Abstract
Background
Patients with severe mental disorders suffer from higher rates of poor somatic health and have shorter life expectancy than the average population. Physical activity can treat and prevent several diseases, e.g. cardiovascular and metabolic disorders as well as psychiatric symptoms. It is therefore of utmost importance to develop effective methods to integrate physical activity into psychiatric care. To meet this need, the physical activity intervention Braining was developed. This study aims to describe Braining, to assess the number of patients reached during the first years of pilot testing, to analyze clinical data in the group of patients participating in Braining 2017–2020 and to assess the intervention.
Methods
In this descriptive retrospective study we analyzed data from all patients participating in Braining training sessions ≥ 3 times (n = 239), the Braining Participants. Regular patients at the clinic served as a comparison. Furthermore, medical records were studied for a smaller cohort (n = 51), the Braining Pilot Cohort. Data was analyzed using Chi-square and Fisher’s tests.
Results
During the introduction period of Braining, 580 patients attended an information meeting about Braining, or at least one training session. 239 patients participated in ≥ 3 training sessions, considered to be participants of Braining. These Braining Participants (n = 239), ages 19 to 82, males 23.4%, attended between 3 and 308 training sessions (median 9). The main diagnoses were affective and anxiety disorders. Number of diagnoses ranged from 0 to 10 (median = 2). For the subsample, the Braining Pilot Cohort (n = 51), participants attended between 3 and 208 training sessions (median = 20). Twelve percent were working full-time, and symptom severity of depression and general anxiety was moderate. Two thirds had ≥ 3 different classes of medication. Regarding metabolic morbidity, 28% had been diagnosed with hypertension, though blood lipids, blood glucose as well as blood pressure were within the normal range. Thirty-seven percent were prescribed Physical Activity on Prescription during 2017–2020. One severe adverse event was reported.
Conclusions
The Braining intervention reached all age-groups and patients with a wide and representative diagnostic panorama, suggesting that Braining could be a promising and safe method for implementing physical activity in a psychiatric patient population.
Similar content being viewed by others
Background
Mental illness in general is one of the leading causes of disability globally [1, 2]. Affective disorders and anxiety disorders cause major suffering and high societal costs and are common challenges in Psychiatric care [1, 2]. Individuals with depression and anxiety disorders are less physically active than average [3,4,5]. In depression both psychological and pharmacological treatments are recommended [6, 7]. In anxiety disorders psychological treatment is considered first-line treatment, but pharmacological treatment is also recommended [7, 8]. About 50% of those treated with cognitive behavioral therapy (CBT) for anxiety or depression recover and many others show significant clinical improvement [9]. However, access to psychological treatment is limited, mainly due to lack of resources and expertise [10,11,12]. Access to pharmacological treatment with antidepressant medication such as selective serotonin reuptake inhibitors (SSRIs) is sufficient in many countries; however, compliance over time is poor and these medications have well-known side effects [13]. About a third of patients do not respond to SSRIs or CBT and it usually takes weeks before response to treatment occurs [14, 15]. Therefore, in specialized psychiatric care, patients are often prescribed multiple psychopharmaceuticals [16, 17]. Of these, many have a metabolic side effect profile which contributes to impaired somatic health [18,19,20,21].
Physical activity is defined by the World Health Organization (WHO) as any bodily movement produced by skeletal muscles that requires energy expenditure is effective as prevention and treatment in many of the most prevalent somatic non-communicable diseases such as cardiovascular disease, various cancers, type 2 diabetes, osteoporosis, and obesity [19]. Physical exercise can be defined as a subset of physical activity that is planned, structured, and repetitive with the objective to improve or maintain physical fitness [22] and onwards, physical exercise will be defined by its specific attributes when described. The most physically inactive, including psychiatric patients as an important risk group, have a risk-reducing effect with only a minor increase of physical activity dosage [21]. A prospective cohort study shows that 15 min of daily moderate intensive aerobic physical activity could extend life expectancy by three years [23]. Additionally, physical activity has very few side effects.
The WHO’s general recommendation for physical activity for adults are also applicable for patients with depression [19]. Additionally, for mild to moderate depression there is growing evidence for effects of physical activity [24]. Studies show a comparable reduction in depressive symptoms to treatment with antidepressants or psychotherapy [25,26,27,28,29,30,31]. Physical exercise is not only effective as treatment of mild to moderate depression. In moderate to severe depression there are clinical as well as molecular studies, indicating that physical exercise as add- on to pharmacological treatment could have a positive synergistic effect [26, 32]. However, there is still a lack of studies regarding physical exercise and physical activity of clinically well characterized psychiatric patients compared to the load of research done on CBT and SSRIs for instance. Furthermore, the risk of developing or relapsing into depression, as well as developing anxiety symptoms or disorders is reduced by regular physical activity as well as reduced time spent sedentary [31, 33,34,35].
Despite the growing evidence of the effects of physical activity on psychiatric symptoms, it remains to define what the specific mode, intensity and duration should be for optimal effect [36]. Some studies have shown no differences in effect on depression between aerobic and strength training or between exercise conducted at different intensities [25, 37]. Other studies have shown greater effects of aerobic training performed at moderate to high intensity level compared to low intensity activities [27, 31, 38].
Physical activity has shown an anxiety reducing effect both acutely and long-term [39, 40]. Though the research available is limited, physical activity is recommended as an add-on treatment [41]. In several studies [41,42,43], occasional exercise sessions of vigorous intensity could reduce the risk of panic attacks in patients with panic disorder. In accordance with those findings, patients with generalized anxiety disorder experienced an improvement in anxiety symptoms and feelings of energy directly after vigorous intensity exercise [18, 41, 44]. Regular physical activity can reduce symptoms in people with anxiety symptoms or anxiety disorders [18, 24, 45]. Physical activity has anxiety-reducing effects and better long-term effects than placebo, but significantly less effects than CBT or pharmacological treatment [45, 46]. Regarding bipolar disorder, there are few RCTs investigating physical exercise as part of lifestyle interventions. However, the main outcome in these studies have been metabolic changes, rather than mental health improvement [47,48,49].
Despite the clear positive effects of physical activity on symptoms and somatic side-effects in psychiatric patients, it is not yet implemented in the normal treatment range in psychiatric care [4, 25, 50, 51]. Physical Activity on Prescription has been scientifically studied [52] and is considered implemented as a method for promoting physical activity for patients in Sweden. This has led to an ongoing project cofounded by the European Union aiming to spread Physical Activity on Prescription in several countries in Europe [53]. A recent report from the National Board of Health and Welfare notes 5–10 Physical Activity Prescription/1000 patients visits per year in primary care in Sweden [54], but there is a lack of studies on Physical Activity on Prescription in psychiatric care as well as for patients in primary care with psychiatric disorders.
Due to the clear health benefits of being physically active, there is a need to develop a structured physical activity method that can be implemented and integrated into everyday psychiatric care. Therefore, in 2017, we developed Braining, a structured clinical intervention to support patients to initiate and execute moderate to vigorous physical activity, at a large psychiatric clinic in Region Stockholm. This study aims to retrospectively describe the method, the participating patients, and their participation in training sessions during the first four years.
Methods
Aims
This study aims to describe the method Braining, to assess the number of patients reached by the intervention during the first years of implementation, to analyze clinical data in the group of patients participating in Braining during the initial years 2017–2020 regarding medical and demographic variables, and to assess the intervention in terms of participation in training sessions, as well as any adverse events.
Participants and setting
Patients at two outpatient units (the Affective Outpatient Unit, and the Affective, Anxiety, and Trauma Outpatient Unit, n≈2 100 patients) at a large psychiatric clinic (n≈11 000 patients) in Region Stockholm, Psychiatry Southwest were the main target group for Braining during the study period 2017–2020. The patients at these units were predominantly patients with bipolar disorders, depression, anxiety disorders and post-traumatic stress disorder (PTSD). To a minor extent, patients from other units with depression, anxiety, sleep disturbance or stress as sub-symptoms of other psychiatric disorders, were also allowed to participate. Patients were mainly participating when in outpatient care but could also participate while subjected to inpatient care.
During 2017–2020, 580 patients participated in Braining on any occasion of which 566 were available to be contacted and were included in the study. Of these, the 239 patients that participated in three or more training sessions were invited to participate in long-term follow-up including a medical record review. Onward in this text, this group of 239 patients are called the Braining Participants. 51 patients that met the inclusion criteria and not the exclusion criteria agreed to participate, namely the Braining Pilot Cohort.
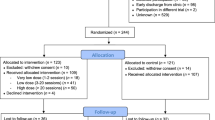
Inclusion criteria: all participants with three or more training sessions in total. Exclusion criteria: participants deceased at time for inclusion (n = 13), lacking baseline data (n = 0), difficulty speaking or understanding the Swedish language (n = 3), cared for in accordance with the Compulsory Mental Care Act (Lagen om psykiatrisk tvångsvård) (n = 1) at the time of inclusion. Difficulty speaking or understanding the Swedish language was defined as needing translator services to communicate with staff. Also excluded were participants having an invalid social security number, protected identity, invitation letter in return to sender/moved, incomplete or belated form of consent or unknown (n = 8) (Fig. 1).
Design and procedure
The study is a retrospective, descriptive cohort study. Data were retrieved from available medical records, as well as from the central register at the Health Care Services Stockholm County (Stockholms Läns Sjukvårdsområde). Patients who fulfilled the inclusion criteria (n = 239) were sent written information about the study along with a written consent form. Those who did not respond in writing, were reminded by follow-up letters at up to two times. They had the opportunity to ask questions via a telephone contact number. Out of these, 51 patients did not meet the exclusion criteria, agreed, and were included in the cohort planned for long-term follow-up and medical record review (Fig. 1).
For all participants in Braining, data was collected on an individual level from the central register at the Health Care Services Stockholm County (Stockholms Läns Sjukvårdsområde). In attempt to visualize representativity, the patient group enrolled at the two outpatient units (the Affective Outpatient Unit, and the Affective, Anxiety, and Trauma Outpatient Unit) was used as reference group and data was only available on a group level.
The same information was obtained, on the same central register level for the Braining Pilot Cohort (n = 51) with written consent to medical record review and long-term follow-up.
The Braining method
Since 2017, patients at Psychiatry Southwest in Region Stockholm, have been offered Braining, in order to initiate, support and execute physical exercise regularly. This novel method per se has not yet been validated, though it aims to follow the recommendations for physical activity from the WHO [19] when it comes to intensity, duration and recommended frequency. Braining is a structured clinical intervention, with core components of repeated 30–45 min moderate to vigorous intensity group physical exercise sessions. The Braining physical exercise sessions consist of a 5 to 7 min long warm up followed by 20 to 30 min of interval based aerobic movements e.g., jogging or jumping jacks as well as body weight strength exercises e.g., squats and pushups. The sessions end with a short cool down with mobility or balance focus. The sessions are supervised by two trained members of the psychiatric staff, one instructor and one host. The instructor is teaching the session and thereby showing correct technique and intensity. The host supports the participants and gives them individual adjustments during the class. To ensure quality and consistency, the instructor and host use the Braining Box, a physical and digital tool with photos, written instructions and filmed exercises as well as complete classes, developed by physiotherapists, psychiatrists and employees at the clinic. The material in the Braining Box is publicly available [55]. The Braining instructors use the Borgs scale of rated perception of exertion [56] to mediate eligible intensity level between 11 and 17. Whenever participants appear to exceed 17 or perform under the limit of 11, the Braining leader will encourage them to adapt. Since this was a clinical project, the intensity was not controlled for with any other tools at this stage. Physical exercise is accompanied by continuous short follow-ups and support to promote compliance, all led by educated and licensed psychiatric staff. Before and after the intervention period, measurements and evaluations are performed. Physical exercise is added to treatment as usual, included in the patient care plan, and covered by the regular healthcare fee. Each physical exercise session is preceded by a short individual visit with staff for a brief assessment of mental and physical status and for motivational support.
The goal for participation when introducing Braining is three physical exercise sessions/week during a three-month period, but patients participate voluntarily. Each participation in the structured program begins and ends with a motivational and educational visit, provided in a group seminar and/or an individual visit. In conjunction with this, participants are also offered a mental and physical examination, assessment scales on symptoms and quality of life, and the ability to submit blood samples. The main target group during the study period was patients with predominantly affective disorders or anxiety disorders in outpatient care, but patients with other diagnoses or inpatient care were also allowed to participate.
Variables
The burden of disease and level of function was measured regarding psychiatric diagnoses, medical use, psychiatric care visits, and occupational status. For all patients, namely the reference group (n = 2 144), the Braining Participants (n = 239), and the Braining Pilot Cohort (n = 51), data was collected regarding age, gender, and psychiatric diagnoses. For the reference group, data was only available on a group level.
Braining participants
The patients participating in three or more training sessions (n = 239) in 2017–2020 are described in terms of age, gender, ICD-10 (International Classification of Diseases) psychiatric diagnoses, number of training sessions, and number of contacts with psychiatric health care in outpatient units, emergency units and inpatient care. Data on training sessions was accessible through the Swedish Classification System of Care measures (Klassifikation av vårdåtgärder), where every group training session was coded with a specific Braining group session code (QV011). This data could not be related to individuals and was obtained for the different subgroups separately, to enable statistical analyses.
Information about the patient group enrolled in total (n = 2 144) at the two outpatient units, used as reference group, were available on a general level, which was also used for comparison with the group that were reached by the structured intervention Braining.
Braining pilot cohort
For the Braining Pilot Cohort (n = 51) more detailed data was available and extracted from medical records, in addition to description of age, gender, number of training sessions, and number of contacts with psychiatric health care in outpatient units, emergency units and inpatient care, as for the Braining Participants.
Additional data included psychiatric and somatic diagnoses, level of function in terms of degree of sick leave/occupational status, symptom level based on self-assessment scales for symptoms of depression in terms of PHQ-9 [57] and anxiety in terms of GAD-7 [58], self-assessed health-related quality of life in terms of EQ-5D-5L/EQ-5D-3L [59], clinician assessed severity of psychopathology in terms of CGI-S [60, 61] as well as psychopharmaceutical treatment classified by ATC (Anatomical Therapeutic Chemical Classification System) code, blood pressure, molecular parameters (blood lipids, blood glucose).
PHQ-9 (9-item Patient Health Questionnaire-9) is a questionnaire designed to screen for depression in medical settings. Its sensitivity to detect major depressive disorder has been thoroughly tested and has yielded good results. The total score ranges from 0 to 27 and the standard cut-off score to detect possible major depression is 10 or above. 10–14 constitutes a diagnostic grey area and 15–27 indicates the existence of major depressive disorder [57].
GAD-7 (7-item Generalized Anxiety Disorder Questionnaire) is one of the most frequently used measures for anxiety, because of its validity and diagnostic reliability. It has been deemed sensitive to detect changes in anxiety severity over the course of treatment, with a minimal clinically important difference equal to 4. The seven items of the questionnaire describe the seven core symptoms for generalized anxiety disorder and asks how often participants have experienced these symptoms within the last two weeks. Each item is scored as 0–3 with 0 translating to not at all and 3 to almost every day. The total score ranges from 0 to 21, with 5 constituting the threshold value for mild anxiety, 10 for moderate and 15 for severe anxiety [58].
CGI (Clinical Global Impression Scale) [62] is a widely used tool in psychiatric clinical practice designed to rate the patient’s severity of symptoms (CGI-S), improvement (CGI-I), and the effectiveness of a specific treatment (CGI-E) [60]. The present study used the CGI-S, severity of symptoms measure. Several studies evaluating the reliability and validity of CGI have been published, also with adjustments to bipolar disorders [63] but results are mixed, and no established psychometric properties exists. Promising studies has shown sensitivity to change, significant correlations to other clinical routine outcome measures, and satisfactory interrater reliability [63, 64].
EQ-5D-5L is a well-known, reliable and valid instrument measure of an individual’s health-related quality of life. It has also been deemed relatively responsive to changes in health status. The questionnaire consists of five dimensions; mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Each dimension has five response categories ranging from no problems to severe/extreme problems, which creates a total of 3125 unique health states. This generates an index value of -0,285 to 1,00, where 1,00 constitutes perfect health, 0 is a state equal to death and negative values constitute a state worse than death. The measure is administered jointly with a visual analogue scale (VAS), where participants rate their current health state on a scale of 1 to 100. EQ-5D-3L is the preceding version of the instrument, used clinically during the first part of the present study period, thus exchanged clinically along the way when the instrument was updated [59].
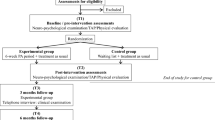
Time measurement points
The time measurement points used were defined in relation to the first occasion the patient took part in a training session within the Braining intervention. Due to the naturalistic setting, and the retrospective design, minor adjustments were made in order not to lose data that for example were dated a week outside the originally planned measurement point. Therefore, an additional 2 weeks were added to the time frames for diagnoses, molecular parameters, blood pressure and assessment scales (Fig. 2).
Method assessment
The participation in Braining in terms of number of training sessions is described for both groups, as well as any adverse events.
Statistical analysis
Descriptive statistics
All variables were summarized and tabulated for the three separate groups Reference group, Braining Participants, and Braining Pilot Cohort, respectively. Categorical variables were described with frequencies (n) and percentages (%). Continuous variables were described with medians or means, and standard deviations.
The background variables describing the Reference group included: age, gender and psychiatric diagnoses. For the group Braining Participants, additional variables were available: number of contacts with psychiatric health care in outpatient units, emergency units and inpatient care, and number of training sessions. Finally, for the Braining Pilot Cohort, further additional variables were available: both psychiatric and somatic diagnoses, level of function in terms of degree of sick leave/occupational status, symptom level based on self-assessment scales for symptoms of depression and anxiety, self-assessed health-related quality of life, clinician assessed severity of psychopathology as well as psychopharmaceutical treatment classified by ATC (Anatomical Therapeutic Chemical Classification System) code, blood pressure and molecular parameters.
Description of the different groups were presented with tabulation of diagnostic spectra. In addition, number of diagnoses and number of medications were presented graphically with bar plots.
The feasibility of the Braining intervention was evaluated with description of the different groups and observation of the actual participation of patients in training sessions. Participation was partly visualized in a bar plot for Braining Participants to show frequency distribution, see Fig. 1. Additionally, number of training sessions were tabulated for Braining Participants and Braining Pilot Cohort.
Comparison between groups
The variables of diagnostic spectra, number of training sessions, outpatient visits, emergency visits and inpatient care were summarized and tabulated for Braining Participants and Braining Pilot Cohort to enable comparison.
Specific data on similarities and differences between groups could inform on the ability of the Braining intervention to reach out to different patient groups, and also inform on research questions for further studies. Notably, the clinical nature of study design does limit the conclusion possible to make from observed differences and similarities between groups.
Significant statistical differences between groups
Significant testing of group differences between Braining Participants and Braining Pilot Cohort was performed for the variables of gender and age. Differences between groups on variable of gender was evaluated with Chi-squared tests. Single cells in the categorical variable of age groups included less than five subjects so data did not meet the assumptions of Chi-squared test. Instead, Fisher’s exact test was chosen to evaluate differences in age distribution.
All data analysis was conducted using R [65], the tidyverse package [66] version 1.2.0 and the tableone package [67] version 0.13.2.
Results
In a naturalistic, clinical setting at two outpatient units during the first phase of implementation, 580 patients attended an information meeting about Braining, or at least one training session, during the first four years. 239 patients participated in ≥ 3 training sessions, here called the Braining Participants. In 2021, these were invited in writing to participate in the Braining retrospective study, 55 patients accepted and gave informed consent. Out of these 51 did not meet the exclusion criteria and could be included in the planned cohort, here called the Braining Pilot Cohort (Fig. 1).
Braining participants
Among the Braining Participants (n = 239), ages ranged from 19 to 82. There was a significant difference in age composition; 8.4% were in the age group 20–30 compared to 18.3% in the reference group. There was also a significant difference regarding gender, where 23.4% were male compared to 32.7% in the reference group. The main diagnoses in the reference group were represented, namely depression, bipolar disorders, anxiety disorders, PTSD, attention deficit hyperkinetic disorder (ADHD) and autism. Number of diagnoses ranged from 0 to 10 (median = 2) (Tables 1 and 2 and Fig. 3).
Number of psychiatric diagnoses among Braining Participants. Distribution of number of diagnoses per participant. We noted that 30 participants (12.6%) did not have a diagnose in the data material. An additional 22 participants (9.2%) only had a diagnose for examination or observation (ICD-10 codes Z00.4 and Z03.2). Note that listed diagnoses above show the total number of diagnoses and does not represent individual patients
The amount of individual training sessions varied from 3 to 308 (median = 9) for the most active participant. 13 participants exercised more than 60 times, 5 exercised more than 150 times (median = 9). In total, this rendered 5235 training session visits (Table 3 and Fig. 4).
The number of outpatient visits (physical, video and telephone), training sessions excluded, varied from 0 to 313 (median = 53). In total this rendered 14,960 outpatient visits. The number of emergency visits varied from 0 up to 66 (median = 2). The number of hospitalizations ranged from 0 up to 27 (median = 1) (Table 3).
Braining pilot cohort
Data from medical records were available for the Braining Pilot Cohort (n = 51). Ages ranged from 21 to 75. The main diagnoses in the reference group were represented in this group as well (depression, bipolar disorder, autism, ADHD, PTSD, general anxiety disorder, panic syndrome, social phobia, and obsessive–compulsive disorder) (Table 2).
The amount of training sessions varied from 3 up to 208 for the most active participant (median = 20). In total, this rendered 1 766 individual training session visits (Table 3 and Fig. 4). The number of outpatient visits (physical, video and telephone), training sessions excluded, varied from 0 to 313 (median = 45). The number of emergency visits varied from 0 up to 66 (median = 2). In total this rendered 2 913 outpatient visits. The number of hospitalizations ranged from 0 up to 27 (median = 1) (Table 3). Data concerning training sessions and health care contacts includes 4 additional participants that were later excluded during medical record review (Fig. 1). Out of the group, 37.3% were prescribed Physical activity on Prescription (Table 4).
On a group level, depression, and general anxiety symptom severity (PHQ-9, GAD-7) were moderate. Clinician assessed evaluation measure of severity of psychopathology (CGI-S) was mild to moderate. Data on occupational status showed that 11.8% were working full-time, 62.7% were on full- or part-time sick-leave, and 19.6% were retired. Regarding somatic morbidity, 27.5% had been diagnosed with hypertension, and 35.3% with a pain condition. Blood lipids, blood glucose as well as blood pressure were within the normal range (Table 4).
Two thirds had ≥ 3 different classes of medication (Fig. 5). 64.7% of the patients had treatment with antidepressants, 50% with antipsychotics, 27.5% with lithium, 25.5% with antiepileptics, 33.3% with antihistamines. 21.6% were treated with benzodiazepines, 43.1% with benzodiazepine-related sleep medications and 8% were treated with opioids (Table 4).
Between 2017 and 2020, two adverse events were reported. First, one patient with a previously known somatic condition had a serious event during a training session. Second, an administrative difficulty to register an inpatient for a training session, resulted in the patient leaving the premises without permission, and later returning safely to the ward. The former was classified as a serious adverse event.
Discussion
This is the first study to describe the method Braining, a structured clinical intervention led by trained psychiatric staff, with core components of 30–45 min of moderate to vigorous intensity group physical exercise sessions accompanied by continuous short follow-ups and support to promote compliance.
The main finding in the present study was that the intervention Braining, was able to introduce physical exercise to a large group of psychiatric patients in a psychiatric outpatient setting. The population was patients in need of psychiatric outpatient care, with a variety of symptom severity and a few severely ill inpatients. The core components of the method offered 5235 training session visits as add on to their on-going treatment as usual, suggesting that patients were offered closer contact to the clinic during this period of their care compared to before Braining was introduced. Another important finding was that Braining could be implemented in ordinary psychiatric care without adding external resources. Moreover, during the observed time frame, very few adverse events were reported, suggesting an adequate level of safety.
Additionally, Braining is a new and integrated clinical method that might be more accessible to clinics with limited resources. The Braining intervention, executed on the premises of the clinic and with psychiatric staff as participating supervisors, has similarities as well as unique features compared to other physical exercise interventions in previously published studies. The main focus of aerobic physical exercise, aiming to reach the WHO guidelines [19] is in line with a majority of studies [68, 69]. Previous studies of physical exercise interventions have had both supervised and unsupervised physical exercise sessions. However, in those studies, mainly external physical exercise specialists such as physiotherapists and trainers [68] supervised the sessions. Therefore, this type of method might serve in situations with limited resources. Furthermore, since psychiatric staff take an active part in the treatment, there are possible occupational health benefits, which would be in line with previous studies on physical activity among health care staff [70], and could possibly improve caregiver and patient relationship.
Moreover, an important finding was the burden of disease and ongoing advanced treatment in the patients participating in Braining during the study period, indicating that the method reached a group who benefits the most from physical exercise. Almost one third of the participants had a hypertension diagnosis, but on a group level, blood pressure was registered during the intervention period within the normal range. During medical record review, we noticed that 6 out of 51 individuals had an elevated blood pressure, defined as a single measured value of ≥ 140/90 mmHg. This could be comprehended as well-treated blood pressure in this population.
Only 10% of the group were working full-time, and the amount of regular outpatient visits, emergency visits and in-patient care during the studied period was considerable. Two thirds of the group had ≥ 3 different classes of psychopharmacological medications. Altogether, this could indicate that the burden of disease in the group was substantial. However, the symptom level based on self-assessment scales on a group level was moderate. A possible explanation could be that Braining probably was introduced more often when patients were past the most acute phase symptom wise. The fact that training sessions were scheduled during daytime, could also have favored patients without full-time occupation.
As expected in this clinical population, participation frequency varied greatly. Some patients participated actively over several years, accumulating hundreds of physical exercise sessions, while others participated in a limited number of sessions. For this reason, with the present study design it is impossible to draw conclusions concerning the amount of Braining physical exercise sessions that the fully implemented Braining method might lead to. In a large-scale Swedish RCT comparing physical exercise with treatment as usual for depression, 31.7% attended no exercise sessions at all and 39.6% attended 12 or more sessions during the 12-week intervention period [37]. This indicates a large variation in participation/execution in this type of physical exercise intervention. Another study using running as add-on treatment for patients with severe depression in psychiatry reported a decline rate of 40% among eligible patients due to lack of interest or time and a drop-out of 55% at 6 months in included participants [71], altogether indicating that studies in this population are challenging to conduct.
From March and onwards during 2020, the Covid-19 pandemic greatly affected the healthcare system. Psychiatry Southwest continued to offer Braining as outdoor group training sessions, while most group therapy sessions and many physical visits were cancelled in psychiatric care in Sweden and even more so in other countries. This was not at focus in the present study, but as expected, the clinical impression was that the participating rate was lower during 2020 than in 2017–2019, mainly due to pandemic restrictions.
Another important finding of this study was the low number of adverse events, with only two such events reported during the first four years. A review and meta-analysis of exercise intervention studies concluded that the risk of serious adverse events was not elevated, but that the relative risk of minor adverse events was increased [72]. As in this retrospective study, adverse events were often not defined prior to the study and the ways of reporting minor adverse event were not clearly defined. However, in the long run, the positive health aspects from physical activity outnumber the eventual minor health risks [18, 19].
Another interesting finding was that that 37,3% of the Braining Pilot Cohort were prescribed Physical Activity on Prescription. Compared to the rest of the clinic Psychiatry Southwest, and even more so compared to primary care patients in Sweden [54], this is a substantial proportion. The result indicates that the implementation of Braining might lead to raised awareness regarding the importance of physical activity in the clinic. Studies investigating the implementation of Physical Activity on Prescription in psychiatry are scarce. A survey among forensic psychiatry staff in Sweden indicates that 50% of staff use Physical Activity on Prescription at least occasionally [73].
Strengths and limitations
The prerequisites for this observational study led to several limitations affecting the outcome of data analyses. At the outset, no plans were made in preparation for a research project. However, since the participation rate during the first years was unexpectedly high, in addition to clinical observations regarding participant morbidity, a decision was made to conduct a retrospective study. As a result of this naturalistic setting, clinical data collection was incomplete. A participant could, for example, have participated in sessions prior to submitting start-up evaluations and measurements, which the set time variable did not cover. Furthermore, training sessions, submission of blood samples and other measurements were not mandatory. Regarding results of diagnoses in the reference group, there was a certain overlap in data, meaning that one patient could contribute with several data points in the same diagnosis group. For this reason, data in Table 1 is presented with a larger margin of error. Yet another limitation that affected evaluation of the implementation was our definition of patient participation as number of registered sessions in patient medical records. In other words, there were no objective measurements nor self-report inventories to ensure that participants attained the intended level of exertion during the sessions. At the same time, the naturalistic setting offers a well-needed perspective on the challenges of intervention implementation in a clinical setting with a substantial rate of high morbidity. This study could therefore provide a foundation for study design and hypothesis generating of upcoming research projects.
Future studies
In order to evaluate the effects on patients´ mental and physical health as well as the method´s feasibility in a clinical setting, additional studies are needed. Some are already planned, such as long-term follow-up interviews with the clinical Braining Pilot Cohort (n = 51). The main focus will be patients´ experience of Braining, as well as long-term effects of participation. Additionally, we will enquire about minor adverse events that were not previously reported. Controlled feasibility studies that measure change in physical exercise (Braining sessions as well as other forms of physical exercise) are necessary, preferably using both objective measures such as accelerometer and validated questionnaires. A pilot study followed by a multicenter RCT studying the effects on patients, the implementation process and the experience end possible health effects on the participating staff are planned in this manner. In order to explore the compliance, effect, implementation, and patient experience of Physical Activity on Prescription in psychiatry, further studies on Physical Activity on Prescription in psychiatric care are needed.
Conclusions
This retrospective study shows that a new structured physical exercise intervention called Braining has reached patients in all age-groups and with a wide and representative diagnostic panorama, indicating that Braining might be a promising and safe method to implement physical activity in a psychiatric setting. We suggest that the method is evaluated in future clinical trials, in regards of feasibility, effects, cost effectiveness and experiences from patients and personnel.
Availability of data and materials
The datasets generated and analyzed during the current study are not publicly available due to individual privacy even though pseudonymized but are available from the corresponding author on reasonable request.
Change history
03 May 2024
A Correction to this paper has been published: https://doi.org/10.1186/s12888-024-05775-3
Abbreviations
- ATC:
-
Anatomical Therapeutic Chemical Classification System
- ADHD:
-
Attention Deficit Hyperactivity Disorder
- CBT:
-
Cognitive behavioral therapy
- EQ5D-3L, EQ5D-5L:
-
EQ5D™ is a trademark of the EuroQol Group, a self-assessment instrument for describing and valuing health status
- GAD-7:
-
Generalized Anxiety Disorder 7 Items
- ICD-10:
-
International Classification of Diseases and Related Health Problems, 10th Revision
- PHQ-9:
-
Patient Health Questionnaire9 Items
- PTSD:
-
Post-traumatic stress disorder
- RCT:
-
Randomized Controlled Trial
- SSRI:
-
Selective serotonin reuptake inhibitors
- WHO:
-
World Health Organization
References
GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9(2):137–50.
Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382(9904):1575–86.
Schuch F, Vancampfort D, Firth J, Rosenbaum S, Ward P, Reichert T, et al. Physical activity and sedentary behavior in people with major depressive disorder: a systematic review and meta-analysis. J Affect Disord. 2017;210:139–50.
Helgadóttir B, Forsell Y, Ekblom Ö. Physical activity patterns of people affected by depressive and anxiety disorders as measured by accelerometers: a cross-sectional study. PLoS ONE. 2015;10(1): e0115894.
Goodwin RD. Association between physical activity and mental disorders among adults in the United States. Prev Med. 2003;36(6):698–703.
National Institute for Health and Care Excellence: Guidelines. Depression in adults: treatment and management. London: National Institute for Health and Care Excellence (NICE). Copyright © NICE 2022; 2022.
Nationella riktlinjer för vård vid depression och ångestsyndrom : stöd för styrning och ledning. Stockholm: Socialstyrelsen; 2021.
National Institute for Health and Care Excellence: Guidelines. Generalised anxiety disorder and panic disorder in adults: management. London: National Institute for Health and Care Excellence (NICE). Copyright © NICE 2020; 2019.
Hofmann SG, Asnaani A, Vonk IJ, Sawyer AT, Fang A. The efficacy of cognitive behavioral therapy: a review of meta-analyses. Cognit Ther Res. 2012;36(5):427–40.
Shafran R, Clark DM, Fairburn CG, Arntz A, Barlow DH, Ehlers A, et al. Mind the gap: Improving the dissemination of CBT. Behav Res Ther. 2009;47(11):902–9.
Layard R, Clark DM. Why more psychological therapy would cost nothing. Front Psychol. 2015;6:1713.
Wolitzky-Taylor K, Zimmermann M, Arch JJ, De Guzman E, Lagomasino I. Has evidence-based psychosocial treatment for anxiety disorders permeated usual care in community mental health settings? Behav Res Ther. 2015;72:9–17.
David DJ, Gourion D. Antidepressant and tolerance: Determinants and management of major side effects. Encephale. 2016;42(6):553–61.
Driessen E, Hollon SD. Cognitive behavioral therapy for mood disorders: efficacy, moderators and mediators. Psychiatr Clin North Am. 2010;33(3):537–55.
Al-Harbi KS. Treatment-resistant depression: therapeutic trends, challenges, and future directions. Patient Prefer Adherence. 2012;6:369–88.
Amerio A, Russo D, Miletto N, Aguglia A, Costanza A, Benatti B, et al. Polypharmacy as maintenance treatment in bipolar illness: a systematic review. Acta Psychiatr Scand. 2021;144(3):259–76.
Baandrup L. Polypharmacy in schizophrenia. Basic Clin Pharmacol Toxicol. 2020;126(3):183–92.
Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Washington, DC: U.S. Department of Health and Human Services; 2018. p. 2018.
Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–62.
Abosi O, Lopes S, Schmitz S, Fiedorowicz JG. Cardiometabolic effects of psychotropic medications. Horm Mol Biol Clin Investig. 2018;36(1):0065.
Ekelund U, Tarp J, Steene-Johannessen J, Hansen BH, Jefferis B, Fagerland MW, et al. Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: systematic review and harmonised meta-analysis. BMJ. 2019;366: l4570.
Caspersen Cj Fau - Powell KE, Powell Ke Fau - Christenson GM, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. 1985;(0033–3549 (Print).
Wen CP, Wai JP, Tsai MK, Yang YC, Cheng TY, Lee MC, et al. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet. 2011;378(9798):1244–53.
Singh B, Olds T, Curtis R, Dumuid D, Virgara R, Watson A, et al. Effectiveness of physical activity interventions for improving depression, anxiety and distress: an overview of systematic reviews. Br J Sports Med. 2023;bjsports-2022:106195.
Cooney GM, Dwan K, Greig CA, Lawlor DA, Rimer J, Waugh FR, et al. Exercise for depression. Cochrane Database Syst Rev. 2013;9:CD004366.
Kvam S, Kleppe CL, Nordhus IH, Hovland A. Exercise as a treatment for depression: a meta-analysis. J Affect Disord. 2016;202:67–86.
Stubbs B, Vancampfort D, Hallgren M, Firth J, Veronese N, Solmi M, et al. EPA guidance on physical activity as a treatment for severe mental illness: a meta-review of the evidence and Position Statement from the European Psychiatric Association (EPA), supported by the International Organization of Physical Therapists in Mental Health (IOPTMH). Eur Psychiatry. 2018;54:124–44.
Bueno-Antequera J, Munguía-Izquierdo D. Exercise and depressive disorder. Adv Exp Med Biol. 2020;1228:271–87.
Kramer A. An overview of the beneficial effects of exercise on health and performance. Adv Exp Med Biol. 2020;1228:3–22.
MdZemberi NFN, Ismail MM, Abdullah MFIL. Exercise interventions as the primary treatment for depression: evidence from a narrative review. Malays J Med Sci. 2020;27(5):5–23.
Andersson E, Hovland A, Taube J, et al. (YFA) Yfa. Fysisk aktivitet i sjukdomsprevention och sjukdomsbehandling (Fyss) [Physical Activity in the Prevention and Treatment of Disease]. 2.9. Fysisk aktivitet vid depression [physical activity for depression]. Stockholm: Läkartidningen Förlag AB; 2021. p. 319–24.
Guerrera CS, Furneri G, Grasso M, Caruso G, Castellano S, Drago F, et al. Antidepressant drugs and physical activity: a possible synergism in the treatment of major depression? Front Psychol. 2020;11:857.
Schuch FB, Vancampfort D, Firth J, Rosenbaum S, Ward PB, Silva ES, et al. Physical activity and incident depression: a meta-analysis of prospective cohort studies. Am J Psychiatry. 2018;175(7):631–48.
Powell KE, King AC, Buchner DM, Campbell WW, DiPietro L, Erickson KI, et al. The Scientific Foundation for the Physical Activity Guidelines for Americans, 2nd Edition. J Phys Act Health. 2018;1–11.
Gianfredi V, Blandi L, Cacitti S, Minelli M, Signorelli C, Amerio A, et al. Depression and objectively measured physical activity: a systematic review and meta-analysis. Int J Environ Res Public Health. 2020;17(10):3738.
Pedersen BK, Saltin B. Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports. 2015;25(Suppl 3):1–72.
Helgadóttir B, Hallgren M, Ekblom Ö, Forsell Y. Training fast or slow? Exercise for depression: a randomized controlled trial. Prev Med. 2016;91:123–31.
Schuch FB, Vancampfort D, Richards J, Rosenbaum S, Ward PB, Stubbs B. Exercise as a treatment for depression: a meta-analysis adjusting for publication bias. J Psychiatr Res. 2016;77:42–51.
Morais NS, Viana RB, Silva WF, Santos DA, Costa TG, Campos MH, et al. Effect of both dance exergame and a traditional exercise on state anxiety and enjoyment in women. J Sports Med Phys Fitness. 2022;62(4):560–7.
Ensari I, Greenlee TA, Motl RW, Petruzzello SJ. Meta-analysis of acute exercise effects on state anxiety: an update of randomized controlled trials over the past 25 years. Depress Anxiety. 2015;32(8):624–34.
Hovland A, Martinsen EW, Kjellman B, et al. (YFA) Yffa. Fysisk aktivitet i sjukdomsprevention och sjukdomsbehandling (Fyss). [Physical Activity in the Prevention and Treatment of Disease] 2.35 Fysisk aktivitet vid ångestsymtom och ångestsyndrom [physical activity for anxiety symptoms and anxiety disorders]. Stockholm: Läkartidningen Förlag AB; 2021. p. 483–9.
Ströhle A, Graetz B, Scheel M, Wittmann A, Feller C, Heinz A, et al. The acute antipanic and anxiolytic activity of aerobic exercise in patients with panic disorder and healthy control subjects. J Psychiatr Res. 2009;43(12):1013–7.
Esquivel G, Díaz-Galvis J, Schruers K, Berlanga C, Lara-Muñoz C, Griez E. Acute exercise reduces the effects of a 35% CO2 challenge in patients with panic disorder. J Affect Disord. 2008;107(1–3):217–20.
Herring MP, Monroe DC, Gordon BR, Hallgren M, Campbell MJ. Acute exercise effects among young adults with analogue generalized anxiety disorder. Med Sci Sports Exerc. 2019;51(5):962–9.
Aylett E, Small N, Bower P. Exercise in the treatment of clinical anxiety in general practice - a systematic review and meta-analysis. BMC Health Serv Res. 2018;18(1):559.
Stubbs B, Vancampfort D, Rosenbaum S, Firth J, Cosco T, Veronese N, et al. An examination of the anxiolytic effects of exercise for people with anxiety and stress-related disorders: a meta-analysis. Psychiatry Res. 2017;249:102–8.
Simjanoski M, Patel S, Boni R, Balanzá-Martínez V, Frey BN, Minuzzi L, et al. Lifestyle interventions for bipolar disorders: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2023;152: 105257.
Frank E, Wallace ML, Hall M, Hasler B, Levenson JC, Janney CA, et al. An Integrated Risk Reduction Intervention can reduce body mass index in individuals being treated for bipolar I disorder: results from a randomized trial. Bipolar Disord. 2015;17(4):424–37.
Gillhoff K, Gaab J, Emini L, Maroni C, Tholuck J, Greil W. Effects of a multimodal lifestyle intervention on body mass index in patients with bipolar disorder: a randomized controlled trial. Prim Care Companion J Clin Psychiatry. 2010;12(5):PCC.09m00906.
Mead GE, Morley W, Campbell P, Greig CA, McMurdo M, Lawlor DA. Exercise for depression. Cochrane Database Syst Rev. 2008;4:CD004366.
Rimer J, Dwan K, Lawlor DA, Greig CA, McMurdo M, Morley W, et al. Exercise for depression. Cochrane Database Syst Rev. 2012;7:CD004366.
Onerup A, Arvidsson D, Blomqvist Å, Daxberg EL, Jivegård L, Jonsdottir IH, et al. Physical activity on prescription in accordance with the Swedish model increases physical activity: a systematic review. Br J Sports Med. 2019;53(6):383–8.
EUPAP. EU physical activity on prescription (Available from: https://www.eupap.org/). Accessed 1 Mar 2023.
Folkhälsomyndigheten[Public Health Agency of Sweden]. FaR i Sverige – En beskrivning av regionernas arbete med metoden Fysisk aktivitet på recept [Elektronisk resurs]. 2022;21232.
Anger Å, Sundelin S, Lithman M, Martinsson L. Brainingboxen (Available from: https://www.braining.nu/brainingboxen). Accessed 15 June 2023.
Borg G. Borg’s perceived exertion and pain scales. 1998.
Levis B, Benedetti A, Thombs BD. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ. 2019;365: l1476.
Toussaint A, Hüsing P, Gumz A, Wingenfeld K, Härter M, Schramm E, et al. Sensitivity to change and minimal clinically important difference of the 7-item Generalized Anxiety Disorder Questionnaire (GAD-7). J Affect Disord. 2020;265:395–401.
Payakachat N, Ali MM, Tilford JM. Can the EQ-5D detect meaningful change? A systematic review. Pharmacoeconomics. 2015;33(11):1137–54.
Busner J, Targum SD. The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry (Edgmont). 2007;4(7):28–37.
Leon AC, Shear MK, Klerman GL, Portera L, Rosenbaum JF, Goldenberg I. A comparison of symptom determinants of patient and clinician global ratings in patients with panic disorder and depression. J Clin Psychopharmacol. 1993;13(5):327–31.
Guy W, National Institute of Mental Health . Psychopharmacology Research B, Early Clinical Drug Evaluation P. ECDEU assessment manual for psychopharmacology. Rev ed. Rockville: U.S. Dept. of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute of Mental Health, Psychopharmacology Research Branch, Division of Extramural Research Programs; 1976.
Spearing MK, Post RM, Leverich GS, Brandt D, Nolen W. Modification of the Clinical Global Impressions (CGI) Scale for use in bipolar illness (BP): the CGI-BP. Psychiatry Res. 1997;73(3):159–71.
Berk M, Ng F, Dodd S, Callaly T, Campbell S, Bernardo M, et al. The validity of the CGI severity and improvement scales as measures of clinical effectiveness suitable for routine clinical use. J Eval Clin Pract. 2008;14(6):979–83.
Team RC. R: A language and environment for statistical computing. Vienna, Austria.: R Foundation for Statistical Computing; 2022.
Hadley Wickham MA, Jennifer Bryan, Winston Chang, Lucy D’Agostino McGowan RF, Garrett Grolemund, Alex Hayes LH, et al. Welcome to the Tidyverse. J Open Source Softw. 2019;4(43):1686.
Yoshida K. BA. tableone: Create “Table 1” to Describe Baseline Characteristics with or without Propensity Score Weights. version 0.13.2, R Studio package. ed. Vienna: RStudio, Inc.; 2022.
Falkai P, Schmitt A, Rosenbeiger CP, Maurus I, Hattenkofer L, Hasan A, et al. Aerobic exercise in severe mental illness: requirements from the perspective of sports medicine. Eur Arch Psychiatry Clin Neurosci. 2022;272(4):643–77.
Heissel A, Heinen D, Brokmeier LL, Skarabis N, Kangas M, Vancampfort D, et al. Exercise as medicine for depressive symptoms? A systematic review and meta-analysis with meta-regression. Br J Sports Med. 2023;57(16):1049–57.
Naczenski LM, Vries JD, Hooff M, Kompier MAJ. Systematic review of the association between physical activity and burnout. J Occup Health. 2017;59(6):477–94.
Kruisdijk F, Hopman-Rock M, Beekman ATF, Hendriksen I. EFFORT-D: results of a randomised controlled trial testing the EFFect of running therapy on depression. BMC Psychiatry. 2019;19(1):170.
Niemeijer A, Lund H, Stafne SN, Ipsen T, Goldschmidt CL, Jørgensen CT, et al. Adverse events of exercise therapy in randomised controlled trials: a systematic review and meta-analysis. Br J Sports Med. 2020;54(18):1073–80.
Bergman H, Nilsson T, Andiné P, Degl'Innocenti A, Thomeé R, Gutke A. The use of physical exercise in forensic psychiatric care in Sweden: a nationwide survey. J Ment Health. 2021;1–9.
Acknowledgements
The authors are very grateful to the participating patients, staff, and Braining Team at Psychiatry Southwest. We would like to thank Beata Nilsson for providing excellent support during data retrieval, Anifa Ameti for assisting in the recruiting process, and Johan Zetterqvist for performing the statistical analyses. We would also like to thank Nitya Jayaram-Lindström and Nils Lindefors for believing in the Braining Project and making it possible.
Funding
Open access funding provided by Karolinska Institute. The study was funded by the regional agreement on medical training and clinical research (ALF) between Stockholm Regional Council, Stockholm Health Care Services and Karolinska Institutet, as well as the Centre for Psychiatry Research, Stockholm.
Author information
Authors and Affiliations
Contributions
LM, ÅA, AW, SS, CJS designed the research plan. LM acquired the funding and supervised the project. AW obtained ethical approval. All authors contributed to the conceptualization and design of the paper. AW and LK conducted the data collection. AW, ÅA and LK wrote the original draft, and were responsible for the rewriting process. LM, SS, CJS, TL contributed to editing. All authors have read and agreed to the published version of the manuscript.
Authors’ information
LM and ÅA founded the Braining method in 2017, as consulting psychiatrists at Psychiatry Southwest, and were pioneer Braining group training instructors. AW, LK and RB have been part of the Braining team staff.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study has been ethically approved by Swedish Ethical Review Authority, Medical Division. Approval number 2021-01717 and 2022-01077-02. Written informed consent was obtained from the participants. All methods were carried out in accordance with relevant guidelines and regulations in the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Anger, Å., Wallerblad, A., Kaaman, L. et al. Introducing Braining—physical exercise as adjunctive therapy in psychiatric care: a retrospective cohort study of a new method. BMC Psychiatry 23, 566 (2023). https://doi.org/10.1186/s12888-023-05053-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-023-05053-8