measure [77]. Cohort studies that include both good quality measures of loneliness, social support and related constructs, and substantial numbers of participants with diagnoses such as psychosis, bipolar disorder, “personality disorder”, anxiety disorders or eating disorders would be of considerable value.
Whilst better epidemiological evidence is very desirable, action to alleviate loneliness among people with mental health problems should not need to wait until a comprehensive body of high-quality observational evidence is available. Especially regarding depression, the substantial evidence for a close relationship with social constructs suggests that the development and testing of theory-driven interventions to prevent onset or improve prognosis by pathways involving social construct is justified, especially as interventions with social targets tend to draw strong support from service users [78]. Regarding other conditions, we are still further from a clear understanding of causal relationships, and high-quality research elucidating pathways between social relationships and conditions such as eating disorders, psychosis, bipolar and “personality disorders” is still needed to develop interventions and policy initiatives with secure foundations. However, given the overall evidence that loneliness and social isolation have negative effects on a wide range of aspects of quality of life and health, including a substantial impact on physical health, there is a case for attempting to alleviate these difficulties among people with mental health conditions that are associated with a greater risk of being lonely and/or lacking in support.
Lived experience commentary by Beverley Chipp
Loneliness and social isolation both have correlations with mental health, however they are distinct entities, and each may exist without the other, or co-occur. Not differentiating, or even using the terms interchangeably, has clouded good research and is challenging to unpick within systematic reviews. The second challenge is the generalised grouping of mental health conditions. This welcomed paper is one of the few which looks at specific diagnoses.
More research is needed beyond depression, for being lonely may itself generate that. The paucity of systematic reviews for anxiety and PTSD is unfortunate as both conditions can compel people to withdraw from social contact. In PTSD it may be a necessary stage in order to decompress, feel safe and heal before restorative socialisation can commence. Anxiety, conversely, may require timely habituation and exposure therapy. These nuances, learned from our lived experience community, highlight the importance of examining discrete mental health conditions, and whilst we can confidently say that building social capital is good, what type is most beneficial or needed for each cohort remains underexplored.
Overall, the relationship between both loneliness and social isolation and mental health conditions and symptoms is shown to be strong, but qualitative work reveals that the relationship is bidirectional [75]. This may extend too to some of the associated behaviours, such as eating disorders, or self-harming. In these ‘chicken or egg’ situations, which is it better to treat first? Or both simultaneously? Again, this may differ according to primary diagnosis. There is a need for more focused longitudinal studies exploring causality, and for co-produced qualitative research to gain deeper understanding of the dynamics. However, the sheer weight of the evidence already suggests there should be no delays in incorporating routine screening for social isolation and loneliness into practice, and establishing appropriate social programmes at the earliest opportunity, particularly noting the protective effect against relapse. Understanding social isolation’s knock-on costs in the bigger picture would make this a prudent investment.
Beverley Chipp (November 2022).
Data Availability
This review relied on published papers and these are available via journal websites, which in some case require institutional access. All the data analysis reported in the review is provided in tables in the main manuscript or in the supplementary material.
Abbreviations
- DSM:
-
Diagnostic and Statistical Manual of Mental Disorders (diagnostic manual)
- ICD:
-
International Classification of Diseases (diagnostic manual)
- OCD:
-
obsessive compulsive disorder
- SAD:
-
seasonal affective disorder
- GAD:
-
generalised anxiety disorder
- PTSS:
-
Post-traumatic stress symptoms
- PTSD:
-
post-traumatic stress disorder UK = United Kingdom
- USA:
-
United States of America
References
Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):e1000316.
Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. 2015;10(2):227–37.
Valtorta NK, Kanaan M, Gilbody S, Ronzi S, Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart. 2016;102(13):1009–16.
Hawkley LC, Thisted RA, Masi CM, Cacioppo JT. Loneliness predicts increased blood pressure: 5-Year cross-lagged analyses in Middle-Aged and older adults. Psychol Aging. 2010;25(1):132–41.
Yang YC, Boen C, Harris KM. Social Relationships and Hypertension in Late Life: evidence from a nationally Representative Longitudinal Study of older adults. J Aging Health. 2015;27(3):403–31.
Jaremka LM, Andridge RR, Fagundes CP, Alfano CM, Povoski SP, Lipari AM, et al. Pain, Depression, and fatigue: loneliness as a longitudinal risk factor. Health Psychol. 2014;33(9):948–57.
Lauder W, Sharkey S, Mummery K. A community survey of loneliness. J Adv Nurs. 2004;46(1):88–94.
Badcock JC, Shah S, Mackinnon A, Stain HJ, Galletly C, Jablensky A, et al. Loneliness in psychotic disorders and its association with cognitive function and symptom profile. Schizophr Res. 2015;169(1–3):268–73.
Meltzer H, Bebbington P, Dennis MS, Jenkins R, McManus S, Brugha TS. Feelings of loneliness among adults with mental disorder. Soc Psychiatry Psychiatr Epidemiol. 2013;48(1):5–13.
Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, et al. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59(11):1218–39.
Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychol Aging. 2006;21(1):140–51.
Shaw RJ, Cullen B, Graham N, Lyall DM, Mackay D, Okolie C, et al. Living alone, loneliness and lack of emotional support as predictors of suicide and self-harm: a nine-year follow up of the UK Biobank cohort. J Affect Disord. 2021;279:316–23.
Michalska da Rocha B, Rhodes S, Vasilopoulou E, Hutton P. Loneliness in psychosis: a meta-analytical review. Schizophr Bull. 2018;44(1):114–25.
Lim MH, Gleeson JFM, Alvarez-Jimenez M, Penn DL. Loneliness in psychosis: a systematic review. Soc Psychiatry Psychiatr Epidemiol. 2018;53(3):221–38.
Martens WHJ. Schizoid personality disorder linked to unbearable and inescapable loneliness. Eur J Psychiatry. 2010;24(1):38–45.
Boss L, Kang DH, Branson S. Loneliness and cognitive function in the older adult: a systematic review. Int Psychogeriatr. 2015;27(4):541–55.
Evans IEM, Martyr A, Collins R, Brayne C, Clare L. Social isolation and cognitive function in later life: a systematic review and Meta-analysis. J Alzheimers Disease. 2019;70:119–S144.
Lara E, Martin-Maria N, De la Torre-Luque A, Koyanagi A, Vancampfort D, Izquierdo A, Miret M. Does loneliness contribute to mild cognitive impairment and dementia? A systematic review and meta-analysis of longitudinal studies. Ageing Res Rev. 2019;52:7–16.
Wang J, Lloyd-Evans B, Giacco D, Forsyth R, Nebo C, Mann F, et al. Social isolation in mental health: a conceptual and methodological review. Soc Psychiatry Psychiatr Epidemiol. 2017;52(12):1451–61.
Arcelus J, Haslam M, Farrow C, Meyer C. The role of interpersonal functioning in the maintenance of eating psychopathology: a systematic review and testable model. Clin Psychol Rev. 2013;33(1):156–67.
Greenberg S, Rosenblum KL, McInnis MG, Muzik M. The role of social relationships in bipolar disorder: a review. ’ Psychiatry research. 2014;219(2):248–54.
Bayrampour H, Vinturache A, Hetherington E, Lorenzetti DL, Tough S. Risk factors for antenatal anxiety: a systematic review of the literature. J Reproductive Infant Psychol. 2018;36(5):476–503.
Chau AK, Zhu C, So SH. Loneliness and the psychosis continuum: a meta-analysis on positive psychotic experiences and a meta-analysis on negative psychotic experiences. Int Rev Psychiatry. 2019;31(5–6):471–90.
Papatheodorou S. Umbrella reviews: what they are and why we need them. Eur J Epidemiol. 2019;34(6):543–6.
Solmi M, Veronese N, Galvano D, Favaro A, Ostinelli EG, Noventa V, et al. Factors Associated with loneliness: an Umbrella Review of Observational Studies. J Affect Disord. 2020;271:131–8.
Degnan A, Berry K, Sweet D, Abel K, Crossley N, Edge D. Social networks and symptomatic and functional outcomes in schizophrenia: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. 2018;53(9):873–88.
Razurel C, Kaiser B, Sellenet C, Epiney M. Relation between perceived stress, social support, and coping strategies and maternal well-being: a review of the literature. Women Health. 2013;53(1):74–99.
Choi H, Irwin MR, Cho HJ. Impact of social isolation on behavioral health in elderly: systematic review. World J psychiatry. 2015;5(4):432.
Cohen-Mansfield J, Hazan H, Lerman Y, Shalom V. Correlates and predictors of loneliness in older-adults: a review of quantitative results informed by qualitative insights. Int Psychogeriatr. 2016;28(4):557.
Courtin E, Knapp M. Social isolation, loneliness and health in old age: a scoping review. Health Soc Care Commun. 2017;25(3):799–812.
Worrall C, Jongenelis M, Pettigrew S. Modifiable protective and risk factors for depressive symptoms among older community-dwelling adults: a systematic review. J Affect Disord. 2020;272:305–17.
Erzen E, Çikrikci Ö. The effect of loneliness on depression: a meta-analysis. Int J Soc Psychiatry. 2018;64(5):427–35.
Wang J, Mann F, Lloyd-Evans B, Ma R, Johnson S. Associations between loneliness and perceived social support and outcomes of mental health problems: a systematic review. BMC Psychiatry. 2018;18(1):1–16.
Mahon NE, Yarcheski A, Yarcheski TJ, Cannella BL, Hanks MM. A meta-analytic study of predictors for loneliness during adolescence. Nurs Res. 2006;55(5):308–15.
Schwarzbach M, Luppa M, Forstmeier S, König HH, Riedel-Heller SG. Social relations and depression in late life—a systematic review. Int J Geriatr Psychiatry. 2014;29(1):1–21.
Guo M, Stensland M. A systematic review of correlates of depression among older chinese and korean immigrants: what we know and do not know. Aging Ment Health. 2018;22(12):1535–47.
Mohd T, Yunus R, Hairi F, Hairi NN, Choo WY. Social support and depression among community dwelling older adults in Asia: a systematic review. BMJ open. 2019;9(7):e026667.
Qiu QW, Qian S, Li JY, Jia RX, Wang YQ, Xu Y. Risk factors for depressive symptoms among older chinese adults: a meta-analysis. J Affect Disord. 2020;277:341–6.
Santini ZI, Koyanagi A, Tyrovolas S, Mason C, Haro JM. The association between social relationships and depression: a systematic review. J Affect Disord. 2015;175:53–65.
Gariepy G, Honkaniemi H, Quesnel-Vallee A. Social support and protection from depression: systematic review of current findings in western countries. Br J Psychiatry. 2016;209(4):284–93.
Scott H, Pitman A, Kozhuharova P, Lloyd-Evans B. A systematic review of studies describing the influence of informal social support on psy1hological wellbeing in people bereaved by sudden or violent causes of death. BMC Psychiatry. 2020; Vol 20 2020, ArtID 265 20.
Hong S, Kim H, Park MK. Impact of COVID-19 on post-traumatic stress symptoms in the general population: an integrative review. Int J Ment Health Nurs. 2021;30(4):834–46.
Guruge S, Thomson MS, George U, Chaze F. Social support, social conflict, and immigrant women’s mental health in a canadian context: a scoping review. J Psychiatr Ment Health Nurs. 2015;22(9):655–67.
Rueger S, Malecki C, Pyun Y, Aycock C, Coyle S. A meta-analytic review of the association between perceived social support and depression in childhood and adolescence. Psychol Bull. 2016;142(10):1017–67.
Hall W. Psychosocial risk and protective factors for Depression among Lesbian, Gay, Bisexual, and Queer Youth: a systematic review. J Homosex. 2018;65(3):263–316.
Gilmour J, Machin T, Brownlow C, Jeffries C. Facebook-Based Social Support and Health: a systematic review. Psychol Popular Media. 2020;9(3):328–46.
Edwards L, Bretherton R, Gresswell M, Sabin-Farrell R. The relationship between social support, spiritual well-being, and depression in Christian clergy: a systematic literature review. Mental Health Religion & Culture. 2020;23(10):857–73.
Visentini C, Cassidy M, Bird VJ, Priebe S. Social networks of patients with chronic depression: a systematic review. J Affect Disord. 2018;241:571–8.
Fan S, Guan JP, Cao L, Wang ML, Zhao H, Chen L. L Psychological effects caused by COVID-19 pandemic on pregnant women: a systematic review with meta-analysis. Asian J Psychiatry. 2021; 56.
Nisar A, Yin J, Waqas A, Bai X, Wang DL, Rahman A. Prevalence of perinatal depression and its determinants in Mainland China: a systematic review and meta-analysis. J Affect Disord. 2020;277:1022–37.
Zeleke TA, Getinet W, Tessema ZT, Gebeyehu K. Prevalence and associated factors of post-partum depression in Ethiopia. A systematic review and meta-analysis. PLoS ONE. 2021; 16(2).
Tolossa T, Fetensa G, Yilma M, Abadiga B, Wakuma M, Besho G et al. Postpartum depression and associated factors among postpartum women in Ethiopia: a systematic review and meta-analysis. Public Health Rev. 2020; 41(1).
Desta M, Memiah P, Kassie B, Ketema DB, Amha H, Getaneh T, et al. Postpartum depression and its association with intimate partner violence and inadequate social support in Ethiopia: a systematic review and meta-analysis. J Affect Disord. 2021;279:737–48.
Qi WJ, Zhao FQ, Liu YT, Li Q, Hu J. Psychosocial risk factors for postpartum depression in chinese women: a meta-analysis. BMC Pregnancy Childbirth. 2021; 21(1).
Bedaso A, Adams J, Peng W, Sibbritt D. The relationship between social support and mental health problems during pregnancy: a systematic review and meta-analysis. Reproductive Health. 2021;18(1):1–23.
Tarsuslu B, Durat G, Altinkaynak S. Postpartum Depression in fathers and Associated Risk factors: a systematic review. Turk Psikiyatri Dergisi. 2020;31(4):280–9.
Hards E, Loades ME, Higson-Sweeney N, Shafran R, Serafimova T, Brigden A et al. Loneliness and mental health in children and adolescents with pre-existing mental health problems: a rapid systematic review. Br J Clin Psychol. 2021; 16.
Zimmermann M, Chong AK, Vechiu C, Papa A. Modifiable risk and protective factors for anxiety disorders among adults: A systematic review. Psychiatry Research. 2020; Vol 285 2020, ArtID 112705 285.
Palumbo C, Volpe U, Matanov A, Priebe S, Giacco D. Social networks of patients with psychosis: a systematic review. BMC Res Notes. 2015;8(1):1–12.
Gayer-Anderson C, Morgan C. Social networks, support and early psychosis: a systematic review. Epidemiol psychiatric Sci. 2013;22(2):131.
Allen L, Jones C, Fox A, Copello A, Jones N, Meiser-Stedman R. The correlation between social support and post-traumatic stress disorder in children and adolescents: a meta-analysis. J Affect Disord. 2021;294:543–57.
Trickey D, Siddaway AP, Meiser-Stedman R, Serpell L, Field AP. A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clin Psychol Rev. 2012;32(2):122–38.
Zalta AK, Tirone V, Orlowska D, Blais RK, Lofgreen A, Klassen B, et al. Examining moderators of the relationship between social support and self-reported PTSD symptoms: a meta-analysis. Psychol Bull. 2021;147(1):33–54.
Blais RK, Tirone V, Orlowska D, Lofgreen A, Klassen B, Held P et al. Self-reported PTSD symptoms and social support in US military service members and veterans: a meta-analysis. Eur J Psychotraumatology 2021; 12(1).
Tirone V, Orlowska D, Lofgreen AM, Blais RK, Stevens NR, Klassen B, et al. The association between social support and posttraumatic stress symptoms among survivors of betrayal trauma: a meta-analysis. Eur J Psychotraumatology. 2021;12(1):1883925.
Studart PM, Bezerra Filho S, Studart ABD, Galvao-de Almeida A, Miranda-Scippa Â. Social support and bipolar disorder. Archives of Clinical Psychiatry. 2015;42(4):95–9.
Miniati M, Marzetti F, Palagini L, Marazziti D, Orru G, Conversano C et al. Eating Disorders Spectrum during the COVID pandemic: a systematic review. Front Psychol 2021; 12.
Casale M, Wild L. Effects and processes linking social support to caregiver health among HIV/AIDS-affected carer-child dyads: a critical review of the empirical evidence. AIDS Behav. 2013;17(5):1591–611.
Tajvar M, Fletcher A, Grundy E, Arab M. Social support and health of older people in Middle Eastern countries: a systematic review. Australas J Ageing. 2013;32(2):71–8.
De Silva MJ, McKenzie K, Harpham T, Huttly SR. Social capital and mental illness: a systematic review. J Epidemiol community health. 2005;59(8):619–27.
Ehsan AM, De Silva MJ. Social capital and common mental disorder: a systematic review. J Epidemiol Community Health. 2015;69(10):1021–8.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook.
Pollock M, Fernandes RM, Becker LA, Pieper D, Hartling L, Chapter V. Overviews of Reviews. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook.
Galderisi S, Heinzk A, Kastrup M, Beezhold J, Sartorius M. Toward a new definition of mental health. ’World Psychiatry. 2015;14(2):231–3.
Birken M, Chipp B, Shah P, Rowan Olive R, Nyikavaranda P, Hardy J, et al. Exploring the experiences of loneliness in adults with mental health problems: a co-produced participatory qualitative interview study. PLoS ONE. 2022;18(3):e0280946.
Office for National. Statistics Measuring loneliness: guidance for use of the national indicators on surveys. 2018.
Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. (). ‘A short scale for measuring loneliness in large surveys: results from two Population-Based Studies.’ Research on aging. 2004; 26(6): 655–72.
Johnson S. Social interventions in mental health: a call to action. Soc Psychiatry Psychiatr Epidemiol. 2017;52(3):245–7.
Acknowledgements
Other co-applicants and collaborators in the UKRI Loneliness and Social Isolation in Mental Health Research Network commented on aspects of design and conduct of the study.
Funding
The authors are members of the UKRI-funded Loneliness and Social Isolation in Mental Health Research Network [grant number ES/S004440/1], which is led by SJ and AP, coordinated by EP and MB, and of which BLE, JK, and DO are co-investigators.
Author information
Authors and Affiliations
Contributions
MB, EP, SJ, AP, BLE, JK conceived the research, MB ran the searches, MB, MT, YN and EP screened the papers, MB, EP JY, EC, AS, LKC, MT, YN and MC completed data extraction and quality ratings, SP, JW, MS and SJ wrote sections of the first drafts of the paper, and BC provided lived experience feedback and wrote the lived experience commentary. All authors commented on the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This review relied on published data and ethical approval was not required.
Consent for publication
This review does not include personal data and consent for publication was not required.
Competing interests
JW, AP, BLE and SJ are authors of two systematic reviews included in this umbrella review. JW, BLE and SJ are authors of a conceptual review underpinning selection of search terms [19]. All other authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pearce, E., Birken, M., Pais, S. et al. Associations between constructs related to social relationships and mental health conditions and symptoms: an umbrella review. BMC Psychiatry 23, 652 (2023). https://doi.org/10.1186/s12888-023-05069-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-023-05069-0