Abstract
Background
Given the unique socioeconomic structures, and the rural/urban differentials in the prevalence of mental illnesses in the country, this study aimed to explore the associations of childhood, adulthood and late-life rural/urban place of residence with mental health outcomes, namely depressive symptoms and cognitive impairment, among older adults in India. The study also examined the relationship between older individuals’ life-course rural/urban place of residence and late-life mental and cognitive health.
Methods
Utilizing data from the Longitudinal Aging Study in India (n = 28,027 older adults age 60 years and above), the study employed multivariable logistic and linear regression models to examine the association between urban/rural residential status, life-course residence, depressive symptoms and cognitive impairment among older adults.
Results
Childhood and adulthood place of residence was not associated with depressive symptoms in older men and women. Current rural place of residence was positively associated with depressive symptoms in older women [adjusted odds ratio (aOR): 1.37, confidence interval (CI): 1.05–1.80] but not men. Childhood [aOR: 1.88, CI: 1.16–3.04], adulthood [aOR: 2.00, CI: 1.26–3.16] and current rural residence [aOR: 1.93, CI: 1.27–2.91] was positively associated with cognitive impairment in men. Only current rural residence [aOR: 1.71, CI: 1.29–2.27] was associated with cognitive impairment in women. There was no significant association between life-course place of residence and depressive symptoms except in case of lifetime rural residence Respondents with urban-urban-urban (childhood-adulthood-current) place of residence were less likely to have depressive symptoms [adjusted coefficient (aCoef.): -0.14, CI: -0.21- -0.07] compared to those with rural-rural-rural place of residence. There were significant associations between life-course residence and cognitive impairment except among rural-urban-rural and urban-rural-rural migrants, showing an urban advantage in cognitive function among older adults.
Conclusions
This study showed significant associations between life-course residence and depressive symptoms among permanent rural/urban residents. The study also showed significant associations between life-course residence and cognitive impairment except among rural-urban-rural and urban-rural-rural migrants. Considering the rural disadvantage in mental and cognitive health among older adults, the government should continue to support policies that can improve access to education and healthcare among people residing in rural areas and women, in particular. The findings also urge social scientists and gerontologists in particular, to consider the importance of lifetime historical context while evaluating mental and cognitive health of older persons.
Similar content being viewed by others
Background
The proportion of older population in India is expected to increase from 9.4% in 2017 (126 million), to 19.1% in 2050 (317 million) [1]. With the increase in the proportion of the ageing population, the health risks accumulated over the life course are also increasing. Studies among older adults in the Indian context have shown that sedentary lifestyles were associated with an increase in the risk of obesity and resultant cardiovascular diseases and disability, especially in urban areas [2, 3]. The intensive care needs and long- term support for older adults with poor mental health and reduced cognition can burden the healthcare system in India significantly as this population continues to grow.
With growing urbanization, people are exposed to large number of social, physical and environmental risk factors in urban areas that contribute to their increased stress, which in turn, deteriorates their mental health [4]. By contrast, urban centers provide better access to education, highly paid jobs and health care facilities that result in increased treatment seeking [5, 6]. Further, a longitudinal study suggested that availability of physical and health resources and facilities associated with lifetime residential status in urban areas may lead to mental health improvement in later life among urban residents than rural counterparts [7]. The balance between the risk factors and protective factors of mental health associated with rural/urban residence calls for a better understanding of the interactions between life-course residential status and mental health. Similarly, multiple studies have shown that migration from one residential area (rural or urban) to another area is an important factor that could impact later-life cognitive function [8,9,10]. Most of the migration from one place to another mostly happens during adulthood; males tend to migrate for employment-related reasons, whereas females migrate predominantly due to marriage and family-related reasons [11, 12].
After moving from a rural area to an urban area at any stage of life, multiple factors at individual, family and community levels might contribute to improving or worsening mental and cognitive health of people in their later life. For example, rural to urban migration after entering to adulthood may reduce the quality relationships which can limit social interactions and cognitive stimulation among adults, and the resultant cumulative stress can undermine mental health and cognitive function in the long term [7, 13]. On the other hand, according to the healthy migrant phenomenon, those who migrate tend to be healthier and potentially less vulnerable to adverse health effects than those who do not migrate [14]. Moreover, those who migrate to urban areas may achieve better socioeconomic position, work and living conditions and access to healthcare [15,16,17], and therefore lower levels of mental disorders compared to people who reside in rural areas. Besides, urban non-migrants may have higher chances of improved mental health as they experience the beneficial aspects of the urban environment such as higher levels of education and income that allow them to maintain good health and wellbeing and avoid potential stressor of migration [18].
Recent studies have explored the socioeconomic factors and wealth-based inequalities associated with depression and cognitive impairments of older people in developing countries [19,20,21,22,23], and found that the socioeconomic structures, the pattern of rural/urban inequality and associated mental health outcomes in India are not similar to what is previously tested in Western societies. Therefore, there is a substantial knowledge gap regarding depressive symptoms and cognitive impairment among the rapidly growing older people with different status of rural/urban place of residence in India. This study aimed to explore the associations of childhood, adulthood and late-life place of residence with mental health outcomes (depressive symptoms and cognitive impairment) among older Indians. Guided by a life course perspective, the study also examined the relationship between older individuals’ life-course place of residence and late-life mental and cognitive health in India.
Methods
Data
This study used data from the first wave of the Longitudinal Aging Study in India (LASI, 2017-19). The Harvard T.H. Chan School of Public Health, the International Institute for Population Sciences (IIPS), and the University of Southern California (USC) collaborated on data collection procedures of the LASI survey. The nationally representative longitudinal survey is proposed to collect crucial information on the physical, social, and cognitive well-being of India’s older citizens over a 25-year period. The baseline survey of LASI collected data of over 72,000 people age 45 and over, as well as their spouses (of any age), across India’s states and union territories. The sample is based on a multistage stratified cluster sample design that includes three and four separate phases of rural and urban region selection, respectively. The LASI report contains information on sample design, survey instruments, fieldwork, data collecting and processing, and response rates [24]. The details of the survey strategies are also described elsewhere [25]. The final sample for the current study included 28,027 (14,286 males and 13,741 females) older Indian adults age 60 years or older with information on formal residence during childhood and adulthood and late life residence (at present).
Measures
Outcome variables
Major probable depression as an outcome variable of this study was coded as 0 for not having depressive symptoms and 1 for having depressive symptoms. Probable depression among older adults with symptoms of dysphoria, was calculated using the Short Form Composite International Diagnostic Interview (CIDI-SF) [26, 27]. This scale estimates a probable psychiatric diagnosis of major depression and has been validated in field settings [28, 29]. It has 3 screening and 7 symptom-based questions and a score of three or more on a scale of 0–10 leads to a 0.55 probability of CIDI caseness of major depression [30], which in this study is labelled as having depressive symptoms. The scale was validated with well-established cross-cultural applicability especially by non-clinicians in general population surveys and widely used in population-based health surveys [29, 31, 32]. Cronbach’s alpha indicated that CIDI-SF has acceptable reliability (α = 0.7). The scale was used in continuous form as the outcome, modelled as the number of depressive symptoms, during the analysis of life-course residential status and depressive symptoms.
Cognitive impairment was another outcome variable of this study and was measured through five broad domains (memory, orientation, arithmetic function, executive function, and object naming). Memory was measured using immediate word recall, delayed word recall; orientation was measured using time and place measure; arithmetic function was measured through backward counting, serial seven, and computation method; executive function was measured through paper folding and pentagon drawing method, and object naming was also done to measure the cognitive impairment among older adults. The overall score ranged between 0 and 43, and a higher score indicated better cognitive functioning. The lowest 10th percentile was used as a proxy measure of poor cognitive functioning [28]. Further, during the analysis of life-course residential status and cognitive impairment, the score was reversed to assess the cognitive impairment among older adults and thus after reversing, the higher score indicated higher levels of cognitive impairment.
Exposure variables
Current place of residence was coded as urban (those residing in statutory/Census towns) and rural (those residing in villages). Further, considering information on their formal residence, respondents were classified as urban or rural residents according to their residence during childhood and adulthood if they reported living in either town or village locations in response to survey questions on where they spent most of their childhood (up to age 14) and most of their adult life. Additionally, those who responded to the question “How many years have you been living (continuously) in this area?” as “since birth”, were accorded a childhood/ adulthood place of residence respective to their current place of residence. Further, categories of lifetime residence were created using a sequence of childhood, adulthood, and current time periods with responses classified as urban or rural. This was based on the survey questions on where individuals spent most of their childhood and most of their adult life, along with the location of their current household residence, and resulted in 8 possible life-course patterns: 1) rural-rural-rural; 2) rural-rural-urban; 3) rural-urban-urban; 4) rural-urban-rural; 5) urban-rural-rural; 6) urban-urban-rural; 7) urban-rural-urban and 8) urban-urban-urban. The same approach was followed in previous studies [33, 34].
Other covariates
Independent variables considered for adjustment in the analysis included sex (male/female); age (60–69, 70–79, and 80 + years); education (no formal education, primary, secondary and higher); work status (never worked, worked but currently not, currently working and retired) marital status (currently married, widowed and others which included separated, divorced and never married); and living arrangements (living alone, with spouse, with spouse and children and with others). Further, to control for the possible confounding of physical health in the association of residential status with mental health outcomes, self-rated health and functional difficulty were included in the analysis and self-rated health was coded as good which includes very good, good and fair whereas, poor includes poor and very poor. Difficulty in activities of daily living and instrumental activities of daily living (ADL and IADL) were categorised into yes if the respondent reported at least one difficulty in the daily living basic and instrumental activities, respectively [35].
Besides, the following socio-demographic variables were selected and included in the analysis as per literature. Monthly per capita consumption expenditure (MPCE) quintile was assessed using household consumption data and was divided into five quintiles of poorest, poor, middle, rich and richest [24]. Religious group was coded as Hindu, Muslim, Christian, and Others. Caste group was recoded as Scheduled Caste/Scheduled Tribe (SC/ST), Other Backward Classes (OBC), and others [24]. Others refer to those with higher social status, mostly belonging to the higher socioeconomic groups and upper castes [36]. Finally, the regions of the country were categorised into North, Central, East, Northeast, West, and South.
Statistical analysis
Descriptive statistics were reported at the initial stage. Bivariate analysis (cross-tabulations) was conducted to report the prevalence of depressive symptoms and cognitive impairment among the study participants. Mean scores of depressive symptoms and cognitive impairment along with their confidence intervals (CI) were reported across the eight categories of life-course residence. For analyzing the statistical significance of the associations for each category, t-test was conducted and p-values are reported. Multivariable logistic regression models were employed to examine the unadjusted and adjusted (model 1 adjusted for age, education and work status model 2 adjusted for all the covariates included in this study) associations of urbanicity of residence in childhood and adulthood as well as late life with depressive symptoms and cognitive impairment.
Further, linear regression models were employed to examine the association of life-course residential status (with eight possible categories) with depressive symptoms and cognitive impairment (continuous outcomes) adjusting for all the covariates included in this study. Unadjusted and adjusted odds ratios (uOR and aOR) and coefficients (uCoef and aCoef) along with beta coefficients are presented along with 95% CI. Individual weights were applied during the analysis to account for the clustered and stratified survey design. The values of area under the receiver operating characteristic curve (AUROC) of 0.7 and 0.8 for the outcomes of depressive symptoms and cognitive impairment in the logistic regressions (supplementary material Figure S1a and b) suggested good fit models. Also, linear regressions met all assumptions and included tests for linearity and normality of residuals and multi-collinearity of predictor variables and are presented through visual inspections of scatterplots, quantile-quantile plots and variance inflation factors (VIFs) (supplementary material Figures S2a- S3b and Table S1, respectively). All the analysis was conducted in Stata version 15.1.
Results
Descriptive statistics of older men and women in this study are displayed in Table 1. A little more than half of the sample population was males (51.37%) and a total of 16.6% of older men and 55.02% of older women were widowed. A total of 2.54% older men and 9.01% older women lived alone. More than 61% and 85% of older women had no or primary level of formal education. A proportion of 22.16% and 26.13% of older men and women had poor self-rated health, respectively. Notably, 26.68% of older men and 32.2% of older women currently resided in urban areas. On the other hand, 4.3% of rural-dwelling older adults and 6.26% urban-dwelling older adults were living alone. A total of 22.16% of older men and 26.13% of older women as well as 21.48% of rural-dwellers and 25.17% of urban-dwellers reported a poor self-rated health in this study.
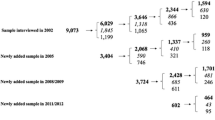
Figure 1 presents the percentage distribution of older adults by childhood, adulthood and current residence. Further, among the male and female sample with urban childhood residence, the rate of depressive symptoms was 6.62% and 5.56%, while the rate among older adults with rural childhood residence was 7.78% and 10.81% in men and women respectively. Similarly, the rate of cognitive impairment was substantially higher among women than men with only 2.43% and 10.29% of older men with rural and urban childhood residence having cognitive impairment against 8.43% and 23.19% of older women with respective childhood residence having cognitive impairment (Fig. 2a). The rates of depressive symptoms in the samples based on type of adulthood residence were 6.41% and 6.35% for urban and 7.87% and 10.67% for rural residence. Also, the rate of cognitive impairment among men and women with rural residence in adulthood was 8.66% and 23.28% and with urban residence only 2.27% and 10.75%, respectively (Fig. 2b). By current place of residence, higher percent of men (7.99%) and women (11.15%) residing in rural areas had depressive symptoms compared to those in urban areas (6.21% and 6.45%), and higher percent of rural residing men (8.97%) and women (24.7%) had cognitive impairment than their counterparts in urban areas (2.4% and 10.3%) (Fig. 2c).
There were no significant associations between childhood and adulthood residence with depressive symptoms among older men in this study (Table 2). However, in the unadjusted logistic regression model, the odds for men who reside in rural areas in their late life were 1.28 (95% CI: 1.02–1.61), which was higher in comparison to men who reside in urban areas. The association was insignificant after adjusting for the selected covariates in the study. For female counterparts, there was significant positive association of childhood rural residence (aOR: 1.47, 95% CI: 1.04–2.07) and current rural residence (aOR: 1.37, 95% CI: 1.05–1.80) with depressive symptoms after adjusting for all the covariates. In case of adulthood residence, the odds of depressive symptoms after adjusting for age, education and work status were 1.44 times (95% CI: 1.05–1.96) higher among women who spent most of their childhood in rural areas in comparison to women who spent most of their childhood in urban areas.
In case of cognitive impairment, childhood (aOR: 1.88, 95% CI: 1.16–3.04), adulthood (aOR: 2.00, 95% CI: 1.26–3.16) and current (aOR: 1.93, 95% CI: 1.27–2.91) rural residences were independently associated with cognitive impairment among older men. Similarly, current rural residence was positively associated with cognitive impairment among older women (aOR: 1.71, 95% CI: 1.29–2.27). However, in case of older women, after controlling for all the covariates, there was no significant but positive associations of childhood (aOR: 1.25, 95% CI: 0.85–1.85) and adulthood (aOR: 1.35, 95% CI: 0.95–1.92) rural residence with cognitive impairment.
Table 3 presents the depressive symptoms and cognitive impairment among older adults in the study by their life-course place of residence. A higher percentage of the sample (69.26%) had a lifetime rural place of residence (rural childhood, rural adulthood and rural current place of residence). On the other hand, 18.19% of the sample population had a lifetime urban place of residence (urban childhood, urban adulthood and urban current place of residence). Further, older adults who had a rural childhood, urban adulthood and rural late-life place of residence had higher mean score of depressive symptoms compared to all other categories. However, older adults who had an urban childhood, rural adulthood and rural late-life place of residence had higher mean score of cognitive impairment compared to all other categories.
Table 4 presents the adjusted linear regression estimates of depressive symptoms by life-course place of residence among older adults. Older adults who had a lifetime urban place of residence (urban childhood, urban adulthood and urban current place of residence) had significantly lower likelihood of depressive symptoms (aCoef: 0.14, p < 0.001) than those who had lifetime rural place of residence.
Table 5 presents the adjusted linear regression estimates of cognitive impairment by life-course place of residence among older adults. Older adults who had a lifetime urban place of residence (urban childhood, urban adulthood and urban current place of residence) had significantly lower likelihood of cognitive impairment (aCoef: 2.34, p < 0.001) than those who had lifetime rural place of residence.
Discussion
The study observed significant differences in depressive symptoms and cognitive impairment among older Indians by their urban/rural residential status. Rural place of residence was a significant risk factor for depressive symptoms among older women and cognitive impairment among older men and women in this study. Again, older adults who resided in urban areas during childhood, adulthood and later life had the lowest level of depressive symptoms and cognitive impairment; whereas those who resided in rural areas during their lifetime had the highest level of depressive symptoms and cognitive impairment among the eight groups. These findings remained after adjusting for the socio-demographic and economic factors such as age, education, work status, household consumption quintiles, religion, caste and regions as well as psychosocial resources such as marital status and living arrangements and self-rated health and functional difficulties, although they accounted for much of the associations.
Previous studies among different populations in different age groups have shown that urban/rural residential status of individuals has significant association with their health and wellbeing [37, 38]. A study among adolescents in West Africa suggests that schooling and urban residence may have positive effects on their behaviors and skills which in turn result in the improvement of cognitive abilities [39]. Another study among the general population in Indonesia found that social capital increases life satisfaction among urban residents but not rural residents [40]. Also, older adult social participation was shown to have differential effects on health in rural and urban areas [41]. The higher rates of depression and cognitive impairment in rural areas in this study may be explained by the fact that the rural population is engaged in highly stressful jobs, have lack of formal education, inadequate healthcare and housing facilities, and perform worse in other social determinants of health. Previous studies have also reported a similar urban-rural gradient in depression and cognitive function among older adults in India, with a rural disadvantage [42,43,44,45]. Multiple studies in other countries have however, reported positive, negative and no effect of rural residence on depression in later life [46, 47]. The current analysis showed no significant association of place of residence at any stage of life with depressive symptoms among older men. The current finding is consistent with a study in Ghana that found no significant association between childhood, adulthood and late life urbanicity with depression [48]. This is also in line with an earlier study suggesting that current rural residence is more important in predicting depression than a prior history of a rural residence [33].
However, the current analysis showed that older women who resided in rural areas during their childhood are more likely to develop depressive symptoms than older women who lived their childhood in urban communities. The association remained significant even after adjusting for all the covariates in the study. Although the association is of borderline statistical significance, the finding may be explained by increased stress among people with limited resource in village areas. Separating from one’s biological family may in turn cause greater levels of stress, lower levels of social cohesion, and the loss of social support that could adversely affect cognitive function [49]. The different levels of depressive symptoms and cognitive impairment among rural resident older men and women may be explained by differential impact of lack of social networks, food insecurity and unequal gender norms on mental health of men and women in rural areas [50]. This may also be explained by the limited access to education and healthcare as well as lower rate of labor force participation in rural settings particularly among women [43, 51].
On the other hand, the positive association of rural residence during adulthood with depressive symptoms disappeared after adjusting for socioeconomic characteristics. Notably, the effect that is not seen in models adjusting for potential confounding factors may suggest that other factors directly related to mental health might have also contributed to influence the finding. For instance, lack of income, long distance to health facilities, and limited services and amenities may lead to increased risk of depressive symptoms among older people who reside in rural areas. However, as documented in previous studies, the factors that potentially reduce the risk of mental illnesses in rural areas may include residential stability, quality relationships and stable social networks. Again, individual factors such as resilience, independence and self-sufficiency may reduce the risk of depressive symptoms and cognitive impairment among rural residents. These could be considered while developing future policies and programs for older Indian adults.
Furthermore, considering the life-course residential patterns, the association between place of residence and mental health outcomes in this study is only significant in case of older people who stayed in the same residential area and those who resided in urban areas throughout their life had lower chances of depressive symptoms or cognitive impairment. On the other hand, people who resided in rural areas during childhood and adulthood and migrated to urban areas had less likelihood of depressive symptoms and cognitive impairment in this study compared to rural non-migrants. This is in line with multiple cross-sectional as well as longitudinal studies on the positive effects of rural-to-urban migration on mental health of older adults [4, 47]. The finding also supports the “healthy migrant” hypothesis, which states that migrants represent a positively selected group of individuals with respect to health, relative to the general population in origin societies [52, 53]. However, the current finding is in contrary to a previous study in China that suggested that migration from rural to urban areas may lead to experience of social stigma, discrimination and inequity, which ultimately result in social exclusion and negatively affect the mental health of migrant people compared to non-migrant people [54].
Interestingly, unlike depressive symptoms, the associations of life-course residential status with cognitive impairment were highly significant in this study. Compared to non-migrant rural residents, those who moved to urban areas during adulthood or late life were less likely to have cognitive impairment. The underlying mechanism by which residential changes may influence cognitive function is not well established yet. Health and wellbeing of a person is influenced by the complex interactions between environmental factors and body functions and structures as well as activities and participation [55, 56]. As people age, functional or intrinsic capacities, like walking, hearing, seeing, and cognitive ability will reduce and this is escalated in poor socioeconomic setting [57, 58]. Besides, people’s health conditions and adaptability change as they move in and out of different neighborhood over the life course [59, 60]. Studies have reported that residential mobility and migration are associated with an increased economic instability and changes in marital status, family composition and employment [61], which may gradually contribute to cognitive reserve and improved cognitive abilities among older people. In addition, the psychological and cognitive health is improved by the social participation among older people facilitated by the urban community environment [62, 63].
On the other hand, people from rural areas who resided in urban areas during adulthood had lower chances of cognitive impairment than rural non-migrants. Similarly, non-migrant urban residents were less likely to have cognitive impairment in this study. This is supportive of earlier findings that urban residence is positively associated with cognitive function among older adults, attributed to several reasons such as higher literacy, educational and occupational opportunities and health resources [64]. Similarly, urban environment is considered as psychologically and socially demanding [65], which may positively affect the cognitive reserve among older urban residents. Further, the lifetime urban residence might also include those who migrate from one urban area to another during their life time. Consistently, moving from one urban area to another urban area may reflect an increase in socioeconomic standing, such as education and income [12]. The higher magnitude of the association of life-time urban residents with better cognition than those who moved to urban areas during adulthood or late life suggest that the rural-to-urban migrants may have lower access to utilization of health care and limited social support than urban residents [66,67,68]. This is again reflected in the reduced odds after accounting for socioeconomic characteristics in the fully adjusted analysis. The finding, thus, suggest that, the differences may be largely due to the socioeconomic disadvantages among rural-to-urban migrants compared with urban residents [69]. Nevertheless, specific environmental effects independent of socioeconomic conditions on mental and cognitive health need further exploration including the effect of population density, green areas, noise and diet.
The study covers a large sample of older adults from a geographically large and socioeconomically heterogeneous country. Moreover, the findings are robust as the analysis employed multiple linear regression models after adjusting for a large number of potential confounders. Furthermore, during the data collection, the LASI used reliable valid measures and trained interviewers gathered the data. Nevertheless, there are several limitations to be noted. Without knowing the reasons for and/or implications of relocating from urban-to-rural areas in India, it is unclear whether and how this form of migration is associated with cognitive function. Further, in the absence of indicators of reasons for migration, the migration variable used in this study may not have adequately captured all aspects of people’s migration history. Although the study included many of the possible confounding factors that may relate to cognition, additional unmeasured factors such as genetic factors, occupational status, environmental pollution, and healthcare utilization may have contributed to the associations [70]. Similarly, length of stay in rural or urban areas may have differential impact on cognitive function among older persons [71, 72], which is not accounted in this study. Further, the sample size of some groups of life-course residential categories was small (e.g., rural-urban-rural migrants) which might have influenced the study findings. Lastly, due to the cross-sectional nature of the analysis, interpretation of the results requires caution. Additional longitudinal studies are required to further examine these and other factors that may contribute to migration-related differences in mental health and cognitive function. Another limitation is the difficulty accounting for different rural factors (population density, distance to services, economic base, etc.), which may affect depressive symptoms and cognitive abilities.
The findings are crucial in terms of its policy implications. Taken together, effective interventions should be developed and implemented in rural areas to reduce the higher rate of depressive symptoms and prevent or prolong cognitive decline in older adults, especially among those who are life time rural-dwellers. To that end, health care providers should promote and employ early screening for probable depression and cognitive impairments among older adults living in rural areas and among rural resident women in particular and identify at-risk subpopulations. The current findings based on the life course residence indicating the differential impact of transitions in rural/urban residence across different stages of life on mental health and wellbeing add to the knowledge gap in environmental influence on older adults’ healthy and active aging, especially in low- and middle-income country settings. This study also calls for further attention to future research on the mind sponge mechanism suggesting that individuals’ wellbeing is negatively influenced by their exposure to multiple contextual risk factors such as lack of health awareness and limited healthcare services, particularly in rural areas [73, 74].
Conclusions
This study showed significant associations between life-course residence and depressive symptoms among permanent rural/urban residents. The study also showed significant associations between life-course residence and cognitive impairment except among rural-urban-rural and urban-rural-rural migrants. Current findings are important for policy-makers and clinicians. Considering the rural disadvantage in mental and cognitive health among older adults, the government should continue to support policies that can improve access to education and healthcare among people residing in rural areas and women, in particular. Clinicians working in rural areas should be aware that their patients have an increased risk of developing mental illnesses such as depression and cognitive impairment than people in urban centres. Besides, there are considerable barriers in the delivery of care to older adults with depressive symptoms in rural areas. For individuals residing in rural areas, access to primary and secondary care, as well as access to social and psychological services may be limited by travel distance, lack of service providers, and cultural factors, which can increase their risk of mental illnesses and cognitive decline. Thus, models of care for older adults with depressive symptoms and cognitive impairment require further research with special attention to rural areas. The findings also urge social scientists and gerontologists, in particular, to consider the importance of lifetime historical context while evaluating mental and cognitive health of older persons.
Availability of data and materials
The data are available at The Gateway to Global Aging Data (https://g2aging.org/?section=overviews&study=lasi).
References
United Nations Department of Economic and Social Affairs, Population Division. World population ageing report. 2017.
Rastogi T, Vaz M, Spiegelman D, Reddy KS, Bharathi AV, Stampfer MJ, et al. Physical activity and risk of coronary heart disease in India. Int J Epidemiol. 2004;33(4):759–67.
Muhammad T, Srivastava S, Hossain B, Paul R. Decomposing rural–urban differences in successful aging among older Indian adults. Sci Rep. 2022;12(1):1–14.
Zhang J, Chandola T, Zhang N. Understanding the longitudinal dynamics of rural–urban mental health disparities in later life in China. Aging Ment Health. 2022;26:1–10.
Thirthalli J, Reddy KS, Kare M, Das S, Gangadhar BN. Rural–urban differences in accessing mental health treatment in patients with psychosis. Int J Soc Psychiatry. 2017;63(8):694–8.
Srivastava S, Sulaiman KM, Drishti D, Muhammad T. Factors associated with psychiatric disorders and treatment seeking behaviour among older adults in India. Sci Rep. 2021;11(1):1–13.
Pearce J, Cherrie M, Shortt N, Deary I, Ward Thompson C. Life course of place: a longitudinal study of mental health and place. Trans Inst Br Geogr. 2018;43(4):555–72.
Raina SK, Razdan S, Pandita KK. Prevalence of dementia in ethnic Dogra population of Jammu district, North India: a comparison survey. Neurol Asia. 2010;15(1):65.
Raina SK, Raina S, Chander V, Grover A, Singh S, Bhardwaj A. Is dementia differentially distributed? A study on the prevalence of dementia in migrant, urban, rural, and tribal elderly population of Himalayan region in northern India. North Am J Med Sci. 2014;6(4):172.
Xu H, Dupre ME, Gu D, Wu B. The impact of residential status on cognitive decline among older adults in China: results from a longitudinal study. BMC Geriatr. 2017;15(1):107.
Bhagat RB. Changing pattern of internal migration in India. Contemporary demographic transformations in China, India and Indonesia. Berlin: Springer; 2016; p. 239–54.
Bhagat RB. Urban migration trends, challenges and opportunities in India. World Migr Rep. International Organization for Migration. Switzerland. 2015;5–30.
Orsholits D, Cullati S, Cheval B, Ghisletta P, Oris M, Maurer J, et al. Residential trajectories across the life course and their association with cognitive functioning in later life. Sci Rep. 2022;12(1):1–10.
Lu Y. Test of the ‘healthy migrant hypothesis’: a longitudinal analysis of health selectivity of internal migration in Indonesia. Soc Sci Med. 2008;67(8):1331–9.
Lu Y. Mental health and risk behaviours of rural–urban migrants: longitudinal evidence from Indonesia. Popul Stud. 2010;64(2):147–63.
Zhang X, Dupre ME, Qiu L, Zhou W, Zhao Y, Gu D. Urban-rural differences in the association between access to healthcare and health outcomes among older adults in China. BMC Geriatr. 2017;17(1):1–11.
Chatterjee, S., & Sarkar, K. Appraisal of urban–rural disparities in access to health care facilities and exposure to health risk factors: A case study of Durgapur Industrial region, India. GeoJournal. 2022;87(5):4007–24.
Albers HM, Kinra S, Radha Krishna KV, Ben-Shlomo Y, Kuper H. Prevalence and severity of depressive symptoms in relation to rural-to-urban migration in India: a cross-sectional study. BMC Psychol. 2016;4(1):47.
Muhammad T, Srivastava S, Sekher TV. Association of self-perceived income sufficiency with cognitive impairment among older adults: a population-based study in India. BMC Psychiatry. 2021;21(1):1–14.
Muhammad T, Sekher TV, Srivastava S. Association of objective and subjective socioeconomic markers with cognitive impairment among older adults: cross-sectional evidence from a developing country. BMJ Open. 2022;12(8): e052501.
Muhammad T, Srivastava S, Sekher TV. Assessing socioeconomic inequalities in cognitive impairment among older adults: a study based on a cross-sectional survey in India. BMC Geriatr. 2022;4(1):389.
Patel R, Singh U. Prevalence study of cognitive impairment and its associated sociodemographic variables using mini-mental status examination among elderly population residing in field practice areas of a medical college. Indian J Community Med. 2018;43(2):113.
Muhammad T, Skariah AE, Kumar M, Srivastava S. Socioeconomic and health-related inequalities in major depressive symptoms among older adults: a Wagstaff’s decomposition analysis of data from the LASI baseline survey, 2017–2018. BMJ Open. 2022;12(6):e054730.
International Institute for Population Sciences (IIPS), National Programme for Health Care of Elderly (NPHCE), MoHFW, Harvard T. H. Chan School of Public Health (HSPH) and the University of Southern California (USC). Longitudinal ageing study in India (LASI) wave 1, 2017-18, India Report. Mumbai; 2020.
Bloom DE, Sekher TV, Lee J. Longitudinal aging study in India (LASI): new data resources for addressing aging in India. Nat Aging. 2021;1(12):1070–2.
Meher T, Muhammad T, Gharge S. The association between single and multiple chronic conditions and depression among older population in India: a comparative study between men and women. Int J Geriatr Psychiatry. 2021;37(1)
Muhammad T, Meher T, Sekher TV. Association of elder abuse, crime victimhood and perceived neighbourhood safety with major depression among older adults in India: a cross-sectional study using data from the LASI baseline survey (2017–2018). BMJ Open. 2021;11(12): e055625.
International Institute for Population Sciences (IIPS), MoHFW NPHCE, Harvard TH, Chan School of Public Health (HSPH), The University of Southern California (USC). Longitudinal Ageing Study in India (LASI) Wave 1. India report. Mumbai; 2020.
Kessler RC, Üstün BB. The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) Composite International Diagnostic interview (CIDI). Int J Methods Psychiatr Res. 2004.
Walters EE, Kessler RC, Nelson CB, Mroczek D. Scoring the World Health Organization’s composite international diagnostic interview short form (CIDI-SF). Geneva: World Health Organ; 2002.
Trainor K, Mallett J, Rushe T. Age related differences in mental health scale scores and depression diagnosis: adult responses to the CIDI-SF and MHI-5. J Affect Disord. 2013;151(2):639–45.
Haro JM, Arbabzadeh-Bouchez S, Brugha TS, De Girolamo G, Guyer ME, Jin R, et al. Concordance of the Composite International Diagnostic interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health surveys. Int J Methods Psychiatr Res. 2008;17(Suppl 14):78–82.
Kim JM, Stewart R, Shin IS, Yoon JS, Lee HY. Lifetime urban/rural residence, social support and late-life depression in Korea. Int J Geriatr Psychiatry. 2004;19(9):843–51.
Yiengprugsawan V, Caldwell BK, Lim LLY, Seubsman SA, Sleigh AC. Lifecourse urbanization, social demography, and health outcomes among a national cohort of 71,516 adults in Thailand. Int J Popul Res. 2011;2011:1–9.
Sharma P, Maurya P, Muhammad T. Number of chronic conditions and associated functional limitations among older adults: cross-sectional findings from the longitudinal aging study in India. BMC Geriatr. 2021;21(1):1–12.
Zacharias A, Vakulabharanam V. Caste stratification and wealth inequality in India. World Development. 2011;39(10):1820–33.
Hou B, Nazroo J, Banks J, Marshall A. Impacts of migration on health and well-being in later life in China: evidence from the China Health and Retirement Longitudinal Study (CHARLS). Health Place. 2019;58:102073.
Fontanella CA, Hiance-Steelesmith DL, Phillips GS, Bridge JA, Lester N, Sweeney HA, et al. Widening rural-urban disparities in youth suicides, United States, 1996–2010. JAMA Pediatr. 2015;169(5):466–73.
Jukes MCH, Zuilkowski SS, Grigorenko EL. Do schooling and urban residence develop cognitive skills at the expense of social responsibility? A study of adolescents in the Gambia, West Africa. J Cross-Cult Psychol. 2018;49(1):82–98.
Nugroho TW, Hanani N, Toiba H, Sujarwo S. Promoting subjective well-being among rural and urban residents in Indonesia. Does social capital matter? Sustainability. 2022;14(4):2375.
Vogelsang EM. Older adult social participation and its relationship with health: rural-urban differences. Health Place. 2016;42:111–9.
Lee J, Smith JP. Regional disparities in adult height, educational attainment, and late-life cognition: findings from the longitudinal aging study in India (LASI). J Econ Ageing. 2014;4:26–34.
Lee J, Shih R, Feeney K, Langa KM. Gender disparity in late-life cognitive functioning in India: findings from the longitudinal aging study in India. J Gerontol B Psychol Sci Soc Sci. 2014;69(4):603–11.
Muhammad T, Meher T. Association of late-life depression with cognitive impairment: evidence from a cross-sectional study among older adults in India. BMC Geriatr. 2021;21(1):1–13.
Shidhaye R, Patel V. Association of socio-economic, gender and health factors with common mental disorders in women: a population-based study of 5703 married rural women in India. Int J Epidemiol. 2010;39(6):1510–21.
Purtle J, Nelson KL, Yang Y, Langellier B, Stankov I, Diez Roux AV. Urban-rural differences in older adult depression: a systematic review and meta-analysis of comparative studies. Am J Prev Med. 2019;56(4):603–13.
Zhang J, Nazroo J, Zhang N. Gender differences in rural-urban migration and its impact on depression in later life. Health Place. 2022;77: 102890.
Adjaye-Gbewonyo D, Rebok GW, Gallo JJ, Gross AL, Underwood CR. Residence in urban and rural areas over the life course and depression among Ghanaian and South African older adults. Health Place. 2020;63: 102349.
DiNapoli EA, Wu B, Scogin F. Social isolation and cognitive function in Appalachian older adults. Res Aging. 2014;36(2):161–79.
Perkins JM, Nyakato VN, Kakuhikire B, Tsai AC, Subramanian SV, Bangsberg DR, et al. Food insecurity, social networks and symptoms of depression among men and women in rural Uganda: a cross-sectional, population-based study. Public Health Nutr. 2018;21(5):838–48.
Xu H, Vorderstrasse AA, Dupre ME, McConnell ES, Østbye T, Wu B. Gender differences in the association between migration and cognitive function among older adults in China and India. Arch Gerontol Geriatr. 2019;81:31–8.
Chiswick BR, Lee YL, Miller PW. Immigrant selection systems and immigrant health. Contemp Econ Policy. 2008;26(4):555–78.
Lu Y, Qin L. Healthy migrant and salmon bias hypotheses: a study of health and internal migration in China. Soc Sci Med. 2014;102:41–8.
Li J, Rose N. Urban social exclusion and mental health of China’s rural-urban migrants–a review and call for research. Health Place. 2017;48:20–30.
Marmot M. Social determinants of health inequalities. The lancet. 2005;365(9464):1099–104.
Irwin A, Valentine N, Brown C, Loewenson R, Solar O, Brown H, et al. The commission on social determinants of health: tackling the social roots of health inequities. PLoS Med. 2006;3(6):0749–51.
Aliberti MJR, Bertola L, Szlejf C, Oliveira D, Piovezan RD, Cesari M, et al. Validating intrinsic capacity to measure healthy aging in an upper middle-income country: findings from the ELSI-Brazil. Lancet Reg Health Am. 2022;12:100284.
Muneera K, Muhammad T, Althaf S. Socio-demographic and lifestyle factors associated with intrinsic capacity among older adults: evidence from India. BMC Geriatr. 2022;22(1):1–16.
Kley S. Explaining the stages of migration within a life-course framework. Eur Sociol Rev. 2011;27(4):469–86.
Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186(1):125–45.
Geist C, McManus PA. Geographical mobility over the life course: motivations and implications. Popul Space Place. 2008;14(4):283–303.
Yang L, Cheng J, Wang H. Place of residence and cognitive function in older adults in China: the mediating role of social participation. Int J Environ Res Public Health. 2021;19(1): 13.
Sun J, Lyu S. Social participation and urban-rural disparity in mental health among older adults in China. J Affect Disord. 2020;274:399–404.
Saenz JL, Downer B, Garcia MA, Wong R. Cognition and context: rural–urban differences in cognitive aging among older Mexican adults. J Aging Health. 2018;30(6):965–86.
Lederbogen F, Kirsch P, Haddad L, Streit F, Tost H, Schuch P, et al. City living and urban upbringing affect neural social stress processing in humans. Nature. 2011;474(7352):498–501.
Xu H, Luo J, Wu B. Self-reported diabetes treatment among chinese middle-aged and older adults with diabetes: comparison of urban residents, migrants in urban settings, and rural residents. Int J Nurs Sci. 2015;2(1):9–14.
Zhong BL, Liu TB, Huang JX, Fung HH, Chan SS, Conwell Y, et al. Acculturative stress of chinese rural-to-urban migrant workers: a qualitative study. PLoS One. 2016;11(6):e0157530.
Chen J. Chronic conditions and receipt of treatment among urbanized rural residents in China. BioMed Res Int. 2013;2013:568959.
Saenz JL, Downer B, Garcia MA, Wong R. Rural/urban dwelling across the life-course and late-life cognitive ability in Mexico. SSM Popul Health. 2022;17:101031.
Kalaria RN, Maestre GE, Arizaga R, Friedland RP, Galasko D, Hall K, et al. Alzheimer’s disease and vascular dementia in developing countries: prevalence, management, and risk factors. Lancet Neurol. 2008;7(9):812–26.
Hill TD, Angel JL, Balistreri KS, Herrera AP. Immigrant status and cognitive functioning in late-life: an examination of gender variations in the healthy immigrant effect. Soc Sci Med. 2012;75(12):2076–84.
Zahodne LB, Schofield PW, Farrell MT, Stern Y, Manly JJ. Bilingualism does not alter cognitive decline or dementia risk among spanish-speaking immigrants. Neuropsychology. 2014;28(2):238.
Nguyen MH, La VP, Le TT, Vuong QH. Introduction to Bayesian Mindsponge Framework analytics: an innovative method for social and psychological research. MethodsX. 2022;9:101808.
Kumar M, Srivastava S, Muhammad T, Saravanakumar P. Examining the association between health status and subjective life expectancy among older indian adults based on the mindsponge approach. Humanit Soc Sci Commun. 2022;9(1):1–10.
Acknowledgements
“The Longitudinal Aging Study in India Project is funded by the Ministry of Health and Family Welfare, Government of India, the National Institute on Aging (R01 AG042778, R01 AG030153), and United Nations Population Fund, India.“
Funding
The analysis received no funding.
Author information
Authors and Affiliations
Contributions
T. Muhammad conceived and designed the research, performed statistical analysis, drafted the manuscript, and made critical revisions of the manuscript for key intellectual content. The author read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Indian Council of Medical Research (ICMR) Ethics Committee in January 2017 and written or oral informed consent was obtained from the participants or their guardians. All methods were carried out in accordance with relevant guidelines and regulations and in accordance with the World Medical Association Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1a and b.
The receiver operating characteristic (ROC) curves with respective area under the curve (AUC). Figure S2a and b. Plots of residuals against fitted values (close to zero variation of mean of the residuals (y-axis) against fitted values (x-axis) of predictors suggests no violation of linearity). Figure S3a and b. Quantile-quantile plots showing the normality of the residuals. Table S1. VIF estimates for the selected explanatory variables.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Muhammad, T. Life course rural/urban place of residence, depressive symptoms and cognitive impairment among older adults: findings from the Longitudinal Aging Study in India. BMC Psychiatry 23, 391 (2023). https://doi.org/10.1186/s12888-023-04911-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-023-04911-9