Abstract
Background
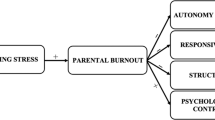
Parental burnout has become increasingly common, which can lead to a range of adverse outcomes. Postnatal mothers are vulnerable and mothers with high postpartum depression scores may be more prone to parental burnout. This study aims to investigate the association between postnatal depressive symptoms and parental burnout at both the population and individual levels.
Methods
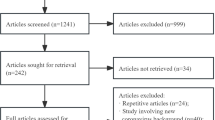
This study comprised a cross-sectional study design and participants were recruited using convenience sampling. A total of 560 postnatal mothers answered a questionnaire on their general information, postnatal depressive symptoms and parental burnout. Multiple linear regression and binary logistic regression analysis were used to examine the association between postnatal depressive symptoms and parental burnout. Furthermore, latent class analysis was used to identify subtypes of parental burnout. Finally, binary logistic regression was used to examine the differences in postnatal depressive symptoms between latent classes comprising parental burnout.
Results
The prevalence of burnout was approximately 10%. At the population level, postnatal depressive symptoms were positively associated with parental burnout (all P < 0.05). At the individual level, two latent classes were identified (i.e., “low parental burnout class” and “high parental burnout class”). Moreover, mothers with postnatal depressive symptoms were more likely to be associated with high parental burnout (PB) class than the low parental burnout class (OR = 1.12, 95% CI:1.03 to 1.23).
Conclusion
This study found a positive relationship between postnatal depressive symptoms and parental burnout. It provided evidence for developing depression-targeted programs for parental burnout, which could bring great benefits for both mothers and infants.
Similar content being viewed by others
Introduction
While parenthood is a joyful event, it places pressure on mothers and may even lead to parental burnout. Parental burnout is common. It is estimated that approximately 20% of mothers experiences parental burnout [1]. The adverse effects of parental burnout are considerable. It may not only bring about addictive behaviours, sleep problems, and suicidal ideation in mothers themselves, but also may damage couple relationships and increase the risk of maladaptive parenting behaviour (e.g., neglect, violence) [2].
Postnatal mothers are vulnerable for parental burnout. This may result from special challenges during this period [3]. For example, the increasing psychosomatic discomforts during postnatal period, substantial acute (e.g., infant’s illness, falls) and chronic parenting stressors (e.g., difficult infant temperament) from infants [4]. Therefore, it is necessary to consider parental burnout among postnatal mothers.
Among the influencing factors mentioned above, maternal postnatal depressive symptoms could be an important factor. The severity and specialty of postnatal depression have been recognized worldwide. In China, 14.8% of mothers suffer from postnatal depression [5]. Postnatal depression not only affects the mother’s social and occupational functioning [6], but also interferes with the mother-infant relationship and impairs the cognitive, behavioral, and social-emotional development of the offspring[7]. Considering the adverse effects of postnatal depression [8], timely and early treatment of maternal depression is important to protect the health of the mother and offspring(e.g. electroconvulsive therapy) [9], and studies have found that if left untreated it can lead to poorer parenting behaviors and thereby increased parental burnout [10]. Limited studies have underscored the relationship between maternal depressive symptoms and parental burnout [1, 11,12,13]. However, previous studies mostly focused on mothers with older children. Exploring the association between postnatal depressive symptoms and parental burnout during one year postpartum could provide evidence for developing depression-targeted programs for parental burnout, which could bring great benefits for both mothers and infants. In addition, previous studies used non-specialized parental burnout measures, like BMI-10 [14], to measure parental burnout, which may lead to inexact estimation about the severity of parental burnout and further bias the association between depression symptoms and parental burnout [1, 12, 13]. Furthermore, a few recent studies have indicated the heterogeneity of parental burnout [15, 16]. For example, Lebert-Charron et al. identified five clusters based on parental burnout symptoms in French mothers [15]. The results further showed that affective variables (e.g., anxiety, depressive symptoms, and burden) differed between the clusters. However, this study only used ANOVA for comparisons between clusters, which ignored the effect of confounding factors.
Ignoring individual heterogeneity may hinder the ability to distinguish between groups with different characteristics in a population. Latent Class Analysis (LCA) is a person-centered analysis method that determines the potential characteristics of individuals for classification based on their classification on dimensions of scale, identifies groups with different characteristics in the population, maximizes the differences between groups, minimizes the differences within groups, and allows the accuracy and validity of the classification to be assessed using objective fit indicators [17]. The categories recognized by mothers are based on the level of manifestations of parental burnout at the individual level. Thus, clinicians are able to identify mothers experiencing significant challenges, promote specific primary prevention, and advise on targeted therapeutic interventions for parental burnout [15]. This study aimed to investigate the association between postnatal depressive symptoms and parental burnout at both the population and individual levels.
Methods
This study comprised a cross-sectional study design. Using a convenience sampling, participants were recruited from a pediatric health clinic at a tertiary care hospital in Jinan, China, between October 2020 and October 2021.
Participants
The inclusion criteria were as follows: (1) within a year postpartum, (2) age ≥ 18 years at the time of conception, (3) natural pregnancy, (4) singleton pregnancy, (5) full-term delivery, (6) normal verbal communication and comprehension skills, as well as ability to read and complete the questionnaire correctly. Patients with (1) severe psychiatric disorders, (2) severe physical diseases, or (3) a baby diagnosed with a congenital or severe disease were excluded from the study.
Sample size caculation
In the multiple linear regression, the expected effect size (f2) was taken as a medium effect size of 0.15, the statistical efficacy was taken as 90%, the significance level was set at 0.05, and the estimated number of predictor variables was 13. In G*power, the minimum sample size required for the calculation was 164. Considering a null response rate of approximately 20%, the minimum sample size required was 208. Empirically, a minimum of 300 cases was required to identify the optimal number of potential class models [18], and considering a null response rate of approximately 20%, the minimum sample size required was 375. In summary, the minimum required sample size was 375.
Measures
Parental burnout assessment (PBA)
The PBA was used to measure the level of parental burnout [19]. The scale contains 23 items and has four dimensions, namely, exhaustion in parenting, contrast with the previous parental self, feelings of being fed up, and emotional distancing. Responses were obtained on a 7-Point Likert scale ranging from 1 (never) to 7 (every day). Higher scores indicated higher levels of parental burnout. The scale has been validated to have good reliability and validity [19], and the Cronbach’s α in this study was 0.95.
Edinburgh postnatal depression scale (EPDS)
The EPDS was developed and revised by Cox et al. [20]. The scale contains 10 items. Each item was scored from 0 to 3. Higher summed scores indicated increased severity of postnatal depression. The EPDS has been widely used and has good reliability and validity [21]. The Cronbach’s α in this study was 0.86.
Covariates
The self-administered general information questionnaire includes the maternal age, infant’s age, maternal education level, marital status, average monthly family income, family residence, current work status, parity, difficulty in breastfeeding, and perceived parenting support from elders. Previous studies have shown that infants with self-regulation problems (e.g., sleep problems and crying) may be more likely to suffer from poor maternal-infant relationships, which might be associated with parental burnout [22]. Therefore, this study further adjusted for the difficult infant temperament. Difficult infant temperament was measured using the Parenting Stress Index-Short Form subscale (Difficult Child Temperament) [23]. The subscale is self-reported by the assessor and has a total of 5 items. Each item is scored on a 5-point Likert scale, with 1 indicating strong disagreement and 5 indicating strong agreement. The higher the total score of the items summed, the higher the degree of parenting difficulties of the offspring. The scale has been validated to have good reliability and validity [23], and the Cronbach’α in this study was 0.91.
Statistical analyses
Statistical analyses were conducted using IBM SPSS software (v26.0) and Mplus 8. Frequencies and percentages were calculated for the categorical variables. Means and standard deviations were used to summarize continuous variables. Prior to conducting a multiple linear regression, a Pearson correlation analysis was performed to explore the relationship between postnatal depressive symptoms and parental burnout. Multiple linear regression was conducted to examine the association between postnatal depressive symptoms and the four dimensions of parental burnout after controlling for covariates.
This study was interested in examining the types of naturally occurring latent classes of parental burnout indicators that could be identified. Latent class analyses for different latent groups were conducted and the fit indices and class frequencies were compared. The variances were estimated to be equal between the classes. The estimation was performed step-by-step, starting from a one-class solution to estimate the parameters for 2, 3, …, k-class solutions. The solution that best fitted the data in accordance with the indicators, and that was deemed reasonable in terms of interpretation was chosen as the final latent class model. The model fitting indexes included the Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), Adjusted Bayesian Information Criteria (aBIC), Lo-Mendell-Rubin test (LMR), Bootstrap Likelihood Ratio Test (BLRT), and entropy. Binary logistic regression analysis was used to explore the differences between the latent classes of parental burnout in terms of postnatal depressive symptoms. In the sensitivity analysis, the scores of the four dimensions of parental burnout were dichotomized to further explore the robustness of the relationship between postnatal depressive symptoms and parental burnout using a binary logistic regression. As there was no definite cut-off value for the four dimensions of parental burnout, the mean plus 1.5 standard deviations was considered positive [24]. Statistical significance was set at two-sided, with a p-value of < 0.05.
Results
Characteristics of mothers in the study
In total, 583 mothers responded to the survey. Among them, mothers who did not answer key variables (postnatal depressive symptoms and parental burnout) were excluded, and 560 participants were finally included in the analysis.
The mean age of women was 30.8 ± 4.8 years and the mean age of these infants was 9.0 ± 3.2 months; the mean score for maternal postnatal depressive symptoms was 9.4 ± 5.0. The scores and symptom prevalence rates for the four dimensions of parental burnout are shown in Table 1. Pearson’s correlation analysis revealed a positive correlation between postnatal depressive symptoms and exhaustion in parenting (r = 0.495, p < 0.001) and contrast (r = 0.434, p < 0.001), and feelings of being fed up (r = 0.358, p < 0.001) and distance (r = 0.348, p < 0.001).
Associations between postnatal depressive symptoms and parental burnout
As shown in Table 2, postnatal depressive symptoms are positively associated with the four dimensions of parental burnout (all p < 0.05) after controlling for covariates. The results of the sensitivity analysis also indicated that postnatal depressive symptoms were associated with different dimensions of parental burnout (See Supplementary Table 2).
Latent categories of parental burnout and comparison of different categories
As shown in Table 3, a comparison of the fit indices and class frequencies showed that the model fit indices were the worst when the number of latent classes was set to 1 (zero models). When a second group was included in the analyses, the BIC, aBIC, and AIC slightly decreased and the entropy value slightly increased compared to the three profile solutions, and the class sizes were acceptable. The p-values of LMR and BLRT of the two-category model were significant, indicating that the two-category model was better than the one-category model. In the three-category model, the p-value of LMR of the three-category model was not significant, indicating that the three-category model was not superior to the two-category model. Therefore, because the two-category model was theoretically meaningful, and the goodness-of-fit indices indicated that the second latent group was necessary, the two-latent-group solution was considered the best model. The mean probability of attribution for each latent class ranges from 0.988 to 0.998, indicating that this classification is plausible.
The first latent class, 90% of the mothers, was characterized by a low level of all parental burnout components. The second latent class (10% of the parents) was characterized by a relatively high level of all parental burnout components. The latent classes were labeled low parental burnout (i.e., low PB) and high parental burnout (i.e., high PB). High PB scores were higher than low PB scores in all dimensions (See Table 4; Fig. 1).
The binary logistic regression model showed that postnatal depressive symptoms were an influential factor for the different subtypes of parental burnout (OR = 1.15, 95% CI:1.09 ~ 1.22, p < 0.001, Model 1). This result remained significant after controlling for confounding factors (OR = 1.12, 95% CI: 1.03 ~ 1.23, p = 0.011, Model 2) (See Supplementary Table 1).
Discussion
Parental burnout is attracting the attention of researchers because of its pervasive consequences. To the best of our knowledge, this study is the first to focus on one of the vulnerable groups, postnatal women. This study found that the prevalence of the four burnout dimensions was 9.5% (exhaustion in parenting), 9.1% (contrast with previous parental self), 9.3% (feelings of being fed up), and 9.3% (emotional distancing). Additionally, the relationships between postnatal depressive symptoms and each dimension of parental burnout at both population and individual levels were examined using multiple methods.
At the population level, postnatal depressive symptoms were positively associated with all dimensions of parental burnout, which was also verified by sensitivity analysis. This finding was consistent with previous results drawn from studies of mothers raising older children [1, 13], which also found a close association between postnatal depressive symptoms and parental burnout.
First, the association was analyzed from the individual perspective by using person-oriented research (LCA), making it possible to identify distinct homogenous classes of mothers who suffer from parental burnout. Two categories were found, namely, the low PB class, characterized by a low level of all components of parental burnout, and the high PB class, characterized by a relatively high level of all components of parental burnout. These results are partially consistent with previous research showing that approximately 85.7% of Finnish parents reported low scores on different dimensions of parental burnout and 8% reported high scores on three dimensions of parental burnout, except for a low level of emotional distancing. Furthermore, a third profile was characterized by a high level of emotional distancing from one’s children and an average level of parental exhaustion, in contrast with the previous self, and feelings of fed up were computed [16]. These differences may be because the study was conducted in Finnish on parental burnout among fathers and mothers, whereas the present study focused only on parental burnout in postpartum mothers. The study results suggest that parental burnout symptoms manifest differently among postpartum mothers, and that mothers in the high parental burnout group had higher depression scores than those in the low parental burnout group. A person-centered approach facilitates the identification of individual differences for individualized interventions.
The results of this study suggest a close association among postnatal women. It may be because the postpartum period refers to a specific period in a mother’s life that can increase the risk of mental health problems [8]. Mothers with high postpartum depression scores are in an unstable mental state and may be prone to negative emotions, such as self-denial, when dealing with parenting-related issues. Furthermore, they are reluctant to solve child-related problems, stay away from their children both psychologically and behaviorally, and are more prone to parenting burnout. This study indicated that the postpartum period should be a sensitive window for intervention because of the high prevalence of maternal depression and burnout at this stage. Their close relationship suggests that postnatal depressive symptoms may be an indicator of parental burnout. Therefore, mothers with postnatal depressive symptoms should be closely screened for parental burnout. Intervention programs targeting postnatal depressive symptoms are promising because they may be effective in improving parental burnout and, therefore, bring great benefits.
Despite these potentials and values, this study still has some limitations. First, postnatal depressive symptoms and parental burnout in the study were collected through a self-assessment questionnaire, it may be subject to recall bias and social desirability bias. In addition, mothers included in this study were mainly recruited from a tertiary hospital in one city (Jinan, Shandong Province), mostly lived in the city and were well-educated, which limited the generalizability of the findings. In addition, this study was a cross-sectional study and cannot disclose the causal relationship between postpartum depressive symptoms and parental burnout in mothers.
Conclusion
In this study, the prevalence of parental burnout in the first year postpartum is approximately 10%. The postnatal depressive symptoms were positively associated with parental burnout, and this association is consistent at both individual and population levels. These results suggest that decreasing postnatal depression symptoms may be a possible way to prevent parental burnout in postnatal mothers. Some intervention programs such as meditation and cognitive behavioral therapy [25, 26], have been proven to be effective in reducing postnatal depressive symptoms. Based on our results, those with parental burnout may also benefit from these available intervention programs for postnatal depression. Further studies are needed to examine this assumption.
Data Availability
The datasets generated and/or analysed during the current study are not publicly available due maternal privacy implications but are available from the corresponding author on reasonable request.
References
Séjourné N, Sanchez-Rodriguez R, Leboullenger A, Callahan S. Maternal burn-out: an exploratory study. J Reprod Infant Psychol. 2018;36(3):276–88.
Mikolajczak M, Brianda ME, Avalosse H, Roskam I. Consequences of parental burnout: its specific effect on child neglect and violence. Child Abuse Negl. 2018;80:134–45.
Pearlstein T, Howard M, Salisbury A, Zlotnick C. Postpartum depression. Am J Obstet Gynecol. 2009;200(4):357–64.
Matvienko-Sikar K, Murphy G, Murphy M. The role of prenatal, obstetric, and post-partum factors in the parenting stress of mothers and fathers of 9-month old infants. J Psychosom Obstet Gynaecol. 2018;39(1):47–55.
Nisar A, Yin J, Waqas A, Bai X, Wang D, Rahman A, Li X. Prevalence of perinatal depression and its determinants in Mainland China: a systematic review and meta-analysis. J Affect Disord. 2020;277:1022–37.
Jones I, Shakespeare J. Postnatal Depress BMJ. 2014;349:g4500.
Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, Howard LM, Pariante CM. Effects of perinatal mental disorders on the fetus and child. Lancet. 2014;384(9956):1800–19.
Bydlowski M. Transparence psychique de la grossesse et dette de vie. Hors Collect. 2004;1(3):39–68.
Bulbul F, Copoglu US, Alpak G, Unal A, Demir B, Tastan MF, Savas HA. Electroconvulsive therapy in pregnant patients. Gen Hosp Psychiatry. 2013;35(6):636–9.
Rueger SY, Katz RL, Risser HJ, Lovejoy MC. Relations between parental affect and parenting behaviors: a meta-analytic review. Parent Sci Pract. 2011;11(1):1–33.
Astrid LC, Géraldine D, Emilie B, Jaqueline W. Maternal burnout syndrome: contextual and psychological Associated factors. Front Psychol. 2018;9:885.
Sánchez-Rodríguez R, Orsini É, Laflaquière E, Callahan S, Séjourné N. Depression, anxiety, and guilt in mothers with burnout of preschool and school-aged children: insight from a cluster analysis. J Affect Disord. 2019;259:244–50.
Séjourné N, Sanchez-Rodriguez R, Leboullenger A, Callahan S. Maternal burn-out: an exploratory study. J Reprod Infant Psychol, 2018: p. 1.
Malach-Pines A. The burnout measure, short version. Int J Stress Manag. 2005;12(1):78.
Lebert-Charron A, Dorard G, Wendland J, Boujut E. Who are and are not the burnout moms? A cluster analysis study of french-speaking mothers. J Affect Disord Rep, 2021.
Upadyaya K, Salmela-Aro K. Latent profiles of parental burnout during COVID-19: the role of child-related perceptions. Front Psychol, 2021: p. 3740.
Lazarsfeld PF, Henry NW. Latent Struct Anal Am Sociol Rev, 1968. 34(2).
Nylund-Gibson K, Garber AC, Carter DB, Chan M, Arch DAN, Simon O, Whaling K, Tartt E, Lawrie SI. Ten frequently asked questions about latent transition analysis. Psychol Methods, 2022.
Roskam I, Brianda ME, Mikolajczak M. A Step Forward in the conceptualization and measurement of parental burnout: the parental Burnout Assessment (PBA). Front Psychol. 2018;9:758.
Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry. 1987;150(6):782–6.
Levis B, Negeri Z, Sun Y, Benedetti A, Thombs BD. Accuracy of the Edinburgh postnatal depression scale (EPDS) for screening to detect major depression among pregnant and postpartum women: systematic review and meta-analysis of individual participant data. BMJ, 2020. 371.
Davies SM, Silverio SA, Christiansen P, Fallon V. Maternal-infant bonding and perceptions of infant temperament: the mediating role of maternal mental health. J Affect Disord. 2021;282:1323–9.
Luo J, Wang MC, Gao Y, Zeng H, Yang W, Chen W, Zhao S, Qi S. Refining the parenting stress index-short form (PSI-SF) in chinese parents. Assessment. 2021;28(2):551–66.
Goitein M. Nonstandard deviations. Medical physics, 1983. 10(5): p. 709–11.
Milgrom J, Danaher BG, Seeley JR, Holt CJ, Holt C, Ericksen J, Tyler MS, Gau JM, Gemmill AW. Internet and face-to-face cognitive behavioral therapy for postnatal Depression compared with treatment as Usual: Randomized Controlled Trial of MumMoodBooster. J Med Internet Res. 2021;23(12):e17185.
Dimidjian S, Goodman SH, Felder JN, Gallop R, Brown AP, Beck A. Staying well during pregnancy and the postpartum: a pilot randomized trial of mindfulness-based cognitive therapy for the prevention of depressive relapse/recurrence. J Consult Clin Psychol. 2016;84(2):134–45.
Acknowledgements
We would like to acknowledge the maternities who participated in this study.
Funding
This work was supported by the National Natural Science Foundation of China [Grant Number: 32071084, Grant Recipient: Fenglin Cao].
Author information
Authors and Affiliations
Contributions
Yongqi Huang: conceptualization, writing original draft; writing-review & editing, formal analysis validation. Fangxiang Mao: conceptualization, writing original draft; writing-review & editing. Xuan zhang: conceptualization, methodology, validation. Juan Wang: conceptualization, methodology, validation. Zhaojuan Xu: methodology. Fenglin Cao: conceptualization, project administration, resources, supervision, validation, writing review& editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the College of Nursing and Rehabilitation, Shandong University(2020-R-25), all methods were carried out in accordance with relevant guidelines and regulations in the Declaration of Helsinki, and all participants signed an informed consent form.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Huang, Y., Mao, F., Zhang, X. et al. Exploring the relationship between postnatal depressive symptoms and parental burnout from the perspective of the population and individual level. BMC Psychiatry 23, 409 (2023). https://doi.org/10.1186/s12888-023-04853-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-023-04853-2