Abstract
Background
Although hospitalization can be a burdensome experience for all patients, research into the sources of this distress and potential protective factors has so far been scattered, specifically among the broad hospitalized population across all disease types and inpatient units. The present study explores the frequency and nature of the foremost experienced hassles among a sample of Lebanese hospitalized patients, tracing their correlations with depression and anxiety while also investigating positive coping (i.e., perceived social support and spiritual well-being) as potential moderator of these relationships.
Methods
A total of 452 Lebanese inpatients from all medical units filled a survey composed of a list of 38 stressors experienced during hospitalization and other measures assessing depression, anxiety, perceived social support, and spiritual well-being.
Results
Pain was the most common stressor experienced by the patients (88.9%), followed by the feeling of being overwhelmed (80.3%). When conducting a factor analysis, 18 stressors loaded on 4 distinct factors, hence yielding 4 main stressor groups (i.e., Illness Apprehension, Hopelessness/Uselessness, Social Isolation, and Spiritual Concerns). The multivariable analysis showed that increased illness apprehension (Beta = 0.69) and hopelessness (Beta = 1.37), being married (Beta = 1.17) or divorced (Beta = 1.38) compared to single, being admitted in a two-bed room compared to one-bed (Beta = 1.59), higher financial burden (Beta = 0.24), and lower socio-economic status (Beta = 1.60) were significantly associated with higher anxiety. Additionally, increased hopelessness (Beta = 0.82) and being married (Beta = 0.79) compared to single were significantly associated with higher depression. However, among patients experiencing high levels of stressors, those with high spiritual well-being and perceived social support had lower depressive/anxiety symptoms.
Conclusion
Our study characterized the principal stressors encountered during hospitalization, underscoring their associations with Lebanese inpatients’ mental health. On the other hand, as perceived social support and spiritual well-being acted as negative moderators of these associations, intervention programs aimed at enhancing such adaptive coping techniques are strongly called upon to palliate the psychological distress of patients in hospital settings.
Similar content being viewed by others
Introduction
Hospitalization is often accompanied by high levels of distress, which can engender considerable psychiatric comorbidities; worsen disease severity and patient disability; prolong hospital stays; and heighten hospital’s cost, burden, and rates of readmission [1,2,3,4]. Numerous investigations have indeed highlighted the intractable impact of hospitalization on the development of depressive and anxiety symptoms. For instance, a meta-analysis of 31 studies estimated that the prevalence of depression among general medical and surgical hospital inpatients ranges between 5% and 34%, with an average rate of 12% [5]. Likewise, another meta-analysis of 32 studies calculated prevalence estimates of 3%, 5%, 8%, and 28% for panic disorders, generalized anxiety disorders, anxiety disorders (all types), and anxiety symptoms among general hospital inpatients, respectively [6].
In return, it is noteworthy that positive psychology/psychiatry interventions (PPIs), a subset of psychosocial interventions, have shown promising benefits in alleviating such distress in medical patients [7]. Nonetheless, most of the previous analyses of depressive/anxiety symptoms and their predicting variables in the hospital context have focused on specific inpatients populations, namely cardiac/cardiovascular patients [8, 9], surgical patients [10,11,12], high-risk obstetrical patients [13], patients with Human Immunodeficiency Virus (HIV) [14], or patients with chronic diseases [15] such as diabetes mellitus [16] or malignancy [17, 18].
For example, within the Lebanese population, a previous study found high levels of depression, anxiety, and stress (21.3%, 61.3%, and 48.7%, respectively) among hospitalized patients with chronic illnesses, showing that avoidant coping styles, comorbidities, educational level, and female gender were significantly associated with higher ratings on psychological distress [15]. Another Lebanese study discovered a very high rate of anxiety (61.4%) among inpatients with substance use disorders, with better educated people experiencing less severe symptoms [19]. Furthermore, an investigation of suicidal risk among Lebanese psychiatric inpatients revealed that 37.5% tested positive for acute suicidal ideation; however, high spiritual well-being was significantly associated with lower suicidality in this specific inpatient population [20].
Nonetheless, to our best knowledge, only one precedent study has attempted to portray the sources of hospital discomfort and how they relate to anxiety among a heterogenous hospital-wide sample of inpatients from the United States [21]; nonetheless, it did neither address depressive symptoms nor explore factors that might have lessened the negative effects of hospital’s stressors on mental health. Consequently, owing to a scarcity of studies scrutinizing the reasons behind hospitalization-related depression and anxiety among the broad medical inpatient, it has been somewhat challenging to tailor treatment interventions and maximize their effectiveness among this general, though vulnerable, population [7].
Actually, bolstering positive mental states, cognitions, emotions, attitudes, and behaviors through a systematic execution of intentional exercises is what PPIs call for [22]; they require patients to conduct activities in their everyday life, which can be either clinician-led or self-guided, to self-build positive resources and happy experiences and so improve well-being. Thus, they do not just work towards assuaging psychological distress, which make them surpass traditional psychological therapeutic approaches (e.g., cognitive-behavioral therapy) [22]. As a result, PPIs can be widely applied in healthcare settings to aid in the prevention and treatment of depressive/anxiety symptoms and promote general well-being when dealing with diseases, as they are generally applicable to patients with and without psychopathology [7, 22,23,24,25]. Namely, thankfulness, seeking hope/faith and purpose in life (e.g., feeling good spiritually), fostering positive connections (e.g., feeling socially supported), kindness, or simply savoring are common themes pertaining to positive psychology [26]. However, while patients with somatic illnesses may strongly benefit from enhancements in their well-being through PPIs [27], to the best of our knowledge, no study has inquired about how positive psychology components, such as perceived social support and spiritual well-being, can modulate mental distress among hospitalized inpatients.
In sum, although hospitalization can be a burdensome experience for all patients, research into the sources of this distress and potential protective factors has so far been scattered, specifically among the general hospitalized population across all disease types and residing in all inpatient units. Moreover, treatment and support programs for depression and anxiety in the hospital have surprisingly been overlooked and/or underdeveloped, owing primarily to the paucity of research aimed at comprehending the emotional and environmental factors that trigger or assuage hospital-related psychological distress [7]. To this end, this works aims to (1) suggest a protective role for certain factors that would be negatively associated with mental distress among Lebanese inpatients, and thus, (2) preliminarily allude to potential therapeutic targets in the management of hospital-specific distress and associated mental disorders within Lebanese hospitals. Considering that this public health issue has received the least attention in developing countries, such contribution in Lebanon—a Middle-Eastern developing country—could enlighten the path towards implementing efficient PPIs and national mental health supporting policies for inpatients.
Therefore, in the present study, our objective was to explore the frequency and nature of the foremost experienced hassles among a sample of Lebanese hospitalized patients, tracing their correlations with depression and anxiety while also investigating positive coping/psychological adaptation (i.e., perceived social support and spiritual well-being) as potential moderator of these relationships. For exploratory purposes, we also evaluated the moderating effects of comorbidities and sociodemographic characteristics, such as age, gender, and the socio-economic status, in the relationships between stressors and mental health problems, relying on previous work highlighting the associations between these factors and mental health problems in hospitalized patients [15, 21, 28,29,30].
Methods
Study design
From November 2021 through January 2022, 452 Lebanese inpatients, distributed in all the inpatient medical units of a university hospital (i.e., The Centre Hospitalier Universitaire Notre Dame de Secours located in Byblos, Lebanon), took part in our cross-sectional survey. Eligibility was defined by being aged 18 years or over and able to read the Arabic language, whereas exclusion criteria were cognitive impairment, unconsciousness/unresponsiveness, and isolation. These exclusion criteria were assessed by looking at the medical records of the patients. At the start of each day within this period, the hospital records were reviewed, and all newly admitted eligible inpatients were approached and invited to participate. In total, 452 out of the 550 eligible hospitalized patients participated in the survey; the response rate was 82.2%, as 98 patients refused to participate. All the participants could access the Google Forms survey’s link via their smartphones, in order to answer the survey questions on their own. Participation was voluntary and anonymous. The study’s objectives were intelligibly stated in the introductory section of the survey, and patients had to read the instructions and consent to participate (by answering “yes”) before proceeding to the next sections.
Minimal sample size calculation
The G*power 3.1.9.7 software (linear multiple regression: fixed model, R2 increase) [31] showed that a minimal sample of 395 inpatients was necessary to achieve satisfactory statistical power, when accepting a 5% risk of error, a 80% power, a small 2% effect size (f2) (as categorized by Cohen [32]), and 10 variables in the multivariable model.
Questionnaire and variables
The questionnaires were administered in Arabic, Lebanon’s native language. The needed time for completion was 15 min. The first sections gathered data about socio-demographic characteristics, namely patient’s age, gender, marital status, educational level (i.e., primary, complementary, secondary, or university level), and experienced financial burden (rated from 1 to 10). The overall socioeconomic status of the participants was also appraised by the household crowding index, a measure that computes the ratio of the total number of people over the total number of rooms in the house except the bathrooms and kitchen. Higher ratios are indicative of lower socioeconomic households [33]. Questions tackling insurance type (i.e., private, national security, Lebanese army, and public health ministry), room type (i.e., one-bed or two-bed room), and general comorbidities (i.e., cardiovascular disease, hypertension, diabetes, chronic kidney disease, neurological disease, and psychiatric illness) were also included.
Additionally, based on a previous study scrutinizing stressors that correlated with anxiety symptoms among a general hospitalized population [21], we included a list of 38 potential stressors (displayed in Table 1). The endorsement of these stressors was categorized into Yes or No, after asking the patients if each particular stress factor was a source of burden during the current hospitalization (i.e., exclusively while in the hospital). The other parts of the survey comprised:
The patient health questionnaire (PHQ-9)
This brief 9-item tool is greatly efficacious to detect depression among clinical samples. Each item (e.g., “Little interest or pleasure in doing things” and “Feeling down, depressed, or hopeless”) is scored from 0 (i.e., “not at all”) to 3 (i.e., “nearly every day”), quantifying symptoms’ severity [34]. This scale was validated in Arabic among the Lebanese population [35]. (Cronbach’s alpha in this study = 0.88)
The lebanese anxiety scale (LAS-10)
This scale is a brief tool to screen for anxiety, composed of 10 items that were derived from the diagnostic criteria retained in the DSM-5, HAM-A, and STAI measures for anxiety. For instance, items include “I have an anxious mood (worries, anticipation of the worst, fearful anticipation, irritability)” and “I feel that difficulties are piling up so that I cannot overcome them”. Increased scores represent an escalation of anxiety symptoms. This scale was intentionally conceived and validated to depict anxiety among the Lebanese population [36, 37]. (Cronbach’s alpha in this study = 0.93)
The multidimensional scale of perceived social support (MSPSS)
This short 12-item instrument gauges self-perceptions of social support that comes from family, friends, and a significant person. It consists of three subscales, and each comprises 4 items. Items, which include “My family really tries to help me”, “I can count on my friends when things go wrong”, and “There is a special person in my life who cares about my feelings”, are rated from 1 (i.e., “strongly disagree”) to 7 (i.e., “strongly agree”) [38]. Higher scores denote a greater perceived social support. This measure was also validated in Lebanon [39]. (Cronbach’s alpha in this study = 0.96)
The functional assessment of chronic illness therapy 12-item spiritual well-being scale (FACIT-Sp-12)
This tool detains 3 subscales that assess faith, meaning of life, and peace (e.g., “I find comfort in my faith or spiritual beliefs”, “I feel a sense of purpose in my life”, and “I feel peaceful”). Response options range from “not at all” (scored as 0) to “very much” (scored as 4). The greater the total score, the higher the spiritual well-being [40]. (Cronbach’s alpha in this study = 0.89)
Statistical analysis
To explore the factor structure of the 38 stressors, we computed a factor analysis using the FACTOR software [41, 42]. We verified all requirements related to item-communality [43], average item correlations, and item-total correlations [44]. The Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy (which should ideally be ≥ 0.80) and Bartlett’s test of sphericity (which should be significant) ensured the adequacy of our sample [45]. The procedure for determining the number of factors to extract was parallel analysis (PA) [46], using the polychoric correlation matrix. We used the robust diagonally weight least squares to extract the factors and the weighted varimax for the rotation start. The rotation to achieve factor simplicity was done using the robust promin.
The SPSS software v.25 was used to conduct the remaining analyses. Anxiety and depression scores were normally distributed. The Student t and ANOVA tests were used to compared two and three or more means, respectively. Pearson test was used to correlate two scores. Two linear regressions were then conducted, taking the anxiety and depression scores as dependent variables, respectively. The absence of multicollinearity was verified through the calculation of the Variance Inflation Factor (VIF); VIF values < 5 indicate the absence of multicollinearity [47]. Moderation models were analyzed using the PROCESS macro v.3.4 model 1 [48]. Factors that showed a p < 0.25 were taken as independent variables in the model. Significance was set at p < 0.05.
Results
Sociodemographic and other characteristics of the participants
A total of 452 patients filled the survey (mean age: 47.60 years; 52.7% females). Details related to the marital status, education, insurance coverage, comorbidities, and other characteristics of the patients can be found in Table 2.
Prevalence of each stressor
Pain was the most common stressor experienced by the patients (88.9%), followed by the feeling of being overwhelmed (80.3%). The prevalence rates of the other stressors are summarized in Table 1.
Factor analysis of the stressors
All stressors were entered in the factor analysis; all items with a factor loading > 0.4, a communality < 0.3 and a normed MSA > 0.5 were removed; 18 stressors remained at the end and loaded on four factors (F1: Illness Apprehension; F2: Hopelessness/Uselessness; F3: Social Abandonment; and F4: Spiritual Concerns), which explained 75.31% of the total variance. The Cronbach’s alpha of the four factors were excellent (Table 3).
Bivariate analysis taking anxiety and depression as dependent variables
Higher anxiety was significantly associated with increased depression, all stressor groups (i.e., illness apprehension, hopelessness, social isolation, and spiritual concerns), higher financial burden, and higher household crowding index (i.e., lower socio-economic status). It was also associated with lower perceived social support and spiritual well-being. Higher depression was significantly associated with the same variables as anxiety, except the household crowding index (no significant association found) (Table 4). In addition, higher mean anxiety/depression scores were found in widowed participants compared to the other categories, in those with a primary level of education compared to the other categories, in those who do not have private insurance, in those who were admitted in a two-bed room compared to one bed, and in those who have cardiovascular problems, diabetes, neurological and psychiatric diseases compared to not. Moreover, higher anxiety scores were significantly found in patients who have hypertension compared to not (Table 5).
Multivariable analysis taking anxiety and depression as dependent variables
The results of the multivariable analysis, taking anxiety as the dependent variable, showed that higher spiritual well-being (Beta=-0.43) was significantly associated with lower anxiety, whereas increased illness apprehension (Beta = 0.69) and hopelessness (Beta = 1.37), being married (Beta = 1.17) or divorced (Beta = 1.38) compared to single, being admitted to a two-bed room compared to one bed (Beta = 1.59), higher financial burden (Beta = 0.24), and higher household crowding index (i.e., lower socio-economic status) (Beta = 1.60) were significantly associated with higher anxiety (Table 6, Model 1).
The results of the multivariable analysis, taking depression as the dependent variable, showed that higher spiritual well-being (Beta=-0.29) was significantly associated with lower depression, whereas increased hopelessness (Beta = 0.82) and being married (Beta = 0.79) compared to single were significantly associated with higher depression (Table 6, Model 2).
Moderators between stressors and depression/anxiety
The results of the moderation analysis are summarized in Table 7. The interactions illness apprehension by perceived social support/age were significantly associated with anxiety; in patients with high illness apprehension, having high perceived social support (Fig. 1) and older age (Fig. 2) were significantly associated with lower anxiety.
The interactions illness apprehension by age were significantly associated with depression; in patients with high illness apprehension, younger age (Fig. 3) was significantly associated with lower depression.
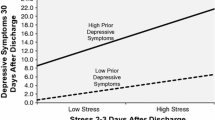
The interactions hopelessness by spiritual wellbeing/household crowding index were significantly associated with depression; in patients with high hopelessness, having high spiritual wellbeing (Fig. 4) and a high household crowding index (lower socioeconomic status) (Fig. 5) were significantly associated with lower depression.
The interaction social isolation by spiritual wellbeing was significantly associated with anxiety; in patients with high social isolation, having high spiritual wellbeing was significantly associated with lower anxiety (Fig. 6).
The interactions spiritual concerns by perceived social support/spiritual wellbeing were significantly associated with anxiety; in patients with high spiritual concerns, having high perceived social support (Fig. 7) and high spiritual well-being (Fig. 8) were significantly associated with lower anxiety.
The interactions spiritual concerns by perceived social support/age/household crowding index were significantly associated with depression; in patients with high spiritual concerns, having high perceived social support (Fig. 9), younger age (Fig. 10) and high household crowding index (lower socioeconomic status) (Fig. 11) were significantly associated with lower depression.
Discussion
Within this study, pain was the most endorsed stressor by the participants, in line with several previous studies reporting a high prevalence of pain in hospitalized patients [21, 49, 50]. The factor analysis identified four multi-item factors measuring stressors among our hospitalized sample, which were related to the following themes: illness apprehension/fear, hopelessness/usefulness, social isolation, and spiritual concerns. In fact, illness-related fear and uncertainty in illness (i.e., illness apprehension) are well-established concerns in the healthcare setting, which may also exert detrimental impacts on patients’ mental health and quality of life [8, 21, 51]. Further, in line with our results, a meta-analysis found that lung cancer patients expressed illness-associated emotional experiences related to fear, worries, uncertainties, despair, uselessness, dependency, and loneliness [52]. In addition, being away from family members (i.e., social isolation) has also been identified as a potent source of post-surgical anxiety [9]. Our findings are also consistent with prior research indicating high levels of depression/anxiety among hospitalized patients who had the need to speak to a spiritual advisor, feel more supported by their relatives, and feel less abandoned [53]. Actually, spiritual distress and suffering related to lack of meaning in life (i.e., hopelessness and spiritual concerns) are common struggles identified in medical disease patients [21], such as cancer patients undergoing chemotherapy [54].
Furthermore, our study showed that patients who felt hopeless and useless during hospitalization had higher symptoms of depression and anxiety. Similarly to our results, McKenzie et al. showed that pessimism and worthlessness were highly correlated with major depression among hospitalized, medically ill patients [55]. Additionally, in line with previous research [21, 51, 56], patients with high illness apprehension displayed a significantly greater level of anxiety. Our study thus extends the results of prior research conducted among general and specific subgroups of inpatients, suggesting their relevance among all Lebanese inpatients regardless of disease type and severity.
On another hand, our results indicated that being married/divorced compared to single was significantly associated with higher scores of anxiety. In addition, married participants had higher levels of depression compared to single inpatients, in line with prior research among patients diagnosed with oral cancer [57]. Our findings thus speculate that single patients might be less prone to depressive/anxiety symptoms in the hospital context since they do not have additional responsibilities to a partner or child/children. Moreover, patients with lower socio-economic status and higher financial burden exhibited higher anxiety symptoms in our population. Similarly, low income and being unemployed were found to be among the prime factors associated with psychological distress among hospitalized patients with diabetes mellitus in Saudi Arabic and cancer patients attending follow-up in Ethiopia, respectively [16, 58]. Certainly, patients who find it difficult to afford the costs of their treatment and hospitalization would be more susceptible to anxiety, fearing the progress of their disease if they could not obtain the necessary care. In line with this perspective, patients residing in a two-bed room compared to one-bed were more vulnerable to anxiety. The latter association may also be related to the socio-economic status of the patients who cannot afford a private hospital room. From another standpoint, those patients’ anxiety might result from hearing the burdens and complaints of their hospital roommates or from witnessing a bad course of their disease.
In contrast, our findings revealed that greater spiritual well-being was significantly associated with lower depression and anxiety symptoms. Moreover, in patients experiencing high levels of stressors, those with high spiritual well-being and perceived social support had less depressive/anxiety symptoms. Consistent with our findings, a previous study showed that patients with serious and advanced diseases who had greater spiritual well-being as measured by the FACIT-Sp; including beliefs about the role of faith in illness and meaning, peace, and purpose in life; were considerably less depressed and anxious [59]. Another study observed that perceived social support was related to a better quality of life in oral cancer patients in China [60]. These observations may have paramount clinical implications for implementing targeted interventions (i.e., enhancing social support and promoting spiritual well-being) to alleviate in-hospital depression and anxiety across all medical units.
Concerning the moderating roles of sociodemographic characteristics, a lower socioeconomic status had a negative moderating effect in the association between stressors (hopelessness and spiritual concerns) and depression. This finding implies that people from lower socioeconomic backgrounds may face more difficulties and thus develop coping strategies and resilience to stress [61, 62], which may contribute to a lower susceptibility to depressive symptoms in response to emotional stressors the hospital. Finally, our study found that the associations between stressors and depression were weaker in younger people, whereas older people had lower anxiety in response to stressors. In line with our results, a prospective longitudinal study on cancer patients found that anxiety declines with age while depression rises [30]. Another study also demonstrated that older patients had more depressive symptoms post-stroke [63]. In light of our findings, we cautiously suggest that programs to reduce anxiety in younger patients are required, while more resources and attention should be directed towards identifying and treating depression in older hospitalized patients.
Clinical implications
This study is important for broadening physicians’ understanding of a wide range of stressors experienced by general hospitalized patients, as many of which may be present at subclinical levels and hence go unnoticed for effective psychological/psychiatric assessment and management. Understanding the factors that are favorably and adversely linked with their depressed and anxiety symptoms, in order to create efficient screening programs and clinical preventive/therapeutic interventions, could help to improve the hospital experience for all patients. Precisely, our study prompts hospital-wide interventions in Lebanon, who would work towards developing strong social support networks for inpatients (e.g., extending hospitals’ visiting hours, encouraging patients’ communication with their family/entourage, family counseling, etc.). Further, our results provided a tool to identify inpatients who need support, and highlighted the need of promoting their spiritual well-being; hence, they might benefit the hospital personnel (i.e., hospital chaplains) who operate through all hospital units.
Limitations
Despite its important contribution to the literature tackling the psychological well-being of Lebanese hospitalized patients, the current study is not devoid of certain limitations. First, its cross-sectional nature allows to only capture a snapshot in time, hence hindering the ability to establish causal and temporal associations. Second, the symptoms were self-reported; although anonymous self-report surveys limit social undesirability, patients might misunderstand some statements. Third, we recruited the patients from a single hospital, which limits the generalizability of our results to the whole Lebanese population. Fourth, by studying moderators, this study provided a deeper comprehensive analytical approach to the relationships between stressors in the hospital and mental health outcomes; nevertheless, we found a very high negative correlation between anxiety and spiritual well-being in our sample (i.e., -0.8), which means that higher spiritual well-being was very closely linked to lower anxiety in our population. This high correlation might have also significantly influenced the moderation analysis. Finally, not all possible confounding factors were examined in the present study. For instance, our study did not consider the time of stay in the hospital, the hospital admission frequency, or the medications used as independent variables, which might have affected the outcomes. Further research with a wider range of predictors are highly encouraged to complement our results.
Conclusion
Our study characterized the principal stressors encountered during hospitalization, underscoring their associations with Lebanese inpatients’ mental health. On the other hand, as perceived social support and spiritual well-being acted as negative moderators of these associations, intervention programs aimed at enhancing such adaptive coping techniques are strongly called upon to palliate the psychological distress of patients in hospital settings. Future prospective studies are needed to deepen our insights into the variety of biopsychosocial factors eliciting distress across the wide hospital inpatient population, and their mitigating counter-force, in order to enact preventive/therapeutic interventions that would benefit a large number of patients.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to restrictions from the ethics committee, but are available from the corresponding author on reasonable request.
References
Katon W, Lin MD, Elizabeth HB, Kroenke MDMPH. The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. Gen Hosp Psychiatry. 2007;29(2):147–55. https://doi.org/10.1016/j.genhosppsych.2006.11.005.
Roy-Byrne PP, Davidson MD, Kessler KWPhD. Anxiety disorders and comorbid medical illness. Gen Hosp Psychiatry. 2008;30(3):208–25. https://doi.org/10.1016/j.genhosppsych.2007.12.006.
Nikayin S, Rabiee MD, Hashem AMD. Anxiety symptoms in survivors of critical illness: a systematic review and Meta-analysis. Gen Hosp Psychiatry. 2016;43:23–9. https://doi.org/10.1016/j.genhosppsych.2016.08.005.
Beeler PE, Cheetham M, Held U, Battegay E. Depression is independently associated with increased length of stay and readmissions in multimorbid inpatients. Eur J Intern Med. 2020;73:59–66.
Walker J, Burke K, Wanat M, et al. The prevalence of depression in general hospital inpatients: a systematic review and meta-analysis of interview-based studies. Psychol Med. 2018;48(14):2285–98.
Walker J, van Niekerk M, Hobbs H, et al. The prevalence of anxiety in general hospital inpatients: a systematic review and meta-analysis. Gen Hosp Psychiatry. 2021;72:131–40.
Brown L, Ospina JP, Celano CM, Huffman JC. The Effects of positive psychological interventions on medical patients’ anxiety: a Meta-analysis. Psychosom Med. 2019;81(7):595–602. https://doi.org/10.1097/PSY.0000000000000722.
Giammanco MD, Gitto L. Coping, uncertainty and health-related quality of life as determinants of anxiety and depression on a sample of hospitalized cardiac patients in Southern Italy. Qual Life Res. 2016;25(11):2941–56.
Nesami MB, Shorofi SA, Jafari A, Khalilian AR, Tabari SZ. The relationship between stressors and anxiety levels after CABG in Sari, Iran. Iran Red Crescent Med J 2016;18(5)
Brown SM. Quantitative measurement of anxiety in patients undergoing surgery for renal calculus disease. J Adv Nurs. 1990;15(8):962–70.
Karanci AN, Dirik G. Predictors of pre-and postoperative anxiety in emergency surgery patients. J Psychosom Res. 2003;55(4):363–9.
Johnston M. Anxiety in surgical patients. Psychol Med. 1980;10(1):145–52.
Byatt, Nancy DO, Hicks-Courant MBAFAPM, Davidson KBA. Depression and anxiety among high-risk obstetric inpatients. Gen Hosp Psychiatry. 2014;36(6):644–9. https://doi.org/10.1016/j.genhosppsych.2014.07.011.
Tesfaw G, Ayano G, Awoke T, et al. Prevalence and correlates of depression and anxiety among patients with HIV on-follow up at Alert Hospital, Addis Ababa, Ethiopia. BMC Psychiatry. 2016;16(1):1–7.
Fattouh N, Hallit S, Salameh P, Choueiry G, Kazour F, Hallit R. Prevalence and factors affecting the level of depression, anxiety, and stress in hospitalized patients with a chronic disease. Perspect Psychiatr Care. 2019;55(4):592–9.
AlBekairy A, AbuRuz S, Alsabani B, et al. Exploring factors associated with depression and anxiety among hospitalized patients with type 2 diabetes mellitus. Med Principles Pract. 2017;26(6):547–53.
van den Brekel L, van der Baan FH, Zweers D, et al. Predicting anxiety in hospitalized cancer patients. J Pain Symptom Manage. 2020;60(3):522–30. e1.
Park EM, Gelber S, Rosenberg SM, et al. Anxiety and depression in young women with metastatic breast cancer: a cross-sectional study. Psychosomatics. 2018;59(3):251–8.
Haddad C, Darwich MJ, Obeid S, et al. Factors associated with anxiety disorders among patients with substance use disorders in Lebanon: results of a cross-sectional study. Perspect Psychiatr Care. 2020;56(4):745–52. https://doi.org/10.1111/ppc.12462.
Kassem M, Haddad C, Hallit S, Kazour F. Impact of spirituality and religiosity on suicidal risk among a sample of lebanese psychiatric in-patients. Int J psychiatry Clin Pract. 2021;25(4):336–43. https://doi.org/10.1080/13651501.2020.1787453.
Palmer PK, Wehrmeyer K, Florian MP, Raison C, Idler E, Mascaro JS. The prevalence, grouping, and distribution of stressors and their association with anxiety among hospitalized patients. PLoS ONE. 2021;16(12):e0260921.
Seligman ME, Steen TA, Park N, Peterson C. Positive psychology progress: empirical validation of interventions. Am Psychol. 2005;60(5):410.
Chakhssi F, Kraiss JT, Sommers-Spijkerman M, Bohlmeijer ET. The effect of positive psychology interventions on well-being and distress in clinical samples with psychiatric or somatic disorders: a systematic review and meta-analysis. BMC Psychiatry. 2018;18(1):1–17.
Chaves C, Lopez-Gomez I, Hervas G, Vazquez C. A comparative study on the efficacy of a positive psychology intervention and a cognitive behavioral therapy for clinical depression. Cogn therapy Res. 2017;41(3):417–33.
Sin NL, Lyubomirsky S. Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: a practice‐friendly meta‐analysis. J Clin Psychol. 2009;65(5):467–87.
Schueller SM, Parks AC. The science of self-help: translating positive psychology research into increased individual happiness. Eur Psychol. 2014;19(2):145.
De Ridder D, Geenen R, Kuijer R, van Middendorp H. Psychological adjustment to chronic disease. The Lancet. 2008;372(9634):246–55.
Patel RS, Shrestha S, Saeed H et al. Comorbidities and consequences in hospitalized heart failure patients with depression. Cureus 2018;10(8)
McCusker J, Cole M, Dufouil C, et al. The prevalence and correlates of major and minor depression in older medical inpatients. J Am Geriatr Soc. 2005;53(8):1344–53.
Weiss Wiesel TR, Nelson CJ, Tew WP, et al. The relationship between age, anxiety, and depression in older adults with cancer. Psycho-oncology (Chichester England). 2015;24(6):712–7. https://doi.org/10.1002/pon.3638.
Faul F, Erdfelder E, Buchner A, Lang A. Statistical power analyses using GPower 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–60. https://doi.org/10.3758/BRM.41.4.1149.
Cohen J. Statistical power analysis for the behavioral sciences 2nd edition ed. L. Erlbaum Associates: Hillsdale, NJ, USA; 1988.
Melki IS, Beydoun HA, Khogali M, Tamim H, Yunis KA. Household crowding index: a correlate of socioeconomic status and inter-pregnancy spacing in an urban setting. J Epidemiol Commun Health. 2004;58:476–80. https://doi.org/10.1136/jech.2003.012690.
Kroenke K, Spitzer RL, Williams JBW. The PHQ-9. J GEN INTERN MED. 2001;16(9):606–13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
Sawaya H, Atoui M, Hamadeh A, Zeinoun P, Nahas Z. Adaptation and initial validation of the Patient Health Questionnaire – 9 (PHQ-9) and the generalized anxiety disorder – 7 questionnaire (GAD-7) in an arabic speaking lebanese psychiatric outpatient sample. Psychiatry Res. 2016;239:245–52. https://doi.org/10.1016/j.psychres.2016.03.030.
Hallit S, Obeid S, Haddad C, et al. Construction of the lebanese anxiety scale (LAS-10): a new scale to assess anxiety in adult patients. Int J psychiatry Clin Pract. 2020;24(3):270–7. https://doi.org/10.1080/13651501.2020.1744662.
Merhy G, Azzi V, Salameh P, Obeid S, Hallit S. Anxiety among Lebanese adolescents: scale validation and correlates. BMC Pediatr. 2021 Jun 22;21(1):288. https://doi.org/10.1186/s12887-021-02763-4.
Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional Scale of Perceived Social Support. J Pers Assess. 1988;52(1):30–41. https://doi.org/10.1207/s15327752jpa5201_2.
Fekih-Romdhane F, Fawaz M, Hallit R, Sawma T, Obeid S, Hallit S. Psychometric Properties of an Arabic Translation of the Multidimensional Social Support Scale (MSPSS) in a community sample of Lebanese Adults. In Review, preprint, Nov. 2022. https://doi.org/10.21203/rs.3.rs-1983450/v1.
Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy—spiritual well-being scale (FACIT-Sp). Ann Behav Med. 2002;24(1):49–58.
Lorenzo-Seva U, Ten Berge JM. Tucker’s congruence coefficient as a meaningful index of factor similarity. Methodology: Eur J Res Methods Behav Social Sci. 2006;2(2):57.
Lorenzo-Seva U, Ferrando PJ. Evaluating structural equation models with unobservable variables and measurement error. Behav Res Methods Instrum Comput. 2006;38(1):88–91.
Worthington RL, Whittaker TA. Scale development research: a content analysis and recommendations for best practices. Couns Psychol. 2006;34(6):806–38.
Clark LA, Watson D. Construct validity: basic issues in objective scale development. Psychol Meas. 1995;28:61–75.
Hair JF. Multivariate data analysis. 2009.
Timmerman ME, Lorenzo-Seva U. Dimensionality assessment of ordered polytomous items with parallel analysis. Psychol Methods. 2011;16(2):209.
Gareth J, Daniela W, Trevor H, Robert T. An introduction to statistical learning: with applications in R Spinger; 2013.
Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. Guilford publications; 2017.
Whelan CT, Jin L, Meltzer D. Pain and satisfaction with pain control in hospitalized medical patients: no such thing as low risk. Arch Intern Med. 2004;164(2):175–80.
Conway Morris A, Howie N. Pain in medical inpatients: an under-recognised problem? J Royal Coll Physicians Edinb. 2009;39(4):292–5. https://doi.org/10.4997/JRCPE.2009.401.
Stewart KE, Hart PhD, Gibson RPPhD, Psy DP, Fisher D. Illness apprehension, Depression, anxiety, and quality of life in liver transplant candidates: implications for psychosocial interventions. Psychosom (Washington D C). 2014;55(6):650–8. https://doi.org/10.1016/j.psym.2013.10.002.
Refsgaard B, Frederiksen K. Illness-related emotional experiences of patients living with Incurable Lung Cancer: a qualitative metasynthesis. Cancer Nurs. 2013;36(3):221–8. https://doi.org/10.1097/NCC.0b013e318268f983.
Rosselli M, Salimbeni MV, Bessi C, et al. Screening of distress among hospitalized patients in a department of internal medicine. Asian J psychiatry. 2015;18:91–6. https://doi.org/10.1016/j.ajp.2015.08.003.
Caldeira S, Timmins F, de Carvalho EC, Vieira M. Clinical validation of the nursing diagnosis spiritual distress in Cancer Patients undergoing chemotherapy. Int J Nurs Knowl. 2017;28(1):44–52. https://doi.org/10.1111/2047-3095.12105.
McKenzie DP, Clarke PhD, Forbes DMPhDFRANZCP, Sim ABPhD, Pessimism MRPhDFAFOMFFOM. Worthlessness, Anhedonia, and thoughts of death identify DSM–IV Major Depression in Hospitalized, medically ill patients. Psychosom (Washington D C). 2011;51(4):302–11. https://doi.org/10.1016/S0033-3182(10)70701-5.
Sehlo MG, Mohamed WS, Youssef UM, Lotfi SE, El-deen GMS. Prevalence and determinants of anxiety in patients with epilepsy during COVID-19 pandemic. Egypt J Neurol Psychiatry Neurosurg. 2022;58(1):78. https://doi.org/10.1186/s41983-022-00513-6.
Yuan L, Pan B, Wang W, Wang L, Zhang X, Gao Y. Prevalence and predictors of anxiety and depressive symptoms among patients diagnosed with oral cancer in China: a cross-sectional study. BMC Psychiatry. 2020;20(1):394. https://doi.org/10.1186/s12888-020-02796-6.
Ayalew M, Deribe B, Duko B, et al. Prevalence of depression and anxiety symptoms and their determinant factors among patients with cancer in southern Ethiopia: a cross-sectional study. BMJ open. 2022;12(1):e051317.
Johnson KS, Tulsky JA, Hays JC, et al. Which domains of spirituality are Associated with anxiety and depression in patients with Advanced Illness? J GEN INTERN MED. 2011;26(7):751–8. https://doi.org/10.1007/s11606-011-1656-2.
Zhang Y, Cui C, Wang Y, Wang L. Effects of stigma, hope and social support on quality of life among chinese patients diagnosed with oral cancer: a cross-sectional study. Health Qual Life Outcomes. 2020;18(1):1–8.
Perzow SED, Bray BC, Wadsworth ME. Financial stress response profiles and psychosocial functioning in low-income parents. J Fam Psychol. 2018;32(4):517–27. https://doi.org/10.1037/fam0000403.
Goldstein E, Benton S, Barrett B. Health Risk Behaviors and Resilience among Low-Income, Black Primary Care Patients: qualitative findings from a trauma-informed primary care intervention study. Fam Community Health. 2020;43(3):187–99. https://doi.org/10.1097/FCH.0000000000000260.
Sadlonova M, Wasser K, Nagel J, et al. Health-related quality of life, anxiety and depression up to 12 months post-stroke: influence of sex, age, stroke severity and atrial fibrillation – a longitudinal subanalysis of the Find-AFRANDOMISED trial. J Psychosom Res. 2021;142:110353. https://doi.org/10.1016/j.jpsychores.2020.110353.
Acknowledgements
The authors would like to thank all the patients who helped them during this study as well as Dr Urbano Lorenzo Seva for his help in the analysis.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study design. SH conducted the statistical analysis and interpreted the results. SG collected the data and wrote the manuscript. All authors reviewed the manuscript and gave their consent.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study’s protocol was approved by the Psychiatric Hospital of the Cross Ethics Committee (HPC-042-2021). Informed consent was obtained from all study participants when submitting the form online. All methods were carried out in accordance with relevant guidelines and regulations.
Competing interests
No conflicts of interest.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gerges, S., Hallit, R. & Hallit, S. Stressors in hospitalized patients and their associations with mental health outcomes: testing perceived social support and spiritual well-being as moderators. BMC Psychiatry 23, 323 (2023). https://doi.org/10.1186/s12888-023-04833-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-023-04833-6