Abstract
Background
Health risk behaviours (e.g., harmful drinking and smoking) often cluster together and can be associated with poor mental health and stress. This study examined how health risk behaviours cluster together in individuals in a high stress occupation (UK Police Service), and the associations with mental health and job strain.
Methods
Data was obtained from the Airwave Health Monitoring Study (25,234 male and 14,989 female police employees), which included measures of health risk behaviours (alcohol use, diet, smoking status, physical activity), poor mental health (depression, anxiety, post-traumatic stress disorder [PTSD]), and job strain (low, high, active, passive). Classes of health risk behaviours were identified using Latent Class Analysis (LCA) and the associations with mental health and job strain were analysed through multinomial logistic regressions.
Results
For men and women, a 5-class solution was the best fit. Men and women with depression, anxiety, and/or PTSD (analysed as separate variables) had at least double the odds of being assigned to the “high health risk behaviours” class, compared to those with no mental health problem. Compared to those reporting low strain, men and women reporting high strain had increased odds of being assigned to the “low risk drinkers with other health risk behaviours” classes.
Conclusions
These finding highlight the importance of holistic interventions which target co-occurring health risk behaviours, to prevent more adverse physical health consequences. Police employees with poor mental health are more likely to engage in multiple health risk behaviours, which suggests they may need additional support. However, as the data was cross-sectional, the temporal associations between the classes and mental health or job strain could not be determined.
Similar content being viewed by others
Introduction
Health behaviours are actions to maintain, attain or regain good health, such as exercising regularly and eating a balanced diet [1]. Contrarily, health risk behaviours, such as heavy drinking and smoking [2], are major causes of chronic disease and premature mortality [3]. Whilst health risk behaviours are often researched separately, evidence suggests they co-occur [4,5,6], particularly heavy drinking and smoking [7, 8]. However, not all health risk behaviours cluster together. According to the Theory of Triadic Influence (TTI), some behaviours have similar experiences and consequences (e.g., alcohol and nicotine may both be used to alleviate negative affective states), therefore it is logical that they co-occur [9]. Certain sociodemographic characteristics are related to clustered health risk behaviours, such as male gender [7, 10] and older age [11]. Further, clusters of health risk behaviours have associations with mental health problems [12, 13]. One study showed that men and women with depression had double the odds of being assigned to one of the three health risk behaviour clusters, than the healthiest cluster [12]. Additional research identified that individuals reporting more frequent mental distress were more likely to experience clustered poor diet, insufficient physical activity and poor sleep [14].
Work stressors impact health behaviours and mental health [15, 16], with evidence suggesting that high job strain (high demands, low control) is linked to heavy drinking and smoking [17, 18], and poor mental health [19]. High strain could be linked to health risk behaviours through maladaptive coping, but conversely, there is evidence that health behaviours, such as keeping active, can be used as a form of proactive coping, though over-exercising can be problematic [20, 21]. Certain occupations are characterised by stressors (e.g., intensive demands, lack of control) which negatively impact mental health, such as policing [22,23,24], which could have associations with health risk behaviours. For example, one third of United Kingdom (UK) police employees met criteria for hazardous or harmful drinking, and those with a mental health problem were twice as likely to drink harmfully [25]. Contradicting previous evidence, police employees reporting high strain were less likely to drink hazardously than those with low strain [25], which may reflect proactive coping. These findings highlight the importance of understanding how health risk behaviours cluster in those working in stressful occupations, and to determine the characteristics of those more likely to engage in multiple health risk behaviours.
Policing is a highly stressful occupation and police employees in the UK show high levels of heavy drinking [25]. However, it is not known how health risk behaviours cluster together in UK police employees. Latent Class Analysis (LCA) is a statistical technique used to identify distinct classes based on responses to multiple variables, and has previously been used to determine classes of health risk behaviours in adolescents [26], vocational education students [27], older adults [28] and the UK general population [29]. This study aims to utilise LCA to identify classes of health risk behaviours (alcohol use, fruit and vegetable intake, red meat consumption, smoking, physical activity) in UK police employees, and to determine their associations with mental health (depression, anxiety, PTSD) and job strain (high, low, active, passive). The sociodemographic and occupational associations with the identified classes will be explored, to determine the characteristics of each class and the covariates to be included in the main analyses. This study has been pre-registered with Open Science Framework, where the aims and hypotheses are described in detail https://osf.io/4j7mx.
Methods
Study Sample
The study sample was obtained from the Airwave Health Monitoring Study [30]. Data were collected through an enrolment questionnaire sent from administration or occupational health services, and through health screens conducted by trained nurses (advertised through force-wide publicity). Data on a range of health risk behaviours were collected, as well as measures of mental health, job strain, sociodemographics and occupational factors. Data was collected between June 2006 and March 2015 from 28 participating forces (out of 54), with the current sample including 40,986 police officers and staff (response rate averaged 50% across participating forces). The study was open to police employees from all roles (at any level) and police employees could still participate in the health screen even if they did not belong to one of the participating forces. The sample was representative of the UK Police Service in terms of gender and ethnic composition [31]. A detailed design and protocol for the Airwave Health Monitoring Study is available elsewhere [30].
Measures of health risk behaviours
Alcohol use
Two measures of alcohol use were included: categorisation of alcohol consumption (non-drinkers, low risk, hazardous, harmful), and frequency of binge drinking (6 or more drinks on one occasion). Participants who stated “no” to ever drinking alcohol were categorised as “non-drinkers”. The remaining categories were derived from the UK Chief Medical Officer’s guidelines for “low risk” drinking (0–14 units per week) [32], and the National Institute for Health and Care Excellence (NICE) guidelines for hazardous (> 14 to 35/50 units for women/men) and harmful drinking (> 35/50 units for women/men) [33]. Participants stated the number of drinks consumed (white wine, red wine, fortified wine, beer, and spirits) over the past seven days, which was converted to units. Frequency of binge drinking was measured using a single item (“How often do you have six or more drinks on one occasion?”), with the following options: never, monthly or less, two to four times a month, two to three times a week, and daily or almost daily.
Smoking status
Smoking status was derived from two items which asked if participants currently smoked cigarettes and if so, how many cigarettes did they smoke per day. Participants were categorised as “non-smokers”, “0 to 10 cigarettes per day” (light to moderate smoking) or “more than 10 cigarettes per day” (heavy smoking) [34].
Physical activity
Physical activity was measured using the validated seven-item International Physical Activity Questionnaire – Short Form [35, 36], which has also been validated in occupational settings [37, 38]. The IPAQ-SF measures the frequency, intensity and duration of walking, moderate and vigorous physical activity. Metabolic equivalent (MET; the ratio of work metabolic rate to resting metabolic rate) minutes were computed for each activity (one minute of walking = 3.3 MET mins, moderate activity = 4 MET mins, vigorous activity = 8 MET mins). High physical activity was defined as vigorous intensity activity on at least three days (minimum of 1500 MET minutes), or seven days of any combination of walking, moderate or vigorous intensity activities (minimum of 3000 MET minutes). Moderate physical activity was defined as three or more days of vigorous intensity activity, five or more days of moderate intensity activity, five or more days of walking (at least 30 min per day), or five or more days of any combination of walking, moderate or vigorous intensity activities (minimum of 600 MET minutes per week). Low physical activity was categorised as not meeting either criteria [35]. UK government guidelines recommend achieving a minimum of 600 MET minutes per week [39].
Average daily fruit and vegetable intake
Four items measured frequency (days per week) and quantity (how many) of fruit (portions) and vegetable (heaped tbsp.) consumption. Public Health England (PHE) guidance recommends five portions of fruit and vegetables per day, and states that three heaped tbsp of vegetables is equivalent to one portion [40]. Quantity of vegetables was divided by three to reflect portions. Average daily fruit and vegetable intake was computed by calculating total weekly fruit and vegetable intake, multiplying frequency and quantity, then dividing by seven. This was categorised into “2 or less servings per day”, “3 to 4 servings per day”, and “5 or more servings per day”.
Red meat consumption
A single item asked, “How often do you eat red meat (beef, veal, lamb, mutton, or pork)?”, with the following response options: “never”, “less than once a week”, “once a week”, “two or more times a week”.
Measures of mental health and job strain
Probable depression
The Patient Health Questionnaire-9 (PHQ-9) [41] is a 9-item self-report screen of symptoms of depression (e.g., trouble sleeping, suicidal thoughts), where responses are provided on a 4-point Likert scale, ranging from “not at all” to “nearly every day”. Scores range from 0 to 27, with a validated cut-off of 10 indicating probable depression. McDonald’s omega (ω) indicated excellent internal reliability within this sample (ω = 0.93).
Probable anxiety
The anxiety subscale of the Hospital Depression and Anxiety Scale (HADS-A) [42] is a 7-item self-report screen of symptoms of anxiety (e.g., feeling tense, restlessness). Scores range from 0 to 21, with a validated cut-off of 9 indicating probable anxiety. The scale showed excellent internal reliability within this sample (ω = 0.90).
Probable PTSD
The Trauma Screen Questionnaire (TSQ) [43] is a 10-item screen of symptoms of PTSD (e.g., upsetting thoughts/memories, bodily reactions). Participants were only asked these items if they reported a traumatic experience in the 6 months prior to the survey. A 4-point Likert scale was used, ranging from “not at all” to “extremely”. However, responses to the TSQ are usually binary, so “not at all” was coded as 0 and all other response options were coded as 1. Scores ranged from 0 to 10, with a validated cut-off of 6 indicating probable PTSD. The scale showed excellent internal reliability within this sample (ω = 0.99).
Job strain
Job strain was measured using six items from the Job Content Questionnaire (JCQ) [44], with four items measuring control and two items measuring demand. The scale showed good internal reliability within this sample (ω = 0.82). A validated quadrant approach was used to group participants into high strain (high demand, low control), low strain (low demand, high control), active strain (high demand, high control), and passive strain (low demand, low control). The sample medians for total scores on the demand items and control items were used to categorise participants into high or low demand and control [45].
Sociodemographic and occupational measures
The Airwave Health Monitoring Study obtained several self-reported sociodemographic measures: age, gender, country (England, Wales, Scotland), marital status (married/cohabitating, divorced/separated, single, other), education (GSCE or below, vocational qualifications/NVQ1 + 2, A levels/Highers or equivalent, Bachelor’s or postgraduate degree), ethnicity (White, Asian, Black, Mixed ethnic background, other), and number of children under 18 (none, one, two, three or more). Several self-reported occupational variables were measured, including job role (police officer, police staff, other), income (less than £25,999, £26 k to £37,999, £38 k to £59,999, more than £60 k), years in the police force (less than five, six to ten, 11 to 20, more than 20), and number of days sickness absence in the past year (none, one to five, six to ten, more than ten). Body Mass Index (BMI) was derived from participant’s weight and height (underweight > 18.5 kg/m2, normal weight 18.5 to 25 kg/m2, overweight 25 to 30 kg/m2, obese < 30 kg/m2).
Data analysis
LCA is a statistical technique used to identify membership in unobserved (latent) subgroups (classes), based on individual responses from multiple variables [46]. For the current study, LCA was conducted in Mplus version 8.3, to determine underlying classes of health risk behaviours by estimating and evaluating a series of models with an incrementally greater number of classes, starting with a 2-class model, to determine the optimal number of classes (Fig. 1).
In LCA, the number of classes is considered optimal when there is homogeneity within the classes and heterogeneity between the classes. The models were evaluated with a range of model fit criteria: Akaike Information Criterion (AIC) [47], Bayseian Information Criteria (BIC) [48], sample size adjusted BIC (SSABIC) [49], entropy values [50], number of bivariate residuals (BVR) [51], and Voung-Lo-Mendell-Rubin likelihood ratio test (VLMR LRT) [52]. Smaller AIC, BIC and SSABIC values indicate better model fit [53]. Larger entropy values (> 0.70) indicate better classification accuracy [50, 54]. Non-significant (p > 0.05) VLMR LRT indicates that an additional class does not provide a better fit than a model with one less class, favouring a simpler model [53]. Models containing fewer significant BVR (> 3.84) suggest better model fit [51, 55]. Response probabilities were assessed across all models to determine the most informative and meaningful number of classes [53]. After the optimal number of classes was determined, gender was added using “knownclass”, to examine what the classes looked like for each gender (class memberships and response probabilities can differ for men and women).
Class membership and the conditional probability of assignment to each class were saved in Mplus and imported into STATA SE 15, for the regression analyses. The probability of assignment was used as a probability weight in the regression models to account for individual differences (i.e., individuals in the same class will not all have a probability of 1.0) [56]. Descriptive statistics (mean and standard deviation) explored differences in BMI across the classes.
Unadjusted multinomial regression analyses were first used to determine the sociodemographic (age, education, marital status, children under 18) and occupational (role, years in police force, income, days of sickness absence) associations with each of the classes, separately for men and women (Supplementary materials). Variables with strong statistically significant (p < 0.001) associations were included as covariates in the subsequent analyses. Adjusted multinomial regression analyses then determined the mental health (depression, anxiety, PTSD) and job strain (high, low, active, passive) associations with each of the classes, separately for men and women. The reference groups were determined based on size and characteristics of the classes (i.e., sufficient numbers and meaningfulness of reference class).
Missing data
The proportion of missing data was typically less than 1%, except for PTSD and job role. For PTSD, 6% (N = 2,469) of the data was missing (completely at random), as participants who completed the study in 2006 were not provided with the PTSD items. For police role, 9% (N = 3,859) of the data was missing, with no record of a result having been received and no explanation why. PTSD and role were only explored as stand-alone variables when looking at their independent associations with the classes of health risk behaviours, and so, the missing data for these variables did not impact the sample size for main latent class model. The minimal missing data for the health risk behaviour variables included in the LCA were handled using Full Information Maximum Likelihood (FIML) estimation, whereby the available data was used to estimate the model and population parameters.
Results
Sample characteristics
The sociodemographic and occupational characteristics of the current sample (N = 40,986) are outlined in Supplementary table 1. Descriptive statistics for the health risk, mental health, and job strain variables, for the full sample, are shown in Table 1. Most of the sample were low-risk drinkers (55%). Only 14% of the sample reported sufficient fruit and vegetable intake (5 or more servings per day). Around 70% of the sample consumed red meat once a week or more. Almost all participants were non-smokers. Over 50% met criteria for high physical activity. The screening measures of mental health indicated that 10% met criteria for probable depression, 8% for probable anxiety and 4% for probable PTSD.
Latent class analysis of health risk behaviours
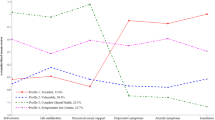
The LCA identified a five-class solution as the best fit for the full sample, based on the model fit criteria and meaningfulness of the classes (Table 2). The AIC, BIC and SSABIC decreased with every additional class, though reductions levelled off after five classes (supplementary Fig. 1). The number of significant BVRs decreased from 20 for four classes, to seven for five classes, suggesting greater conditional independence for a five-class solution. Entropy was highest for four classes (0.85), indicating better classification accuracy, though this was still sufficient for five classes (0.71) [54]. When examining the item-response probabilities across models with an incremental number of classes, the additional fifth class was meaningful as it created two distinct classes of varied health and health risk behaviours (i.e., low-risk drinkers but engaged in other health risk behaviours versus physically active but engaged in other health risk behaviours). After selecting a five-class model, gender was added using the “knownclass” function, to allow for gender differences in assignment to the classes. The entropy value and number of significant BVRs indicated that a five-class solution was a good fit to the multigroup model.
The response probabilities for men (N = 25,788) and women (N = 15,198) are shown in Table 3 and the class descriptions are defined in Table 4, with the probability-weighted proportions of participants in each class. There were five distinct classes for men and women. Both genders had a “healthiest” class (17.6% of men, 28.7% of women) and a “healthy abstainers” class (13.8% of men, 16.2% of women). These two classes can be distinguished as the “healthiest” class consisted mostly of drinkers (at a low-risk level) and had the highest probabilities for sufficient fruit/vegetable intake, low red meat consumption, non-smoking, and physical activity, whereas the “healthy abstainers” class comprised mostly abstainers who also had high probabilities (but not as high) for these items. The largest class for both genders was “low risk drinkers but other health risk behaviours” (35.6% of men, 39.1% of women), with high probabilities of low-risk drinking, but also insufficient fruit/vegetable intake and low physical activity. The smallest class for both genders was “high health risk behaviours” (4.1% of men, 3.8% of women). For men, the final class reflected “some health risk behaviours but physically active” (28.9%), as this class was defined by hazardous/binge drinking, light/moderate smoking, but high physical activity. For women, the final class reflected “moderate health risk” (12.2%), which had similar characteristics to the final class for men.
Sociodemographic and occupational associations
The sociodemographic and occupational associations with each class are outlined in Supplementary table 2 for men and Supplementary table 3 for women. The “healthiest” class was the reference group for both men and women.
Men over 40 had double the odds of being in the “high health risk” class, and men aged over 50 had 1.5 times greater odds of being in the “healthy abstainers” class, but reduced odds of being in the “low risk drinkers but other health risks” class (versus < 29 years old). Men who held a GCSE education or below had increased odds of being in the “high health risk” class, compared to all other categories. Asian men showed 9 times greater odds of being in the “healthy abstainers” class, and Black men showed 3 times greater odds (versus White men). Police staff showed 1.7 times greater odds of being in the “healthy abstainers” class than police officers, and those who had served for over 10 years (versus < 5) showed double the odds of being in the “high health risk” class. Men with the lowest income (versus all other categories) were significantly more likely to be in the “healthy abstainers” class. Men with more than 10 days of sickness absence (versus none) had at least 1.5 times greater odds of being in the “high health risk” class and the “healthy abstainers” class.
Women aged 40–49 years old had double the odds of being in the “high health risk” class, and women over 50 had reduced odds of being in the “moderate health risk” class (versus < 29 years old). Women under 29 had increased odds of being in the “low risk drinkers but other risks” class, versus all other age groups. Women with a bachelor’s/postgraduate degree showed reduced odds of being assigned to the “high health risk” and “low risk drinkers but other risks” classes (versus GCSE education or below). Asian women had 5.4 times greater odds of being in the “healthy abstainers” class, and Black women had 4.6 times greater odds, compared to White women. Single women had at least 1.3 times greater odds of being assigned to the “low risk drinkers but other risks” and “moderate health risk” classes, than married/cohabiting women. Women who had served for more than 10 years (versus < 5) showed 1.8 times greater odds of being in the “high health risk” class, but reduced odds of being in the “low risk drinkers but other risks” class. Women with more than 10 days of sickness absence (versus none) were 1.6 times more likely to be in the “high health risk” class and “healthy abstainers” class.
Mental health and job strain associations
The mental health and job strain associations with class membership are shown in Table 5, separately for men and women. The sociodemographic and occupational variables found to be significantly associated with class membership in men and women (age, country, education, ethnicity, marital status, number of children under 18, years in police force, income, days of sickness absence in past year) were included as covariates (except for role, due to a large proportion of missing data). The “healthiest” classes for men and women were the reference groups.
Men with probable depression, anxiety or PTSD had 2.5 to 3.5 times greater odds of being in the “high health risk behaviours” class (versus those with no mental health problem). Men with depression or anxiety had double the odds of being in the “healthy abstainers” class, with weaker associations for PTSD. Men with depression, anxiety or PTSD had between 1.3 to 1.8 greater odds of being assigned to the “health risk behaviours but physically active” class. Men with probable depression or anxiety, but not PTSD, had at least 1.5 times the odds of being in the “low risk drinkers but other health risk behaviours” class.
Women with probable depression or anxiety had at least double the odds of being in the “high health risk behaviours” class, compared to those without depression or anxiety. Probable PTSD was also associated with 1.7 times greater odds of being in the “high health risk behaviours” class, and 1.4 times greater odds of being in the “moderate health risk behaviours” class. Women with probable depression had 1.3 times greater odds of being in the “healthy abstainers”, “moderate health risk behaviours” and “low risk drinkers but other health risk behaviours” classes, compared to those without depression. Women with probable anxiety showed 1.1 and 1.2 times greater odds of being in the “moderate health risk behaviours” and “low risk drinkers but other health risk behaviours” classes, respectively.
Both men and women reporting high strain (versus low strain) were significantly more likely to be in the “low risk drinkers but other health risk behaviours” class, but the odds ratios were small (1.1 for men, 1.2 for women).
Discussion
Key findings
This study utilised a large, representative sample of UK police employees, to explore how health risk behaviours cluster together and to determine their associations with mental health and job strain. Five classes were identified, with the smallest reflecting “high health risk behaviours” in both men and women, the most common reflecting “low risk drinkers but other health risk behaviours”, and two healthy classes, reflecting the “healthiest” and “healthy abstainers”. The final class for men reflected “some health risks but physically active” and “moderate health risk” for women. For both genders, those with probable depression, anxiety, or PTSD (compared to no mental health problem) had greater odds of being assigned to the “high health risk behaviours” class, though the odds were not as large for women. Men and women with probable depression were more likely to be in the “healthy abstainers” class, which was also apparent in men with probable anxiety and PTSD. Men and women reporting high strain (compared to low strain) had increased odds of being in the “low risk drinkers with other health risk behaviours” class. These findings highlight the importance of understanding clustering health risk behaviours, as the mental and physical health consequences will be greater for those with multiple risks [57].
Classes of health risk behaviours
Previous literature has identified similar clusters of health risk behaviours, with clusters at either end of the spectrum (healthiest versus multiple health risk behaviours), with remaining classes reflecting a mixture of behaviours, which are usually more common [4, 12,13,14]. This is in line with the Theory of Triadic Influence (TTI), which proposes that behaviours are determined by one’s intentions, meaning health risk behaviours cluster together and healthy behaviours cluster together, because they align to similar social-cultural intentions [9]. Across the literature, there are differences in the proportion of participants considered “healthy”. In this study, 35% of male police employees and 42% of female police employees were in the two healthy classes (“healthiest” and “healthy abstainers”), compared to 80% of the Dutch general population [12], 23% of the UK general population [11], and 36% of men and 37% of women in the Australian general population [14], being in the “healthiest” classes. These findings suggest that UK police employees may engage in some health behaviours more than the UK general population, such as physical activity, but show other health risk behaviours, such as poor diet (13% met criteria for recommended fruit and vegetable intake, vs 25% of UK general population [58]). This may be because a certain level of fitness is required in police employees, and the latter may relate to shift work, which is associated with irregular eating patterns and unhealthy eating [59].
Mental health and job strain
Previous findings of the same sample showed a relationship between poor mental health with harmful drinking and abstinence [25]. The present findings extend this, now showing a relationship between poor mental health and multiple health risk behaviours, with two–three times greater odds for male police employees with a mental health problem. This is in line with the few existing studies which demonstrate that individuals with poor mental health are more likely to be assigned to clusters of high health risk behaviours [12, 14, 60]. One study of vocational education students explored the clustering of physical and mental health risks, finding a class of high anxiety, high depression, and multiple health risk behaviours (smoking, risky alcohol use, poor diet, physical inactivity) [27]. A study independently examining associations between health risk behaviours and mental health, found that poor mental health was linked with smoking, low fruit and vegetable intake, and abstinence [61]. The latter is harmonious with current findings, showing poorer mental health in “healthy abstainers” than police employees in the “healthiest” class, and with a growing body of literature evidencing a J-shaped relationship, whereby poor mental health is associated with abstinence and heavy drinking [62,63,64]. This can be explained by the sick quitter hypothesis, which proposes that individuals become abstinent because of the physical or mental health consequences of heavy drinking [65]. It may be that those with poor mental health use health risk behaviours as a coping mechanism, such as smoking or heavy drinking, or health risk behaviours may be a consequence of having poor mental health, for example, not feeling motivated to exercise or eat healthily.
Regarding job strain, existing evidence in police employees showed that those reporting high strain (compared to low strain) had reduced odds of heavy drinking [25, 66], contradicting previous evidence [67]. The present findings can disentangle these unexpected findings, as police employees reporting high strain were more likely to be low risk drinkers but engage in other health risk behaviours. High demands and low control may reduce free time to eat healthily [45] or exercise regularly [68]. However, the current evidence-base is limited and mixed. Some research links high strain with smoking, and high control with high physical activity [69], with other research showing weak and inconsistent associations between high strain and health risk behaviours across samples [17]. Nevertheless, high strain is consistently associated with poor mental health [70] and increased days of sickness absence due to poor mental health [71]. In line with this, police employees in the “low risk drinkers but other health risk behaviours” class, characterised by high strain, also showed strong associations with probable depression and sickness absence, more so for men.
Sociodemographic and occupational contributors
Male and female police employees engaging in multiple health risk behaviours were characterised by older age, lower educational attainment, having served longer in the police service, and having several days of sickness absence in the past year. These factors were previously found to be associated with harmful alcohol use in the same sample [25], and can now be linked to co-occurring health risk behaviours, such as smoking and poor diet. Conversely, police employees who were low risk drinkers but reported other health risk behaviours were characterised by younger age and fewer than five years in service, in line with findings from the UK general population, indicating a decline in youth drinking [72]. There were some gender differences in the characteristics of the classes. For example, having children was unrelated to class membership in men, but having no children (compared to one or two) was associated with moderate health risk behaviours in women. Compared to the healthiest class, all other classes were characterised by lower educational attainment. The link between low education and health risk behaviours is well-established [5, 73]. However, the specific pathways in which education influences health behaviours are complex and could be attributed to a range of economic and/or social inequalities [74].
Strengths and limitations
This is the first study to determine classes of health risk behaviours in police employees, and one of few studies examining their mental health associations, in any population. This study utilised a representative sample with a good response rate and sufficient data to stratify by gender. Using LCA, this study determined co-occurring health risk behaviours and their associations, contrasting previous literature researching health risk behaviours independently [61]. However, these findings may not be the same for other occupational groups, given the specific nature of policing (e.g., expected level of physical fitness, time spent driving). Due to the cross-sectional nature of the data, temporal associations could not be determined, and it is unknown whether poor mental health is a contributor or consequence of engaging in health risk behaviours. Existing longitudinal evidence found associations with poor mental health and subsequent health risk behaviours but not vice versa [75], and this should be explored in police employees. This analysis is further limited, as the use of secondary data meant that only the available items could be included, and additional health risk behaviours (e.g., sleep quality) could not be explored.
Implications
This study emphasises the importance of developing interventions which target co-occurring health risk behaviours, as individual behaviours have adverse physical and/or mental health consequences, but the combined impact of multiple health risk behaviours is much greater [57, 76, 77]. According to transfer theory, interventions should target co-occurring behaviours that are similar in their nature [78], as individuals are more likely to transfer their knowledge from one behaviour change to another if the behaviours share similar domains (relating to TTI [9]). Police employees experiencing poor mental health may engage in multiple health risk behaviours and workplace mental health support should incorporate a whole person approach, facilitating ones’ physical and mental health needs [79]. The workplace offers an advantageous environment for interventions targeting health risk behaviours, given the amount of time spent working [80, 81]. At an organisational level, health promotion campaigns can encourage healthy eating, smoking cessation, and physical activity. Addressing demand-control imbalances could allow more free time to for health behaviours. This study identified the characteristics of police employees who may be more likely to engage in multiple health risk behaviours and can be targeted by workplace interventions at an individual level.
Conclusions
This is the first study to determine how health risk behaviours cluster in police employees, and their associations with mental health and job strain. Police employees with poor mental health were more likely to engage in multiple health risk behaviours, than those without a mental health problem. Those reporting high strain were more likely to be low risk drinkers but engage in other health risk behaviours, such as low physical activity and poor diet, than those reporting low strain. These findings highlight the importance of targeting co-occurring, not just individual, health risk behaviours to prevent physical and/or mental health consequences.
Availability of data and materials
The data that support the findings of this study are available through a formal application process (https://police-health.org.uk/applying-access-resource), but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available.
References
Cockerham WC. Health behavior. The wiley blackwell encyclopedia of health, illness, behavior, and society. 2014:764–6.
World Health Organization. Global health risks: mortality and burden of disease attributable to selected major risks: World Health Organization; 2009.
World Health Organization. The global burden of disease: 2004 update: World Health Organization; 2008.
Schuit AJ, van Loon AJM, Tijhuis M, Ocké MC. Clustering of lifestyle risk factors in a general adult population. Prev Med. 2002;35(3):219–24.
Meader N, King K, Moe-Byrne T, Wright K, Graham H, Petticrew M, et al. A systematic review on the clustering and co-occurrence of multiple risk behaviours. BMC Public Health. 2016;16(1):1–9.
McAloney K, Graham H, Law C, Platt L. A scoping review of statistical approaches to the analysis of multiple health-related behaviours. Prev Med. 2013;56(6):365–71.
Noble N, Paul C, Turon H, Oldmeadow C. Which modifiable health risk behaviours are related? A systematic review of the clustering of Smoking, Nutrition, Alcohol and Physical activity (‘SNAP’) health risk factors. Prev Med. 2015;81:16–41.
Atorkey P, Byaruhanga J, Paul C, Wiggers J, Bonevski B, Tzelepis F. Multiple health risk factors in vocational education students: A systematic review. International Journal of Environmental Eesearch & Public Health. 2021;18(2):637.
Flay B, Patraitis J. The theory of triadic influence. Adv Med Sociol. 1994;4:19–44.
Kritsotakis G, Psarrou M, Vassilaki M, Androulaki Z, Philalithis AE. Gender differences in the prevalence and clustering of multiple health risk behaviours in young adults. J Adv Nurs. 2016;72(9):2098–113.
Birch J, Petty R, Hooper L, Bauld L, Rosenberg G, Vohra J. Clustering of behavioural risk factors for health in UK adults in 2016: a cross-sectional survey. J Public Health. 2019;41(3):e226–36.
Vermeulen-Smit E, Ten Have M, Van Laar M, De Graaf R. Clustering of health risk behaviours and the relationship with mental disorders. J Affect Disord. 2015;171:111–9.
Conry MC, Morgan K, Curry P, McGee H, Harrington J, Ward M, et al. The clustering of health behaviours in Ireland and their relationship with mental health, self-rated health and quality of life. BMC Public Health. 2011;11(1):692.
Oftedal S, Kolt GS, Holliday EG, Stamatakis E, Vandelanotte C, Brown WJ, et al. Associations of health-behavior patterns, mental health and self-rated health. Prev Med. 2019;118:295–303.
Jones F, Kinman G, Payne N. Work stress and health behaviors: A work-life balance issue. Work-life balance: A psychological perspective. 2006:185–215.
Payne N, Kinman G, Jones F. Work, stress and health behaviors. Contemporary occupational health psychology: Global perspectives on research and practice. 2012;2:239–55.
Lallukka T, Lahelma E, Rahkonen O, Roos E, Laaksonen E, Martikainen P, et al. Associations of job strain and working overtime with adverse health behaviors and obesity: evidence from the Whitehall II Study, Helsinki Health Study, and the Japanese Civil Servants Study. Soc Sci Med. 2008;66(8):1681–98.
Lallukka T, Sarlio-Lähteenkorva S, Roos E, Laaksonen M, Rahkonen O, Lahelma E. Working conditions and health behaviours among employed women and men: the Helsinki Health Study. Prev Med. 2004;38(1):48–56.
Karasek RA Jr. Job demands, job decision latitude, and mental strain: Implications for job redesign. Adm Sci Q. 1979;24(2):285–308.
Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56(2):267.
Aspinwall LG, Taylor SE. A stitch in time: Self-regulation and proactive coping. Psychol Bull. 1997;121(3):417.
Gershon RR, Barocas B, Canton AN, Li X, Vlahov D. Mental, physical, and behavioral outcomes associated with perceived work stress in police officers. Crim Justice Behav. 2009;36(3):275–89.
Papazoglou K, Andersen JP. A guide to utilizing police training as a tool to promote resilience and improve health outcomes among police officers. Traumatology: An International Journal. 2014;20(2):103.
Sterud T, Hem E, Ekeberg Ø, Lau B. Occupational stress and alcohol use: a study of two nationwide samples of operational police and ambulance, personnel in Norway. J Stud Alcohol Drugs. 2007;68(6):896–904.
Irizar P, Gage S, Fallon V, Field M, Goodwin L. The prevalence of hazardous and harmful alcohol use in the UK Police Service and the co-occurrence of mental health problems and job strain. Epidemiology & Psychiatric Sciences. 2021;30:E51.
Laska MN, Pasch KE, Lust K, Story M, Ehlinger E. Latent class analysis of lifestyle characteristics and health risk behaviors among college youth. Prev Sci. 2009;10(4):376–86.
Atorkey P, Paul C, Wiggers J, Bonevski B, Nolan E, Oldmeadow C, et al. Clustering of multiple health-risk factors among vocational education students: a latent class analysis. Translational Behavioral Medicine. 2021;11(10):1931–40.
Liao J, Mawditt C, Scholes S, Lu W, Umeda M, Muniz Terrera G, et al. Similarities and differences in health-related behavior clustering among older adults in Eastern and Western countries: A latent class analysis of global aging cohorts. Geriatr Gerontol Int. 2019;19(9):930–7.
Mawditt C, Sacker A, Britton A, Kelly Y, Cable N. The clustering of health-related behaviours in a British population sample: testing for cohort differences. Prev Med. 2016;88:95–107.
Elliott P, Vergnaud A-C, Singh D, Neasham D, Spear J, Heard A. The Airwave Health Monitoring Study of police officers and staff in Great Britain: rationale, design and methods. Environ Res. 2014;134:280–5.
Allen G, Audickas L. Police Service Strength Briefing Paper No. SN-00634. London: House of Commons Library. 2020.
Department of Health and Social Care. UK Chief Medical Officers' low risk drinking guidelines. Department of Health.; 2016.
NICE. Alcohol-use disorders: preventing harmful drinking. Evidence update March 2014. National Institute for Health Care Excellence (NICE); 2014.
Jones SE, Kann L, Pechacek TF. Cigarettes smoked per day among high school students in the US, 1991–2009. Am J Prev Med. 2011;41(3):297–9.
IPAQ-SF. Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ) - short and long forms.; 2015.
Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–95.
Prince SA, Reid RD, Bernick J, Clarke AE, Reed JL. Single versus multi-item self-assessment of sedentary behaviour: A comparison with objectively measured sedentary time in nurses. J Sci Med Sport. 2018;21(9):925–9.
Puciato D, Rozpara M, Mynarski W, Oleśniewicz P, Markiewicz-Patkowska J, Dębska M. Physical activity of working-age people in view of their income status. BioMed research international. 2018;2018:8298527.
Department of Health and Social Care. Physical activity guidelines: UK chief medical officers' report, 2019. 2019.
Public Health England. The eatwell guide. Public Health England London; 2016.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–70.
Brewin CR, Rose S, Andrews B, Green J, Tata P, McEvedy C, et al. Brief screening instrument for post-traumatic stress disorder. Br J Psychiatry. 2002;181(2):158–62.
Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3(4):322.
Gibson R, Eriksen R, Singh D, Vergnaud A-C, Heard A, Chan Q, et al. A cross-sectional investigation into the occupational and socio-demographic characteristics of British police force employees reporting a dietary pattern associated with cardiometabolic risk: findings from the Airwave Health Monitoring Study. Eur J Nutr. 2018;57(8):2913–26.
Lazarsfeld PF. The logical and mathematical foundation of latent structure analysis. Studies in Social Psychology in World War II Vol IV: Measurement and Prediction. 1950:362–412.
Akaike H. Factor analysis and AIC. Selected papers of hirotugu akaike: Springer; 1987. p. 371–86.
Gideon S. Estimating the dimension of a model. Ann Stat. 1978;6(2):461–4.
Sclove SL. Application of model-selection criteria to some problems in multivariate analysis. Psychometrika. 1987;52(3):333–43.
Ramaswamy V, DeSarbo WS, Reibstein DJ, Robinson WT. An empirical pooling approach for estimating marketing mix elasticities with PIMS data. Mark Sci. 1993;12(1):103–24.
Maydeu-Olivares A, Joe H. Limited information goodness-of-fit testing in multidimensional contingency tables. Psychometrika. 2006;71(4):713.
Lo Y, Mendell NR, Rubin DB. Testing the number of components in a normal mixture. Biometrika. 2001;88(3):767–78.
Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Struct Equ Modeling. 2007;14(4):535–69.
Boeschoten L, Oberski DL, de Waal T. Estimating classification error under edit restrictions in combined survey-register data. CBS Discussion Paper 2016 12; Den Haag: Statistics Netherlands2016.
Schreiber JB, Pekarik AJ. Using Latent Class Analysis versus K‐means or Hierarchical Clustering to understand museum visitors. Curator: The Museum Journal. 2014;57(1):45–59.
Clark SL, Muthén B. Relating latent class analysis results to variables not included in the analysis. 2009.
Akasaki M, Ploubidis GB, Dodgeon B. Bonell CPJJoa. The clustering of risk behaviours in adolescence and health consequences in middle age. 2019;77:188–97.
Oyebode O, Gordon-Dseagu V, Walker A, Mindell JS. Fruit and vegetable consumption and all-cause, cancer and CVD mortality: analysis of Health Survey for England data. J Epidemiol Community Health. 2014;68(9):856–62.
Souza RVd, Sarmento RA, Almeida JCd, Canuto R. The effect of shift work on eating habits: a systematic review. Scandinavian Journal of Work, Environment, Health. 2019;45(1):7–21.
Kwan M, Arbour-Nicitopoulos K, Duku E, Faulkner G. Patterns of multiple health risk–behaviours in university students and their association with mental health: application of latent class analysis. Health promotion and chronic disease prevention in Canada: research, policy and practice. 2016;36(8):163.
Stranges S, Samaraweera PC, Taggart F, Kandala N-B, Stewart-Brown S. Major health-related behaviours and mental well-being in the general population: the Health Survey for England. BMJ open. 2014;4(9):e005878.
Puddephatt J-A, Jones A, Gage SH, Fear NT, Field M, McManus S, et al. Associations of alcohol use, mental health and socioeconomic status in England: findings from a representative population survey. Drug Alcohol Depend. 2020;219: 108463.
El-Guebaly N. Investigating the association between moderate drinking and mental health. Ann Epidemiol. 2007;17(5):S55–62.
Goodwin L, Norton S, Fear N, Jones M, Hull L, Wessely S, et al. Trajectories of alcohol use in the UK military and associations with mental health. Addict Behav. 2017;75:130–7.
Shaper AG, Wannamethee G, Walker M. Alcohol and mortality in British men: explaining the U-shaped curve. The Lancet. 1988;332(8623):1267–73.
Siegrist J, Rödel A. Work stress and health risk behavior. Scand J Work Environ Health. 2006;26(6):473–81.
Heikkilä K, Nyberg ST, Fransson EI, Alfredsson L, De Bacquer D, Bjorner JB, et al. Job strain and alcohol intake: a collaborative meta-analysis of individual-participant data from 140 000 men and women. 2012;7(7):e40101.
Kouvonen A, Kivimäki M, Elovainio M, Virtanen M, Linna A. Vahtera JJPm. Job strain and leisure-time physical activity in female and male public sector employees. 2005;41(2):532–9.
Hellerstedt WL, Jeffery RW. The association of job strain and health behaviours in men and women. Int J Epidemiol. 1997;26(3):575–83.
Burns RA, Butterworth P, Anstey KJ. An examination of the long-term impact of job strain on mental health and wellbeing over a 12-year period. Soc Psychiatry Psychiatr Epidemiol. 2016;51(5):725–33.
Mather L, Bergström G, Blom V, Svedberg P. High job demands, job strain, and Iso-strain are risk factors for sick leave due to mental disorders: a prospective Swedish twin study with a 5-year follow-up. J Occup Environ Med. 2015;57(8):858–65.
Oldham M, Callinan S, Whitaker V, Fairbrother H, Curtis P, Meier P, et al. The decline in youth drinking in England—is everyone drinking less? A quantile regression analysis Addiction. 2020;115(2):230–8.
Cutler DM. Lleras-Muney AJJohe. Understanding differences in health behaviors by education. 2010;29(1):1–28.
Raghupathi V, Raghupathi W. The influence of education on health: an empirical assessment of OECD countries for the period 1995–2015. J Archives of Public Health. 2020;78:1–18.
Walsh JL, Senn TE. Carey MPJTbm. Longitudinal associations between health behaviors and mental health in low-income adults. 2013;3(1):104–13.
Spring B, Moller AC, Coons MJJJoph. Multiple health behaviours: overview and implications. 2012;34(suppl_1):i3-i10.
Bellis MA, Hughes K, Nicholls J, Sheron N, Gilmore I, Jones L. The alcohol harm paradox: using a national survey to explore how alcohol may disproportionately impact health in deprived individuals. BMC Public Health. 2016;16(1):1–10.
Perkins D, Salomon G. Transfer of Learning. In: Husen T, Postlethwaite T, editors. The International Encyclopedia of Education. 11. 2nd Ed. ed. Oxford: Pergamon; 1992. p. 6452–7.
Vreeland BJTJocp. Bridging the gap between mental and physical health: a multidisciplinary approach. 2007;68(suppl 4):26–33.
Goldgruber J, Ahrens D. Effectiveness of workplace health promotion and primary prevention interventions: a review. J Public Health. 2010;18(1):75–88.
Malik SH, Blake H, Suggs LS. A systematic review of workplace health promotion interventions for increasing physical activity. Br J Health Psychol. 2014;19(1):149–80.
Acknowledgements
This research has been conducted using the Airwave Study Tissue Bank Resource. We thank all participants in the Airwave Study for their contribution. We would also like to thank Andy Heard, He Gao and Maria Aresu from the Airwave Health Monitoring Study Research team for the provision of the data and data management support over the course of this project.
Funding
This work was part of Patricia Irizar’s PhD studentship, which is funded by the Economic and Social Research Council and North West Social Science Doctoral Training Partnership (Grant Number: ES/P000665/1). The studentship is part funded by the charity Alcohol Change UK. The funders had no role in the study design, collection, analysis, or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
PI conceptualised and designed the study and pre-registered the study with Open Science Framework. PI conducted the data analysis and interpreted the findings; wrote the initial manuscript, reviewed and revised the manuscript; and approved the final manuscript as submitted. SHG and VF reviewed and revised the manuscript; and approved the final manuscript as submitted. LG provided extensive feedback and supervision; contributed to conceptualisation of the study design and formal analysis; reviewed and revised the manuscript; and approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Airwave Health Monitoring Study received ethical approval from the National Health Service multi-site research ethics committee (MREC/13/NW/0588). Written informed consent was obtained from all subjects. All methods were performed in accordance with the Declaration of Helsinki.
Consent for publication
Written informed consent for publication was obtained from all subjects.
Competing interests
All authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Table S1. Descriptive statistics for the sociodemographic and occupational variables (N = 40,986). Table S2. Multinomial logistic regressions exploring the sociodemographic and occupational associations with the identified classes of health (risk) behaviours for men (N = 25,788). Percentages are weighted with conditional probability weights. Unadjusted multinomial odds ratios (MOR) with 95% confidence intervals (CIs) are shown. Table S3. Multinomial logistic regressions exploring the sociodemographic and occupational associations with the identified classes of health (risk) behaviours for women (N = 15,198). Percentages are weighted with conditional probability weights. Unadjusted multinomial odds ratios (MOR) with 95% confidence intervals (CIs) are shown. Fig S1. Plot showing AIC, BIC, and SSABIC model fit criteria for each additional class.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Irizar, P., Gage, S.H., Fallon, V. et al. A latent class analysis of health risk behaviours in the UK Police Service and their associations with mental health and job strain. BMC Psychiatry 22, 426 (2022). https://doi.org/10.1186/s12888-022-04054-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-022-04054-3