Abstract
Background
Enterococcus gallinarum (EG) is typically found in the gastrointestinal tracts of birds and mammals. Although its strains are rarely isolated from clinical specimens, EG can lead to septicemia in immunocompromised individuals. EG infections are uncommon in household settings, but their incidence has been rising due to increased antibiotic usage and invasive treatments, particularly in Neonatal Intensive Care Units (NICUs). EG inherently exhibits resistance to vancomycin but is highly sensitive to linezolid. Despite showing in vitro resistance, vancomycin has shown clinical efficacy in treating EG meningitis.
Case presentation
A neonate born at 30 + 2 weeks gestation was admitted to the Neonatal Intensive Care Unit (NICU) after EG was detected in blood and cerebrospinal fluid cultures. Susceptibility testing indicated that the bacterial strain was resistant to vancomycin and sensitive to linezolid. Initially, vancomycin was selected for treatment. However, due to persistent EG cultures in the blood and cerebrospinal fluid, the treatment was adjusted to linezolid. This led to a rapid decrease in platelet (PLT) count, suspected to be an adverse reaction. Concurrently, the patient experienced recurrent fever and elevated inflammatory marker levels, prompting the discontinuation of linezolid and a return to vancomycin. Subsequent administration of vancomycin stabilized the patient’s condition, as evidenced by improved C-reactive protein (CRP), procalcitonin (PCT), and cerebrospinal fluid parameters, ultimately leading to discharge after an eight-week treatment period.
Conclusion
This retrospective analysis highlights the efficacy of vancomycin in treating EG infections, suggesting that specific genetic phenotypes may influence treatment sensitivity. Monitoring vancomycin blood levels is crucial for determining treatment effectiveness.
Similar content being viewed by others
Background
Enterococcus gallinarum (EG) is a predominant component of the normal flora in the intestinal tracts of avian species. Although its strains are seldom isolated from clinical specimens, EG, a facultative anaerobe, catalase-negative, chain-forming gram-positive D-group coccus, is occasionally found in human foods such as fish, meat, and cheese. In immunocompromised hosts, EG can lead to septicaemia. Despite some reports, the clinical epidemiology of EG remains poorly understood. Colonization and infection by species of the E. gallinarum group are less frequent than those of other well-known enterococcal species, such as E. faecalis and E. faecium. However, according to existing trends, their frequency may increase worldwide [1]. Although the isolation of EG from cerebrospinal fluid is infrequent, its occurrence has been rising due to increased antibiotic use and invasive therapeutic interventions, particularly in NICUs [2]. EG inherently exhibits resistance to vancomycin but shows high sensitivity to linezolid [3]. Despite in vitro resistance, vancomycin has demonstrated clinical efficacy in treating EG meningitis.
Case presentation
A male neonate, born at 30 + 2 weeks gestation and weighing 1.79 kg, was admitted to a local hospital due to progressive leukopenia over three days. Initially, the infant received noninvasive ventilation and ceftazidime for infection control. However, day 1 of admission at the local hospital, a decrease in leukocytes prompted a switch to cefepime/tazobactam. Day 2 of admission, frequent episodes of respiratory arrest necessitated invasive ventilatory support, and further leukocyte reduction led to the initiation of meropenem. Day 3 of admission, blood culture revealed the presence of EG, and cerebrospinal fluid examination indicated purulent meningitis with a white blood cell (CSF-WBC) count of 10,050 × 106/L and a protein concentration of 3120 mg/L. In response, vancomycin was initiated for infection control, and the patient was transferred to our hospital for further management.
Upon admission, the infant exhibited a temperature of 36.5 °C, a pulse rate of 140 beats/min, a respiratory rate of 53 breaths/min, a blood pressure of 57/34 mmHg, and an oxygen saturation of 98% (under normobaric oxygen supply). The infant did not display seizure activity but showed poor responsiveness without irritability or agitation. Blood tests revealed a white blood cell (WBC) count of 9.23 × 109/L, a neutrophil percentage (NE%) of 58.5%, a platelet (PLT) count of 71 × 109/L, a C-reactive protein (CRP) level of 101 mg/L, and a procalcitonin (PCT) level of 12.28 ng/mL. Cranial ultrasonography revealed no significant abnormalities. On the first day after admission, the infant received intravenous meropenem (0.71 g, 40 mg/kg) and vancomycin (0.027 g, 15 mg/kg) every 8 h. By the fifth day, the blood concentration of vancomycin reached 38.4 µg/mL, leading to a dose reduction to 10 mg/kg every 12 h. On the sixth day, blood tests revealed a WBC of 12.13 × 109/L, an NE percentage of 46.9%, a PLT of 288 × 109/L, a CRP concentration of 9 mg/L, and a PCT concentration of 0.58 ng/mL. Cultures from cerebrospinal fluid and blood confirmed the presence of EG (identified using bile esculin agar (BEA) and biochemical reactions). Drug sensitivity tests (using the broth method and MIC method) demonstrated resistance to vancomycin (minimum inhibitory concentration (MIC) of 1 mg/L), penicillin (MIC ≥ 64 mg/L) and ampicillin (MIC ≥ 32 mg/L), but sensitivity to tetracycline (MIC ≤ 8 mg/L) and linezolid (MIC of 2 mg/L). CSF analysis revealed a CSF-WBC of 518 × 106/L, a protein concentration of 3549 mg/L, a glucose concentration of 1.15 mmol/L, and a chloride concentration of 134.2 mmol/L. The laboratory indicators and antimicrobial agents used are detailed in Table 1.
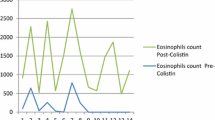
Despite a decrease in inflammatory markers and cerebrospinal fluid leukocyte count, the patient continued receiving combined therapy with meropenem and vancomycin, while the patient’s condition was continuously monitored. On the 11th day, the vancomycin concentration was 9.02 µg/mL. By the 14th day of treatment, with no significant reduction in cerebrospinal fluid protein (CSF-WBC 266 × 106/L, protein 3453 mg/L), vancomycin was changed to linezolid (0.02 g, 10 mg/kg) administered intravenously every 8 h, based on drug sensitivity results and treatment experience. On the 18th day after admission, the patient developed a fever of 37.7 °C. Blood tests revealed a WBC of 9.63 × 109/L, an NE% of 29.9%, a PLT of 55 × 109/L, a CRP of 54 mg/L, and a PCT of 1.98 ng/mL. Cerebrospinal fluid re-examination revealed a CSF-WBC of 131 × 106/L and a protein level of 3141 mg/L. Despite a decrease in CSF-WBC following linezolid treatment, recurrent fluctuations in blood inflammatory markers and an insignificant reduction in cerebrospinal fluid protein were observed, along with a rapid decline in PLT count.
Given the child’s improvement during previous vancomycin treatment and previous literature indicating that vancomycin had a gene phenotype of low-level resistance to EG, linezolid was discontinued for infection control. Treatment was adjusted to meropenem (0.09 g, 40 mg/kg) and vancomycin (0.02 g, 10 mg/kg) administered intravenously every 8 h, with the goal of maintaining vancomycin blood concentrations between 10 and 15 µg/mL. On the 19th day after admission, blood tests revealed a WBC of 8.44 × 109/L, an NE% of 33.7%, and a PLT of 115 × 109/L, with a CRP level of 19 mg/L, indicating a recovery in PLT count. On the 21st day after admission, the vancomycin blood concentration was 10 µg/mL. CSF examination revealed a CSF-WBC of 74 × 106/L, a protein level of 2566 mg/L, and a glucose level of 1.38 mmol/L. Subsequent cultures from cerebrospinal fluid and blood showed no bacterial growth, confirming treatment efficacy. The treatment lasted for eight weeks until the patient’s inflammation indices returned to normal. At discharge, blood tests revealed a WBC of 7.96 × 109/L, an NE% of 18.7%, a PLT of 579 × 109/L, and a CRP level of 19 mg/L. Cerebrospinal fluid examination revealed a CSF-WBC of 14 × 106/L and a protein level of 1365 mg/L. During the course of medication, the patient experienced mild, tolerable gastrointestinal reactions without severe adverse effects. Multiple head ultrasound and MRI scans during the hospital stays indicated good brain development. The patient displayed excellent development in subsequent follow-ups with no residual neurological symptoms.
Discussion and conclusions
EG infections are typically observed in immunocompromised individuals and post-trauma surgical patients [3]. In this particular case, the patient was a premature infant born at 30 weeks gestation. EG infection was confirmed through blood and cerebrospinal fluid cultures upon admission to the local hospital. Sensitivity testing indicated the susceptibility of EG to linezolid. For such cases, the recommended pediatric dosage for linezolid is 10 mg/kg every 8 h for children aged 12 years or younger. Common adverse effects include diarrhea and decreased PLT count [4]. After three days of linezolid treatment, blood tests revealed a PLT count of 55 × 109/L. Furthermore, the absence of routine monitoring of linezolid blood concentrations has hindered tailored dosage adjustment for patients, potentially contributing to this adverse reaction [5, 6]. Thus, linezolid therapy was discontinued.
EG is naturally resistant to vancomycin. Enterococcus strains can be classified into VanA, VanB, and VanC phenotypes based on glycopeptide resistance. EG strains carrying the VanC gene typically exhibit low-level inherent resistance to vancomycin, displaying either in vitro sensitivity or low-level resistance [1, 7]. The low resistance of EG to vancomycin might explain its mode of action.
After the initial treatment, adjusting the frequency of vancomycin to q12h due to higher blood concentrations resulted in decreased therapeutic effectiveness. A randomized study showed that a dosage of 15 mg/kg q12h in premature infants was insufficient for adequate plasma exposure, while 12 mg/kg q8h improved both efficacy and safety [8]. Newborns under 29 weeks and those between 29 and 35 weeks of gestation required higher final doses to achieve therapeutic levels, necessitating approximately 2x and 1.5x the empirical dosing, respectively [9]. The change in vancomycin frequency from q8h to q12h early in treatment led to slight improvements in cerebrospinal fluid protein levels. However, the compromised antimicrobial effect may be attributed to lower blood concentrations and reduced dosing frequency. For neonatal and pediatric patients, vancomycin concentrations between 5 and 15 mg/L are recommended [10]. However, there are substantial interindividual differences in the vancomycin dosages required to achieve therapeutic concentrations in critically ill children. Many dosing regimens fail to meet these targets, highlighting the need for optimized dosing to prevent inadequate treatment. A concentration range of 10–20 mg/L is considered effective and safe [11]. Therefore, in neonatal treatment, the dosage and frequency of vancomycin administration must be carefully adjusted according to the patient’s specific conditions to ensure both therapeutic efficacy and safety.
Although vancomycin is not the first-line treatment for EG infections, different genetic phenotypes of EG can exhibit varying sensitivities to vancomycin in clinical scenarios. In our case, vancomycin trough concentrations in premature infants were continuously monitored and maintained within an effective range of 10–15 µg/mL, successfully treating EG meningitis.
A retrospective analysis highlighted the efficacy of vancomycin in treating EG infections, with sensitivity potentially influenced by specific genetic phenotypes of the bacterium. Monitoring vancomycin blood levels proved crucial for ensuring treatment effectiveness. Attention was also given to the impact of linezolid on PLT counts in premature infants. Future expectations include more clinical data to assist NICU physicians in selecting optimal antimicrobial strategies against EG, minimizing adverse reactions, and improving clinical cure rates.
This case demonstrates the importance of personalized treatment and emphasizes the necessity for flexible treatment regimen adjustment based on the individual responses and clinical needs of pediatric patients, especially in the absence of direct evidence.
Data availability
Data related to the case are presented in this article.
Abbreviations
- EG:
-
Enterococcus gallinarum
- NICUs:
-
Neonatal Intensive Care Units
- NICU:
-
Neonatal Intensive Care Unit
- PLT:
-
Platelet
- CRP:
-
C-reactive protein
- PCT:
-
Procalcitonin
- CSF:
-
Cerebrospinal fluid
- WBC:
-
White blood cell count
- NE%:
-
Neutrophil percentage
- MIC:
-
Minimum inhibitory concentration
- BEA:
-
Bile esculin agar
- MRI:
-
Magnetic Resonance Imaging
References
Prakash VP, Rao SR, Parija SC. Emergence of unusual species of enterococci causing infections, South India. BMC Infect Dis. 2005;5:14. https://doi.org/10.1186/1471-2334-5-14.
Li X, Fan S, Lin X, et al. The first case report of Enterococcus gallinarum meningitis in neonate: a literature review. Med (Baltim). 2018;97(7):e9875. https://doi.org/10.1097/MD.0000000000009875.
Monticelli J, Knezevich A, Luzzati R, Di Bella S. Clinical management of nonfaecium nonfaecalis Vancomycin-resistant enterococci infection. Focus on Enterococcus gallinarum and Enterococcus casseliflavus/flavescens. J Infect Chemother. 2018;24(4):237–46. https://doi.org/10.1016/j.jiac.2018.01.001.
Chiappini E, Conti C, Galli L, de Martino M. Clinical efficacy and tolerability of linezolid in pediatric patients: a systematic review. Clin Ther. 2010;32(1):66–88. https://doi.org/10.1016/j.clinthera.2010.01.019.
Rao GG, Konicki R, Cattaneo D, et al. Therapeutic drug monitoring can improve Linezolid Dosing regimens in current clinical practice: a review of Linezolid Pharmacokinetics and Pharmacodynamics. Ther Drug Monit. 2020;42(1):83–92. https://doi.org/10.1097/FTD.0000000000000710.
Ogami C, Tsuji Y, To H, Yamamoto Y. Pharmacokinetics, toxicity and clinical efficacy of linezolid in Japanese pediatric patients. J Infect Chemother. 2019;25(12):979–86. https://doi.org/10.1016/j.jiac.2019.05.025.
Leclercq R, Dutka-Malen S, Duval J, Courvalin P. Vancomycin resistance gene vanC is specific to Enterococcus gallinarum. Antimicrob Agents Chemother. 1992;36(9):2005–8. https://doi.org/10.1128/AAC.36.9.2005.
Mulubwa M, Griesel HA, Mugabo P, Dippenaar R, van Wyk L. Assessment of Vancomycin Pharmacokinetics and Dose Regimen optimization in Preterm neonates. Drugs R D. 2020;20(2):105–13. https://doi.org/10.1007/s40268-020-00302-7.
Sosnin N, Curtis N, Cranswick N, Chiletti R, Gwee A. Vancomycin is commonly underdosed in critically ill children and neonates. Br J Clin Pharmacol. 2019;85(11):2591–8. https://doi.org/10.1111/bcp.14084.
He N, Su S, Ye Z, et al. Evidence-based Guideline for Therapeutic Drug Monitoring of Vancomycin: 2020 update by the Division of Therapeutic Drug Monitoring, Chinese Pharmacological Society. Clin Infect Dis. 2020;71(Suppl 4):S363–71. https://doi.org/10.1093/cid/ciaa1536.
Dao K, Guidi M, André P, et al. Optimization of Vancomycin exposure in neonates based on the best level of evidence. Pharmacol Res. 2020;154:104278. https://doi.org/10.1016/j.phrs.2019.104278.
Acknowledgements
Thanks for the help from various departments during my clinical pharmacist training in Chengdu Women’s and Children’s Central Hospital.
Funding
None.
Author information
Authors and Affiliations
Contributions
LH drafted the initial manuscript, and reviewed and revised the manuscript. HW reviewed and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
As this is a case report, ethics approval is not reruired as per our institution’s policy.
Consent for publication
Written informed consent was obtained from the baby’s parents to publish the clinical details.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hao, L., Wang, H. Successful treatment of Enterococcus gallinarum infection in a neonate with vancomycin: a case report. BMC Pediatr 24, 527 (2024). https://doi.org/10.1186/s12887-024-05004-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-024-05004-6