Abstract
Background
Stigma towards people with mental health problems (PMHP) is known to have substantial negative impacts on their lives. More in-depth exploration of the stigma and discrimination experienced by PMHP in low- and middle-income countries is needed. Previous research suggests that negative attitudes towards PMHP are widespread among the Filipino general public. However, no study has investigated PMHP’s own experiences of being stigmatised in the Philippines.
Methods
A qualitative study was conducted on the stigma experienced by PMHP (including people with epilepsy) and its related factors in the Philippines, employing the constructivist grounded theory approach. We analysed data on 39 PMHP collected through interviews with PMHP, their carers, and community health volunteers who know them well.
Results
The findings highlight the culturally and socio-economically specific contexts, consequences, and impact modifiers of experiences of stigma. Participants emphasised that PMHP face stigma because of the cultural traits such as the perception of mental health problem as a disease of the family and the tendency to be overly optimistic about the severity of the mental health problem and its impact on their life. Further, stigma was experienced under conditions where mental health care was not readily available and people in the local community could not resolve the PMHP’s mental health crisis. Stigma experiences reduced social networks and opportunities for PMHP, threatened the economic survival of their entire family, and exacerbated their mental health problems. An individual’s reaction to negative experiences can be fatalistic in nature (e.g. believing in it is God’s will). This fatalism can help PMHP to remain hopeful. In addition, traditional communal unity alleviated some of the social exclusion associated with stigma.
Conclusions
The study indicates that existing stigma-reduction strategies might have limitations in their effectiveness across cultural settings. Therefore, we propose context-specific practical implications (e.g. emphasis on environmental factors as a cause of mental health problems, messages to increase understanding not only of the possibility of recovery but also of challenges PMHP face) for the Philippines.
Similar content being viewed by others
Background
Stigma and discrimination against people with mental health problems (PMHP) are a global public health issue [1,2,3] and can have substantial negative impacts on all aspects of a person’s life, from employment and housing to social and family life [4,5,6,7]. Public stigma, the general public’s reaction towards a stigmatised group, can be conceptualised as having three distinct elements [8]. First, a negative belief about a stigmatised group is seen as stereotype. Second, an emotional reaction to the stereotype is seen as prejudice. Third, a behavioural manifestation of the prejudice is discrimination. Historically, research on stigma related to mental health has been conducted mainly on stereotypes, prejudices, and intentions to discriminate that are held by the general public with regard to PMHP. Such research revealed that the general public frequently label PMHP as dangerous, blameworthy, incompetent and weak, which is often accompanied with emotions of fear and anger and can lead to behavioural intention of avoidance, punishment, and coercion [9,10,11,12]. Further, the literature shows that internalisation of public stigma or self-stigma is also frequent among PMHP, which reduces self-esteem, causes social isolation, and inhibits help-seeking behaviour [6, 13,14,15].
Recent research has more often investigated levels of discrimination using direct reports from PMHP. The results of such research suggest that discrimination against PMHP is a universal phenomenon around the world [2, 3, 16]; however, PMHP’s experiences of discrimination and its related factors might differ in high-income countries (HICs) versus low- and middle- income countries (LMICs). Some studies suggest that PMHP experience a lower level of stigma in LMICs [17], such as India [18], China [19], and Nigeria [20], compared with HICs. The reasons for the more positive acceptance of PMHP in those settings have been considered to be a more supportive environment with social cohesion as well as more social role options that PMHP are able to fulfil [21, 22]. At the same time, there is also accumulating evidence revealing that in LMICs, experiences of stigma, discrimination and human rights abuses related to mental health problems are common and severe [23,24,25,26,27]. The stigmatisation in LMICs has been attributed to the combined effects of socioeconomic and ethno-cultural characteristics of the setting [28]. For example, the economic situation of widespread poverty may contribute to further marginalisation of PMHP who are not able to financially contribute to society [29]. Moreover, the cultural value of collectivism may results in discrimination towards PMHP especially with regarding to marriage and childrearing, since a person’s mental health problem is often seen as the family’s mental health problem [30]. Overall, practices and outcomes of stigma differ across cultures and socioeconomic backgrounds [29, 31, 32], and meaningful comparison across cultural settings may not be achievable with cross-cultural measures [33]. In consideration of this, researchers have called for an in-depth qualitative exploration of the experiences of stigma among PMHP in LMICs settings, where about 85% of the world’s population live [21].
PMHP in the Philippines, a lower-middle income country in Asia, might experience a significant level of stigma and discrimination. Filipino immigrants believed that personal characteristics (i.e. self-centeredness and “soul weakness”) resulted in mental health problems [34, 35], which have been shown to be related to blaming PMHP and discriminatory behaviour in other settings [36]. Also, a multi-country survey revealed that, among 16 countries surveyed, the Philippines had the second highest proportion of citizens who agreed that PMHP should not be hired for a job even if they are qualified [37]. Further, some studies that involved interviews with Filipino immigrants living in Australia and the United States and that sampled from the general population revealed that a fear of being labelled as ‘crazy’ and spoiling their family’s reputation made Filipinos hesitate to seek help from mental health professionals [35, 38, 39]. Although these previous studies provide some knowledge regarding public stigma in the Filipino context, all of them looked at stereotypes, prejudices and intentions to discriminate held by the general public towards PMHP. To our knowledge, there is no study investigating PMHP’s own experiences of being stigmatised and discriminated against and the related factors in the Philippines.
To fill the gaps in the literature, we conducted a qualitative study on the factors related to experiences of stigma as well as the experiences itself of PMHP in the Philippines, using interviews with PMHP and people who know them well. Revealing the existence, types, and sources of stigma experienced by PMHP in the Philippines can contribute to the stigma research in Asian LMIC settings. Further, exploring the experiences of stigma and its related factors can provide fundamental knowledge for the design of an effective stigma reduction program in the Filipino setting.
Methods
The current research utilised the principles of constructivist grounded theory, which is deemed suitable for revealing the social phenomenon of PMHP’s experiences of stigma [40] in the Filipino context. The constructivist grounded theory assumes a relativist ontology (accepting that multiple realities exist) and a subjectivist epistemology (involving a co-construction of meaning through interaction between the researcher and participant) [41]. It provides a means of studying power, inequality, and marginality [42].
Setting
Our study was conducted in Muntinlupa, the southernmost city in the Philippines’ National Capital Region. The city has a population of 481,461 as of 2016. The majority comprises Tagalog ethnic groups and professes Christian, primarily Roman Catholic, faith. Households below the food threshold, the minimum income required to meet basic food needs, account for 21.5% of the total in the city [43]. The majority of citizens cannot afford private medical services, which cost five times more than the public medical services [44]. With respect to public psychiatric service, the city has one outpatient and no in-patient facility. The nearest public in-patient psychiatric facility is located about 23 km away.
Main data collection
Participants
We collected data on PMHP from three different sources of information: PMHP themselves, their carers, and community health volunteers who knew them well. The eligibility criteria for PMHP were 1) having a mental health problem, listed in the Diagnostic and Statistical Manual of Mental Disorders 5 (DSM-5), or epilepsy, and 2) currently not using residential care. Epilepsy was included for several reasons. First, people with epilepsy are known to suffer stigma and discrimination [45, 46]. Second, the condition has a long history of being classified as a psychiatric problem [47]. Third, even with the present-day efforts promoting mental health in LMICs, epilepsy is often treated together with mental health issues [48]. Last, pilot interviews revealed that local lay people do not clearly differentiate epilepsy from mental health problems.
For the recruitment, we approached 42 PMHP in person; one of them declined to participate owing to time constraints. Thus, we obtained informed consent from 41 PMHP. Among them, two PMHP were excluded because they were confirmed to have only physical health problems and no mental health problems as listed in DSM-5. Consequently, we used data of 39 PMHP for our analysis. The profiles of the final sample are shown in Table 1. In 20 of the PMHP, we interviewed the PMHP and their main carer, usually a parent or sibling. In the remaining 19 PMHP, only a main carer was interviewed, as the 19 PMHP had communication difficulties that hindered them from answering interview questions. Additionally, in 11 PMHP, we conducted interviews with a community health volunteer who was in charge of the district in which the PMHP lived.
Recruitment
We aimed to include a wide variation in the characteristics of the PMHP, namely, gender, age, marital status, educational attainment, employment status, religion, type of mental health problem, and history of using health and welfare services. To achieve this, the participants were recruited by purposive sampling in cooperation with two different collaborating stakeholders. First, as stigma was considered to inhibit Filipino people from seeking professional help for their mental condition [35, 49], we recruited the majority of PMHP (n = 36) in cooperation with community health volunteers, which enabled us to recruit PMHP regardless of their history of receiving health care. The community health volunteers had good knowledge of the profiles of the residents of the district under their charge and covered all the areas of the city. Second, we recruited a small number of PMHP (n = 3) with common mental health problems (e.g. anxiety and depressive problems) from the outpatient clinical practice of a psychiatrist, as the community health volunteers did not identify any people with these types of problems.
To check the eligibility of those who had never been diagnosed by a specialist as having a mental health problem, a research member, ET, carefully reviewed the data of the individual participants, including interview recordings, transcriptions, and field notes, and then provided informed presumption if the participants had a mental health problem or not. ET also assessed which chapter, the broadest classification in DSM-5, the participant most fitted. ET has clinical experience as a psychiatrist in Japan for over 15 years.
Interview procedures
Data on the PMHP were collected through semi-structured in-depth interviews. Prior to the beginning of data collection, an interview guide was developed, referring to previous research [18, 50], and then modified based on six pilot interviews in the setting. The interview guide had a series of open questions on three major topics: onset of mental health problems and coping behaviours, experiences of being treated negatively owing to the problem and its consequences, and activities PMHP gave up because of how others might respond to their health problem. The interview guides for interviews with PMHP and for interviews with carers and community health volunteers can be accessed in Additional files 1 and 2, respectively. Consistent with the grounded theory methods, we used the interview guide as a flexible tool that could be revised as the analysis progressed. The carers and community health volunteers were not asked about their own experiences of stigma as a carer or person working in mental health. Instead, we asked them about the PMHP’s experiences regarding the same topics, based on their observations. Demographic data of the PMHP were also obtained at the beginning of the interview.
The first author, CT (female, a Japanese public health nurse), conducted all of the data collection between January and March 2017. During the interview, Tagalog or English was used as preferred by the participants. When Tagalog was chosen, the interviews were interpreted by one of two health workers who had lived in the city for more than 30 years and were fluent in both Tagalog and English. After explaining the study and gaining informed consent, the interviews were conducted in their home, a health centre, or the city hospital, depending on the participants’ preference. Wherever possible, we conducted interviews in a space where there was no one but the interviewee, interviewer, and interpreter around. However, five PMHP were not willing to be interviewed alone. In which case, a family member was in the same place and assisted the interview. All the interviews were digitally recorded with interviewees’ permission and lasted between 19 and 53 min; the median length was 29 min. The participants received 100 Philippine pesos (1.9 US dollars) as acknowledgement for their participation.
Supplementary data collection
We included data of interviews with seven health workers into our analysis to gain a wider perspective on the stigma experienced by PMHP. CT conducted the interviews during her one-month participant observation at health services provided by the city government. During the observation, CT discussed the role of stigma and its impact on PMHP with more than 85 health and welfare workers. We analysed seven interviews with those who shared episodes on PMHP with whom they were in direct contact as a part of their duty at work. The interviewees were three community health volunteers, two nurses, one doctor, and one rehabilitation program officer. Notes were taken during the interviews and six out of seven interviews were audiotaped with their permission.
Analyses
All of the recordings were transcribed verbatim by two trained transcribers. Tagalog recordings were simultaneously translated into English by the transcribers fluent in English and Tagalog. An independent research assistant randomly selected 10% of the English transcripts and checked their accuracy by matching them with the Tagalog and English recordings. During this checking process, no significant errors were found thus the transcripts were quality assured.
Data analysis started as soon as the initial data were collected. We set aside theoretical ideas from the existing literature; instead, we remained open to exploring the theoretical possibilities we could discern from the data. After reading each of the transcripts at least twice, CT and ET independently conducted the initial coding. Simple codes were created to describe the phenomenon in each segment of data, using the qualitative data analysis software, Nvivo Version 11.4.1 (QSR International, 2016). The initial codes with identical meanings were merged through discussion, whereas those with different meanings were left unchanged to increase the variety in the interpretation of the data. We used data from interviews with cares, health volunteers, health and welfare workers to increase variety of data on stigma experienced by PMHP and gain comprehensive understanding of its context. Thus, when accounts showed some discrepancy between a person with mental health problem and his/her carer or a person who knew him/her well, we used the data from both accounts for our analysis.
The authors gradually moved on to the focus coding, in which the initial codes were concentrated on or collapsed into categories that make analytical sense, and then tested these against extensive data. The interpersonal interaction between people with and without mental health problems was treated as the central phenomenon of our interest. To explore comprehensively PMHP’s experiences of stigma, we decided to treat any “uncomfortable treatments from others” reported as stigma experience, regardless of the actors’ motivation. We constantly compared data on similarities and differences within a participant as well as across participants to examine the categories and develop links among them. CT led the preliminary focus coding. Subsequently, discussions were held between CT, ET, and HM, in which we reviewed the developed categories and links to determine if they were grounded in data and sufficiently explained the phenomenon.
After analysing the data of the 35 PMHP, a tentative model that explains the relations between categories was developed. We then collected and analysed data on four additional PMHP. Through discussion, the full research team determined that the categories and themes were sufficiently relevant and that the model held true for these additional PMHP. We then concluded that the model was theoretically saturated.
Results
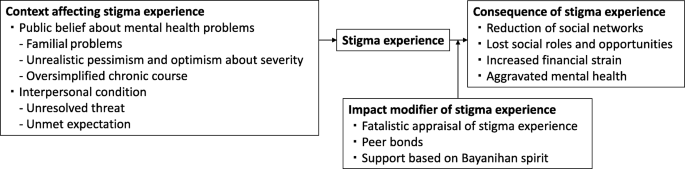
Analyses revealed four interrelated themes surrounding stigma experienced by PMHP: (1) the context affecting stigma experience, (2) stigma experience, (3) impact modifier of the stigma experience, and (4) consequence of the stigma experience. Figure 1 shows the relationship among the themes.
Context affecting stigma experience
We identified two contextual categories that changed how others treated PMHP in a negative way.
Public belief about mental health problems
Public beliefs surrounding mental health issues are a contextual category of stigma experienced by PMHP in the Philippines. It consists of three themes: familial problems, unrealistic pessimism and optimism about severity, and oversimplified chronic course.
Familial problems
Community health volunteers and health workers observed that families of PMHP and people in the local community do not provide appropriate support for PMHP because they perceive mental affliction as a family problem and indicative of so-called “bad blood”. The belief that mental health problems can be transmitted among relatives pushed families of PMHP to deny the existence of mental health issues and people in the community to distance themselves from PMHP. A nurse shared an episode of a male patient with depression:
His family could not accept the idea that one of their relatives is actually depressed. (…) It’s because in our culture, when it comes to mental illness, it tends to be a family affair. People think if one of you has a history of mental illness, there is a chance that almost all of you already have that as well. We care about how others think about our family more than anything else. And other people feel that it is not their place to intervene in some family matters. (Interview 48, Nurse, Female)
In particular, marrying age PMHP faced stigma because of the belief in heredity. People in the community often believe that PMHP have mental health problems in their family’s blood and are afraid of developing those problems in their kinship via marriage.
I had one neighbour that I reported to the barangay [district government] because she mocked me. She was saying that I had mental illness in our blood and no one dare marry me and get in trouble. (Interview 51, PMHP, Male)
Unrealistic pessimism and optimism about severity
PMHP experienced stigma when others were overly pessimistic about the severity of a mental health problem. Participants often criticised those who believe that mental health problems generally cause severe functional impairments. This belief has resulted in unfair treatment towards PMHP in the Philippines.
[Researcher: What is the biggest challenge for the [social inclusion] program?] Finding a job. It’s very difficult. The community people don’t believe they [PMHP] are functional and don’t hire them. (…) So now some barangays [district governments] have started to hire them. We hope people see them working hard and start to trust them. (Interview 27, Rehabilitation program officer, Male)
Meanwhile, unrealistic optimism about its severity also caused stigma. The commonly held belief is that individuals are able to overcome any psychological suffering by themselves, and as a result, it will not become a serious problem. It was common for PMHP to be doubted or withheld empathy in such a culture that emphasises resilience and humour under stressful situations.
Filipinos are proud of being resilient. We find something funny in any difficult situation. But when you have this illness, that kind of thinking gives you a huge pressure. (…) One day, I opened up about my mental illness to my friends, but they all had the same reaction. They laughed at me and didn’t take it seriously. (Interview 71, PMHP, Female)
Oversimplified chronic course
The oversimplified chronic course of mental health problems emerged as one of the causes of stigma. People without any experience of a mental health problem often misunderstand the repetitive relapse and remission in the course of a mental health problem. They tend to apply an acute illness model and expect a complete cure in the short term. However, as the symptoms are prolonged, they begin to mistrust the PMHP’s account.
After one month of no work, I was able to work and sleep. But in February, it came back. I couldn’t sleep for several days. (...) My supervisors were thinking that I should be working a night shift duty, but I told them that I would have to take sick leave. But because it was the same reason for my previous absent, they are already thinking that I am making up stories. (Interview 30, PMHP, Male)
Interpersonal condition
Interpersonal condition was identified as a direct trigger of stigma experience. It consists of two themes: unresolved threat and unmet expectation.
Unresolved threat
Unresolved threat is a condition where PMHP are at risk of hurting themselves or others owing to their mental health problems, with the people in contact with the PMHP failing to manage such risks. Under such conditions, PMHP often experience physical violence, being avoided, and being restricted by others. Although the PMHP, their families, and community health volunteers attributed the threats to PMHP’s personal factors, such as personality and outwardly noticeable symptoms, they also emphasised the culpability of people in the local community for their lack of understanding and skills in interacting with PMHP. When others became familiar with PMHP, they successfully managed those threats and prevented PMHP from experiencing stigma. The mother of a boy with a neurodevelopmental problem told us:
My son easily becomes violent. For example, when someone takes and plays with his toy. The neighbours don’t understand why he is angry and they bully him. But there are also some playmates who fully understand him. When they know that my son is about to be angry, they immediately keep distance from him. And after a while, my son calms down and they start playing around together. (Interview 4, Mother of a boy with a mental health problem)
Unmet expectation
Unmet expectation was another context of stigma. In this context, there is a gap between PMHP’s abilities and other people’s expectations of them. Some PMHP reported suffering from stigma when others’ expectations were too high for their situation. People in this cultural setting tend to value strong bonds and reciprocity among families and neighbours. PMHP sometimes were unable to perform in accordance with this value owing to their mental health conditions. Violation of this value was judged as morally wrong.
They [the neighbours] say I should help my mum by doing washing, cleaning, and taking care of my brother, even when I say I feel weak or don’t know how to. (Interview 5, PMHP, Female)
She is big but still doesn’t help her mother. That’s why the neighbours don’t like her. They say she is not a good daughter. (Interview 18, Community health volunteer, Female)
Meanwhile, some other PMHP experienced stigma when others underestimated PMHP’s abilities. Families often criticised other people that looked only at PMHP’s disabilities but not at their abilities.
When someone in our neighbourhood was trying to talk to my sister and she did not respond back, they started bullying her and calling her crazy. [Researcher: How do you think we can change such situation?] I think proper communication towards her would be the best since she’s really a good listener. The problem is that other people don’t know she actually understands things really well. (Interview 8, Sister of a woman with a mental health problem)
Stigma experience
Although we frequently found that PMHP were positively treated by others because of their mental health problems, we also discovered that almost all the PMHP participants were faced with negative treatment from others. PMHP experienced psychological abuse (e.g. being verbally insulted, laughed at, stared at, gossiped about, doubted), physical violence (e.g. being hit, stones being thrown at them), being restricted (e.g. being told not to go outside alone, tied with a rope to a pillar), not being supported (e.g. lack of understanding and sympathy), being taken advantage of (e.g. being cheated out of money and belongings), being neglected (e.g. privacy not being protected, medical care not being provided), and being rejected (e.g. not being associated with, not being hired). Families were an important source of stigma in terms of prominence as stigma from families was often repetitive (e.g. frequently being slapped) and prolonged (e.g. being locked up in a room for several months). PMHP also experienced stigma frequently from their neighbours, and sometimes from school friends, co-workers and employers. People who were involved with PMHP as a part of their duty at work (i.e. health workers and public safety officers) were a source of stigma as well. For complete information on the stigma experience by source, please see Table 2.
Impact modifier of stigma experience
Even if the nature of stigma experiences were similar, the extent and degree of its influence on PMHP’s life varied depending on impact modifier of stigma experience. PMHP had three impact modifiers consisting of internal (i.e. fatalistic appraisal) and external (i.e. peer bonds, community unity) factors.
Fatalistic appraisal of stigma experience
Fatalistic appraisal of stigma experience offered PMHP and their families a strategy to cope with the emotional pain caused by stigma experience. People in the setting generally believed that God predetermined life events in the past, present and future. Some PMHP and their family accepted unfair treatments from others as “fate.” They were able to remain hopeful because they believed that God would help them if they had faith in God.
Sometimes people say he is crazy. [Researcher: What do you do in response to that?] Nothing. People say what they want to say. We just say “God is good.” As long as we believe in Him, it will be alright. (Interview 23, Sister of a man with a mental health problem)
Peer bonds
Peer bonds, the emotional bonds with other people with similar mental health problems, empowered PMHP to change their stigmatised situation in a positive way. Stigma experience could marginalise them in the community, but when they were together with peers who understood not only their health condition but also their lowered social status, they were empowered and motivated to change the situation for themselves and their peers.
[Researcher: What are the barriers to your recovery?] The different perceptions of people towards us [she and other people with mental health problems]. It is so discouraging for us. And we are the only ones who can understand each other very well. We are like brothers and sisters already. Nevertheless, we make sure that the reason we join the [rehabilitation] program is not only for ourselves but to show them that we can change ourselves for the better. If we will be given a chance to work again, we will make 100 percent effort to get things done accordingly. (Interview 34, PMHP, Female)
Support based on Bayanihan spirit
Support based on Bayanihan spirit, a traditional concept of community unity, relieved the negative impacts of stigma on PMHP. It was not rare that community people gave food or rented a house free to PMHP and their family who had little income. Helping one another in a time of need was inherent in their lives, called Bayanihan in Tagalog. For example, a homeless woman with schizophrenia told us that she had felt hopeless because she had been bullied at school and was in a materially deprived circumstance. However, she was now enjoying her life and managing to make a living because some of her neighbours treated her as a valued community member (e.g. regularly invited her to a local dancing event) and occasionally gave her food. A community health volunteer explained why she had good relationships with the community as follows:
That is natural here. When your family member is sick, neighbours and friends are there to pay for medicines, bring food, help with housework, and take care of small kids. We call it Bayanihan. (Interview 3, Community health volunteer, Female)
Consequence of stigma experience
Stigma experience was found to bring about a substantial negative impact on PMHP’s social networks, roles, opportunities, and mental health.
Reduction of social networks
Stigma experience reduced PMHP’s social networks, which led to them spending their days isolated at home without any interaction with people outside of their immediate family. This was due not only to the direct influence of experiences of stigma (i.e. being physically restrained, being avoided by others) but also the indirect influence of changes in three aspects: PMHP’s behaviour, restriction by families, and relationships with others. First, after being negatively treated, PMHP tended to “close off to everybody” and distanced themselves from others.
Going out is sometimes like an obstacle. (…) After that [hearing my friends gossiping about me], I have been afraid of people’s judgments. (Interview 62, PMHP, Female)
Second, families started to restrict PMHP’s behaviour to protect them from further stigma experiences.
We do not allow him to go out. We are afraid that something like that [neighbours calling him crazy] might happen to him again or someone might abduct him. (Interview 9, Sister of a man with a mental health problem)
Third, stigma experiences provoked conflicts, from a quarrel to a physical fight, and worsened the relationship between PMHP and others. The conflicting relationships produced a further stigmatising attitude towards PMHP.
He got into a fight with his playmates because they said bad words to him. (…) Many of our neighbours told me that he should be in a cell. They told me that they knew a policeman who could put him in jail. (Interview 1, Mother of a man with metal health problem)
Lost social roles and opportunities
As a result of stigma experience, PMHP lost social roles and opportunities, such as being employed, going to school, having a romantic partner, getting married, parenting, helping with household chores and the family business, taking care of younger siblings and joining religious activities.
She was a member of the choir in church. She likes singing and has a good voice. And plenty of friends visited her in the past and they went to church together. But no more. Nobody visits her, and she quit attending it. (Interview 10, Mother of a woman with a mental health problem)
Increased financial strain
Lost social roles and opportunities increased financial strain, which negatively affected the families as well as PMHP themselves. In this setting, PMHP and their families lived in communities where many people find it difficult to make a living. The cost of transportation to medical facilities and treatment fees put them in a further difficult situation economically. In such conditions, entire families often suffered from the financial strain that was due to stigma to the degree that they could not afford basic items including food and clothing.
If only I could find a good job like when I was well. Even though we do not have enough money to buy things, my family really makes an effort to find ways that we can buy those medicines. (Interview 20, PMHP, Male)
Aggravated mental health
The participants reported that the stigma experiences aggravated mental health in PMHP. The memory of negative treatment from others often stuck in their mind and its influence lasted for a long time. A 32-year-old woman with anxiety problem explained how the experience of being bullied when she was a teenager influenced her current condition:
It triggers my anxiety. When I remember their facial expressions, even now, I feel overwhelmed and breathless (Interview 39, PMHP, Female).
The experience of stigma also affected the mental health condition of PMHP by preventing them from seeking help. Some PMHP and their families choose to keep their mental health status a secret. However, families have limited capacities to take care of a person with a mental health problem, especially in the case of someone with severe symptoms. In the worst case in terms of the influence of stigma on PMHP’s mental health, a community health volunteer reported that the parents of a daughter with a mental health problem locked her up in her room and took care of her without seeking professional help. However, her condition kept deteriorating and eventually she committed suicide inside her room.
Discussion
To our knowledge, this is the first study to document the stigma experienced by PMHP in the Philippines. This study adds to the understanding of discrimination in LMIC settings and its related contextual factors in the Philippines.
First, our results showed that PMHP in the Philippines experienced stigma, which brought about negative impacts on PMHP’s social networks, roles and opportunities, financial burden, and mental health. Although stigma types, sources, and areas of impact were generally consistent with the existing literature in this field [4, 6, 51], we found that experiences of stigma threatened the economic survival of the entire family of PMHP and increased the mental health crisis in the LMIC context, given the minimal welfare and mental health care provisions. Several studies with participants recruited from clinical settings have shown that PMHP in LMICs suffered less from stigma [2, 18,19,20]. In this study, we involved PMHP without psychiatric service use, which prevented us from overlooking the stigma experienced by the poorest and most marginalised PMHP. Our findings might better reflect the reality in LMIC settings, where it is estimated that more than 70% of PMHP receive no treatment for their mental health conditions [52].
Second, we found that pessimistic and over-optimistic reactions to a mental health problem are among the important contexts of experiences of stigma in the Philippines. Historically, stigma research has mainly focused on the pessimistic view on the prognosis and its negative effects [10, 53,54,55,56]. Meanwhile, when the over-optimistic view on the outcome of mental health problems has been documented among Filipino immigrants, it was only recognised as a barrier to help-seeking [35, 39]. Our qualitative exploration’s original finding is that the over-optimistic belief among the community regarding the severity of mental health problems results in PMHP’s receiving inappropriate or negative treatment. This is an important finding for the Philippines, because resilience and optimism under difficult situations are among the well-known cultural traits of Filipinos [57, 58]. Stigma resulting from optimism might be prevalent in the Philippines; a prior study showed that among the 16 countries, the Philippines posted the highest proportion of respondents who agreed that mental illness would improve on its own [59].
Third, the results indicated that mental health problems were perceived as problems of the family and discouraged people from accepting mental health problems. The finding is consistent with psychiatrists’ clinical experiences with Filipino patients [60, 61]. We also found that a belief in transmissibility among relatives led to PMHP experiencing reduced marriage opportunities. Previous studies conducted on Chinese descent groups [62,63,64] showed that the threat of genetic contamination was related to endorsement of reproductive restriction. We propose that it might hold true in the Filipino context, meaning that the threat to family lineage through genetic contamination via marriage accounts for some of the discrimination experienced by PMHP.
Fourth, we revealed a context-specific impact modifier of stigma experiences, namely, fatalistic appraisal of stigma experience. Existing studies have discussed that Filipinos typically attribute illness to “the will of God” [39, 49, 65]. A new finding of this study is that negative treatments from others were also attributed to fate. Globally, it is known that fatalistic appraisal of negative events inhibits active coping and worsens health [66, 67]. However, we found that fatalism offered a spiritual coping strategy and shielded PMHP from the adverse effects of stigma in the Catholic dominant setting of the Philippines. These findings are consistent with the literature that have showed that fatalism facilitates adjustment to negative life events [49, 68, 69]. Moreover, support based on Bayanihan spirit was another culturally relevant impact modifier. The origin of the Bayanihan spirit is traced back to the country’s tradition wherein towns’ people cooperate to carry a family’s entire house on their shoulders to a new location. It is considered a core essence of the Filipino culture. Our finding supports the arguments by Lasalvia [21] and Mascayano et al. [29] that communal network, which tends to be better maintained in LMICs, is among the existing strengths to reduce the negative effects of stigma.
Lastly, the research method of obtaining perspectives from multiple participants who witnessed and experienced stigma allowed us to reveal that the interpersonal conditions (i.e. unresolved threat and unmet expectations) preceded stigma experiences. Consistent with previous research from India [24] and Indonesia [70], in the setting where mental health care is not readily available at a local level, people in the community needed to cope with the possible danger of PMHP to self or others and can violate PMHP’s human rights. Similar to the results of prior qualitative analyses of interviews with PMHP and their families [18, 71], the expectations of others in contrast to PMHP’s actual capabilities caused negative reactions from others. Those interpersonal conditions might be a more important determinant of stigma experiences than PMHP’s personal factors, considering the previous studies showing individual variables (e.g. employment status, symptom, and treatment experiences) accounted for only less than 30% of total variance of experienced stigma [2, 3].
Practical implications
Our results suggest that mental health care must have the objective of the reduction of stigma towards PMHP. The Department of Health and Local Government Units are required by the Mental Health Act [72], established in 2018 as the first law of its kind in the Philippines, to initiate and sustain nationwide campaigns to raise the level of awareness on the protection and promotion of mental health and rights. In conducting stigma reduction campaigns, they should: 1) target families of PMHP, community people, health workers, and public safety officers; 2) avoid genetic explanations for mental health problems and emphasise the role of environmental and social factors as its cause; 3) increase public understanding of not only the possibility of recovery but also the challenges that PMHP face; and 4) improve families’ and community members’ skills in assessing and coping with possible danger posed by PMHP to self or others [73,74,75,76]. These interventions might be more effective when they utilise the existing communal network and increase social contact between PMHP and others [77, 78] We also propose that mental health and welfare services for PMHP should: 1) be community-based and support PMHP in meeting expectations that are meaningful for themselves and others; 2) provide opportunities for PMHP to share their experiences with peers to empower them [79,80,81]; and 3) prevent PMHP from internalising experiences of stigma with acknowledgement of fatalistic appraisal of them as a coping strategy. Lastly, to mitigate the adverse influences of stigma, it is necessary to change the structure of health care and welfare service provision for PMHP (e.g. inclusive education, welfare benefits, and job schemes). It is also essential to provide effective and accessible mental health care.
Study limitations
We were unable to recruit people with common mental health problems who were not using psychiatric services. In fact, community health volunteers do not recognise any people having common mental health problems. This may reflect stigma-related situations where local people do not recognise the manifestation of symptoms of those problems as a health issue, or where people with those problems hide their conditions. Additionally, cultural and language barriers may have played a part in data collection and interpretation. However, we also encountered a number of situations where the interviewee provided the data collector, who was from another cultural background, with further explanations, especially on their culture. Further, some interviews were too short to be considered an in-depth interview. Also, we needed to rely in part on data from narratives of people who know PMHP well, instead of from PMHP themselves. These were because the interviewer had difficulty encouraging some participants, especially PMHP, to talk about sensitive topics. Thus, there might be experiences and related themes that we could not explore. Lastly, we conducted the study in one city; thus, the results may not be generalisable to another part of the Philippines (e.g. rural and Muslim-dominant areas).
Conclusions
Our findings highlight that PMHP in the Philippines experience substantial discrimination and its adverse effects are severe to the degree that it threatens the financial survival of the entire family. Culture-bound beliefs and social structure (e.g. perceiving mental health problems as a familial problems, traditional communal unity) played important roles in shaping and modifying stigma experiences. More research is needed to develop stigma reduction interventions utilising these findings and to evaluate their effectiveness.
Abbreviations
- DSM:
-
The Diagnostic and Statistical Manual of Mental Disorders
- HICs:
-
High-income countries
- LMICs:
-
Low- and middle-income countries
- PMHP:
-
People with mental health problems
References
Seeman N, Tang S, Brown AD, Ing A. World survey of mental illness stigma. J Affect Disord. 2016;190:115–121. Available from: https://doi.org/10.1016/j.jad.2015.10.011 Elsevier.
Lasalvia A, Zoppei S, Van Bortel T, Bonetto C, Cristofalo D, Wahlbeck K, et al. Global pattern of experienced and anticipated discrimination reported by people with major depressive disorder: a cross-sectional survey. Lancet. 2013;381:55–62. Available from: https://doi.org/10.1016/S0140-6736(12)61379-8 Elsevier Ltd
Thornicroft G, Brohan E, Rose D, Sartorius N, Leese M. Global pattern of experienced and anticipated discrimination against people with schizophrenia: a cross-sectional survey. Lancet; 2009;373:408–415. Available from: https://doi.org/10.1016/S0140-6736(08)61817-6. Elsevier Ltd
Sharac J, McCrone P, Clement S, Thornicroft G. The economic impact of mental health stigma and discrimination: a systematic review. Epidemiol Psichiatr Soc. 2010;19:223. Available from: https://www.ncbi.nlm.nih.gov/pubmed/21261218.
Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, et al. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med. 2015;45:11–27 Available from: http://www.ncbi.nlm.nih.gov/pubmed/24569086.
Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: a systematic review and meta-analysis. Soc Sci Med. 2010;71:2150–2161. Available from: https://doi.org/10.1016/j.socscimed.2010.09.030 Elsevier Ltd
Link BG, Phelan JC. Conceptualising stigma. Annu Rev Sociol. 2001 [cited 2018 Jul 3];27:363–385. Available from: https://www.annualreviews.org/doi/pdf/10.1146/annurev.soc.27.1.363
Corrigan PW. Mental health stigma as social attribution: implications for research methods and attitude change. Clin Psychol Sci Pract. 2006;7:48–67 Available from: http://doi.wiley.com/10.1093/clipsy.7.1.48.
Mannarini S, Boffo M. Anxiety, bulimia, drug and alcohol addiction, depression, and schizophrenia: what do you think about their aetiology, dangerousness, social distance, and treatment? A latent class analysis approach. Soc Psychiatry Psychiatr Epidemiol. 2015;50:27–37.
McGinty EE, Goldman HH, Pescosolido B, Barry CL. Portraying mental illness and drug addiction as treatable health conditions: effects of a randomized experiment on stigma and discrimination. Soc Sci Med; 2015;126:73–85. Available from: https://doi.org/10.1016/j.socscimed.2014.12.010. Elsevier Ltd
Angermeyer MC, Dietrich S. Public beliefs about and attitudes towards people with mental illness: a review of population studies. Acta Psychiatr Scand. 2006;113:163–79.
Corrigan PW, Markowitz FE, Watson A, Rowan D, Kubiak MA. An attribution model of public discrimination towards persons with mental illness. J Health Soc Behav. 2003;44:162–79.
Corrigan P, Watson A. The paradox of self-stigma and mental illness. Clin Psychol Sci Pract. 2002;9:35–53 Available from: https://onlinelibrary.wiley.com/doi/10.1093/clipsy.9.1.35.
Evans-Lacko S, Brohan E, Mojtabai R, Thornicroft G. Association between public views of mental illness and self-stigma among individuals with mental illness in 14 European countries. Psychol Med. 2012;42:1741–52.
Mccann TV, Renzaho A, Mugavin J, Lubman DI. Stigma of mental illness and substance misuse in sub-Saharan African migrants: a qualitative study. Int J Ment Health Nurs. 2017;27:956–65.
Camden Schizoph E, Corker EA, Beldie A, Brain C, Jakovljevic M, Jarema M, et al. Experience of stigma and discrimination reported by people experiencing the first episode of schizophrenia and those with a first episode of depression: The FEDORA project Anamaria Vasilache 2 , Margda Waern 3,4 , Norman Sartorius 10 , Graham Thornicroft 1 and the FEDORA study group. Int J Soc Psychiatry. 2015 [cited 2018 Jul 3];61:438–445. Available from: http://journals.sagepub.com/doi/pdf/10.1177/0020764014551941
Lasalvia A, Van Bortel T, Bonetto C, Jayaram G, Van Weeghel J, Zoppei S, et al. Cross-national variations in reported discrimination among people treated for major depression worldwide : the ASPEN / INDIGO international study. Br J Psychiatry. 2015;207:507–14.
Koschorke M, Padmavati R, Kumar S, Cohen A, Weiss HA, Chatterjee S, et al. Experiences of stigma and discrimination of people with schizophrenia in India. Soc Sci Med; 2014;123:149–159. Available from: https://doi.org/10.1016/j.socscimed.2014.10.035. Elsevier Ltd
Lv Y, Wolf A, Wang X. Experienced stigma and self-stigma in Chinese patients with schizophrenia. Gen Hosp Psychiatry. 2013;35:83–8. Available from: https://doi.org/10.1016/j.genhosppsych.2012.07.007 Elsevier Inc.
Oshodi YO, Abdulmalik J, Ola B, James BO, Bonetto C, Cristofalo D, et al. Pattern of experienced and anticipated discrimination among people with depression in Nigeria: a cross-sectional study. Soc Psychiatry Psychiatr Epidemiol. 2014;49:259–66.
Lasalvia A. Tackling the mental illness stigma in low- and middle-income countries: lessons learned from high-income countries and mistakes to avoid. Epidemiol Psychiatr Sci. 2015;24:395–8 Available from: https://www.cambridge.org/core/journals/epidemiology-and-psychiatric-sciences/article/tackling-the-mental-illness-stigma-in-low-and-middleincome-countries-lessonslearned-from-highincome-countries-and-mistakes-to-avoid/83D63EA7FD15A3A3F2F9085E7E1700A2.
Rosen A. Destigmatizing day-to-day practices: what developed countries can learn from developing countries. World Psychiatry. 2006;5:21–24. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1472257/.
Alonso J, Buron A, Bruffaerts R, He Y, Posada-Villa J, Lepine JP, et al. Association of perceived stigma and mood and anxiety disorders: results from the world mental health surveys. Acta Psychiatr Scand. 2008;118:305–14.
Mathias K, Kermode M, San Sebastian M, Koschorke M, Goicolea I. Under the banyan tree--exclusion and inclusion of people with mental disorders in rural North India. BMC Public Health. 2015;15:–446 Available from: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-015-1778-2.
Maramis A, Van Tuan N, Minas H. Mental health in Southeast Asia. Lancet. 2011;377:700–2.
Minas H, Diatri H. Pasung: Physical restraint and confinement of the mentally ill in the community. Int J Ment Health Syst. 2008;2 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2442049/.
Tawiah PE, Adongo PB, Aikins M. Mental Health-Related Stigma and Discrimination in Ghana: Experience of Patients and Their Caregivers. Ghana Med J. 2015 [cited 2018 Jul 3];49:30–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26339082.
Lauber C, Rössler W. Stigma towards people with mental illness in developing countries in Asia. Int Rev Psychiatry [Internet]. 2007;19:157–78 Available from: https://www.ncbi.nlm.nih.gov/pubmed/17464793.
Mascayano F, Armijo JE, Yang LH. Addressing stigma relating to mental illness in low- and middle-income countries. Front Psychiatry. 2015;6:1–4.
Abdullah T, Brown TL. Mental illness stigma and ethnocultural beliefs, values, and norms. Clin Psychol Rev. 2011;31:934–48.
Semrau M, Evans-Lacko S, Koschorke M, Ashenafi L, Thornicroft G. stugma and discrimination related to mental illness in low- and middle-income countries. Epidemiol. Psychiatr. Sci. [Internet]. 2015;24:382–94. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25937022.
Yang LH, Kleinman A, Link BG, Phelan JC, Lee S, Good B. Culture and stigma: adding moral experience to stigma theory. Soc Sci Med. 2007;64:1524–35.
Yang LH, Thornicroft G, Alvarado R, Vega E, Link BG. Recent advances in cross-cultural measurement in psychiatric epidemiology: utilizing “what matters most” to identify culture-specific aspects of stigma. Int. J. Epidemiol. [internet]. 2014;43:494–510. Available from. https://www.ncbi.nlm.nih.gov/pubmed/24639447.
Edman JL, Johnson RC. Filipino American and Caucasian American beliefs about the causes and treatment of mental problems. Cultur Divers Ethnic Minor Psychol. 1999;5:380–6.
Thompson S, Hartel G, Manderson L, Woelz-Stirling N, Kelaher M. The mental health status of Filipinas in Queensland. Aust N Z J Psychiatry. 2002;36:674–80.
Corrigan PW, Rowan D, Green A, Lundin R, River P, Uphoff-Wasowski K, et al. Challenging two mental illness Stigmas : personal responsibility and dangerousness. Schizophr Bull. 2002;28:293–310.
Pescosolido BA, Medina TR, Martin JK, Long JS. The “Backbone” of Stigma: Identifying the Global Core of Public Prejudice Associated With Mental Illness. Am. J. Public Health [Internet]. 2013;103:853–60. Available from: https://www.ncbi.nlm.nih.gov/pubmed/23488508.
Gong F, Gage SJL, Tacata LA. Helpseeking behavior among Filipino Americans: a cultural analysis of face and language. J Community Psychol. 2003;31:469–88.
Javier JR, Supan J, Lansang A, Beyer W, Kubicek K, Palinkas LA. Preventing Filipino mental health disparities: perspectives from adolescents, caregivers, providers, and advocates. Asian Am J Psychol [Internet]. 2014;5:316–24 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4319658/.
Charmaz K. Constructing Grounded Theory. 2nd ed. SAGE Publications Ltd; 2014.
Charmaz K. Grounded theory methods in social justice research. In: Denzin NK, Lincoln YS, editors. SAGE Handb. Qual. Res. SAGE; 2011. p. 359–380.
Charmaz K. The Power of Constructivist Grounded Theory for Critical Inquiry. Qual. Inq. [Internet]. 2017;23:34–45. Available from: http://journals.sagepub.com/doi/10.1177/1077800416657105
City Government of Muntinlupa. POVERTY AND EMPLOYMENT STATISTICS [Internet]. 2017 [cited 2017 Jun 30].
Philippine Statistics Authority. Philippines National Demographic and Health Survey 2013. 2013 [cited 2017 Jun 30]. Available from: https://dhsprogram.com/pubs/pdf/FR294/FR294.pdf.
Boling W, Means M, Fletcher A. Quality of Life and Stigma in Epilepsy, Perspectives from Selected Regions of Asia and Sub-Saharan Africa. Brain Sci. [Internet]. Multidisciplinary Digital Publishing Institute (MDPI); 2018 [cited 2018 Jun 27];8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29614761.
Herrmann LK, Welter E, Berg AT, Perzynski AT, Van Doren JR, Sajatovic M. Epilepsy misconceptions and stigma reduction: Current status in Western countries. Epilepsy Behav. [Internet]. 2016 [cited 2018 Jun 27];60:165–73. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27208826.
Koch-Stoecker S. Neuropsychiatric issues in epilepsy. In: Matsuura M, Inoue Y, editors. Neuropsychiatr. issues epilepsy [Internet]. John Libbey Eurotext; 2010 [cited 2018 Jun 27]. p. 233. Available from: https://books.google.co.jp/books?id=FQXhAAAAQBAJ&pg=PA174&lpg=PA174&dq=epilepsy+Emil+Kraepelin&source=bl&ots=r35Oh0rwjA&sig=IZa-67-5hrTVkzSl4HEIoGkaobQ&hl=en&sa=X&ved=0ahUKEwjd26SwkvPbAhWEnZQKHUvrDZsQ6AEIsAEwEw#v=onepage&q=epilepsyAQ28EmilKraepelin&f=false.
World Health Organization. mhGAP Training Manuals - for the mhGAP Intervention Guide for mental, neurological and substance use disorders in non-specialized health settings, version 2.0 [Internet]. WHO. World Health Organization; 2017 [cited 2018 Jun 27]. Available from: http://www.who.int/mental_health/mhgap/training_manuals/en/
Tuliao AP. Mental health help seeking among Filipinos: a review of the literature. Asia Pacific J Couns Psychother [Internet]. 2014;5:124–36 Available from: http://www.tandfonline.com/doi/abs/10.1080/21507686.2014.913641.
Yang LH, Valencia E, Alvarado R, Link B, Huynh N, Nguyen K, et al. A theoretical and empirical framework for constructing culture-specific stigma instruments for Chile. Cad. saude coletiva [Internet]. 2013;21:71–9. Available from: /pmc/articles/PMC3753780/?report=abstract.
Hamilton S, Pinfold V, Cotney J, Couperthwaite L, Matthews J, Barret K, et al. Qualitative analysis of mental health service users’ reported experiences of discrimination. Acta Psychiatr Scand. 2016;134:14–22.
Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization world mental health surveys. JAMA [internet]. 2004;291:2581–90. Available from. http://www.ncbi.nlm.nih.gov/pubmed/15173149.
Wig NN, Suleiman MA, Routledge R, Murthy RS, Ladrido-Ignacio L, Ibrahim HH, et al. Community reactions to mental disorders. A key informant study in three developing countries. Acta Psychiatr. Scand. [Internet]. 1980;61:111–26. Available from: https://www.ncbi.nlm.nih.gov/pubmed/7361584.
Ando S, Yamaguchi S, Aoki Y, Thornicroft G. Review of mental-health-related stigma in Japan. Psychiatry Clin Neurosci. 2013;67:471–82.
van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Comparing stigmatising attitudes towards people with substance use disorders between the general public, GPs, mental health and addiction specialists and clients. Int J Soc Psychiatry [Internet]. 2014;61:539–49 Available from: http://isp.sagepub.com/cgi/doi/10.1177/0020764014562051.
Clement S, Jarrett M, Henderson C, Thornicroft G. Messages to use in population-level campaigns to reduce mental health-related stigma: consensus development study. Epidemiol Psichiatr Soc. 2010;19:72–9.
Dy MB. Values in Philippine culture and education. Washington, DC: CRVP; 1994.
Social Weather Stations. Social Weather Station Survey. [Internet]. 2017 [cited 2017 Nov 9]. Available from: https://www.sws.org.ph/swsmain/artcldisppage/?artcsyscode=ART-20170816103037
Pescosolido BA, Martin JK, Olafsdottir S, Long JS, Medina TR, Martin JK. The theory of industrial society and cultural schemata: does the “cultural myth of stigma” underlie the WHO schizophrenia paradox? Am J Sociol. 2015;121:783–825.
Araneta EG. Psychiatric Care of Pilipino Americans. In: Gaw AC, editor. Cult. Ethn. Ment. Illn. Washington, DC: American Psychiatric Press; 1993. p. 377–412.
Sanchez F, Gaw A. Mental health Care of Filipino Americans. Psychiatr Serv [Internet] 2007;58:810–815. Available from: https://www.ncbi.nlm.nih.gov/pubmed/17535941
Wonpat-Borja AJ, Yang LH, Link BG, Phelan JC. Eugenics, genetics, and mental illness stigma in Chinese Americans. Soc Psychiatry Psychiatr Epidemiol. 2012;47:145–56.
Yang LH, Purdie-Vaughns V, Kotabe H, Link BG, Saw A, Wong G, et al. Culture, threat, and mental illness stigma: identifying culture-specific threat among Chinese-American groups. Soc. Sci. Med. [internet]. Elsevier Ltd. 2013;88:56–67 Available from: https://doi.org/10.1016/j.socscimed.2013.03.036.
Yang LH, Kleinman A. “Face” and the embodiment of stigma in China: the cases of schizophrenia and AIDS. Soc Sci Med. 2008;67:398–408.
Abad PJB, Tan ML, Baluyot MMP, Villa AQ, Talapian GL, Reyes ME, et al. Cultural beliefs on disease causation in the Philippines: challenge and implications in genetic counseling. J Community Genet. 2014;5:399–407.
De Los Monteros KE, Gallo LC. The relevance of fatalism in the study of Latinas’ cancer screening behavior: a systematic review of the literature. Int J Behav Med. 2011;18:310–8.
Roberts RE, Roberts CR, Chen IG. Fatalism and risk of adolescent depression. Psychiatry [internet]. 2000;63:239–52. Available from. http://www.ncbi.nlm.nih.gov/pubmed/11125670.
Cheng H, Sit JWH, Twinn SF, Cheng KKF, Thorne S. Coping with breast Cancer survivorship in Chinese women the role of fatalism or fatalistic voluntarism. Cancer Nurs. 2013;36:236–44.
Gonzalez P, Nuñez A, Wang-Letzkus M, Lim J-W, Flores KF, Nápoles AM. Coping with breast cancer: reflections from Chinese American, Korean American, and Mexican American women. Heal Psychol [Internet] 2016;35:19–28. Available from: https://www.ncbi.nlm.nih.gov/pubmed/26389720.
Nurjannah I ,Mills J PT& UK. Human rights of the mentally ill in Indonesia. Int Nurs Rev. 2015;62:153–61.
Habtamu K, Alem A, Hanlon C. Conceptualizing and contextualizing functioning in people with severe mental disorders in rural Ethiopia: a qualitative study. BMC psychiatry [internet]. 2015;15:34. Available from: https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-015-0418-9.
An act establishing a national mental health policy for the purpose of enhancing the delivery of integrated mental health services, promoting and protecting the rights of persons utilizing psychiatric, neurologic and psychosocial health services, APPROPRI [Internet]. Republic of the Philippines; 2018. Available from: http://www.officialgazette.gov.ph/2018/06/20/republic-act-no-11036/
Kitchener B, Jorm A. Mental health first aid training for the public: evaluation of effects on knowledge, attitudes and helping behavior. BMC Psychiatry [Internet]. 2002;2:10. Available from: http://www.biomedcentral.com/1471-244X/2/10
Morgan AJ, Ross A, Reavley NJ. Systematic review and meta-analysis of Mental Health First Aid training: Effects on knowledge, stigma, and helping behaviour. Doran CM, editor. PLoS One [Internet]. 2018 [cited 2018 Jun 28];13:e0197102. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0197102.
Bond KS, Jorm AF, Kitchener BA, Reavley NJ. Mental health first aid training for Australian medical and nursing students: an evaluation study. BMC Psychol. [Internet]. 2015 [cited 2018 Jun 28];3:11. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25914827.
Jorm AF, Kitchener BA, Fischer J-A, Cvetkovski S. Mental Health First Aid Training by e-Learning: A Randomized Controlled Trial. Aust. New Zeal. J. Psychiatry [Internet]. 2010 [cited 2018 Jun 28];44:1072–81. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21070103.
Corrigan PW, Morris SB, Michaels PJ, Rafacz JDRN. Challenging the public stigma of mental illness: a meta-analysis of outcome studies. Psychiatr. Serv. [Internet]. 2012;63:963–73 Available from: https://www.ncbi.nlm.nih.gov/pubmed/23032675.
Corrigan PW, Michaels PJ, Vega E, Gause M, Larson J, Krzyzanowski R, et al. Key ingredients to contact-based stigma change: A cross-validation. Psychiatr. Rehabil. J. [Internet]. 2014 [cited 2018 Jun 28];37:62–4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24417232.
Corrigan PW, Larson JE, Michaels PJ, Buchholz BA, Del Rossi R, Fontecchio MJ, et al. Diminishing the self-stigma of mental illness by coming out proud. Psychiatry Res. 2015;229:148–54.
Rüsch N, Abbruzzese E, Hagedorn E, Hartenhauer D, Kaufmann I, Curschellas J, et al. Efficacy of Coming Out Proud to reduce stigma’s impact among people with mental illness: pilot randomised controlled trial. Br. J. Psychiatry [Internet]. 2014 [cited 2018 Jun 28];204:391–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24434073.
Corrigan PW, Rüsch N, Scior K. Adapting disclosure programs to reduce the stigma of mental illness. Psychiatr. Serv. [internet]. 2018 [cited 2018 Jun 28];appi.Ps.2017004. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29606076.
Acknowledgments
We are grateful to the interviewees for their participation. We would like to thank Dr. Magdalena C. Meana, Dr. Ma. Luisa Babaran-Echavez, and barangay health workers for their assistance with data collection.
Availability of data and materials
The transcripts from the interviews are confidential and will not be shared.
Author information
Authors and Affiliations
Contributions
CT had a major role in the conception of the study, undertook the data collection, carried out the data analysis, and had a major role in writing the manuscript. MT contributed to the design of the study, assisted the data collection and interpretation, and supervised writing the manuscript. ET assisted data collection, conducted data analysis, and revised the manuscript. YT assisted data collection and revised the manuscript. HM supervised the design of the study, had a role in data analysis, and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the ethical committee of the Graduate School of Health Sciences, Kobe University, Japan (reference number 561). The study was conducted in accordance with the ethical guidelines set forth by the Declaration of Helsinki and the Ethical Guidelines for Medical and Health Research Involving Human Subjects provided by the Ministry of Health, Labour, and Welfare of Japan. The City Health Office of the local government approved a head of time our study protocol, especially ethical aspects for potentially participating citizens. Potential participants received written and oral information about the study. It was emphasized that participation was voluntary. During the data collection, we obtained written consent from all the interviewees and verbal assent from PMHP whose carers participated in the interviews. In the case where the interviewee was under 18 years old, we gained verbal assent from them and written consent from their parents.
Consent for publication
Participants were informed that the information they shared in the interviews would be published in anonymised form. Written informed consent for publication was obtained.
Competing interests
The authors declare that they have no competing interest.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Interview guide for interviews with people with mental health problems. A set of questions we referred while interviewing PMHP. (DOCX 88 kb)
Additional file 2:
Interview guide for interviews with carers and community health volunteers. A set of questions we referred while interviewing carers and community health volunteers. (DOCX 90 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tanaka, C., Tuliao, M.T.R., Tanaka, E. et al. A qualitative study on the stigma experienced by people with mental health problems and epilepsy in the Philippines. BMC Psychiatry 18, 325 (2018). https://doi.org/10.1186/s12888-018-1902-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-018-1902-9