Abstract
Background
Despite over two years of COVID-19 worldwide, the outbreak of the Omicron variant has given rise to an unprecedented surge of infection with diverse lockdown measures implemented globally. Whether the emergence of a new wave of COVID-19 could further affect mental health in the population after nearly two years of the pandemic remains to be addressed. Furthermore, whether changes in smartphone overuse behaviours and physical activity – both of which are particularly relevant to young people – would together contribute to changes in distress symptoms during this wave of COVID-19 was also examined.
Methods
A total of 248 young people from an ongoing household-based epidemiological study in Hong Kong who completed their baseline assessments prior to the Omicron variant outbreak, i.e., fifth wave of COVID-19 (July–November 2021), were invited for a 6-month follow-up study during this wave of infection (January–April 2022) (mean age = 19.7 years, SD = 2.7; 58.9% females). At both time points, levels of global distress symptoms, perceived stress, smartphone overuse, frequency of engagement in vigorous physical activity, and other potential risk and protective factors were assessed.
Results
The proportion of young people presenting moderate-to-severe distress (6-item Kessler Psychological Distress Scale ≥ 5) significantly increased from 45.6 to 54.4% during the fifth wave of COVID-19 (p < 0.010). Significantly increased levels of smartphone overuse and reduced days of vigorous physical activity were also observed during the fifth wave. Notably, increased smartphone overuse and reduced physical activity both additively and interactively contributed to elevated distress at 6 months, even after accounting for demographic characteristics, psychiatric history, childhood adversity, as well as baseline distress symptoms, resilience, and recent personal stressors.
Conclusions
The findings suggest that the emergence of a new wave of COVID-19, specifically the Omicron outbreak, can further aggravate mental distress even after a protracted period of the pandemic. Awareness of the dynamic nature of COVID-19 is necessitated to address the pressing mental health needs of populations. Supporting young people in healthier patterns of smartphone use and physical activity can be helpful.
Similar content being viewed by others
Background
For over two years, the global society has experienced multiple waves of COVID-19 infections since its initial outbreak with new variants of concern. The Omicron variant, despite its possibly lower case fatality, has raised serious public health concerns owing to its higher transmissibility and lower vaccine efficiency [1,2,3]. Notably, the Omicron variant had emerged at a time of prolonged COVID-19 stress [4, 5]. Whether individuals will adapt and become acclimatised to pandemic lockdowns, or rather become sensitised amid the ongoing fluctuations of COVID-19, becomes an ever-important question.
Studies across countries have raised concerns over the mental health impacts of COVID-19 on the general population, such as increased levels of depressive and anxiety symptoms, as well as psychological distress [5,6,7,8,9]. Of note, the increase in mental distress in relation to COVID-19 appeared most pronounced among young people [6, 10]. Few studies, however, have yet examined factors that can potentially be modified during lockdowns to prevent the negative mental health impacts of COVID-19 [11].
Based on observations from earlier studies, the World Health Organization (WHO) has published several reports to consolidate existing findings on the impact of COVID-19 as a guide for further research [12,13,14]. The barriers to access to traditional mental health services had also been also highlighted, together with suggestions on approaches that may be adopted during this period, such as mental health helplines, outreach services, teletherapy, as well as self-help techniques [12,13,14].
Specifically, maintaining regular physical activity and staying connected with others (e.g., via phone or online), while minimising the reading of distress-inducing pandemic news, have been raised to be helpful strategies in promoting mental well-being during COVID-19 [13]. Indeed, the mental health benefits of regular physical activity (e.g., maintaining vigorous-intensity aerobic and muscle-strengthening activities at least three days a week for adolescents [15]) have been shown in prior work [16,17,18,19]. Alongside physical activity, with the growing reliance on digital devices today, smartphones have become a convenient means for young people to maintain social relationships and connections with their peers. Nevertheless, unmonitored and prolonged uses of smartphones can increase the risk of smartphone overuse (also referred to as smartphone addiction and compulsive or excessive smartphone use), which has been associated with symptoms of depression, anxiety, and psychological distress [20,21,22,23]. A recent study in an epidemiological sample of young people in Hong Kong has further demonstrated the longitudinal impact of smartphone overuse on severe depressive symptoms and functioning for up to 1 year [24].
Notably, several initial studies have reported significant increases both in sedentary behaviours [25, 26] and smartphone use and overuse [27, 28] in young people since the pandemic. Given that both these factors are modifiable (i.e., may be targets of interventions) and are generally less stigmatising, a more in-depth study into how these factors may together contribute to changes in mental health amid the Omicron lockdown period may offer new insights into the design of more effective and youth-friendly interventions for young people.
Existing evidence in the literature, however, is mostly cross-sectional, with data collected during the initial outbreak of the pandemic; the investigation of changes in distress over time as new waves of infection emerge has seldom been reported. Among the several longitudinal studies available, increased levels of mental distress and psychiatric symptoms have been reported during the early months of COVID-19 [6, 10, 29, 30]. For instance, a representative household-based longitudinal study in the United Kingdom found a significant increase both in the prevalence of severe psychological distress (from 18.9 to 27.3%) and mean levels of distress (from 11.5 to 12.6) compared to the pre-COVID period (2018–2019) [6]. Interestingly, several studies have in contrast observed a gradual decline in distress across waves of COVID-19 [31, 32], which have been taken to suggest a potential “habituation” effect. However, to the best of our knowledge, all such studies had been conducted before the Omicron outbreak [6, 10, 29]. With the distinct profile of the Omicron variant, whether mental distress of the population can be further aggravated after nearly two years of protracted COVID-19 remains to be explored.
Compared to other populations, the COVID-19 situation had generally been well-contained in Hong Kong. This was until the surge of the Omicron variant in December 2021, which resulted in the most severe wave of infection thus far [33, 34]. By March 2022, the 7-day average of new death rates related to COVID-19 had reached one of the highest in the world [35, 36]. While restrictions began to be gradually lifted in other countries, the local government has implemented some of the most restrictive lockdown measures to date [34], including city-wide dine-in restrictions, school lockdowns, work-from-home policies, strict travel restrictions (e.g., flight bans), as well as compulsory COVID-19 testing and compulsory quarantine at designated centres. The high population density and limited living space in Hong Kong make such large-scale lockdowns considerably more difficult to cope with [37, 38]. The unprecedented outbreak of this wave of COVID-19 not only brought about immense disruptions to the everyday lives of the population, but also an immense strain on the public health system and the economy [34, 39, 40].
Of note, before the advent of COVID-19 in early 2020 in Hong Kong, the population has already experienced months of large-scale social unrest from June 2019, with city-wide protests evolving into police-civilian confrontations involving the use of tear gas, bean bag rounds, and rubber bullets [41, 42]. Arrests in connection with the social unrest have in fact been made throughout different waves of COVID-19, including the period of the Omicron outbreak in 2022 [43, 44]. Local data have shown that these two types of population-level stressors (social unrest and pandemic-related) can interact with personal stressors to increase depressive and PTSD symptoms, particularly in young people [45, 46]. A cross-cultural study has also observed disproportionately higher rates of suicidal ideation among young adults during COVID-19 in Hong Kong compared to other Asian and Western countries (e.g., the Philippines, Canada, United States, United Kingdom, New Zealand, Belgium, and Switzerland), which has been attributed to the cumulative effects of the social unrest and COVID-19 [47]. Any further increase in mental distress since the surge of the Omicron variant would therefore suggest its potential to inflict further stress in a population where distress and tension are already rife.
In view of gaps in the current literature, we conducted a 6-month longitudinal study to examine changes in psychological distress among young people from an ongoing epidemiological study before and during the fifth wave of COVID-19 and the potential factors that may contribute to such changes. We hypothesised that young people would show significantly increased distress symptoms and perceived stress during this wave of the Omicron outbreak. We also anticipated a significant increase in smartphone overuse behaviours and reduction in days of vigorous physical activity during this period, which may both additively and interactively contribute to the increased levels of distress observed among these young people.
Methods
Sample and study design
Young people between the ages of 15 and 24 were consecutively invited from an ongoing household-based epidemiological study of youth mental health (HK-YES) in Hong Kong. A stratified multistage cluster sampling design was adopted in the larger HK-YES to improve sample representativeness. Specifically, invitation letters were posted to a random selection of addresses obtained from the local government estimated with a residing young person within the age range (stratified by geographic district and housing type). Data were collected through face-to-face interviews by trained researchers in the HK-YES, with the option for online video conferencing following the same procedures during COVID-19. Further details of the HK-YES have been described in our prior works [37, 48, 49]. For the current follow-up study, all participants invited from the HK-YES (n = 274) agreed to take part and had their baseline assessments completed between July and November 2021 (before the Omicron variant outbreak), with 6-month follow-up assessments completed between January and April 2022 (during the Omicron outbreak). Among these participants, none explicitly refused to take part at follow-up, although we were unable to contact 23 of the participants (8.4%). Among the rest who took part in the study at both time points (n = 251), a total of 248 participants provided complete data and were included in this study (98.8%).
The current sample had a mean age of 19.7 years (SD = 2.7) and was comprised of 58.9% (n = 146) females. Seven per cent (n = 17) reported having a psychiatric history. The core demographic characteristics of this sample and the Hong Kong population are presented in Supplementary Material 1. Participants of this study were slightly older (56.0% aged 20–24 vs. 52.7% in the Hong Kong population) and more likely to be females (58.9% vs. 54.3%). Similar proportions in housing type and geographic districts between this sample and the Hong Kong population were observed.
Written informed consents were obtained from all participants or from their parents or guardians for those below the age of 18. The study was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster.
Measures
Apart from participant background information collected as part of the larger HK-YES study (e.g., age, gender, experience of childhood adversity before the age of 17), we obtained data including psychiatric history, global distress symptoms, resilience, as well as experience of personal life stressors, at before and during the fifth wave of COVID-19 through self-administered surveys. Examples of items and their reliability indices are included in Supplementary Material 1.
Global distress symptoms
Global distress symptoms were assessed using the 6-item Kessler Psychological Distress Scale (K6) [50]. Items were rated on a 5-point Likert scale (“all of the time” to “none of the time”) and summed to generate a composite score. The K6 has been widely adopted to identify individuals at risk for potential psychiatric disorders both before and during COVID-19, including in some longitudinal studies [51,52,53,54,55]. Validation of the Chinese version of the K6 has been established among young people in Hong Kong [56]. The conventional cut-off score of 5 or above was used to indicate moderate-to-severe distress symptoms [57, 58]. The internal consistency of the K6 was good in this study (α = 0.89 and α = 0.87 at baseline and follow-up, respectively).
Perceived stress
Perceived stress was assessed using the single-item subjective level of stress (SLS-1) [49], which directly asks participants to indicate the level of stress they consider themselves to have experienced over the past month on a scale of 0 to 10 (0=“not at all”, 10=“extremely”). The content and face validity, incremental validity, as well as predictive validity of the SLS-1 have previously been established in local epidemiological and community youth samples [49].
Smartphone overuse
Smartphone overuse was assessed using two items adapted from the Revised Chen Internet Addiction Scale (CIAS-R) [59] to capture (i) the compulsive use of the Internet through smartphones (“I feel uneasy and am unable to control my compulsion to use the smartphone for the Internet once I stop using it even for just a short period”) and (ii) its impact on work or school and interpersonal relationships (“Using my smartphone to go online has negatively affected my studies or work and relationship with friends or family”). Specifically, the experience of compulsive use has been noted to be one of the key features of smartphone overuse and addiction [60, 61]. The first item used in this study was also based on those of the CIAS-R (11 “fail to control the impulse” and 2 “feel uneasy once I stop going online”) that contributed more strongly to the internal consistency of the scale using data from the larger representative youth epidemiological sample by our team (see Supplementary Material 2). Meanwhile, the second item was based on items of the CIAS-R that captures the impact of smartphone overuse on social and occupational functioning. Both items were rated on a 4-point Likert scale (“strongly disagree” to “strongly agree”). In this study, a rating of “agree” or “strongly agree” was used to define the presence of smartphone overuse and significant functional impact, respectively. Those who reported “strongly disagree” or “disagree” at baseline and “agree” or “strongly agree” at follow-up were considered to have shown increased smartphone overuse or increased functional impact during the Omicron outbreak.
Physical activity
Vigorous physical activity was assessed using an item from the International Physical Activity Questionnaire [62], which asks participants the number of days they have engaged in vigorous physical activities like heavy lifting, digging, aerobics, or fast bicycling during the past 7 days. Those who reported 3 days or more at baseline and less than 3 days at follow-up were considered to have shown reduced engagement in vigorous physical activity.
Resilience and stressful life events
Resilience was assessed using the 2-item Connor-Davidson Resilience Scale (CD-RISC-2), which includes the items “able to adapt to change” and “tend to bounce back after illness or hardship” adapted from the original 25-item CD-RISC [63]. The two items were rated on a 5-point Likert scale (“not true at all” to “true nearly all of the time”) and summed to generate a composite score. The validity and reliability of the Chinese version of the CD-RISC-2, as tested against the full CD-RISC, have been established among the general population in Hong Kong [64]. Cronbach’s alpha of the CD-RISC-2 in this study was 0.70 and 0.73 at baseline and follow-up, respectively.
Personal stressful life events (SLEs) were assessed using the Life Event Checklist for DSM-V [65], which contains 17 SLEs assessed on a binary checklist (yes/no), such as assault (physical, sexual), life-threatening illness or injury, and sudden violent death of a significant other. Items were also summed to determine the number of SLEs experienced.
Personal background factors
Psychiatric history was determined by asking participants whether they had received any official psychiatric diagnosis. Childhood adversity was assessed using items from the childhood section of the Composite International Diagnostic Interview 3.0 [66], which covers experiences in the domains of emotional abuse, physical abuse, neglect, and sexual abuse, with each item rated on a 5-point Likert scale (“never” to “very often”). A score of 3 or above given to any of the childhood adverse experiences was used to define the presence of childhood adversity.
Statistical analysis
Descriptive statistics at baseline and follow-up were generated for all variables (including distress symptoms, perceived stress, resilience, and experience of SLEs). We first tested whether the proportion of participants with moderate-to-severe distress symptoms (K6 ≥ 5) would increase at follow-up during the COVID-19 surge using the McNemar test. We adopted a K6 threshold of 5 or above which corresponds to moderate-to-severe distress symptom level [57, 58] (see above). To test the hypothesis that smartphone overuse and physical activity would be related to increased distress outcomes, we conducted a series of repeated measure ANOVAs and McNemar tests to compare levels of distress symptoms, perceived stress, smartphone overuse (both compulsive use and functional impact), engagement in vigorous physical activity, as well as resilience, and experience of SLEs, before and during the fifth wave of COVID-19 in Hong Kong.
A two-way ANOVA was then applied to determine the potential additive and interaction effects of increased smartphone overuse and reduced vigorous physical activity on 6-month distress symptoms during the fifth COVID-19 wave. Potential confounders, including age, gender, psychiatric history, childhood adversity, as well as baseline K6 score, baseline resilience, and recent personal SLEs (i.e., those reported at 6 months), were accounted for as controlled variables. To further determine the implications of smartphone overuse, another set of two-way ANOVA was applied to determine the potential additive and interaction effects of increased functional impact of smartphone overuse and reduced vigorous physical activity on 6-month distress symptoms (see Supplementary Material 5). All analyses were performed using SPSS version 26.0, with statistical significance set at the p < 0.05 level.
Results
The proportions of young people with moderate-to-severe mental distress significantly increased from 45.6% (n = 113) to 54.4% (n = 135) during the fifth wave (p = 0.009). Significant increases in global distress symptoms and perceived stress were also observed during the fifth wave of COVID-19 (K6: mean = 5.99, SD = 4.42 vs. mean = 5.31, SD = 4.48; SLS-1: mean = 5.62, SD = 2.02 vs. mean = 4.92, SD = 2.36), both p < 0.01 (Table 1).
In addition, significantly increased rates of smartphone overuse (compulsive use: 45.6% vs. 41.9%) and functional impact of smartphone use (29.4% vs. 25.0%), as well as reduced vigorous physical activity (27.8% vs. 36.7%), were also observed, all p < 0.001. No significant difference was observed in the levels of resilience and the number of SLEs experienced before and during the fifth COVID-19 wave, both p > 0.05.
Impact of increased smartphone overuse and reduced vigorous physical activity on distress symptoms before and during the fifth COVID-19 wave
In this sample, 15.7% (n = 39) showed increased smartphone overuse (i.e., no significant compulsive smartphone use at baseline and with compulsive use at follow-up), while 21.0% (n = 52) showed reduced vigorous physical activity (i.e., ≥ 3 days at baseline and < 3 days at follow-up) during the fifth COVID-19 wave. Descriptive statistics of these K6 distress scores are presented in Supplementary Material 4.
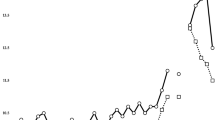
Using 6-month distress symptoms as the outcome, we found significant independent main effects of both increased smartphone overuse, F(1, 237) = 14.0, p < 0.001, and reduced vigorous physical activity, F(1, 237) = 5.6, p = 0.019, as well as a significant smartphone overuse X vigorous physical activity interaction effect, F(1, 237) = 5.2, p = 0.024, even after adjusting for demographics, psychiatric history, childhood adversity, baseline distress symptoms, resilience, as well as recent personal SLEs. These additive and interaction effects are illustrated in Fig. 1), with detailed findings presented in Table 2.
Similar findings were observed when considering the additive and interaction effects of increased functional impact of smartphone overuse and reduced vigorous physical activity on 6-month distress symptoms (all p < 0.05). Detailed findings are presented in Table S4 of Supplementary Material 5.
Discussion
To the best of our knowledge, this was among the first study to examine changes in mental health before and during the surge of the Omicron outbreak amid nearly two years of protracted COVID-19. We found that the emergence of the Omicron variant had contributed to a further increase in distress among young people on top of the prolonged pandemic. Notably, this elevation in distress was related to increased smartphone overuse and reduced physical activity not only in an additive but also multiplicative manner. Our findings highlighted the need to consider strategies to mitigate the consequences of similar public health crises and lockdowns in the future both in terms of mental health interventions and policy design.
The current work added to the literature in the discussion of whether mental health in young people will show patterns of adaptation to pandemic lockdowns or that their symptoms can become further aggravated as a new wave of COVID-19 emerges. In addition to examining changes in mental distress due to the Omicron outbreak, we were also interested in identifying potentially modifiable factors that may be involved in the process. We found that two important factors, namely smartphone overuse and reduced physical activity, had also been exacerbated and contributed to the elevated distress observed during the Omicron lockdown.
Particularly during lockdown periods where in-person activities and social contacts are restricted, it is acknowledged that smartphones can offer a convenient platform for such communications, the gratification of various needs, as well as coping with daily life stress [67, 68]. However, while frequent uses of smartphones may not necessarily be problematic, smartphone overuse can have significant impacts on mental health (also reported before COVID-19 [69, 70]) and can further contribute to poorer psychosocial functioning and both academic and work performance [24, 71]. There had also been suggestions that an increased dependence on smartphone use during COVID-19 can further perpetuate pandemic-related fears and distress [72]. The repeated cycles of news reading can possibly trigger a state of “event-based rumination” (i.e., repetitive thoughts about an external event), which has been shown to be associated with increased psychopathological symptoms amid large-scale population-level stress [73,74,75].
Meanwhile, although reduced physical activity may be understandable in the context of COVID-19, the impact that extended periods of lockdown restrictions has on mental health is of concern. Importantly, our previous study using the experience sampling method has found that engagement in active leisure activities can have protective effects against the impact of restrictive COVID-19 lockdown measures on momentary negative affect [37]. Offering suggestions to young people for maintaining physical activity that can be engaged in at home would be helpful (e.g., rope jumping, fast dancing or aerobic dancing, and even martial arts, are some examples of vigorous-intensity physical activities [76]).
Overall, supporting young people in the healthy use of smartphones and maintaining physical activity during COVID-19 is important. While few studies to date have systematically examined the effectiveness of interventions targeting smartphone overuse, a recent systematic review noted that a combination of psychological and behavioural interventions – particularly exercise interventions – may be optimal [77]. Together with our findings suggesting significant interactions between increased smartphone overuse (both compulsive use and its functional impacts) and reduced physical activity, incorporating exercise interventions in psychological interventions (whether delivered offline or online) may be further explored not only for maintaining physical activity, but also for preventing the worsening of smartphone overuse and improving mental health outcomes.
In the interpretation of findings of this study, we also note that some studies have reported patterns of habituation towards COVID-19 prior to the Omicron outbreak. For instance, findings from a previous local study based on data from an online text-based counselling service (N = 60,775) suggested signs of adaption and improved resilience in community members across four waves of COVID-19 from January 2019 to January 2021 [31]. Another longitudinal study in the United Kingdom has also reported a trend of reduced depressive and anxiety symptoms across the first 20 weeks of initial COVID-19 lockdown [32]. As with the majority of pandemic-related research, however, these studies had only covered the initial periods of COVID-19. Our current observations suggested a hitherto unanticipated effect: that after nearly 24 months of COVID-19, the Omicron surge was still able to trigger a significant aggravation in mental distress. This observation may at least partly be the result of fatigue following an extended period of COVID-19. The different nature of the Omicron variant (e.g., rapid spread to a large proportion of the population, extensive lockdowns in some areas) might also have played a role. These considerations highlighted the need for continued monitoring of the trajectory of youth mental health in the population across periods of COVID-19, as well as in the post-COVID period.
In addition, we did not find changes in resilience and the frequency of stressor exposure from before to during the fifth wave of COVID-19 in this sample. One of the reasons may owe to the assessment of resilience as a general trait (e.g., able to “adapt to change” and “bounce back”), which may be less susceptible to change as compared to adaptation in relation to COVID-19 or towards more severe or traumatic events. The two-year period of COVID-19 prior to the Omicron outbreak may also have equipped the population in adapting to the pandemic. Indeed, more recent studies have emphasised resilience not as the absence of psychopathology, but rather a dynamic and context-dependent process influenced by interdependent systems of developmental, neurobiological, psychological, and environmental factors [78, 79]. Identifying whether subgroups of individuals may be resilient (or more vulnerable) to the impact of COVID-19 lockdowns may facilitate the identification of young people at greater mental health risks. In addition, while an “others” option was provided in the LEC for assessing personal stressors, the stressful events covered in the LEC may be less sensitive to everyday life stressors, which may be more common during COVID-19 lockdowns. Examining the impact of pandemic-related stressors, as well as how their experiences might have differed from earlier waves of the COVID-19, may be helpful for designing more specific and context-relevant interventions.
Strengths and limitations
In contrast to existing longitudinal and cross-sectional studies conducted during the initial phases of COVID-19, the current study provided evidence to document the mental health impacts of the Omicron outbreak. With the use of a longitudinal design, the current investigation offered insights into whether distress levels could be further exacerbated in the context of protracted periods of population stress. We also examined the potential contribution of smartphone overuse and reduced physical activity – both of which are modifiable and less stigmatising – to elevated distress in young people. The observation that these two factors can potentiate the effect of one another to affect mental health outcomes, even after accounting for a wide range of potential confounding factors, suggested the potential importance of considering their roles in future interventions.
Nonetheless, we also acknowledge some limitations in the study. While the K6 is a widely validated measure and has shown to be valid in predicting risk for psychiatric disorders, it cannot replace clinical diagnosis. Our current findings should be taken as a reference for the change in those meeting the threshold of moderate-to-severe distress and distress severity instead of prevalence data. Due to the need for timely data collection, the use of simple self-administered measures is a common practice for tracking the differences in mental health before and since the outbreak of COVID-19 [6, 10, 29, 30]. Studies that aim to establish changes in the prevalence of diagnosable conditions may combine both self-administered and clinician-rated data in the future. Despite the satisfactory follow-up rate and similar profiles of this sample and the Hong Kong population in terms of housing type and household geographic district, our sample was comprised of slightly older and female participants. If longitudinal data before and during later waves of COVID-19 were available from other studies, it would be ideal to test the current observations in other settings and populations to determine their generalisability.
In addition, brief measures indeed can be valid measures of specific phenomena and have the benefit of simple administration, which are particularly beneficial when working with young people and in time-limited settings [49, 80]. Nonetheless, other related symptoms or subdomains of a phenomenon could not be fully captured, which can possibly provide additional information for specific intervention planning. Our single-item measures of smartphone overuse were not intended to determine clinical levels of smartphone addiction but rather to capture two key aspects of the phenomenon, namely compulsion and its impact on social and occupational functioning. It would be worthwhile to further examine whether other symptoms of smartphone overuse, such as tolerance and withdrawal, would also show similar patterns of associations. Lastly, while we focused on vigorous physical activity in this study, capturing physical activities also at light and moderate levels in the future may be helpful for determining the level of physical activity most beneficial for mental health in young people.
Conclusion
The present study underlined the need for the continued monitoring of mental health conditions and its related outcomes in the population over time amid large-scale stressors, such as COVID-19 – especially in young people, even when the situation initially appears to be well-contained. The complexity and unpredictability of the situation prevent the absolute knowledge of whether and when a next wave of infection or other public health crises will arrive. Improving future policies based on prior empirical evidence and preparing the population with adequate strategies using timely data to combat mental health challenges for future changes are imperative.
Data Availability
The data presented in the current manuscript could be made available upon reasonable request. Enquiries may be submitted to the corresponding author.
References
Dong R, Hu T, Zhang Y, Li Y, Zhou XH. Assessing the transmissibility of the New SARS-CoV-2 variants: from Delta to Omicron. Vaccines. 2022 Mar;24(4):496.
Chaguza C, Coppi A, Earnest R, Ferguson D, Kerantzas N, Warner F et al. Rapid emergence of SARS-CoV-2 Omicron variant is associated with an infection advantage over Delta in vaccinated persons. Med (N Y). 2022 May 13;3(5):325–34e4.
Wrenn JO, Pakala SB, Vestal G, Shilts MH, Brown HM, Bowen SM, Strickland BA, Williams T, Mallal SA, Jones ID, Schmitz JE. COVID-19 severity from Omicron and Delta SARS‐CoV‐2 variants. Influenza and other respiratory viruses. 2022 Apr 13; 16(5):832–6.
Karim SSA, Karim QA. Omicron SARS-CoV-2 variant: a new chapter in the COVID-19 pandemic. Lancet. 2021 Dec;11(10317):2126–8.
Choi EP, Hui BP, Wan EY. Depression and anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health. 2020 Jan;17(10):3740.
Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020 Oct;7(10):883–92.
Xiong JQ, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord 2020 Dec 1;277:55–64.
Nieto I, Navas JF, Vázquez C. The quality of research on mental health related to the COVID-19 pandemic: a note of caution after a systematic review. Brain Behav Immun Health. 2020 Aug;7:100123.
Galea S, Merchant RM, Lurie N. The Mental Health Consequences of COVID-19 and physical distancing: the need for Prevention and early intervention. JAMA Intern Med. 2020 Jun;180(1):817–8.
Shanahan L, Steinhoff A, Bechtiger L, Murray AL, Nivette A, Hepp U, et al. Emotional distress in young adults during the COVID-19 pandemic: evidence of risk and resilience from a longitudinal cohort study. Psychol Med. 2022 Apr;52(5):824–33.
Campion J, Javed A, Lund C, Sartorius N, Saxena S, Marmot M, et al. Public mental health: required actions to address implementation failure in the context of COVID-19. Lancet Psychiatry. 2022 Feb;9(2):169–82.
World Health Organization. The impact of COVID-19 on mental, neurological and substance use services: Results of a rapid assessment [Internet]. 2020 Oct. Available from: https://www.who.int/publications/i/item/978924012455.
World Health Organization. Mental health and psychosocial considerations during the COVID-19 outbreak [Internet]. 2020 Mar. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-MentalHealth-2020.1.
World Health Organization. Mental Health and COVID-19: Early evidence of the pandemic’s impact [Internet]. 2022 Mar. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1.
World Health Organization. WHO guidelines on physical activity and sedentary behaviour: at a glance [Internet]. 2020. Available from https://apps.who.int/iris/bitstream/handle/10665/337001/9789240014886-eng.pdf.
O’Brien WJ, Badenhorst CE, Draper N, Basu A, Elliot CA, Hamlin MJ et al. Physical Activity, Mental Health and Wellbeing during the First COVID-19 Containment in New Zealand: A Cross-Sectional Study. Int J Environ Res Public Healt]h 2021 Nov 16;18(22):12036.
Marconcin P, Werneck AO, Peralta M, Ihle A, Gouveia ÉR, Ferrari G et al. The association between physical activity and mental health during the first year of the COVID-19 pandemic: a systematic review. BMC Public Health. 2022 Feb 1;22(1):209.
Karageorghis CI, Bird JM, Hutchinson JC, Hamer M, Delevoye-Turrell YN, Guérin SMR et al. Physical activity and mental well-being under COVID-19 lockdown: a cross-sectional multination study. BMC Public Health 2021 May 27;21(1):988.
Pearce M, Garcia L, Abbas A, Strain T, Schuch FB, Golubic R et al. Association Between Physical Activity and Risk of Depression: A Systematic Review and Meta-analysis. JAMA Psychiatry. 2022 Jun 1;79(6):550–9.
Elhai JD, Dvorak RD, Levine JC, Hall BJ. Problematic smartphone use: a conceptual overview and systematic review of relations with anxiety and depression psychopathology. J Affect Disord 2017 Jan 1;207:251–9.
Kim H, Cho MK, Ko H, Yoo JE, Song YM. Association between smartphone usage and Mental Health in south korean adolescents: the 2017 Korea Youth Risk Behavior web-based survey. Korean J Fam Med. 2020 Mar;41(2):98–104.
Abi-Jaoude E, Naylor KT, Pignatiello A. Smartphones, social media use and youth mental health. CMAJ 2020 Feb 10;192(6):E136–41.
Lian SL, Sun XJ, Niu GF, Yang XJ, Zhou ZK, Yang C. Mobile phone addiction and psychological distress among chinese adolescents: the mediating role of rumination and moderating role of the capacity to be alone. J Affect Disord 2021 Jan 15;279:701–10.
Wong SM, Chen EY, Wong CS, Suen YN, Chan DL, Tsang SH, et al. Impact of smartphone overuse on 1-year severe depressive symptoms and momentary negative affect: longitudinal and experience sampling findings from a representative epidemiological youth sample in Hong Kong. Psychiatry Res. 2022 Nov;2:318:114939.
Yang S, Guo B, Ao L, Yang C, Zhang L, Zhou J, et al. Obesity and activity patterns before and during COVID-19 lockdown among youths in China. Clin Obes. 2020 Dec;10(6):e12416.
Rossi L, Behme N, Breuer C. Physical activity of children and adolescents during the COVID-19 Pandemic-A scoping review. Int J Environ Res Public Health [Internet]. 2021 Oct;30(21):11440.
Serra G, Lo Scalzo L, Giuffrè M, Ferrara P, Corsello G. Smartphone use and addiction during the coronavirus disease 2019 (COVID-19) pandemic: cohort study on 184 italian children and adolescents. Ital J Pediatr. 2021 Jul;2(1):150.
Chun J, Lee HK, Jeon H, Kim J, Lee S. Impact of COVID-19 on Adolescents’ Smartphone Addiction in South Korea. Soc Work Public Health. 2022 Oct;13:1–13.
Ramiz L, Contrand B, Rojas Castro MY, Dupuy M, Lu L, Sztal-Kutas C et al. A longitudinal study of mental health before and during COVID-19 lockdown in the french population. Global Health 2021 Mar 22;17(1):29.
Niedzwiedz CL, Green MJ, Benzeval M, Campbell D, Craig P, Demou E, et al. Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: longitudinal analyses of the UK Household Longitudinal Study. J Epidemiol Community Health. 2021 Mar;75(3):224–31.
Chan CS, Yang CT, Xu Y, He L, Yip PSF. Variability in the psychological impact of four waves of COVID-19: A time-series study of 60,000 text-based counseling sessions. Psychol Med. 2022 Mar 1;1–37.
Fancourt D, Steptoe A, Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry. 2021 Feb;8(1):141–9.
Wong SYS, Kwok KO, Chan FKL. What can countries learn from Hong Kong’s response to the COVID-19 pandemic? CMAJ. 2020 May 11;192(19):E511–5.
Burki T. Hong Kong’s fifth COVID-19 wave—the worst yet. Lancet Infectious Diseases. 2022 Apr 1;22(4):455-6.
Cheung PHH, Chan CP, Jin DY. Lessons learned from the fifth wave of COVID-19 in Hong Kong in early 2022. Emerg Microbes Infect. 2022 Dec;11(1):1072–8.
Smith DJ, Hakim AJ, Leung GM, Xu W, Schluter WW, Novak RT et al. COVID-19 Mortality and Vaccine Coverage - Hong Kong Special Administrative Region, China, January 6, 2022-March 21, 2022. MMWR Morb Mortal Wkly Rep 2022 Apr 15;71(15):545–8.
Wong SMY, Li YY, Hui CLM, Wong CSM, Wong TY, Cheung C, et al. Impact of restrictive COVID-19 measures on daily momentary affect in an epidemiological youth sample in Hong Kong: an experience sampling study. Curr Psychol. 2022 May;17:1–10.
Abu-Odah H, Ramazanu S, Saleh E, Bayuo J, Abed Y, Salah MS. COVID-19 pandemic in Hong Kong and Gaza Strip: Lessons learned from two densely populated locations in the World. Osong Public Health Res Perspect. 2021 Feb;12(1):44–50.
Chan H, Su X. Covid-19: “Exhausted, stressed out, helpless”: Hong Kong hospitals buckle under Omicron wave [Internet]. Hong Kong Free Press. 2022 [cited 2022 Jun 20]. Available from: https://hongkongfp.com/2022/02/17/covid19-exhausted-stressed-out-helpless-hong-kong-hospitals-buckle-under-omicron-wave.
Yau C, Yeo R. Omicron: tough social-distancing measures could hammer Hong Kong economy as experts predict slowdown in growth [Internet]. South China Morning Post. 2022 [cited 2022 Jun 20]. Available from: https://www.scmp.com/news/hong-kong/hong-kong-economy/article/3164581/omicron-tough-social-distancing-measures-could.
Shek DTL. Protests in Hong Kong (2019–2020): a perspective based on quality of life and well-being. Appl Res Qual Life. 2020 Mar;13:1–17.
Ni MY, Yao XI, Leung KSM, Yau C, Leung CMC, Lun P et al. Depression and post-traumatic stress during major social unrest in Hong Kong: a 10-year prospective cohort study. Lancet 2020 Jan 25;395(10220):273–84.
Ng KC. Hong Kong protests: more than 10,200 arrested in connection with unrest since 2019, government tells lawmakers [Internet]. South China Morning Post. 2021 [cited 2023 Jan 5]. Available from: https://www.scmp.com/news/hong-kong/politics/article/3128836/hong-kong-protests-more-10200-arrested-connection-unrest.
Mok L. Explained in data: What happened to Hong Kong’s protesters? [Internet]. Hong Kong Free Press. 2022 [cited 2023 Jan 5]. Available from: https://hongkongfp.com/2022/07/16/explained-in-data-what-happened-to-hong-kongs-protesters/.
Wong SMY, Hui CLM, Wong CSM, Suen YN, Chan SKW, Lee EHM, et al. Mental Health Risks after repeated exposure to multiple stressful events during Ongoing Social Unrest and Pandemic in Hong Kong: the role of rumination: risques pour la santé mentale après une exposition répétée à de multiples événements stressants d’agitation sociale durable et de pandémie à Hong Kong: le rôle de la rumination. Can J Psychiatry. 2021 Jun;66(6):577–85.
Wong SMY, Hui CLM, Suen YN, Wong CSM, Chan SKW, Lee EHM, et al. The impact of social unrest and pandemic on mental health of young people in Hong Kong: the transdiagnostic role of event-based rumination. Aust N Z J Psychiatry. 2021 Jun;26(4):376–84.
Schluter PJ, Généreux M, Hung KKC, Landaverde E, Law RP, Mok CPY, et al. Patterns of suicide ideation across eight countries in four continents during the COVID-19 pandemic era: repeated cross-sectional study. JMIR Public Health Surveill [Internet]. 2021 Oct;28(1):e32140.
Wong SMY, Ip CH, Hui CLM, Suen YN, Wong CSM, Chang WC et al. Prevalence and correlates of suicidal behaviours in a representative epidemiological youth sample in Hong Kong: the significance of suicide-related rumination, family functioning, and ongoing population-level stressors. Psychol Med. 2022;1–11.
Wong SMY, Lam BYH, Wong CSM, Lee HPY, Wong GHY, Lui SSY, et al. Measuring subjective stress among young people in Hong Kong: validation and predictive utility of the single-item subjective level of stress (SLS-1) in epidemiological and longitudinal community samples. Epidemiol Psychiatr Sci. 2021;30:e61.
Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003 Feb;60(2):184–9.
Angelina S, Kurniawan A, Agung FH, Halim DA, Wijovi F, Jodhinata C, et al. Adolescents’ mental health status and influential factors amid the Coronavirus Disease pandemic. Clin Epidemiol Glob Health. 2021 Oct;12:100903.
Kessler RC, Green JG, Gruber MJ, Sampson NA, Bromet E, Cuitan M, et al. Screening for serious mental illness in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative. Int J Methods Psychiatr Res. 2010 Jun;19(Suppl 1):4–22.
Sunderland M, Slade T, Stewart G, Andrews G. Estimating the prevalence of DSM-IV mental illness in the australian general population using the Kessler Psychological Distress Scale. Aust N Z J Psychiatry. 2011 Oct;45(10):880–9.
Essau CA, de la Torre-Luque A. Adolescent psychopathological profiles and the outcome of the COVID-19 pandemic: longitudinal findings from the UK Millennium Cohort Study. Prog Neuropsychopharmacol Biol Psychiatry. 2021 Aug;30:110:110330.
McGinty EE, Presskreischer R, Han H, Barry CL. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA 2020 Jul 7;324(1):93–4.
Chan SM, Fung TCT. Reliability and validity of K10 and K6 in screening depressive symptoms in Hong Kong adolescents. Vulnerable Child Youth Stud. 2014 Jan;9(2):75–85.
Prochaska JJ, Sung HY, Max W, Shi Y, Ong M. Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. Int J Methods Psychiatr Res. 2012 Jun;21(2):88–97.
Sakurai K, Nishi A, Kondo K, Yanagida K, Kawakami N. Screening performance of K6/K10 and other screening instruments for mood and anxiety disorders in Japan. Psychiatry Clin Neurosci. 2011 Aug;65(5):434–41.
Chen SH, Weng LJ, Su YJ, Wu HM, Yang PF. Development of Chinese Internet Addiction Scale and its psychometric study. Chinese Journal of Psychology. 2003 Jan 1;45(3):279–94.
Cha SS, Seo BK. Smartphone use and smartphone addiction in middle school students in Korea: prevalence, social networking service, and game use. Health Psychol Open. 2018 Jan;5(1):2055102918755046.
Lin YH, Chang LR, Lee YH, Tseng HW, Kuo TBJ, Chen SH. Development and validation of the Smartphone Addiction Inventory (SPAI). PLoS ONE. 2014 Jun;4(6):e98312.
Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003 Aug;35(8):1381–95.
Vaishnavi S, Connor K, Davidson JRT. An abbreviated version of the Connor-Davidson Resilience Scale (CD-RISC), the CD-RISC2: psychometric properties and applications in psychopharmacological trials. Psychiatry Res 2007 Aug 30;152(2–3):293–7.
Ni MY, Li TK, Yu NX, Pang H, Chan BHY, Leung GM, et al. Normative data and psychometric properties of the Connor-Davidson Resilience Scale (CD-RISC) and the abbreviated version (CD-RISC2) among the general population in Hong Kong. Qual Life Res. 2016 Jan;25(1):111–6.
Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, Keane TM. The life events checklist for DSM-5 (LEC-5). 2013.
Kessler RC, Ustün TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic interview (CIDI). Int J Methods Psychiatr Res. 2004;13(2):93–121.
Li J, Zhan D, Zhou Y, Gao X. Loneliness and problematic mobile phone use among adolescents during the COVID-19 pandemic: the roles of escape motivation and self-control. Addict Behav. 2021 Jul;118:106857.
Ratan ZA, Zaman SB, Islam SMS, Hosseinzadeh H. Smartphone overuse: a hidden crisis in COVID-19. Health Policy Technol. 2021 Mar;10(1):21–2.
Haug S, Castro RP, Kwon M, Filler A, Kowatsch T, Schaub MP. Smartphone use and smartphone addiction among young people in Switzerland. J Behav Addict. 2015 Dec;4(4):299–307.
Sohn SY, Rees P, Wildridge B, Kalk NJ, Carter B. Prevalence of problematic smartphone usage and associated mental health outcomes amongst children and young people: a systematic review, meta-analysis and GRADE of the evidence. BMC Psychiatry 2019 Nov 29;19(1):356.
Shen L, Wu X, Zhen R, Zhou X. Post-Traumatic Stress Disorder, Mobile Phone Dependence, and Academic Boredom in Adolescents During the COVID-19 Pandemic. Front Psychol. 2021 Nov 1;12:724732.
Yam FC, Korkmaz O, Griffiths MD. The association between fear of Covid-19 and smartphone addiction among individuals: the mediating and moderating role of cyberchondria severity. Curr Psychol. 2021 Oct;20:1–14.
Wong SMY, Hui CLM, Wong CSM, Suen YN, Chan SKW, Lee EHM, et al. Induced ideas of reference during social unrest and pandemic in Hong Kong. Schizophr Res. 2021 Mar;229:46–52.
Wong SMY, Hui CLM, Wong CSM, Suen YN, Chan SKW, Lee EHM, et al. Prospective prediction of PTSD and depressive symptoms during social unrest and COVID-19 using a brief online tool. Psychiatry Res. 2021 Apr;298:113773.
Nolen-Hoeksema S, Morrow J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: the 1989 Loma Prieta Earthquake. J Pers Soc Psychol. 1991 Jul;61(1):115–21.
Centre for Health Protection. Intensity of Physical Activity [Internet]. Centre for Health Protection, HKSAR Department of Health. 2012 [cited 2023 Jan 2]. Available from: https://www.chp.gov.hk/archive/epp/en/indexa830.html?MenuID=10.
Liu XXL. A systematic review of prevention and intervention strategies for smartphone addiction in students: Applicability during the COVID-19 pandemic. J Evid-Based Psychother. 2021 Sep 1;21(2):1–36.
Denckla CA, Cicchetti D, Kubzansky LD, Seedat S, Teicher MH, Williams DR, et al. Psychological resilience: an update on definitions, a critical appraisal, and research recommendations. Eur J Psychotraumatol. 2020 Nov;10(1):1822064.
Kaye-Kauderer H, Feingold JH, Feder A, Southwick S, Charney D. Resilience in the age of COVID-19. Bjpsych Advances. 1.
de Boer AG, van Lanschot JJB, Stalmeier PFM, van Sandick JW, Hulscher JBF, de Haes JCJM et al. Is a single-item visual analogue scale as valid, reliable and responsive as multi-item scales in measuring quality of life? Qual life res. 2004 Mar;13(2):311–20.
Acknowledgements
The authors would like to thank all participants of the current study and acknowledge the contribution of all research staff.
Funding
Funding of this study was received from Phase I of the Commissioned Study on Mental Health Survey, Food and Health Bureau, HKSAR Government (Reference number: MHS-P1 (Part 2)) and Hong Kong Jockey Club Charities Trust (Funding reference number: 2020/0012/001).
Author information
Authors and Affiliations
Contributions
SMYW and EYHC designed the study, interpreted the results, and wrote the initial draft of the manuscript. SMYW analysed the data. WH carried out the data collection and cleansed the data. SMYW, EYHC, WH, CLMH, and YNS were involved in developing the study design and analysis plan. All authors revised the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
E. Y. H. Chen has received speaker honoraria from Otsuka and DSK BioPharma, research funding from Otsuka, participated in paid advisory boards for Janssen and DSK BioPharma, and received funding to attend conferences from Otsuka and DSK BioPharma. All other authors declare no competing interests.
Ethics approval and consent to participate
Informed consents were obtained from all participants and from their parents or guardians for those below the age of 18. Ethical approval was granted by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster. All procedures were performed in accordance with the relevant guidelines and regulations and with the 1964 Declaration of Helsinki.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wong, S.M., Chen, E.Y., Suen, Y. et al. Increased psychological distress among young people before and during the fifth wave of COVID-19 after two years of pandemic in Hong Kong: a 6-month longitudinal study. BMC Psychiatry 23, 433 (2023). https://doi.org/10.1186/s12888-023-04933-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-023-04933-3