Abstract
Background
The COVID-19 pandemic has placed an unprecedented physical and mental burden on healthcare workers who are frequently at high risk of infection, particularly in low-income countries. This study aimed to assess the prevalence and associated factors of anxiety, depression, and stress, as well as changes in daily and occupational activities among healthcare professionals due to the COVID-19 pandemic in Colombia.
Methods
An observational, cross-sectional study was conducted between February and June 2021. The survey incorporated validated mental health tools such as the Generalized Anxiety Disorder–7, the Patient Health Questionnaire-9, and the Perceived Stress Scale-10. Multivariable ordinal logistic regression analysis was performed to determine the factors associated with severe mental health outcomes.
Results
Among 1345 healthcare workers the prevalence of anxiety, depression, and stress were 75.61, 59.18, and 53.09%, respectively. Anxiety (OR:1.44; 95%CI:1.16–1.8), depression (OR:1.74; 95%CI:1.27–2.37), and stress (OR:1.51; 95%CI:1.18–1.94) were more frequent in women, and individuals who expressed fear of a negative outcome (death, sequelae) (OR:2.25; 95%CI:1.60–3.25), (OR:1.49; 95%CI:1.03–2.16) and (OR:2.36; 95%CI:1.69–3.29) respectively. Age was negatively associated with anxiety (OR:0.98; 95%CI:0.98–0.99), stress (OR:0.98; 95%CI:0.97–0.99), and depression (OR:0.97; 95% CI:0.96–0.98). Reduction in consultations and surgeries (OR:1.01; 95%CI:1.0–1.01) was positively associated with anxiety. Due to the pandemic, most specialists expected to incorporate drastic long-term (> 1 year) changes in their clinical setting and daily activities.
Conclusions
The prevalence of anxiety, depression, and stress is higher among Colombian healthcare workers compared to previous reports. Further research regarding these psychological outcomes is needed to achieve early mental health intervention strategies.
Trial registration
Hospital Universitario Fundación Santa Fe, Ethical Committee Registration ID: CCEI-12992-2021.
Similar content being viewed by others
Background
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) as the causative agent of COVID-19 has rapidly spread worldwide, drastically disrupting healthcare systems and placing an unprecedented burden on healthcare professionals. By December 2021, the World Health Organization (WHO) has reported over 240 million confirmed cases and nearly 5 million deaths throughout the different waves of the disease, multiple mutations of the virus, and significant differences in clinical patterns and outcomes [1, 2]. In Colombia, up to 6 million cases of COVID-19 and over 133 thousand deaths have been registered, ranking the country as the 11th hardest hit in terms of mortality rate. Although control measures to contain the spread of the disease have been applied and over 6 billion vaccines have now been administered globally, new strains are emerging. During previous severe acute respiratory syndrome outbreaks, disproportionate infection rates among healthcare workers resulting in long-term adverse psychological and occupational outcomes had been reported [3, 4].
Since the spread of COVID-19, Vizheh et al. stated that healthcare specialists reported higher occupational stress levels and higher rates of psychological symptoms [5]. These outcomes could be related to excessive workload, inadequate support, a critical shortage of personal protective equipment, hospital beds, and ventilators [3, 6]. On a more personal level, the restrictions implemented to contain and reduce the risk of infection impacted the regular daily and leisure activities which may also lead to an increased risk of anxiety, depression, burnout syndrome and stigma in healthcare workers [7]. Several studies conducted during the COVID-19 pandemic have reported a decline in mental wellbeing among health care professionals [3, 5, 6]. From June to September 2020, Mental Health America (MHA) applied a survey to describe their experience and reported that 93% of health care workers were experiencing stress, 86% reported anxiety, and 76% reported exhaustion and burnout [8]. Being worried about exposing their child was reported by 76% of participants, and nearly half of them expressed fear of infecting a partner or older adult family member, while 39% of reported inadequate emotional support [8]. In 2021 a systematic review reported the results of 24 studies predominantly from urban China indicating that COVID-19 had a considerable impact on the psychological wellbeing of front-line hospital staff and suggested that nurses may be at higher risk of adverse mental health outcomes [9]. Likewise, in a meta-analysis performed in 2021 with 38 studies, Saragih et al. reported that anxiety, depression, and distress presented a significant rise in healthcare workers during the 2020 COVID-19 pandemic with a pooled prevalence of 40% (95% CI: 29–52%), 37% (95% CI: 29–45%), and 37% (95% CI: 25–50%), respectively [10].
These studies highlight the importance of mental wellness in physicians during times of crisis, yet further studies are needed to capture a broader picture of the situation to efficiently manage future sanitary emergencies and thus prevent long-term impact on front-line staff. To date, very few studies have been published in English regarding these psychological outcomes in Latin America. Regarding the Colombian population, one study reported the effects of the pandemic on the mental health, daily and occupational activities of otolaryngologists, and allergists [11]. A cross-sectional study reported figures that range of 50% for any type of altered mental state [12] and approximately 72% of anxiety symptoms in Colombian physicians [13]. Despite some international studies have performed these analyses using internationally validated questionnaires [14], few studies have applied these tools in Latin American countries. This study aimed to describe the prevalence and associated factors of depression, anxiety, stress, and the changes in daily and occupational activities among Colombian healthcare professionals during the second wave of the COVID-19 pandemic.
Methods
Study design
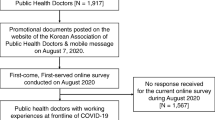
An observational, cross-sectional study was conducted to determine the prevalence and associated factors of anxiety, depression, and stress levels in a group of healthcare professionals during the second wave of the COVID-19 pandemic in Colombia. The study was based on a non-probabilistic, consecutive sampling, using self-administered, anonymous online surveys to collect sociodemographic and mental health data from February 05, 2021, to June 30, 2021. Internationally validated questionnaires such as the Generalized Anxiety Disorder-7 (GAD7), the Patient Health Questionnaire-9 (PHQ9), and the Perceived Stress Scale-10 (PSS10) were used to determine the frequency of anxiety, depression, and stress, respectively. A sociodemographic questionnaire was also applied and assessed information about age, marital status, family income, working status, workload, work income before and after the pandemic, personal protective equipment, and geographic location. Data collection was performed online, and participants were invited to fill out the survey at any time. Ethics Committee of the Hospital Universitario Fundación Santa Fe de Bogotá approved this study (CCEI-12992-2021) according to the Helsinki Declaration, and all methods were performed in accordance with the relevant guidelines and ethic regulations. Moreover, this study was approved and involved the participation of the National Academy of Medicine from Colombia in the dissemination plans of this research. Informed Consent was obtained from all participants. No incentives were offered for study participation.
Study population
In terms of the eligibility criteria, healthcare workers registered in the National Unified Registry of Human Resources in Health from Colombia and conducted in-person consultations and/or telemedicine were included. Exclusion criteria were specialists who reported a prior diagnosis of mental health disorders confirmed by a psychiatrist or mental health professional, and those who reported any acute/chronic condition that could limit their ability to answer the questionnaires. The sample size was estimated based on a meta-analysis by Pappa et al. that assessed the prevalence of mental health disorders among 33,062 healthcare workers due to the COVID-19 pandemic [15]. A minimum sample size of 250 participants was calculated considering a pooled prevalence of depression of 22.8%, bearing in mind the following formula [16]:
A 5% significance and precision level were applied, as well as a 5% adjustment for probable losses. Regarding the sample selection method, a non-probabilistic, consecutive sampling was conducted. Despite the participants registered to do the survey, only the population who completed all the questionnaires was included in the analysis.
Mental health questionnaires
Symptoms of anxiety, depression, and stress were assessed using validated Spanish versions of the following measurement tools: GAD-7 [17], PHQ-9 [18], and PSS-10 [19]. The GAD-7 scale was used to assess symptoms of anxiety over the past 2 weeks, ranging from 0 to 21 points as follows: normal (0–4), mild (5–9), moderate (10–14), and severe (15–21) anxiety (23). The cutoff point for identifying General Anxiety Disorder was a score of 10 in the GAD-7 questionnaire [17]. The PHQ-9 assesses depression symptoms and includes 9 criteria of the Diagnostic and Statistical Manual of Mental Disorders [18]. Each item is scored from 0 (not at all) to 3 (nearly every day) according to the level of discomfort of the patient [18]. The PHQ-9 ranges between 0 to 27 and can be classified as follows: none (0–4), mild (5–9), moderate (10–14), moderately severe (15–19), severe (20–27). A total score of ≥10 in the PHQ-9 has a sensitivity and a specificity of 88% for major depression [18]. The PSS-10 questionnaire contains 10 items that measure the perception of stressful experiences over the past month. Responses range from 0 (never) to 4 (very often), and the total score can be classified as follows: low stress (0–13), moderate stress (14–26), and high perceived stress (27–40) [20]. For this study, the severity of the symptoms of anxiety, depression, and stress was classified considering the cutoff values of the GAD-7, PHQ-9, and PSS-10 scales.
Variables related to COVID-19 and daily activities questionnaires
A “Fear score of COVID-19” developed by the researchers of this study was applied using a scale of 1 to 5 to assess fear of contagion, fear of the possibility of a negative outcome (death, negative sequelae), and fear of infecting a family member and/or friends. Moreover, a questionnaire regarding the opinion on when (less than 3 months, in 3 to 12 months, more than 1 year, never again) healthcare workers would expect to engage again in regular daily and leisure activities was applied. This questionnaire was developed by “The New York Times” and previously applied to 511 epidemiologists [21]. We highlight that their answers only reflect their opinion and individual life circumstances and should not be used as guidelines for the public.
Statistical analysis
Frequencies and percentages were calculated for the quantitative variables. Central tendency, and dispersion measures for the quantitative variables were estimated. The prevalence of symptoms of anxiety, depression, and stress was calculated along with its 95% confidence interval. Bivariate and multivariate analyses were carried out to explore the associations between the levels of anxiety, depression and stress and the sociodemographic and occupational covariates due to the COVID-19 pandemic. These analyses were based on an ordinal logistic regression analysis. The predictors of the model were selected considering the biological plausibility reported by prior studies as primary criteria, and the possible statistical association within the variables. Variables with clinical relevance first, or those with a Fisher or Kruskall Wallis test with a p-value ≤0.2 were included in the multivariate analysis. The full, crude, and adjusted models are reported to compare the strength of the associations with depression and to assess the presence of confounding variables in the analysis. Percentage decrease in monthly income was calculated comparing income before the pandemic and during the fieldwork (October–November 2020). Finally, the goodness of fit of the model was assessed and assumptions were verified through a linearity test, proportional odds, and through the estimation of deviance residuals and leverage values. Statistical significance for the multivariate models was established at p < 0.05. Statistical analysis was performed using Stata 16MP software. A 5% significance level for the comparisons was established before data collection.
Results
A total of 1345 individuals were included in this study, of which 39.26% were over the age of 50, 66.17% (n = 840) were women, and 46.10% (n = 620) were specialist doctors. The baseline demographic characteristics of the study population are described in Table 1. Most of the sample was based in urban Colombia, i.e., Bogotá (n = 663), Antioquia (n = 118), 66% of the participants were women, and nearly 40% were over the age of 50. Near half of the study population (49,44%) performed face-to-face consultation, while 25.58% worked as telemedicine practitioners. Overall, 19.03% (n = 256) of the study population considered that the personal protection elements provided by their employer were not enough to prevent COVID-19 infection. The most frequently used biosafety elements in their practice were surgical masks with 32.94% (n = 443), and N95 respirators with 27.43% (n = 369).
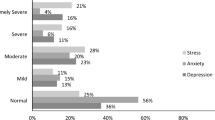
Prevalence of psychological disorders
Table 2 shows the prevalence of depression, anxiety, stress, and burnout in the study population. The frequency of symptoms was established as follows: anxiety (75.61%), depression (59.18%), and stress (53.09%). Overall, the prevalence of anxiety was higher than the frequency of depression or stress. A total of 587 (43.64%) healthcare professionals presented these 3 psychological disorders simultaneously. When considering burnout, the frequency of high-level emotional exhaustion, depersonalization, and low-level personal accomplishment were 34.28, 16.13, and 23.49% respectively.
Factors associated with severity of anxiety, depression, and stress
Bivariate and multivariate analysis via ordinal logistic regression of the demographic and clinical variables associated to anxiety, depression, and stress levels are shown in Table 3. Anxiety (OR: 1.44; 95% CI: 1.16–1.8.), depression (1.74; 1.27–2.37), and stress (1.51; 1.18–1.94) were more severe in women. Age was negatively associated with anxiety (0.98; 0.98–0.99), stress (0.98; 0.97–0.99), and depression severity (0.97; 0.96–0.98). Higher depression levels were found in single/divorced/ widowed participants (2.3; 1.48–3.59). Higher levels of anxiety and depression were found in participants who reported that their workload increased during the pandemic due to COVID-19 (2.18; 1.67–2.84); (2.07; 1.58–2.71), while higher levels of stress were found in the participants who reported that their workload “remained the same”. Likewise, higher levels of anxiety, depression, and stress were found in participants that expressed fear of the possibility of a negative outcome (death, negative sequelae) due to COVID-19 (2.25; 1.60–3.25), (1.49; 1.03–2.16), and (2.36; 1.69–3.29) respectively. The reduction in the number of consultations and surgery (1.01; 1.001–1.01) was also associated positively with anxiety severity, while the reduction in income during the pandemic was positively associated with higher levels of stress (1.01; 1.001–1.02) and depression (1.01; 1.001–1.02). Moreover, active healthcare workers presented higher levels of anxiety, depression, and stress (1.51; 1.21–1.89), (1.43; 1.14–1.79), and (1.31; 1.02–1.69) respectively. An interaction between diabetes and Covid-19 vaccination had statistically significant effects (0.084; 0.017–0.40) on anxiety levels, while an interaction between female gender and marital status (single/divorced/widowed) had statistically significant effects on depression levels (0.54; 0.32–0.89).
No collinearity problems were found through the linearity and the goodness-of-fit tests, both tests showed good models ‘specification. In addition, the proportional odds assumption was not rejected for all models (p values> 0.10). Likewise, no extreme or influential values were found for the residuals and leverage values.
Variables related to COVID-19
At the time of the study, 20.89% (n = 281) of the participants tested positive for SARS-Cov-2 and 41.93% (n = 564) had been isolated on suspicion of infection, in contrast, 84.76% (n = 1140) had been vaccinated for Covid-19. Around 87.96% (n = 1183) reported fear of contagion by SARS-CoV-2, and 85.50% (n = 1150) were afraid of the possibility of a negative outcome as death or negative sequelae due to Covid-19 infection. Finally, up to 92.71% (n = 1247) reported being afraid of the possibility of infecting their family and friends with Covid-19. These results are shown in Table 2.
Changes in daily and leisure activities due to COVID-19
Table 4 reports the daily and leisure activities that participants considered they would soon engage in. The activities that this population expected to engage in within the next 3 months included: eating at a restaurant (56.80%), getting a haircut at a salon or barbershop (49.96%), seeing a doctor for a non-urgent appointment (46.32%), and hiking, or picnicking outdoors with friends (40.52%). Conversely, many healthcare professionals expressed that they would never go out again with someone they do not know well (28.62%), workout at a gym or fitness studio (20.52%), ride a subway/bus (15.17%), attend a church or other religious service (11.52%), work in a shared office (8.62%), or attend a wedding or a funeral (8.25%).
Discussion
Healthcare professionals and front-line workers are especially vulnerable in times of public health crisis and may be at risk for developing adverse psychological outcomes, particularly in low/middle-income Latin American countries [22]. As previously mentioned, a study conducted in Colombian otolaryngologists and allergists during the COVID-19 pandemic reported high rates of psychological outcomes [11, 23]. Our study describes the prevalence of mental health outcomes and associated factors of anxiety, depression, and stress in the general Colombian health care population during the COVID-19 pandemic. A total of 1345 health care professionals participated in this study including nurses, physicians, therapists, and dentists, among others, although nearly half of them were specialist doctors. Adverse psychological outcomes such as anxiety, depression, and stress were reported in 75,61%, 59,18%, and 53,09% of the study population, respectively, echoing the findings of previous studies conducted during the pandemic [23, 24]; as mentioned previously.
A systematic review published in 2020 by Vizheh et al., reported a prevalence of anxiety, depression, and stress among health care professionals of 67.55, 55.89, and 62.99%, respectively [5]. Similarly, a prior study in a Spanish healthcare population that reported a prevalence of psychological distress of up to 80.6% [25], which to date is the highest rate of this mental outcome in healthcare workers. However, we stand out that our results remain among the highest rates of these psychological outcomes compared to prior reports worldwide, which underscores the importance of urgent mental health strategies for healthcare workers. Up to 43.64% of our study population presented these 3 psychological disorders simultaneously, highlighting the importance of prevention and early interventions. However, anxiety, depression, and stress symptoms require psychiatric evaluation and confirmation since the questionnaires applied to the population cannot rule out that these symptoms could be related to adjustment disorders. Our data was collected 1 year after the pandemic started and despite there is a significant amount of scientific information about the mental health in healthcare workers in the beginning of the pandemic, prior authors state that depending on the trajectory of the pandemic the mental health symptoms on healthcare workers could intensify or reduce over time [26].
About the factors associated with the severity of anxiety, depression, and stress; a higher severity of these outcomes was found in women. Similarly, Gómez-Salgado et al reported that among 3801 adults living in Spain during COVID-19 confinement, women had higher levels of psychological discomfort [27]. Previous studies have reported that women can be twice as more prone to depression than men probably due to individual factors such as genetic, environmental, and cultural influences [28, 29]. Furthermore, prior authors describe that woman in healthcare are often victims of additional external factors for mental health outcomes such as bias and discrimination, disparaging or disrespectful comments, lack of career promotion, disparities in resources (including financial and administrative support), rewards, and reimbursement [30, 31]. Additionally, due to school closures during the pandemic, family caregivers may have had a greater burden of responsibilities. This scenario could explain the interaction found between being women and being single/widowed/divorced, since this population was less prone to depression. However, we also stand out that the variable “single/widowed/divorced” was associated with the presence of depression. Prior authors have described this relationship between marital status and depression: a higher prevalence of depression in separated or divorced individuals may be due to both an increased risk of marital disruption, and to the higher risk of this disorder in those with divorced or separated marital status [32]. Organizational support strategies are needed in these populations to increase wellbeing, improve resilience, provide protected time to participate in self-care activities, and convenient access to physical and mental health services should be prioritized.
Age was also negatively associated with psychological outcomes; older age could lead to a lower probability of severe forms of these conditions. Similarly, a prior study in healthcare workers in Iran during the pandemic reported a higher frequency of depression and anxiety in younger participants aged 30–39 years old compared to those aged 40 or older [33]. However, the presentation of depression in older adults may be significantly different to that in younger adults, since it can be present with the absence of an affective component [34, 35]. Therefore, despite depression is the most common mental disorder in older adults, it can be often under-diagnosed probably due to age-related biological and psychological factors, and comorbidities [34, 36]. Moreover, a higher incidence of chronic disease and using regular medication has been associated with higher levels of anxiety and an increased risk of negative mental outcomes [37]. Even though the mental health symptoms may show variations among older populations, higher rates of morbidity and mortality have been described, as well as increased healthcare utilization and economic costs. Further studies assessing these findings should be performed in older populations.
Furthermore, higher levels of anxiety were found in participants that expressed fear of a negative outcome such as death or negative sequelae which is similar to a prior study that included Otolaryngologists and allergists in Colombia [11]. Almost 88% reported fear of contagion, and over 92% were afraid of the possibility of infecting their family and/or friends, highlighting the sense of fear as key in developing adverse emotional symptoms. Although prior authors state that the increase in workload may generally be associated with increased stress [38], in this study the increase in workload may be also associated with anxiety and depression which has been previously described as global public health priority [39]. Moreover, in this study the decrease in consultations was associated with anxiety. This scenario may be related to a decrease in monthly income since an association was also found between a reduction in income during the pandemic and the presence of depression and stress. Prior studies have shown that a significant decrease in household income is associated with an increased risk of incident mood, or anxiety disorders [23, 40]. This highlights the importance of providing not only emotional support but preventive financial measures to healthcare workers who may experience monetary drawbacks due to lockdown policies. On a more personal level, endeavors such as engaging with family and friends or taking part in outdoor activities have been compromised by the sanitary situation, consequently shaping behavioral standards, and altering traditional support systems, and emotional outlets.
More than 28% of healthcare professionals surveyed, expressed that they would never go out again with someone they do not know well. More than 20% expressed that they will never exercise in a gym again, and most participants reported delaying non-urgent medical appointments to up to a year, highlighting the risks in terms of physical as well as emotional health. These changes in work patterns and daily life were also described in a prior study by Colombian otolaryngologists and allergists [9]. Radical changes in the daily life of healthcare workers may predispose them to the accelerated development of mental disorders. Prior authors have described the role of negative future-oriented cognitions in depression prone individuals [41]. However, this scenario could also be related to the timepoint when the questionnaires were applied, since this survey was performed during the highest rates of infection of the pandemic in Colombia. During this period the vaccination programs were still on the first phase and preliminary studies reported the challenges and limited access to vaccination in low- to middle-income countries [42]. Nevertheless, the long-term impact is still to be defined and may change as studies are conducted at different time points of the COVID-19 pandemic.
Among the strengths of this study, we stand out that the study sample included health workers from different professions, since epidemiologic research highlights the critical constructs of “representativeness” and its relationship with the “generalizability” of study results [43]. The current study may encounter limitations regarding the cross-sectional design of the study can display associations between the variables, but no causal relationships. The survey was completed only by 1360 out of 3512 people who registered to the questionnaire (38.72%), which could lead to a selection bias. We highlight that this study was performed prior to the vaccination campaigns in Colombia, therefore these symptoms could have significant differences compared to the results after vaccination.
Shining light upon the importance of mental health in healthcare workers is essential considering the high prevalence of adverse psychological outcomes raised by the COVID-19 pandemic. Preventive strategies include adequate occupational environments, financial support, and incentives to mitigate stresses from financial uncertainty for frontline and independent healthcare workers. Previous studies state that key strategies to reduce anxiety among healthcare workers include limitation of shift hours, clear communication, ensuring adequate rest areas, providing timely and appropriately tailored mental health support through hotline teams, media or multidisciplinary teams, and involving mental health professionals in follow-up, diagnose and provide early therapeutic interventions [44, 45]. A current systematic review stated that clear communication and support from the healthcare institutions, social support, and personal sense of control are protective factors for mental disorders on healthcare workers during pandemic outbreaks [46]. Further studies are essential to support preventive and therapeutic public health strategies to achieve early mental health prevention approaches, as well as therapeutic interventions in this population.
Conclusions
During this COVID-19 pandemic, the frequency of anxiety, depression, and stress is high among this healthcare population compared to prior reports worldwide and the Colombian healthcare population. Anxiety, depression, and stress were more severe in women. Higher levels of anxiety, depression, and stress were found in participants that expressed fear of the possibility of a negative outcome (death, negative sequelae) due to COVID-19. The reduction in the number of consultations and surgery was also associated positively with anxiety severity, while the reduction in income during the pandemic was positively associated with higher levels of stress. Research on these psychological outcomes is needed in Latin America to achieve early mental health prevention approaches, as well as therapeutic interventions in this population. Psychological and/or psychiatric support without occupational stigmatization should be granted by the institutions.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
References
O’Leary VB, Ovsepian SV. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). Trends Genet. 2020;36(11):892–3.
Darmon M, Dumas G. Anticipating outcomes for patients with COVID-19 and identifying prognosis patterns. Lancet Infect Dis. 2021;21(6):744–5.
Danet A. Psychological impact of COVID-19 pandemic in Western frontline healthcare professionals. A systematic review. Med Clin. 2021;156(9):449–58.
Maunder RG, Lancee WJ, Balderson KE, Bennett JP, Borgundvaag B, Evans S, et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. 2006;12(12):1924–32.
Vizheh M, Qorbani M, Arzaghi SM, Muhidin S, Javanmard Z, Esmaeili M. The mental health of healthcare workers in the COVID-19 pandemic: A systematic review. J Diabetes Metab Disord. 2020;19(2):1967–78.
Spoorthy MS, Pratapa SK, Supriya M. Mental health problems faced by healthcare workers due to the COVID-19 pandemic–A review. Asian J Psychiatric. 2020;51:102119 (January).
Rana W, Mukhtar S, Mukhtar S. Mental health of medical workers in Pakistan during the pandemic COVID-19 outbreak. Asian J Psychiatr. 2020;51:102080.
Mental Health America. The Mental Health of Healthcare Workers in COVID-19 | Mental Health America; 2021. p. 1–17. [cited 2021 Dec 22]. Available from: https://mhanational.org/mental-health-healthcare-workers-covid-19
Kock D. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being; 2009. p. 1–360.
Saragih ID, Tonapa SI, Saragih IS, Advani S, Batubara SO, Suarilah I, et al. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: A systematic review and meta-analysis. Int J Nurs Stud. 2021;121(104002):104002.
Pérez-Herrera LC, Moreno-López S, Peñaranda D, Pérez-García IC, García E, Corredor-Rojas G, et al. Effect of the COVID-19 pandemic on the mental health, daily and occupational activities of otolaryngologists and allergists in Colombia: a national study. Int Forum Allergy Rhinol. 2021;7(April):1–5.
Miranda MAM, Visbal JHW. Mental health of colombian general practitioners during the pandemic: Reflections from a brief survey. Vol. 26, Hacia la Promocion de la Salud: Universidad de Caldas; 2021. p. 17–9.
Monterrosa-Castro A, Dávila-Ruiz R, Mejía-Mantilla A, Contreras-Saldarriaga J, Mercado-Lara M, Florez-Monterrosa C. Occupational Stress, Anxiety and Fear of COVID-19 in Colombian Physicians. MedUNAB. 2020;23(2):195–213.
Smallwood N, Karimi L, Bismark M, Putland M, Johnson D, Dharmage SC, et al. High levels of psychosocial distress among Australian frontline healthcare workers during the COVID-19 pandemic: a cross-sectional survey. General Psychiatry. 2021;34(5):e100577 Available from: http://gpsych.bmj.com/content/34/5/e100577.abstract.
Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–7.
Machin D, Campbell MJ, Tan SB, Tan SH. Sample Size Tables for Clinical Studies (Google eBook), vol. 264; 2011.
García-Campayo J, Zamorano E, Ruiz MA, Pardo A, Pérez-Páramo M, López-Gómez V, et al. Cultural adaptation into Spanish of the generalized anxiety disorder-7 (GAD-7) scale as a screening tool. Health Qual Life Outcomes. 2010;8:1–11.
Saldivia S, Aslan J, Inostroza C. Propiedades psicométricas del PHQ-9. Rev Med Chil. 2019;9:53–60.
Campo-Arias A, Oviedo HC, Herazo E. Escala de Estrés Percibido-10: Desempeño psicométrico en estudiantes de medicina de Bucaramanga, Colombia. Revista de la Facultad de Medicina. 2015;62(3):407–13.
Escala LA, Percibido DEE, Trujillo HM. Propiedades psicométricas de la versión española de la Escala de Estrés Percibido ( EEP ). 2007;(April 2019).
Sanger-Katz M, Miller CC, Bui Q. When 511 Epidemiologists Expect to Fly, Hug and Do 18 Other Everyday Activities Again. https://www.nytimes.com/interactive/2020/06/08/upshot/when-epidemiologists-will-do-everyday-things-coronavirus.html. Accessed 30 Oct 2018.
Peñaranda D, Perez-Herrera LC, Moreno-Lopez S, Peñaranda A. COVID-19 Pandemic on Mental Health in Pediatric Otolaryngologists in Latin America. Otolaryngol Head Neck Surg. 2021;165(1_suppl):P318.
Padilla S, Calero-sierra I, Almazara C. Mental health impact of COVID-19 pandemic on Spanish healthcare workers; 2020. p. 8–13.
Di Tella M, Romeo A, Benfante A, Castelli L. Mental health of healthcare workers during the COVID-19 pandemic in Italy. J Eval Clin Pract. 2020;26(6):1583–7.
Gómez-Salgado J, Domínguez-Salas S, Romero-Martín M, Romero A, Coronado-Vázquez V, Ruiz-Frutos C. Work engagement and psychological distress of health professionals during the COVID-19 pandemic. J Nurs Manag. 2021;29(5):1016–25. Available from:. https://doi.org/10.1111/jonm.13239.
Civantos AM, Byrnes Y, Chang C, Prasad A, Chorath K, Poonia SK, et al. Mental health among otolaryngology resident and attending physicians during the COVID-19 pandemic: National study. Head Neck. 2020;42(7):1597–609 Available from: https://pubmed.ncbi.nlm.nih.gov/32496637.
Gómez-Salgado J, Domínguez-Salas S, Rodríguez-Domínguez C, Allande-Cussó R, Romero-Martín M, Ruiz-Frutos C. Gender perspective of psychological discomfort during COVID-19 confinement among Spanish adult population: a cross-sectional study. BMJ Open. 2021;11(12):e051572 Available from: http://bmjopen.bmj.com/content/11/12/e051572.abstract.
Kuehner C. Gender differences in unipolar depression: an update of epidemiological findings and possible explanations. Acta Psychiatr Scand. 2003;108(3):163–74.
Kuehner C. Why is depression more common among women than among men? Lancet Psychiatry. 2017;4:146–58 Elsevier Ltd.
Templeton K, Medical K, Bernstein CA, Einstein A, Sukhera J, Nora LM, et al. Gender-Based Di ff erences in Burnout : Issues Faced by Women Physicians. NAM Perspectives. 2019; Discussion.
Bacigalupe A, Martín U. Gender inequalities in depression/anxiety and the consumption of psychotropic drugs: Are we medicalising women’s mental health? Scand J Public Health. 2020;49(3):317–24.
Bulloch AG, Williams JV, Lavorato DH, Patten SB. The relationship between major depression and marital disruption is bidirectional. Depression Anxiety. 2009;26(12):1172–7.
Hassannia L, Taghizadeh F, Moosazadeh M, Zarghami M, Taghizadeh H, Dooki AF, et al. Anxiety and Depression in Health Workers and General Population During COVID-19 in IRAN: A Cross-Sectional Study. Neuropsychopharmacol Rep. 2021;41(1):40–9. Available from: https://doi.org/10.1002/npr2.12153.
Alexopoulos GS. Depression in the elderly. Lancet. 2005;365(9475):1961–70 Available from: https://linkinghub.elsevier.com/retrieve/pii/S0140673605666652.
Fiske A, Wetherell JL, Gatz M. Depression in Older Adults. Ann Rev Clin Psychol. 2009;5(1):363–89 Available from: https://www.annualreviews.org/doi/10.1146/annurev.clinpsy.032408.153621.
Pocklington C, Gilbody S, Manea L, McMillan D. The diagnostic accuracy of brief versions of the Geriatric Depression Scale: a systematic review and meta-analysis. Int J Geriatr Psychiatry. 2016;31(8):837–57 Available from: https://onlinelibrary.wiley.com/doi/10.1002/gps.4407.
Mete B, Fırıncı B, Doğan E, Pehlivan E. Depression and affecting factors in patients over 50 years of age: A cross-sectional study. J Surg Med. 2018;3:3–8.
Portoghese I, Galletta M, Coppola RC, Finco G, Campagna M. Burnout and workload among health care workers: the moderating role of job control. Saf Health Work. 2014;5(3):152–7 Available from: https://pubmed.ncbi.nlm.nih.gov/25379330.
Søvold LE, Naslund JA, Kousoulis AA, Saxena S, Qoronfleh MW, Grobler C, et al. Prioritizing the Mental Health and Well-Being of Healthcare Workers: An Urgent Global Public Health Priority. Front Public Health. 2021;9 Available from: https://www.frontiersin.org/articles/10.3389/fpubh.2021.679397/full.
Sareen J, Afifi TO, KA MM, Asmundson GJ. Relationship between household income and mental disorders: findings from a population-based longitudinal study. Arch Gen Psychiatry. 2016;68(4):419–27.
Thimm J, Holte A, Brennen T, Wang CE. Hope and expectancies for future events in depression. Front Psychol. 2013:4, 470 Available from: https://www.frontiersin.org/article/10.3389/fpsyg.2013.00470.
Tagoe ET, Sheikh N, Morton A, Nonvignon J, Sarker AR, Williams L, et al. COVID-19 Vaccination in Lower-Middle Income Countries: National Stakeholder Views on Challenges, Barriers, and Potential Solutions. Front Public Health. 2021:9 Available from: https://www.frontiersin.org/article/10.3389/fpubh.2021.709127.
Kukull WA, Ganguli M. Generalizability: the trees, the forest, and the low-hanging fruit. Neurol Int. 2012;78(23):1886–91 Available from: https://pubmed.ncbi.nlm.nih.gov/22665145.
Ramanathan K, Antognini D, Combes A, Paden M, Zakhary B, Ogino M, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):e15–e16.
Blake H, Bermingham F, Johnson G, Tabner A. Mitigating the psychological impact of covid-19 on healthcare workers: A digital learning package. International Journal of Environmental Research and Public Health, núm 17. Recuperado el 16 de Agosto del 2020. Int J Environ Res Public Health. 2020;17(2997):1–15.
De Brier N, Stroobants S, Vandekerckhove P, De Buck E. Factors affecting mental health of health care workers during coronavirus disease outbreaks (SARS, MERS & COVID-19): A rapid systematic review. PLoS ONE. 2020;15(12 December):1–19.
Acknowledgements
This work was supported by the Unidad Medico Quirúrgica de Otorrinolaringología UNIMEQ-ORL from Bogotá, Colombia. Special thanks to all the organizations who supported the fieldwork of this study: Academia Nacional de Medicina, Asociación Colombiana de Fisioterapia, Asociación de Exalumnos de Facultad de Medicina de la Universidad Nacional, ASMEDAS, Asociación Nacional de Enfermeras de Colombia, Colegio Médico Colombiano, Facultades de Medicina de la Universidad de Los Andes, Universidad Nacional y Fundación Universitaria de Ciencias de la Salud, Federación Colombiana de Sindicatos Médicos, Fonoaudiología, Terapia respiratoria y Ocupacional, Federación Médica Colombiana, Médicos Generales Colombianos, and Sociedades Científicas y Sociedades Afiliadas.
Copyright/license for publication
The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, a worldwide license to the Publishers and its licensees in perpetuity, in all forms, formats, and media (whether known now or created in the future), to i) publish, reproduce, distribute, display and store the Contribution, ii) translate the Contribution into other languages, create adaptations, reprints, include within collections and create summaries, extracts and/or, abstracts of the Contribution, iii) create any other derivative work(s) based on the Contribution, iv) to exploit all subsidiary rights in the Contribution, v) the inclusion of electronic links from the Contribution to third party material where-ever it may be located; and, vi) license any third party to do any or all of the above.
Funding
This study was supported by the Unidad Medico Quirúrgica de Otorrinolaringología UNIMEQ-ORL, Bogotá, Colombia.
Author information
Authors and Affiliations
Contributions
Conceptualization: AP EG. Data evidence collection: AP EG DP SML LCPH. Supervision: AP. Statistical analysis and methodology: SML. Analyzed the data: SML AT JM LCPH. Funding acquisition and resources providing: AP. Writing – Original Draft Preparation: AP DP JM SML AT LCPH. Writing – Review & Editing: AP DP JM LCPH SML EG AT. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ethical Committee of the Hospital Universitario Fundación Santa Fe (Protocol Number: CCEI-12992-2021) approved this study. All patients provided informed consent.
Consent for publication
Not applicable.
Competing interests
The authors report no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Peñaranda, A., García, E., Pérez-Herrera, L.C. et al. Effect of the COVID-19 pandemic on the mental health, daily and occupational activities among health professionals in Colombia: a national study. BMC Psychiatry 22, 682 (2022). https://doi.org/10.1186/s12888-022-04337-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-022-04337-9