Abstract
Background
The aim of study was to investigate predictors of long term use of psychiatric services of patients with recent-onset schizophrenia.
Methods
A cohort of 50 clinically stable patients with recent-onset schizophrenia was included in a randomized controlled trial comparing early integrated treatment with treatment as usual. Recent onset was defined as emergence of psychotic symptoms for the first time during the preceding 2 years. The follow up period was from the date of randomization and until 12 years after termination of treatment trial, 14 years forward.
Results
Score on Brief psychiatric rating scale both at baseline and after 2 years of treatment, suicide attempts during 2 years of treatment and being an inpatient during 2 years of treatment were significant predictors of long term use of services.
Conclusion
High score on Brief psychiatric rating scale, suicide attempts and being admitted as inpatient early in the course of schizophrenia are possible predictors of long term use of services.
Trial registration
ClinicalTrials.gov NCT00184509. Registered 15 September 2005.
Similar content being viewed by others
Background
Schizophrenia has been described as a chronic, relapsing disease, although with a heterogeneous course and outcome [1]. It manifests itself as a mixture of positive, negative, cognitive and mood symptoms, with general decay in function and social disability [2]. Schizophrenia is associated with increased suicide-rate [3] and reduced longevity [4]. Onset of psychotic symptoms usually occurs during adolescence or early adulthood.
The so called “critical period hypothesis” claims that in schizophrenia deterioration occurs rapidly during a period of few years following psychotic debut [5]. Subsequently the disease reaches a “plateau”, deterioration slows down or halts, and the disease reaches a level of morbidity which remains relatively stable [6]. Interventions applied at the early stages of the critical period might have the potential of preventing or diminishing the progressive deterioration and thereby improving long term prognosis [7].
Re-hospitalization following relapse is one of the costliest interventions in schizophrenia and increases the burden associated with psychotic illness [8–10]. The prediction of prognosis early in the course of illness can help developing optimal treatment strategies throughout the duration of disease course. Identifying risk factors for the use of in- and outpatient psychiatric services may have implications on clinical decisions, policy for patient care, program development, and service planning. Early identification of poor responders would allow timely adjustments to management programs and modifiable predictors may present specific treatment targets.
The aim of the study was to investigate possible baseline and 2 year predictors of long term use of psychiatric services of patients with recent-onset schizophrenia.
Methods
Participants and design
A cohort of 50 patients with recent-onset non-affective psychosis were included in a randomized controlled trial comparing early integrated treatment (IT) with treatment as usual (TAU). Recent onset was defined as emergence of psychotic symptoms for the first time during the preceding 2 years. TAU comprised optimal pharmacotherapy and case management, while IT also included cognitive-behavioural family treatment, which incorporated skills training, cognitive-behavioural strategies for residual psychotic and non-psychotic problems and home-based crisis management. Participants were randomly allocated using a sequence of sealed pre-numbered envelopes with group assignments according to random numbers provided by the international Optimal Treatment Project administration. Gender was stratified in blocks of varying size (between 8 and 12 and with a ratio of 3:2 of IT to TAU) ensuring that a majority of the patients received the experimental treatment. Prior to randomization written informed consent was obtained. The intervention program and the results of the trial are reported in detail elsewhere [11–14], see also the Additional file 1.
The research was carried out in compliance with the Helsinki Declaration and the study was approved by The Regional Committee for Medical and Health Research Ethics in Central-Norway.
Recruitment
The patients were included from 1992 to 1997. The catchment area was a county in Mid-Norway with a population of about 250.000 inhabitants. At the time of inclusions, no effort was made to reduce the delay in seeking treatment in this region, but efforts were made to get referrals of all patients with recent onset psychotic disorder from psychiatric inpatient units, outpatient clinics, and general practitioners in the area. Patients who were clinically stable and were expected to reside in the county for at least 1 year after inclusion were asked to participate in the study. Patients with substance use disorders or mental retardation were excluded.
The focus of the present study was to identify predictors of long term use of services for patients with a recent-onset psychosis.
Follow up
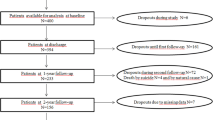
The follow up period was from the date of randomization until 12 years after termination of treatment trial, 14 years forward. The cohort was divided into two groups based on the number of days as psychiatric inpatients during 12 years after termination of the treatment trial. This was based on inspection of the data showing a marked dividing line in participants’ inpatient days around 100 days.
Measures
Data on duration and number of psychiatric hospital admissions was extracted from the official Patient Administrative System, a standard system for clinical data in the health trust. Data was verified trough scrutiny and cross-checking of medical records.
Information used in this study was registered at baseline and 2 years after inclusion into the original study.
Baseline factors: Age, gender and residence. Diagnosis according to DSM-IV and overall function assessed using Global assessment of function (GAF) [15]. Psychopathology was assessed using Brief psychiatric rating scale (BPRS) [16] and Target symptoms rating scale (TSRS) [17]. Incidences and duration of hospitalisations before study entry was also recorded.
Factors after the 2 year treatment trial
Overall function assessed using Global assessment of function (GAF) [15] and psychopathology assessed using Brief psychiatric rating scale (BPRS) [16] and Target symptoms rating scale (TSRS) [17] at the end of the trial. Suicide attempts defined as attempts with an intention to die and adherence to psychosocial treatment and adherence to treatment with psychotropics were also registered during the 2 year trial. Incidences and duration of hospitalisations, incidences and duration of in- and outpatient coercion and contact with community or specialist health services were also registered during the 2 year treatment trial. Integrated treatment or treatment as usual according to the randomized controlled study the 2 year treatment trial. In Table 1 possible predictors of long term use of services at baseline and observations during 2 years of treatment are referred.
Operational variables
During the 2 year treatment trial
“Psychotic relapse” was defined as a two-point increase and a score of six or seven on the TSRS (0–7) [17] and a score of six or seven on one of the key psychotic symptom items on the BPRS (1–7) OR a two-point increase and a score of four or five on the TSRS following a period of remission.
A score of five or more on “hallucinations” or “unusual thoughts” items on BPRS for more than six consecutive months was defined as having “persistent psychotic symptoms” [11]. Positive symptoms sub-score on BPRS was defined as sum score of the items “unusual thought content”, “suspiciousness”, “grandiosity”, “hallucinations”, “conceptual disorganization” and “bizarre behaviour”. Negative symptoms sub-score was defined as sum score of the items “blunted affect”, “emotional withdrawal”, “motor retardation”, “self-neglect” and “disorientation” [18]. Compliance with psychosocial treatment was considered “good” if patients attended at least one session per month during the treatment period. Patients with less than 1 month or fewer than four single weeks without medication were rated as adherent with medication. Patients receiving depot injections of antipsychotics at any time were recorded as depot users [11].
During the 12 year follow-up
“Frequent users” were defined as patients with 100 or more hospital days during the follow up period. “Non-frequent users” were defined as a patient with less than 100 days as psychiatric inpatients during the follow up period.
A subgroup of “frequent users”, with more than 500 inpatient days during the follow up period was defined as “extensive users” for further exploration.
Missing data
Twenty four months registration on the BPRS was missing for five patients. In these cases we used last available registration. Three patients had last registration at 22 months, one at 20 months and one at 6 months.
Analysis
Statistical methods
First, bivariate relationships between frequent users and the independent variables were explored. Second, possible predictors of becoming frequent users were analysed using logistic regression.
For logistic regression, general rules of thumb state that there should be at least five to ten times as many cases in the smallest group as the number of predictors [19, 20]. Hence, we included four predictors simultaneously.
Selection of variables
Selecting factors for inclusion in a multivariable model based on statistical significance in a bivariate analysis is not optimal as it may exclude possible confounders that impacts outcome when included in the model [21]. We therefore based our selection of variables on previous research on prognostic factors in schizophrenia and on what we considered of clinical relevance.
Age at onset and male gender are known to affect prognosis and the extent of use of services of patients with schizophrenia [22, 23], BPRS has been shown to be an applicable tool to predict length of hospital stay [24] and previous admissions have been found to predict future admissions [25]. We selected age, gender and treatment regime (Integrated treatment or treatment as usual) to be adjusted for in the logistic regression analysis of potential predictors of long term use of services.
There was a striking difference between the groups in suicide attempts during the 2 year treatment trial (zero patients attempted suicide in the non-frequent users group and five in the frequent users group) and suicidal behaviour has been found to be a predictor of psychiatric admissions [26].
Statistical analyses
Positive symptoms after 2 years were influenced by an extreme score in the non-frequent group and the variance of days hospitalized and number of hospitalizations during the 2 year treatment period, days involuntary hospitalized and days involuntary outpatient coercion during 2 year treatment period in the two groups, were skewed and therefore we used the non-parametric Mann-Whitney test for these variables in the bivariate analysis. Proportions were compared using the unconditional z-pooled test as recommended by Lydersen, Langaas and Bakke (2012). This test preserves the type I error and has substantially higher statistical power than Fisher's exact test in small samples.
Potential predictors for frequent users were analysed using logistic regression, with one potential predictor at a time, unadjusted, and adjusted for age, sex and treatment group (IT or TAU). Hospital days during 12 years after end of treatment were not normally distributed. As suggested by Tabatchnick & Fidell [27], we attempted the log transformation (after adding 1 to avoid trying to take the logarithm of zero) and the square root transformation. Only the square root gave acceptable approximation to the normal distribution, judged by visual inspection of QQ plots.
As secondary analyses we carried out linear regression analyses with square root transformed days in hospital during 12 years after treatment as dependent variable.
Statistical analyses were done in SPSS 20 except the unconditional z-pooled test which was done in the software http://www4.stat.ncsu.edu/~boos/exact/.
Results
Complete 12 year follow-up data on use of services for 45 of the 50 patients were accessible from hospital records. Five patients had migrated from the region. One patient, randomized into the TAU group, died 4 years and 9 months into the follow-up period. Data from the deceased participant was included. Among the 45 patients, 21 were frequent users and 24 non-frequent users, see Table 2.
Frequent users had a mean (SD) of 710 (656) days as inpatients and a median of 423 (Min 104–Max 2521), while non-frequent users had a mean (SD) of 13 (29) days and a median of zero (Min 0–Max 97), p < 0.001. During the 12 year follow-up period, 17 patients had no hospitalizations and 10 patients were hospitalized for more than 500 days.
Bivariate analysis
In the bivariate analysis, gender, GAF, total score BPRS and score on BPRS positive factors at baseline were significantly associated with being a frequent user.
After the 2 years treatment trial were GAF, total score BPRS, psychotic relapse, suicide attempt, number of hospitalizations, days as inpatient, involuntary admitted, days involuntary admitted, outpatient coercion, days with outpatient coercion and not having good adherence with oral or depot antipsychotics significantly associated with being a frequent user. See Tables 3 and 4.
Regression analysis
Female gender and high score on BPRS and low score on GAF were significant baseline predictors of becoming a frequent user in the logistic regression analysis, see Table 5, both unadjusted and adjusted for age, gender and treatment group.
After the 2 years treatment trial, score on BPRS, score on GAF, being admitted to hospital and having a psychotic relapse were all significant predictors for being a frequent user.
As an alternative, the analyses were carried out in linear regression. In linear regression, the dependent variable number of days was square root transformed to make the residuals approximately normally distributed. Results (data no shown) were similar to those in logistic regression.
In an attempt to identify patients in high risk of long-term frequent or extensive use of services we constructed a “high risk group” from categorical variables showing the most profound difference between groups during the 2 year treatment trial; suicide attempt, outpatient coercion and being hospitalised. 22 patients, 75% of frequent users and all of extensive users, fulfilled the inclusion criteria for the “high risk group”. See Table 6.
Discussion
This is one of few long-term prospective studies of recent onset psychosis and the main findings are that both at baseline and at 2 years there was a remarkable overlap in the predictive value of the psychopathological indices, i.e., this kind of stability indicate that in order to gain knowledge about long term course and hospitalization costs, it may be sufficient to assess risk factors at illness onset and initial treatment response.
During the 2 year treatment trial, poorer functioning, relapses and psychiatric hospitalizations, poor compliance with medication and suicide attempts predict higher use of inpatient services in the long-term follow-up. These also suggest that the initial treatment response is important, as is insight.
Total score on BPRS both at baseline and at 2 years were significant predictors of use of services 12 years after end of trial. Earlier research has shown predictive validity of BPRS score on length of hospital stay and its applicability in identification of patients who required non-acute extended hospital care [18, 28, 29]. Our results suggest that BPRS can be used to identify patients early in the course of schizophrenia who are likely to be frequent users of inpatient services in the future. This can be helpful in planning future interventions for this group of patients in order to improve prognosis and minimize the need of psychiatric services in the future.
Several factors the two first years that usually are considered to have a negative influence on the course of schizophrenia as reduced function (GAF), psychotic relapses, being admitted, being under coercion and reduced compliance with treatment were associated with being a frequent user in the next 12 years in bivariate analyses.
Suicide attempts during intervention period showed a significant relation to use of services in the unconditional z-pooled test indicating a significant association. In the Northern Finland Birth Cohort [30] both suicide attempts and high level of symptoms at baseline predicted poor outcome. Up to 5% of patients with schizophrenia will commit suicide [31] and the estimated rate of suicide attempts are close to 10 times that rate [32]. In our sample one patient died of complications to a suicide attempt and five patients attempted suicide. This relatively low rate of suicidality compared to other studies, may be due to the inclusion criteria excluding patients with substance abuse; a known risk factor for suicide in schizophrenia [33].
Male gender was a significant predictor in the logistic regression analysis for being a non-frequent user, both unadjusted and when adjusted for age and treatment alternatives. Male gender is a known risk factor of suicidality [34], but all of the patients in the present study who attempted or committed suicide were female. Also in the literature males have consistently been found to have a less favourable course of illness than females, [23, 35, 36], but our results appear to show the opposite tendency regarding use of services. The gender differences in suicide attempts and use of services might be due to the exclusion of patients with substance abuse as in schizophrenia this is more prevalent among males [37].
A considerable number of patients, 17 (38%), were not hospitalized during the follow up period. Two other studies with 10 years follow-up of early psychosis showed that around 40% of the patients in the OPUS study had recovery or symptom remission at 10 years follow-up [38] and 46% in the ÆSOP-study had been symptom free for 2 years [39]. This is in accordance to previous research on long term outcome in schizophrenia showing good outcome in up to 50% of patients with schizophrenia [40]. In a previous report we have described that ten patients were extensive users and had more than 500 inpatient days and were responsible for 76% of all inpatient days during the follow up period (14).
By categorizing patients into a high risk group defined by being admitted or having a suicide attempt or at outpatient coercion in the first 2 years in the treatment study, a positive predictive value of 82% for being a frequent user were found. This can be a useful tool when planning future treatment strategies.
Limitations
A sample size of 45 limited the number of variables included in the logistic regression analysis. The selection of variables included was based on previous research on prognostic factors in schizophrenia and on what we considered of clinical significance in the actual sample. Only a large sample size would have been sufficient to test all possible variables from the bivariate analysis. Other variables chosen by other assumptions might have given different results. Dichotomizing a continuous outcome variable may have reduced the statistical power to detect a relation between the independent variables and outcome [41].
Use of inpatient services may not be an optimal measure of outcome in schizophrenia and other aspects of recovery should also be considered. Clinically unstable patients and patients with substance abuse were not included in the study and this might reduce the generalizability of the study. The long observation period, the possibility to get complete data from 90% of the participants and strict selection of appropriate statistical measures are major strengths in the study.
Conclusion
Being admitted in the start of treatment, scores on BPRS and history of suicide attempts appear to be applicable measures in predicting the extent of future use of inpatient services in schizophrenia.
Abbreviations
- BPRS:
-
Brief psychiatric rating scale
- GAF:
-
Global assessment of function
- IT:
-
Integrated treatment
- SD:
-
Standard deviation
- TAU:
-
Treatment as usual
- TSR:
-
Target symptoms rating scale
References
Haro J, Novick D, Suarez D, Ochoa S, Roca M. Predictors of the course of illness in outpatients with schizophrenia: a prospective three year study. Prog Neuro-Psychopharmacol Biol Psychiatry. 2008;32(5):1287–92.
Lieberman JA, Perkins D, Belger A, Chakos M, Jarskog F, Boteva K, Gilmore J. The early stages of schizophrenia: speculations on pathogenesis, pathophysiology, and therapeutic approaches. Biol Psychiatry. 2001;50(11):884–97.
Palmer BA, Pankratz VS, Bostwick JM. The lifetime risk of suicide in schizophrenia: a reexamination. Arch Gen Psychiatry. 2005;62(3):247.
Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007;64(10):1123.
McGorry PD, Killackey E, Yung A. Early intervention in psychosis: concepts, evidence and future directions. World Psychiatry. 2008;7:148–56.
Thara R. Twenty-year course of schizophrenia: the Madras Longitudinal Study. Can J Psychiatry. 2004;49:564–9.
Bird V, Premkumar P, Kendall T, Whittington C, Mitchell J, Kuipers E. Early intervention services, cognitive–behavioural therapy and family intervention in early psychosis: systematic review. Br J Psychiatry. 2010;197:350–6.
Almond S, Knapp M, Francois C, Toumi M, Brugha T. Relapse in schizophrenia: costs, clinical outcomes and quality of life. Br J Psychiatry. 2004;184(4):346–51.
Weiden PJ, Olfson M. Cost of relapse in schizophrenia. Schizophr Bull. 1995;21(3):419–29.
Ascher-Svanum H, Zhu B, Faries D, Salkever D, Slade E, Peng X, Conley R. The cost of relapse and the predictors of relapse in the treatment of schizophrenia. BMC Psychiatry. 2010;10(1):2.
Grawe RW, Falloon IRH, Widen JH, Skogvoll E. Two years of continued early treatment for recent-onset schizophrenia: a randomised controlled study. Acta Psychiatr Scand. 2006;114(5):328–36.
Morken G, Widen JH, Grawe RW. Non-adherence to antipsychotic medication, relapse and rehospitalisation in recent-onset schizophrenia. BMC Psychiatry. 2008;8(1):32.
Morken G, Grawe RW, Widen JH. Effects of integrated treatment on antipsychotic medication adherence in a randomized trial in recent-onset schizophrenia. J Clin Psychiatry. 2007;68(4):566–71.
Sigrúnarson V, Gråwe RW, Morken G. Integrated treatment vs. treatment-as-usual for recent onset schizophrenia; 12 year follow-up on a randomized controlled trial. BMC Psychiatry. 2013;13:200. doi:10.1186/1471-244X-13-200. PubMed PMID: 23898805; PubMed Central PMCID: PMC3733816.
Association AP. Diagnostic and statistical manual of mental disorders DSM-IV. 4th ed. 1994.
Lukoff D, Liberman RP, Nuechterlein KH. Symptom monitoring in the rehabilitation of schizophrenic patients. Schizophr Bull. 1986;12(4):578–602.
Falloon IR, Boyd JL, McGill CW, Razani J, Moss HB, Gilderman AM. Family management in the prevention of exacerbations of schizophrenia: a controlled study. N Engl J Med. 1982;306(24):1437–40.
Anderson SW, Crist AJ, Payne N. Predicting inpatient length of stay with the expanded version of the brief psychiatric rating scale (Version 4.0). Psychiatr Serv. 2004;55(1):77–9.
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49(12):1373–9.
Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol. 2007;165(6):710–8.
Sun G-W, Shook TL, Kay GL. Inappropriate use of bivariable analysis to screen risk factors for use in multivariable analysis. J Clin Epidemiol. 1996;49(8):907–16.
Rabinowitz J, Levine SZ, Häfner H. A population based elaboration of the role of age of onset on the course of schizophrenia. Schizophr Res. 2006;88(1–3):96–101.
Angermeyer MC, Kühn L, Goldstein JM. Gender and the course of schizophrenia: differences in treated outcomes. Schizophr Bull. 1990;16(2):293.
Averill P, Hopko D, Small D, Greenlee H, Varner R. The role of psychometric data in predicting inpatient mental health service utilization. Psychiatry Q. 2001;72(3):215–35.
Mortensen PB, Eaton W. Predictors for readmission risk in schizophrenia. Psychol Med. 1994;24(01):223–32.
Hillard JR, Slomowitz M, Deddens J. Determinants of Emergency Psychiatric Admission for adolescents and adults. Am J Psychiatry. 1988;145(11):1416–9.
Tabachnick BG. Fidell LS. Using multivariate statistics: Osterlind SJ; 2001.
Averill PM, Hopko DR, Small DR, Greenlee HB, Varner RV. The role of psychometric data in predicting inpatient mental health service utilization. Psychiatry Q. 2001;72(3):215–35.
Hopko DR, Lachar D, Bailley SE, Varner RV. Assessing predictive factors for extended hospitalization at acute psychiatric admission. Psychiatr Serv. 2001;52(10):1367–73.
Jaaskelainen E, Haapea M, Rautio N, Juola P, Penttila M, Nordstrom T, Rissanen I, Husa A, Keskinen E, Marttila R, et al. Twenty Years of Schizophrenia Research in the Northern Finland Birth Cohort 1966: A Systematic Review. Schizophrenia research and treatment. 2015;2015:524875.
Tatarelli-roberto R. Suicide risk in schizophrenia: learning from the past to change the future. Ann Gen Psychiatry. 2007;6:10.
Roy A. Suicide in chronic schizophrenia. Br J Psychiatry. 1982;141(2):171–7.
Hawton K, Sutton L, Haw C, Sinclair J, Deeks JJ. Schizophrenia and suicide: systematic review of risk factors. Br J Psychiatry. 2005;187(1):9–20.
De Hert M, McKenzie K, Peuskens J. Risk factors for suicide in young people suffering from schizophrenia: a long-term follow-up study. Schizophr Res. 2001;47(2–3):127–34.
Abel KM, Drake R, Goldstein JM. Sex differences in schizophrenia. Int Rev Psychiatry. 2010;22(5):417–28.
Szymanski S, Lieberman JA, Alvir JM, Mayerhoff D, Loebel A, Geisler S, Chakos M, Koreen A, Jody D, Kane J. Gender differences in onset of illness, treatment response, course, and biologic indexes in first-episode schizophrenic patients. A J Psychiatry. 1995;152(5):698–703.
Dixon L. Dual diagnosis of substance abuse in schizophrenia: prevalence and impact on outcomes. Schizophr Res. 1999;0(0):S93–100.
Austin SF, Mors O, Secher RG, Hjorthoj CR, Albert N, Bertelsen M, Jensen H, Jeppesen P, Petersen L, Randers L, et al. Predictors of recovery in first episode psychosis: the OPUS cohort at 10 year follow-up. Schizophr Res. 2013;150(1):163–8.
Revier CJ, Reininghaus U, Dutta R, Fearon P, Murray RM, Doody GA, Croudace T, Dazzan P, Heslin M, Onyejiaka A, et al. Ten-Year Outcomes of First-Episode Psychoses in the MRC AESOP-10 Study. J Nerv Ment Dis. 2015;203(5):379–86.
Häfner H, an der Heiden W. The course of schizophrenia in the light of modern follow-up studies: the ABC and WHO studies. Eur Arch Psychiatry Clin Neurosci. 1999;249(4):S14–26.
Altman DG, Royston P. Statistics notes: the cost of dichotomising continuous variables. BMJ. 2006;332(7549):1080.
Acknowledgements
We thank patients for their participation in the study, and the health professionals who facilitated our work.
The study was supported and financed by the Central Norway Regional Health Authority. None of the data was presented earlier either in written or oral form. None of the authors have any financial affiliations to declare.
Funding
The study was funded by the Norwegian Research Council, the Norwegian Ministry of Health and The Central Norway Regional Health Authority.
Availability of data and materials
At the time of the point of recruitment to the trial which is more than 16 years ago, the informed consents for participating did not include the possibility for publication of the dataset. The dataset also contains indirect identifiers of the participants which makes publication of patient data difficult.
Authors’ contributions
VS, GM and RWG contributed to the conception and design, the analysis and interpretation of the data. SL contributed to the analysis and interpretation of data. All authors drafted the article and revised it critically. All authors read and approved the version of the manuscript to be published.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The research was carried out in compliance with the Helsinki Declaration and the study was approved by The Regional Committee for Medical and Health Research Ethics in Central-Norway. Prior to randomization written informed consent was obtained.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1:
Supplementary description of methods in the original study. The methods used in the original 2 years randomised controlled trial are described here. (DOCX 17 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Sigrúnarson, V., Gråwe, R.W., Lydersen, S. et al. Predictors of long term use of psychiatric services of patients with recent-onset schizophrenia: 12 years follow-up. BMC Psychiatry 17, 18 (2017). https://doi.org/10.1186/s12888-016-1186-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-016-1186-x