Abstract
Background
Previous studies have shown escitalopram is related to sleep quality. However, effects of escitalopram on dynamics of electroencephalogram (EEG) features especially during different sleep stages have not been reported. This study may help to reveal pharmacological mechanism underlying escitalopram treatment.
Methods
The spatial and temporal responses of patients with major depressive disorder (MDD) to escitalopram treatment were analyzed in this study. Eleven MDD patients and eleven healthy control subjects who completed eight weeks’ treatment of escitalopram were included in the final statistics. Six-channel sleep EEG signals were acquired during sleep. Power spectrum and nonlinear dynamics were used to analyze the spatio-temporal dynamics features of the sleep EEG after escitalopram treatment.
Results
For temporal dynamics: after treatment, there was a significant increase in the relative energy (RE) of δ1 band (0.5 - 2 Hz), accompanied by a significant decrease in the RE of β2 band (20 - 30 Hz). Lempel-Ziv complexity and Co - complexity values were significantly lower. EEG changes at different sleep stages also showed the same regulation as throughout the night sleep. For spatio dynamics: after treatment, the EEG response of the left and right hemisphere showed asymmetry. Regarding band-specific EEG complexity estimations, δ1 and β2 in stage-1 and δ1 in stage-2 sleep stage in frontal cortex is found to be much more sensitive to escitalopram treatment in comparison to central and occipital cortices.
Conclusions
The sleep quality of MDD patients improved, EEG response occurred asymmetry in left and right hemispheres due to escitalopram treatment, and frontal cortex is found to be much more sensitive to escitalopram treatment. These findings may contribute to a comprehensive understanding of the pharmacological mechanism of escitalopram in the treatment of depression.
Similar content being viewed by others
Background
Major depressive disorder (MDD) is one of the most common diseases worldwide and is responsible for premature deaths and disability [7]. In the past, MDD patients have been treated mainly with traditional drugs such as monoamine oxidase inhibitors, or tricyclic and heterocyclic antidepressants [20, 43]. These traditional drugs have some disadvantages such as weak tolerance, large adverse effects and slow action onset. Escitalopram is a highly selective SSRI and therapeutically active S-enantiomer of citalopram, it has been widely used and recommended by clinicians worldwide [5]. Compared to other antidepressants, escitalopram is tolerated better, has fewer adverse effects and has a faster onset of action [5, 27, 36, 39]. However, its pharmacological mechanism has not yet been clarified completely.
Previous study has shown escitalopram can improve sleep quality in MDD patients [29], and was efficacious in treating depressive symptoms in depressed patients suffering from poor sleep quality, and this beneficial effect appeared to be independent of the severity of the patient’s sleep problems [30]. Furthermore, it has been reported that escitalopram is advantageous in the treatment of the core symptoms of MDD, including sleep disturbance [42]. Sleep is a complicated process, and can be divided into different stages both temporally, and spatially, and is related to multiple interactions between different brain regions. Therefore, it is necessary to explore the pharmacological mechanism underlying the action of escitalopram, and to investigate the relationship between escitalopram and sleep in both temporal and spatial dimensions. However, until now, there have been few studies involving both temporal and spatial dimensions, only research involving the eye close and open condition [8]. Currently there are questions still to be resolved, such as whether escitalopram acts the same at each sleep stage, or is specific to certain stages. Also it remains unclear as to whether escitalopram is brain region specific such as the frontal, central, or occipital cortices or displays asymmetries in brain hemispheres.
Electroencephalography (EEG) is a suitable option as a neurophysiological biomarker, and displays several advantages, including higher temporal resolution, non-invasiveness, ease of access and low cost [15, 33]. As a result this method has been widely used for the biomedical investigation of several mental illnesses including MDD, Alzheimer’s disease and others [1, 2, 6, 22]. EEG signals can be analyzed by linear and non-linear dynamic analyses. Linear analysis such as power spectrum is commonly used to extract the features of sleep EEG signals [13, 26, 40, 44]. Spectral characteristic parameters can reflect the energy information transported by each frequency band. Because the brain is a complex non-linear system, the use of non-linear dynamic analysis may also be used to reflect brain states accurately [24, 25, 35]. Among the non-linear features, complexity is suitable as it can be calculated within a short time series and fast speed.
In the present study, we investigated the spatio-temporal dynamics of sleep EEG features before and after escitalopram treatment. Both linear and non-linear dynamic analyses may provide a more comprehensive understanding of the pharmacological mechanism of escitalopram in the treatment of depression.
Methods
Participants
A total of 58 subjects participated in the study, which included 30 MDD patients and 28 healthy controls. However, more than half of MDD patients were excluded from the final analysis because their electrode became detached, more than half of healthy controls were eliminated because their sleep time was less than 6.5 h on the experimental night. Finally, 11 healthy male adult controls and 11 male MDD patients completed the study. The MDD patients ages’ ranged from 22 to 40 years (mean ± SD: 30.64 ± 5.52 years). These patients reported no history of any other psychiatric disorder or prior take of antidepressants. All patients, were from The Peking University Sixth Hospital, and met the criteria for major depression defined in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) [3]. Diagnosis was established by experienced psychiatrists using the Structured Clinical Interview for DSM-5: Research Version (SCID) [18]. A minimum score of 22 points on the 17 item Hamilton Depression Scale (HRSD - 17) [41] was required to be enrolled in the study. Professional scorers from the Peking University Sixth Hospital conducted the HRSD measurements two times. The first time occurred before the treatment of escitalopram, and the second time occurred on day 57 of escitalopram treatment. The exclusion criteria included: (1) age < 18 or 45 > years, (2) presence of additional psychotic symptoms, (3) cognitive impairment or personality disorders, (4) history of other mental illness, (5) suicidal ideation or behaviors.
Control participants included 11 physically and mentally healthy male volunteers whose ages were between 22 and 38 years (mean ± SD: 27.72 ± 4.79 years). The inclusion criteria included: (1) self-reported good sleep and PSQI < 5, matched age with MDD, (2) absence of psychiatric illnesses diagnosed by the DSM-5 criteria, (3) a maximum score of 7 points on the 17 - item HRSD, (4) a maximum score of 7 points on the 14 - item Hamilton Anxiety Scale (HAMA) [34], (5) 18 ≤ BMI < 30.
The exclusion criteria included: (1) any of the exclusion criteria for the MDD group, (2) any past or present history of mental illness that met DSM-5 diagnostic criteria, (3) current or pass chronic physical diseases (e.g., cardiovascular disease, diabetes, rheumatoid arthritis, et al.), (4) shift worker within the preceding year, (5) jet lag travel in the last 2 weeks, (5) total sleep time < 6.5 h.
All of the participants were Han Chinese. They signed written informed consent forms before participation. The study was approved by the ethics committee of Peking University Sixth Hospital, Beijing, China, in accordance with the Helsinki Declaration.
Polysomnographic recording
All the depressive patients underwent polysomnographic recording two times. The first time conducted before the treatment of escitalopram, and the second time conducted on day 57 of escitalopram treatment.
Overnight polysomnographic recording included electroencephalography (EEG; including F3, F4, C3, C4, O1, and O2, with reference to the contralateral mastoid; International10 - 20system), electrooculography (EOG), electromyography (EMG), and electrocardiography (ECG). The signals were digitized at a sampling rate of 256 Hz, and an electrode impedance < 5 KΩ. Thirty - second epochs were used for manual analysis, and sleep stages were scored offline according to the criterion of the American Academy of Sleep Medicine (AASM) [9], using the standard polysomnographic sleep recordings.
EEG signal processing
In the processing environment of MATLAB R2016b, using EEGLAB toolkits (University of California San Diego), power frequency interference was eliminated by using a 50 Hz notch, and data was filtered from 0.5 to 30 Hz by using band pass filter [16]. Each sample had corresponding sleep staging files. However, because the sample duration data was too large, and some data frames had large artifacts, we chose the entire artifact - free frames (30 s) from every sleep type (including Wake, rapid-eye-movement (REM), stage-1, stage-2 (including sleep spindles) and stage-3) according to sleep staging files.
The EEG signal processing includes two aspects: linear analysis and nonlinear dynamic analysis.
Linear analysis: power spectrum
The power spectrum reflects the energy information carried by the brain waves in each frequency band. According to the frequency, the EEG signals are divided into several categories: δ1 (0.5 - 2 Hz), δ2 (2 - 4 Hz), θ (4 - 8 Hz), α (8 - 13 Hz), β1 (13 - 20 Hz) and β2 (20 - 30 Hz) [14]. A previous study revealed that during the night, the frequencies of the most powerful waves are concentrated in the 0.5–2 Hz range and show a continuous tendency to shift towards slower frequencies during sleep. So we divided the delta band into low-delta (0.5–2 Hz) and high-delta (2 - 4 Hz )[31]. In the present study, each frequency band power was obtained by using fast Fourier transform (FFT) analysis [17, 38, 45]. FFT calculation was performed on 3 s non-overlapping consecutive window (Hamming window). The average values of the different sleep stages were computed form the 30 s of data obtained previously. In order to reduce specific individual differences, the relative energy (RE) was computed. The RE corresponds to the ratio between the power value of each frequency band and the sum of the power values in the following calculation:
Nonlinear dynamic analysis: LZC, C0C
Correlation dimension, complexity, entropy and Lyapunov exponents are common non-linear features in EEG signal analysis. Correlation dimension and Lyapunov exponents require large data sets and strict dimensional measurements which are not suitable for EEG analysis. Whereas Lempel-Ziv Complexity (LZC) and Co-complexity (C0C) are more suitable, because they require small datasets and have high computation speeds. Therefore, in the present study, LZC and C0C were used to characterize the sleep state of patients with MDD. LZC represents the rate of appearance of a new pattern in a time series from a one dimensional perspective [32]. A ratio of the area of the disorder component over the area of the original time series is considers as a complexity measurement, which is denoted as C 0[12]. The higher the LZC, the more likely it is that a new model will appear, highlighting complex dynamic behavior. The higher the C0C, the more probability there is that random motion may appear.
In order to obtain 28 s sequences, the first and last second of each of them were removed from the 30 s previously selected sequences. This shortened sequence was then divided into 7 segments of 4 s each for targeted analysis. For each of those time-windows we considered as important EEG features, the mean of the values by itself as well as the characteristic of values according to the sleep stage.
Statistical analysis
All analyses were performed using the SPSS Statistics version 22.0. We used the paired-samples t-test to investigate the changes in the EEG characteristic parameters between the baseline (before treatment) and the final (after treatment) session, and the independent-sample t-test to compare the results from the patients with MDD and healthy control subjects. We then used the paired-samples t-test to analyze differences between the left and right hemispheres of the cortex. The differences of EEG characteristics in different brain regions (frontal, central, occipital) between baseline and final were analyzed by one-way ANOVA. Differences were considered significant when P < 0.05.
Results
EEG response before and after escitalopram treatment of the whole night sleep
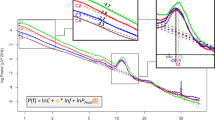
We investigated the EEG response for MDD patients (before and after escitalopram treatment) and healthy control subjects in the spatial and temporal dimensions. For temporal dynamic analysis, firstly, we compared the RE (average value of six channels) of different EEG frequency bands of the whole night sleep between MDD patients (before and after escitalopram treatment) and healthy control subjects. Figure 1 (a & b) indicate that after treatment, the RE of the δ1 band was significantly higher than that before treatment (t(10) = − 2.397, p = 0.028). The RE of the β2 band in patients with MDD before treatment with escitalopram was significantly higher than that in controls (t(20) = 2.513, p = 0.045), it was significantly decreased to control level after treatment (t(10) = 2.513, p = 0.045). Additionally, the RE of other frequency bands in MDD patients also had some improvement after treatment, but not statistically significant.
EEG response before and after escitalopram treatment during the whole night sleep. a Relative energy (RE) in the δ1 band; b RE of other frequency bands (except delta1); c LZC values; d C0C values; The data are expressed as mean ± SD. n = 11 MDD patients. n = 11 healthy controls. *p < 0.05, different from control, #p < 0.05, different from baseline
Secondly, we analyzed whether there existed differences in non-linear LZC and C0C values (average value of six channels) during the whole night sleep for MDD patients (before and after escitalopram treatment) and healthy control subjects. As detailed in Fig. 1 (c & d), the LZC values in patients before treatment with escitalopram was higher than that in controls (t(20) = 2.963, p = 0.010), it was significantly decreased to control level after treatment (t(10) = 2.626, p = 0.030). Furthermore, the C0C values showed the same regulation as LZC values, the C0C values in patients before treatment with escitalopram was higher than that in controls (t(20) = 2.397, p = 0.028), it was significantly decreased to control level after treatment (t(10) = 2.862, p = 0.007).
EEG response before and after escitalopram treatment at different sleep stages
We compared the changes in RE (average value of six channels) of each frequency bands at different sleep stages in MDD patients (before and after escitalopram treatment) and healthy controls. Firstly, we compared the RE of each frequency bands during different sleep stages. As shown in Fig. 2a, a significant increase in the RE of δ1 band in the stage-1 (t(10) = − 2.239, p = 0.049), stage-2 (t(10) = − 2.923, p = 0.015), and REM (t(10) = − 2.648, p = 0.024) sleep stages after treatment with escitalopram was seen. Additionally, a significant decrease in the RE of δ2 band (t(20) = − 2.371, p = 0.027), and θ band (t(20) = − 2.923, p = 0.004) in the stage-1 in patients with MDD before treatment compared with controls (Fig. 2b and c). A significant decrease of the β2 band in the REM (t(10) = 3.126, p = 0.011) sleep phase in patients with MDD after treatment compared with before treatment (Fig. 2f).
EEG response before and after escitalopram treatment during each sleep stage. a Relative energy (RE) in the δ1 band; b RE in the δ2 band; c RE in the θ band; d RE in the α band; e RE in the β1 band; f RE in the β2 band; g LZC values; h C0C values; The data are expressed as mean ± SD. n = 11 MDD patients. n = 11 healthy controls. *p < 0.05, different from control, #p < 0.05, different from baseline
Secondly, we analyzed for differences in non-linear LZC and C0C values (average value of six channels) at different sleep stages in MDD patients and the healthy control subjects. As shown in Fig. 2g, LZC values in patients with MDD after treatment decreased significantly compared with that before treatment during stage-1 (t(10) = 3.946, p = 0.003), stage-2 (t(10) = 3.527, p = 0.005) and REM (t(10) = 2.920, p = 0.015) sleep stage. While during stage-2 LZC values in patients with MDD before treatment increased significantly compared with that in controls (t (20) = 2.847, p = 0.011). As for the C0C values, during stage-2 showed a significant increase in patients with MDD before treatment compared with that in controls (t(10) = 2.387, p = 0.029) and a significantly decreased in patients with MDD after treatment compared with that before treatment (t(10) = 3.126, p = 0.011) in patients with MDD (Fig. 2h).
EEG response before and after escitalopram treatment in left and right hemispheres
For spatio dynamic analysis, we found differences in EEG features between left and right hemispheres in MDD patients (before and after escitalopram treatment). EEG features of left hemisphere were average values of three channels including F3, C3, and O1; EEG features of right hemisphere were average values of another three channels including F4, C4, and O2. Firstly, we analyzed for differences in the RE between left and right hemispheres during different sleep stages. As shown in Fig. 3a, the RE of the δ1 band during stage-2 in the right hemisphere greater significantly compared with that in the left hemisphere (t(10) = − 2.626, p = 0.030) after escitalopram treatment. In Fig. 3c, during the stage-1 sleep stage, the RE of the θ band in the left hemisphere was significantly higher than that in the right hemisphere (t(10) = − 2.626, p = 0.017) after escitalopram treatment. In Fig. 3f, during the REM stage, the β2 band in the right hemisphere showed a significant decrease compared with that in the left hemisphere (t(10) = 2.302, p = 0.05) after escitalopram treatment.
EEG response before and after escitalopram treatment in left and right hemispheres at different sleep stages. a Relative energy (RE) in the δ1 band; b RE in the δ2 band; c RE in the θ band; d RE in the α band; e RE in the β1 band; f RE in the β2 band; g LZC values; h C0C values. The data are expressed as mean ± SD. n = 11 MDD patients. n = 11 healthy controls. #p < 0.05, different from final - left
Secondly, we also explored differences in non-linear LZC and C0C values between left and right hemispheres during different sleep stages. As shown in Fig. 3g, during the REM sleep stage, the LZC values did not differ between the left and right hemispheres before treatment. However, a significant decrease in the LZC value in the right hemisphere compared with that in the left (t(10) = 4.632, p = 0.001) was found after escitalopram treatment.
EEG response among different brain regions
Since escitalopram treatment may have brain region - specific effects, we investigated the EEG response in different cortical areas (frontal, central and occipital) in MDD patients (before and after treatment). EEG features of frontal cortex were average values of two channels including F3 and F4; EEG features of central cortex were average values of two channels including C3 and C4; EEG features of occipital cortex were average values of two channels including O1 and O2.
We found significant changes in the frontal cortex in stage-1, stage-2 and REM sleep stage after treatment. As shown in Fig. 4, for stage-1, we found that the δ1 band RE significantly greater (F(2,30) = 6.961, p = 0.003) in the frontal cortex compared with that in the central and occipital cortices, which illustrated by warmer colors in the frontal lobe. In the same sleep stage, the β2 band RE (F(2,30) = 3.928, p = 0.031) and the non-linear LZC values (F(2,30) = 6.176, p = 0.006) in the frontal cortex significantly smaller compared with that in the central and occipital cortices, which illustrated by colder colors in the frontal cortex.
For the stage-2 and REM sleep stages, the δ1 band RE significantly greater in the frontal cortex, (stage-2: F(2,30) = 6.863, p = 0.004); REM: (F(2,30) = 5.740, p = 0.008), which illustrated by warmer colors in the frontal lobe. These results showed a more intense EEG response in the frontal cortex than that in any other brain regions.
Discussion
With regard to temporal dynamics study, power spectrum results showed that after treatment, the δ1 band RE significant increased, whereas the β2 band RE significantly decrease. Previous studies have found that the δ1 band was seen during phases of reduced alertness and sleep [28]. The β2 frequency range is thought to reflect behavioral arousal and attention processes [21, 37]. Therefore, an increase in the δ1 band and a decrease in the β2 band may be consistent with an improved sleep quality.
It is notable that after escitalopram treatment, non-linear LZC and C0C values also showed a significant overall decrease in different sleep stages and throughout the night sleep. A decrease in LZC and C0C values may correspond to a decrease in brain wave activity and an increase in lethargy. Therefore, the non-linear dynamic features also revealed that escitalopram can improve sleep quality in MDD patients. Until now, there have been few reports looking at changes in non-linear LZC and C0C values before and after escitalopram treatment, especially during the sleep process.
The right and left side of the brain are asymmetric in anatomy and function. A previous review electrophysiological (EEG and event-related potential), behavioral (dichotic and visual perceptual asymmetry), and neuroimaging (PET, MRI, NIRS) evidence of right-left asymmetry in depressive disorders [10]. Our spatial dynamic study also found that after escitalopram treatment, sleep EEG responses in the left and right hemispheres were asymmetrical. For the stage-1, the RE of θ band in the left hemisphere was higher than that in the right. Given the association between θ band activity and rostral anterior cingulate cortex activity, an asymmetry in θ activity may reflect rapid escitalopram - induced activity within the default mode network. This in turn may indicate continued re-establishment of fronto - cingulate connections, which may be required to relieve depressive symptoms.
For the stage-2, the RE of δ1 band in the right hemisphere was significant higher than that in the left after escitalopram treatment. This result is in line with that of Baskaran’s research looking at power spectrum changes under closed eye conditions. In which Baskaran et al. found that escitalopram responders showed greater delta power in the right hemisphere at 2-week of escitalopram treatment [8]. Additionally, right lateralization of delta in escitalopram responders are similar to reports of increased slow wave activity in the right hemisphere in MDD patients [23]. Therefore, this feature may reflect a subtype of MDD patients that respond well to escitalopram.
For the REM sleep stage, the RE of β2 band was lower in the right hemisphere than that in the left after escitalopram treatment. Previous research has found that the EEG beta power has been shown to have a temporal association with cortisol secretion suggesting a mechanistic link between increased hypothalamic - pituitary - adrenal function and higher frequency brain activation [11]. In addition, changes in beta asymmetry observed in the patients after escitalopram treatment may reflect antidepressant induced variations in arousal. Differences in LZC values between the right and left hemispheres in reaction to escitalopram treatment have not yet been explored. In our study, the LZC values of the right hemisphere were lower than that in the left hemisphere during the REM sleep stage after escitalopram treatment. The neurobiological basis of this finding in the context of response to escitalopram treatment is poorly understood, and this finding needs to be further explored and verified in a wider range of studies.
Spatial dynamic research of brain region-specific targets demonstrates that after escitalopram treatment, the frontal cortex showed a more intense EEG response compared with the central, and occipital cortices. Previous research has found that the frontal lobe has a regulatory role in emotional cognition [19]. The prefrontal cortex is rich in 5-HT2A receptors, and pharmacological studies have shown that 5-HT2A receptors are involved in antidepressant behaviors [4], and that they may play an antidepressant role by increasing the release of 5-HT. Therefore, the greater the response of the frontal cortex, may be indicative of a good response to escitalopram treatment in MDD patients.
In summary, the spatio-temporal dynamics of the EEG features during sleep in MDD patients with escitalopram treatment was explored in this study. Our findings may aid in unravelling the mechanisms underlying the action of escitalopram treatment. However, these results were based on a small sample size, and therefore, larger sample size will be needed to verify them for future studies.
Conclusions
The findings presented within this study are encouraging in several aspects. Firstly, temporal dynamics study demonstrated that there appeared an increase in the δ1 band, a decrease in the β2 band, and a decrease in non-linear LZC and C0C values after escitalopram treatment. Secondly, spatial dynamic study indicated that sleep EEG responses in the left and right hemispheres were asymmetrical, the frontal cortex showed a more intense EEG response compared with the central, and occipital cortices. These findings may contribute to a comprehensive understanding of the pharmacological mechanism of escitalopram in the treatment of depression.
Availability of data and materials
All datas are included in this manscript.
References
Abasolo D, Hornero R, Gomez C, Garcia M, Lopez M. Analysis of EEG background activity in Alzheimer's disease patients with Lempel-Ziv complexity and central tendency measure. Med Eng Phys. 2006;28:315–22.
Alhaj H, Wisniewski G, McAllister-Williams RH. The use of the EEG in measuring therapeutic drug action: focus on depression and antidepressants. J Psychopharmacol. 2011;25:1175–91.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5). Washington, D.C: American Psychiatric Publishing; 2013.
Anna CÉ, Lucila K, Pau C, Analía B, Francesc A. 5-HT2A receptors are involved in cognitive but not antidepressant effects of fluoxetine. Eur Neuropsychopharmacol. 2015;25:1353–61.
Azorin JM, Llorca PM, Despiegel N, Verpillat P. Escitalopram is more effective than citalopram for the treatment of severe major depressive disorder. Encephale. 2004;30:158–66.
Babiloni C, Lizio R, Marzano N, Capotosto P, Soricelli A, Triggiani AI, Cordone S, Gesualdo L, Del PC. Brain neural synchronization and functional coupling in Alzheimer's disease as revealed by resting state EEG rhythms. Int J Psychophysiol. 2016;103:88–102.
Baghai TC, Varallo-Bedarida G, Born C, Hafner S, Schule C, Eser D, Zill P, Manook A, Weigl J, Jooyandeh S, Nothdurfter C, von Schacky C, Bondy B, Rupprecht R. Classical risk factors and inflammatory biomarkers: one of the missing biological links between cardiovascular disease and major depressive disorder. Int J Mol Sci. 2018;19(6):1740.
Baskaran A, Farzan F, Milev R, Brenner CA, Alturi S, Pat MM, Blier P, Evans K, Foster JA, Frey BN, Giacobbe P, Lam RW, Leri F, MacQueen GM, Muller DJ, Parikh SV, Rotzinger S, Soares CN, Strother SC, Turecki G, Kennedy SH. The comparative effectiveness of electroencephalographic indices in predicting response to escitalopram therapy in depression: a pilot study. J Affect Disord. 2018;227:542–9.
Berry B, et al. The AASM manual for the scoring of sleep and associated events. In: Rules, Terminology and Technical Specifications. Darien, Illinois: American Academy of Sleep Medicine; 2012. p. 176.
Bruder GE, Stewart JW, McGrath PJ. Right brain, left brain in depressive disorders: clinical and theoretical implications of behavioral, electrophysiological and neuroimaging findings. Neurosci Biobehav Rev. 2017;78:178–91.
Chapotot F, Gronfier C, Jouny C, Muzet A, Brandenberger G. Cortisol secretion is related to electroencephalographic alertness in human subjects during daytime wakefulness. J Clin Endocrinol Metab. 1998;83:4263–8.
Chen F, Xu J, Gu F, Yu X, Meng X, Qiu Z. Dynamic process of information transmission complexity in human brains. Biol Cybern. 2000;83:355–66.
Christian S, Jonathan M, Schmidt R, Mergl F, Ulrich M. Changes in brain arousal (EEG-vigilance) after therapeutic sleep deprivation in depressive patients and healthy controls. Sci Rep. 2018;8:1–10.
Cheng Q, Yang W, Liu K, Zhao W, Wu L, Lei L, Dong T, Hou N, Yang F, Qu Y, Yang Y. Increased sample entropy in EEGs during the functional rehabilitation of an injured brain. Entropy. 2019;21:698.
de Aguiar Neto FS, Rosa JLG. Depression biomarkers using non-invasive EEG: a review. Neurosci Biobehav Rev. 2019;105:83–93.
Delorme A, Makeig S. EEGLAB: an open source toolbox for analysis of single-trial EEG dynamics including independent component analysis. J Neurosci Methods. 2004;134:9–21.
Faust O, Acharya RU, Allen AR, Lin CM. Analysis of EEG signals during epileptic and alcoholic states using AR modeling techniques. Irbm. 2008;29:44–52.
First MB, Williams JBW, Karg RS, Spitzer RL. Structured clinical interview for DSM-5: research version. Arlington: American Psychiatric Association; 2015.
George MS, Ketter TA, Post RM. Prefrontal cortex dysfunction in clinical depression. Depression. 2010;2:59–72.
Hillhouse TM, Porter JH. A brief history of the development of antidepressant drugs: from monoamines to glutamate. Exp Clin Psychopharmacol. 2015;23:1–21.
Hlinka J, Alexakis C, Diukova A, Liddle PF, Auer DP. Slow EEG pattern predicts reduced intrinsic functional connectivity in the default mode network: an inter-subject analysis. Neuroimage. 2010;53:239–46.
Hunter AM, Cook IA, Leuchter AF. The promise of the quantitative electroencephalogram as a predictor of antidepressant treatment outcomes in major depressive disorder. Psychiatr Clin North Am. 2007;30:105–24.
Iznak AF, Sorokin SA. Changes in EEG and reaction times during the treatment of apathetic depression. Neurosci Behav Physiol. 2013;43:79–83.
Janjarasjitt S, Scher MS, Loparo KA. Nonlinear dynamical analysis of the neonatal EEG time series: the relationship between neurodevelopment and complexity. Clin Neurophysiol. 2008;119:822–36.
Kang JH, Chung YG, Kim SP. An efficient detection of epileptic seizure by differentiation and spectral analysis of electroencephalograms. Comput Biol Med. 2015;66:352–6.
Kas MJ, Penninx B, Sommer B, Serretti A, Arango C, Marston H. A quantitative approach to neuropsychiatry: the why and the how. Neurosci Biobehav Rev. 2019;97:3–9.
Kennedy SH, Andersen HF, Thase ME. Escitalopram in the treatment of major depressive disorder: a meta-analysis. Curr Med Res Opin. 2009;25:161–75.
Knyazev GG. EEG delta oscillations as a correlate of basic homeostatic and motivational processes. Neurosci Biobehav Rev. 2012;36:677–95.
Kostyalik D, Vas S, Katai Z, Kitka T, Gyertyan I, Bagdy G, Tothfalusi L. Chronic escitalopram treatment attenuated the accelerated rapid eye movement sleep transitions after selective rapid eye movement sleep deprivation: a model-based analysis using Markov chains. BMC Neurosci. 2014;15:120.
Lader M, Andersen HF, Baekdal T. The effect of escitalopram on sleep problems in depressed patients. Hum Psychopharmacol. 2005;20:349–54.
Lanquart J, Nardone P, Hubain P, Loas G, Linkowski P. The dichotomy between low frequency and delta waves in human sleep. J Neurosci Methods. 2018;293:234–46.
Li C, Wang J. Similarity analysis of DNA sequences based on the generalized LZ complexity of (0,1)-sequences. J Math Chem. 2008;43:26–31.
Mahato S, Paul S. Electroencephalogram (EEG) signal analysis for diagnosis of major depressive disorder (MDD): a review. In: Nath V, Mandal JK, editors. Lecture notes in electrical engineering. Singapore: Springer Singapore; 2019. p. 323–35.
Maier W, Buller R, Philipp M, Heuser I. The Hamilton anxiety scale: reliability, validity and sensitivity to change in anxiety and depressive disorders. J Affect Disord. 1988;14:61–8.
Mikšovský J, Raidl A. Testing for nonlinearity in European climatic time series by the method of surrogate data. Theor Appl Climatol. 2006;83:21–33.
Montgomery SA, Baldwin DS, Blier P, Fineberg NA, Kasper S, Lader M, Lam RW, Lepine JP, Moller HJ, Nutt DJ, Rouillon F, Schatzberg AF, Thase ME. Which antidepressants have demonstrated superior efficacy? A review of the evidence. Int Clin Psychopharmacol. 2007;22:323–9.
Nofzinger EA, Price JC, Meltzer CC, Buysse DJ, Villemagne VL, Miewald JM, Sembrat RC, Steppe DA, Kupfer DJ. Towards a neurobiology of dysfunctional arousal in depression: the relationship between beta EEG power and regional cerebral glucose metabolism during NREM sleep. Psychiatry Res. 2000;98:71–91.
Pardey J, Roberts S, Tarassenko L. A review of parametric modelling techniques for EEG analysis. Med Eng Phys. 1996;18:2–11.
Sanchez C, Reines EH, Montgomery SA. A comparative review of escitalopram, paroxetine, and sertraline: are they all alike? Int Clin Psychopharmacol. 2014;29:185–96.
Santangeli O, Porkka-Heiskanen T, Virkkala J, Castaneda AE, Urrila AS. Sleep and slow-wave activity in depressed adolescent boys: a preliminary study. Sleep Med. 2017;38:24–30.
Snaith RP. Hamilton rating scale for depression. Br J Psychiatry. 1977;131:431–2.
Stein DJ, Lopez AG. Effects of escitalopram on sleep problems in patients with major depression or generalized anxiety disorder. Adv Ther. 2011;28:1021–37.
Steve MG, Bruce A, Simon H, Simon O, Ian R, Frank S, Brian W, Iain C. Efficacy and tolerability of selective serotonin reuptake inhibitors compared with tricyclic antidepressants in depression treated in primary care: systematic review and meta-analysis. Bmj. 2003;326:1014–7.
Ulke C, Huang J, Schwabedal JTC, Surova G, Mergl R, Hensch T. Coupling and dynamics of cortical and autonomic signals are linked to central inhibition during the wake-sleep transition. Sci Rep. 2017;7:11804.
Welch PD. The Fast Fourier Transform and Its Applications by E. Oran Brigham. Education IEEE Transactions on. 1988;12:27–34.
Funding
This work was supported in part by the National Natural Science Foundation of China (no. 81671038). This funding was role in the analysis of data and in writing the manuscript. This work was also supported by the National Natural Science Foundation of China (no.61871165, 81171251 and 81871071), Capital’s Funds for Health Improvement and Research (no. 2014–4-4113), Beijing Municipal Science and Technology Commission (no. Z161100000516128), and Beijing Municipal Natural Science Foundation (no. 7162101). These funding were role in the design of the study and in the collection of data.
Author information
Authors and Affiliations
Contributions
X.Q.W, S.X.L designed this study, collected this data. L. W,Y.Y analyzed data and mainly wrote this manscript. X.Q.W, T.F.D, L. L, Q.Q.C, S.X.L helped in writing the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All of the participants signed written informed consent forms before participation. The study was approved by the ethics committee of Peking University Sixth Hospital, Beijing, China, in accordance with the Helsinki Declaration.
Consent for publication
Not applicable.
Competing interests
All authors declare that there are no conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wu, L., Wang, XQ., Yang, Y. et al. Spatio-temporal dynamics of EEG features during sleep in major depressive disorder after treatment with escitalopram: a pilot study. BMC Psychiatry 20, 124 (2020). https://doi.org/10.1186/s12888-020-02519-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-020-02519-x