Abstract
Background
Necrotizing enterocolitis (NEC) is a multifactorial gastrointestinal disease with high morbidity and mortality among premature infants. However, studies with large samples on the factors of NEC in China have not been reported. This meta-analysis aims to systematically review the literature to explore the influencing factors of necrotizing enterocolitis in premature infants in China and provide a reference for the prevention of NEC.
Methods
PubMed, Embase, Web of Science, Cochrane Library, China National Knowledge Infrastructure (CNKI), China Biomedical Literature Database (CBM), Wanfang and VIP databases were systematically searched from inception to February 2023. We used Stata14.0 software to perform the systematic review and meta-analysis. We used fixed or random effects models with combined odds ratios (ORs) and 95% confidence intervals (CIs), and quality was evaluated using the Newcastle‒Ottawa Scale (NOS).
Results
The total sample was 8616 cases, including 2456 cases in the intervention group and 6160 cases in the control group. It was found that 16 risk factors and 3 protective factors were related to necrotizing enterocolitis in premature infants. Septicemia (OR = 3.91), blood transfusion (OR = 2.41), neonatal asphyxia (OR = 2.46), pneumonia (OR = 6.17), infection (OR = 5.99), congenital heart disease (OR = 4.80), intrahepatic cholestasis of pregnancy (ICP) (OR = 2.71), mechanical ventilation (OR = 1.44), gestational diabetes mellitus (GDM) (OR = 3.08), respiratory distress syndrome (RDS) (OR = 3.28), hypoalbuminemia (OR = 2.80), patent ductus arteriosus (PDA) (OR = 3.10), respiratory failure (OR = 7.51), severe anemia (OR = 2.86), history of antibiotic use (OR = 2.12), and meconium-stained amniotic fluid (MSAF) (OR = 3.14) were risk factors for NEC in preterm infants in China. Breastfeeding (OR = 0.31), oral probiotics (OR = 0.36), and prenatal use of glucocorticoids (OR = 0.38) were protective factors for NEC in preterm infants.
Conclusions
Septicemia, blood transfusion, neonatal asphyxia, pneumonia, infection, congenital heart disease, ICP, GDM, RDS, hypoproteinemia, PDA, respiratory failure, severe anemia, history of antibiotic use and MSAF will increase the risk of NEC in premature infants, whereas breastfeeding, oral probiotics and prenatal use of glucocorticoids reduce the risk. Due to the quantity and quality of the included literature, the above findings need to be further validated by more high-quality studies.
Similar content being viewed by others
Introduction
Necrotizing enterocolitis (NEC) is one of the most common gastrointestinal diseases in neonates [1]. The onset of NEC is not clinically specific, and the disease progresses rapidly and can be complicated by intestinal perforation and necrosis, causing death in severe cases [2]. Surviving children may experience severe sequelae, including intestinal stricture, short bowel syndrome, dependence on total parenteral nutrition, and neurodevelopmental disorders, leading to both growth and mental retardation. These conditions significantly impact the quality of life in later years [3, 4]. Over the past few years, China has made great progress in perinatal and neonatal intensive care, the survival rate has increased, and the number of premature infants has increased sharply, especially very low birth weight (VLBW) or extremely premature infants at high risk of NEC, which reflects the importance of studying the epidemiology of contemporary NEC [5, 6]. In China, the incidence of NEC was found to be 5.5% and 7.0% for infants with birth weights < 1500 g and < 1000 g, respectively, and 4.8% and 7.6% for infants born at < 32 weeks and < 28 weeks, respectively [7]. Therefore, NEC remains a fulminant disease, necessitating improved prevention, early diagnosis, and more rational management.
NEC results from a combination of factors with complex pathophysiology and unclear mechanisms, and individual risk factors remain to be elucidated [8]. Identifying the clinical features that can predict NEC from the many influencing factors is the focus of prevention. Both maternal and neonatal factors may be risk factors for the development of NEC. It has been found that early identification of NEC risk factors, targeted interventions, and timely diagnosis and treatment are extremely important to reduce the morbidity and mortality of NEC [9]. Currently, relevant studies on the influencing factors of NEC in Chinese preterm infants have been reported [10,11,12]. However, the influence of the sample size and the completeness of the children’s data has led to considerable variability in the results of these studies. As a result, the specific risk factors and protective factors related to NEC remain unclear. Although overseas studies on factors affecting NEC in preterm infants have been conducted for a long time [13, 14], differences in medical practices, geographic environments, and demographics between regions may limit the blind generalization of known findings to all areas.
Although meta-analyses of risk factors for neonatal NEC have been reported [15,16,17], opinions differ on the importance of NEC risk factors. The opinion of a panel of 35 international NEC experts pointed to the ambiguity of risk factors affecting NEC except for gestational age (GA), birth weight (BW) and feeding [18]. Studies are limited by differences in population characteristics and different definitions of NEC, leading to some variability in findings. This suggests that there are modifiable risk factors that give healthcare professionals the opportunity to intervene to reduce the risk of NEC. Considering that there is no meta-analysis for the factors affecting NEC in Chinese preterm infants, this study used systematic evaluation and meta-analysis by searching the latest literature to explore the major risk factors and protective factors affecting the occurrence of NEC in preterm infants in China, and to provide a scientific basis for the development of preventive measures for NEC.
Materials and methods
Search strategy
The present systematic review and meta-analysis followed the preferred reporting items in the systematic review and meta-analysis (PRISMA) guidelines [19]. The PRISMA checklist is presented in S Table 1. The databases of China National Knowledge Infrastructure (CNKI), VIP (Chinese) and WanFang (Chinese) database, China Biomedical Literature Database (CBM), Web of Science, Embase, and PubMed were searched for case‒control studies and cohort studies from creation to February 2023. We searched the databases using a combination of subject terms and free words, while references of included studies were hand-searched to supplement the relevant information obtained. The keywords included (“premature infant” OR “preterm infants “OR” Neonatal Prematurity” OR “very preterm infant” OR” extremely preterm infants” OR “Very low birth weight”) AND (“necrotizing enterocolitis”) AND (“risk factor” OR “influence factors”) AND (“ case‒control studies” OR “cohort study”) AND (“Chinese” OR “China”). Detailed information on the search terms and search strategies is shown in S Table 2.
Inclusion and exclusion criteria
Inclusion criteria: (1) Study participants: Chinese preterm infants with NEC, GA < 37 weeks, weight < 2500 g; (2) Clear diagnosis of NEC, defined as stage II and above according to the Bell criteria, with gastrointestinal dysfunction clearly demonstrated by clinical symptoms and imaging assessment [20] (3). Study type: case-control or cohort study. The intervention group in the case-control study was preterm infants with confirmed NEC, and the control group was preterm infants without NEC; the exposure group in the cohort study was preterm infants exposed to risk factors associated with NEC, and the control group was preterm infants not exposed to these risk factors (4). Study outcome: Risk factors and protective factors affecting NEC in preterm infants (5). Study language: Published in English or Chinese (6). Study date: Each database from the establishment to February 2023.
Exclusion criteria: (1) conference abstracts, case reports, review categories, and literature without control groups; (2) literature with incomplete original study data and an inability to extract data; (3) Studies with duplicate publication.
Data extraction and quality assessment
Three researchers independently extracted data according to the developed data collection form, and in case of discrepancies, the three discussed and approved. Data extracted included author, publication year, study area, study time, study type, study population, NEC diagnostic criteria, number of cases/control groups, influencing factors and Newcastle‒Ottawa Scale (NOS) score. Two researchers independently performed quality assessment using the NOS recommended by the Cochrane Collaboration Network [21]. In the event of disagreements, group discussions were held to reach a consensus. This scale includes 3 modules of study population, comparability between groups, and outcome evaluation and is divided into 8 entries with a score out of 9. NOS score ≥ 6 is considered high-quality literature. We assessed the methodological quality of our systematic reviews using the A Measurement Tool to Assess Systematic Reviews 2 (AMSTAR2) [22]. The details of the items in the AMSTAR-2 tool are shown in S Table 3.
Data synthesis and statistical analysis
We used Stata 14.0 software to perform statistical analysis of the extracted data. Heterogeneity among the studies was analyzed using the χ2 test (test level α = 0.1), and the Q test was combined with the I2 statistic to determine heterogeneity. When I2 ≥ 50%, it indicated high heterogeneity among the study results, and a random-effects model was used. Otherwise, the fixed effects model was used. To assess the stability of the combined results for statistically significant risk factors, we conducted sensitivity analysis by comparing the values obtained from both the fixed-effects model and the random-effects model. Funnel plots were used to assess publication bias, and Egger’s statistical test was used to analyze whether publication bias was statistically significant. Differences were considered statistically significant at P < 0.05.
Results
Study selection
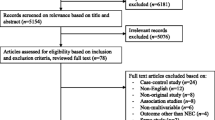
The initial search yielded 2490 articles, and 1152 duplicates were removed after screening by Endnote software; 1180 articles were removed after reading the title and abstract; 158 articles were retained for the full text screening, and 38 eligible articles [10,11,12, 23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57] were finally included. No additional eligible studies were identified through a manual search. The study selection flow chart is shown in Fig. 1.
Study characteristics and qualit y
Thirty-eight studies (36 case‒control studies [10,11,12, 23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54, 57] and 2 cohort studies [55, 56]) were included, containing a total sample size of 8616 cases, with 2456 cases in the intervention group and 6160 cases in the control group, from 16 different provinces in China. The study population consisted of preterm infants with BW less than 2500 g, GA less than 37 weeks, and Bell staging ≥ II. Diagnostic criteria for NEC vary. Twenty-one studies utilized the revised Bell Subdivision periodical standard of Practical Neonatology, 4th edition, for the diagnosis of NEC in preterm infants [58]. Two studies referred to the revised Bell Subdivision periodical standard of Practical Neonatology, 5th edition [59]. Eight studies used the modified BELL-NEC grading scale [20]. Two studies used the revised Bell Subdivision periodical standard [60]. Three studies referred to Avery’s Diseases of the Newborn as the revised Bell marking criteria [61]. One study adopted to the Vermont Oxford Network’s revised diagnostic criteria based on Bell staging [62]. One study referred to the U.S. Guidelines for the Management of Necrotizing Small Bowel Colitis in Very Low Birth Mass Children [63]. The detailed characteristics are shown in Table 1. Nine studies received a NOS quality assessment score of 6, 15 studies scored 7, 9 studies scored 8, and 5 studies scored 9. The overall quality of the studies was above the average (S Table 4).
Meta-analysis results
The heterogeneity analysis for factors influencing NEC in preterm infants revealed that septicemia, blood transfusion, neonatal asphyxia, pneumonia, infection occurrence, intrahepatic cholestasis of pregnancy (ICP), mechanical ventilation, gestational diabetes mellitus (GDM), respiratory distress syndrome (RDS), prenatal application of glucocorticoids, hypoproteinemia, ductus arteriosus, severe anemia, and meconium-stained amniotic fluid (MSAF) exhibited low heterogeneity (I2 < 50%) when analyzed using a fixed-effects model with combined effect sizes. On the other hand, oral probiotics, breastfeeding, congenital heart disease, respiratory failure, and history of antibiotic use had high heterogeneity (I2 ≥ 50%) and were analyzed using a random-effects model. The meta-analysis indicated that intravenous immunoglobulin was not statistically significant with NEC in premature infants (P > 0.05), while all other influencing factors were statistically significant. We divided the factors that affect preterm infants with NEC into two main categories: protective factors and risk factors. Further details are provided in Table 2.
Protective factors
This study showed that breastfeeding [OR = 0.31, 95% CI (0.16, 0.62), P < 0.001], oral probiotics [OR = 0.36, 95% CI (0.25, 0.53), P < 0.001] and prenatal application of glucocorticoids [OR = 0.38, 95% CI (0.24, 0.60), P < 0.001] were protective factors for NEC in preterm infants.
Risk factors
Septicemia [OR = 3.91, 95% CI (3.37,4.55), P < 0.001], blood transfusion [OR = 2.41, 95% CI (1.97, 2.95), P < 0.001], severe anemia [OR = 2.86, 95% CI (2.06, 3.99), P < 0.001], neonatal asphyxia [OR = 2.46, 95% CI (2.07, 2.93), P < 0.001], pneumonia [OR = 6.17, 95% CI (3.98, 9.57), P < 0.001], mechanical ventilation [OR = 1.44, 95% CI (1.22, 1.71), P < 0.001], RDS [OR = 3.28, 95% CI (2.23,4.85), P < 0.001], congenital heart disease [OR = 4.80 95% CI (3.00, 7.68), P < 0.001], hypoproteinemia [OR = 2.80, 95% CI (1.78, 4.41), P < 0.001], PDA [OR = 3.10, 95% CI (1.93, 4.98), P < 0.001], history of antibiotic use [OR = 2.12, 95% CI (1.18,3.81), P = 0.01], infection occurs [OR = 5.99, 95% CI (2.57, 13.93), P < 0.001], ICP [OR = 2.71, 95% CI (1.92, 3.82), P < 0.001], GDM [OR = 3.08, 95% CI (1.73, 5.48), P < 0.001], respiratory failure [OR = 7.51, 95% CI(1.60, 35.10), P = 0.01], MSAF [OR = 3.14, 95% CI (1.64, 6.01), P < 0.001] were risk factors for NEC in preterm infants.
Due to the multitude of influential factors considered, forest plots for septicemia and oral probiotics are presented in this paper (Figs. 2 and 3). Forest plots of other influencing factors are provided in S Figs. 1–18.
Sensitivity analysis and publication bias
Sensitivity analyses were performed by eliminating each study individually, and the remaining articles were recombined for meta-analysis. Sensitivity analyses revealed that the heterogeneity for studies with high heterogeneity, including oral probiotics, breastfeeding, respiratory failure, and history of antibiotic use, remained consistent after removing any individual study, suggesting that the results of the meta-analysis were relatively stable. The study by Tan et al. [56] had a large impact on the outcome of preterm heart disease and was the main source of heterogeneity. Upon excluding this study and reanalyzing the results, a substantial reduction in heterogeneity was observed for the prevalence of heart disease (OR = 4.80, I2 = 1%). For the influencing factors with a statistically significant heterogeneity, both fixed-effects and random-effects were used to combine the effect sizes. The results demonstrated a high degree of consistency between the calculations of the two models, affirming the reliability of this study outcomes.
Sepsis, blood transfusion, oral probiotics, and breastfeeding, which are the influencing factors involved in ≥ 10 publications, were separately funnel plotted. The results indicated asymmetry in the funnel plots (S Figs. 19-22). Egger’s and Begg’s test revealed publication bias (P < 0.05) for blood transfusion, oral probiotics, ICP, and mechanical ventilation (Table 3). Therefore, caution should be taken about the accuracy of the results.
Discussion
To our knowledge, this is the first meta-analysis of factors influencing NEC in preterm infants in China to obtain an updated and thorough quantitative analysis. NEC has a rapid onset and progression of disease, with a high morbidity and mortality rate, and is one of the most important factors contributing to preterm infant mortality [64]. Exploring the protective and risk factors for NEC in preterm infants is important for prevention and developing effective interventions to reduce its incidence.
Risk factors for NEC
This meta-analysis showed that MSAF, history of antibiotic use and preterm infection were risk factors for NEC in preterm infants. Chen et al. [45, 54, 63] also found that MSAF was an independent risk factor for NEC in preterm infants. The inhalation of amniotic fluid contaminated with meconium in utero in preterm infants can lead to the multiplication of intestinal pathogens and early infection [65]. In addition, due to the underdevelopment of the gastrointestinal tract, the imperfect barrier function of the intestinal mucosa, and the high permeability of the intestinal wall in preterm infants, bacteria can easily enter the intestinal tract and cause infections. The application of antibiotics affects the distribution of intestinal flora, leading to an increase in bacteria with potential therapeutic effects and a decrease in normal flora, which can damage the intestinal mucosal epithelium and lead to NEC [66]. The use of empirical antibiotics and the duration of antibiotic exposure in infants are associated with an increased risk of NEC [67]. In a meta-analysis of observational studies and randomized controlled trials, prophylactic antibiotic use in infants was not found to be statistically associated with NEC, but with an increased risk [68]. These factors influencing NEC are independent of each other while also influencing and interacting with one other. We also found sepsis to be a risk factor for NEC in preterm infants, consistent with the findings of Gagliardi et al. [69]. Comparing domestic and international studies on sepsis and NEC, we found that the OR values of sepsis for NEC reported abroad were mostly above 10 [70], while the OR values reported in China were mostly 3 to 5 [71], and the OR value of our study was 3.91. The fact that there are such obvious differences in such a strong risk factor as sepsis suggests that we should be cautious in interpreting the results of epidemiologic studies and medical statistics.
There is controversy surrounding whether blood transfusion in preterm infants contributes to an increased incidence of NEC. The present meta-analysis showed that blood transfusion is a risk factor for complications of NEC in preterm infants, while a recent meta-analysis showed that red blood cell (RBC) transfusion does not increase the risk of NEC [72]. Blood transfusions, especially large amounts of RBC, can cause impaired regulation of the mesenteric vessels, leading to increased adhesion and aggregation of RBC and formation of thrombi, resulting in poor blood flow to the intestine [73]. Whereas, a meta-analysis conducted by Rai et al. [74] demonstrated that erythrocyte infusion within 48 h exerted a protective effect on infants with NEC. Erythropoietin may have a protective effect on the endothelial cell barrier and therefore may attenuate the development of NEC. This study also found that severe anemia in preterm infants was associated with an increased risk of developing NEC [75]. Analysis of the reasons for this may be related to the fact that anemia decreases the expression of the tight junction protein ZO-1, increases the permeability of the intestinal barrier, increases intestinal inflammation by altering the function of macrophages, and predisposes patients to NEC. Patel et al. [75] reported that severe anemia, rather than RBC transfusion, was associated with an elevated risk of NEC and suggested that prevention of anemia may be more beneficial than minimizing RBC transfusions.
In this study, RDS, respiratory failure, neonatal asphyxia, and mechanical ventilation were all risk factors for NEC in preterm infants. Preterm combined VLBW infants are highly susceptible to asphyxia after birth due to their underdeveloped respiratory and neurological systems and their inability to perform effective gas exchange on their own. Infant asphyxia can induce the body’s defense reflex and redistribute the blood flow in the body to ensure the oxygen supply to the heart, brain, kidneys and other important organs, triggering strong constriction of mesenteric vessels, leading to ischemia and hypoxia of intestinal epithelial cells and even degeneration and necrosis, resulting in NEC [76]. Neonates with severe asphyxia often require mechanical ventilation, which was shown to be an independent risk factor for NEC in this study, and this is in agreement with the finding by Gagliardi et al. [69]. However, in a Canadian study, mechanical ventilation was shown to be a risk factor for NEC only in sicker infants [77].
This meta-analysis confirms that PDA, congenital heart disease, hypoproteinemia, and pneumonia are all risk factors for NEC in preterm infants. Preterm birth in combination with PDA and congenital heart disease causes inadequate intestinal blood flow, which induces immune responses, inflammatory mediators, and consequently intestinal mucosal injury and necrosis, leading to NEC [78]. At present, it is difficult to determine whether the presence of PDA or treatment with PDA alters the risk of NEC in infants. In a cohort of infants with PDA aged < 34 weeks, infants with PDA who were not treated with indomethacin had an increased risk of NEC compared with those who were treated [79]. However, in a recent meta-analysis of randomized controlled trials [80], it was found that there was no increased risk of NEC in the absence of PDA treatment.
In this study, maternal ICP and GDM were also found to be risk factors for NEC in preterm infants, which is consistent with the meta-analysis of Lu et al. [16]. Beghetti et al. [81] concluded that high concentrations of bile acids lead to enhanced contraction of placental villi veins exposed to amniotic fluid, reduced blood supply, and impaired intestinal microcirculation, resulting in intestinal mucosal ischemia and hypoxia and the production of multiple free radicals, forming the pathological basis for NEC. In GDM patients, the body is in a hyperglycemic state, and the fetus receives nutrients directly from the mother, which can affect the state of intestinal blood flow, lead to intestinal mucosal damage and induce NEC [30]. In this study, the pooled OR of ICP for NEC was 2.71 with four studies included; the pooled OR for GDM and NEC was 3.08 with only two included studies. Currently, there are fewer studies exploring the relationship between NEC and ICP, GDM, thus caution needs to be taken when making conclusion for the impact of GDM, ICP on NEC based on the observation in this study.
Protect factors for NEC
The safety of oral probiotics in preterm infants is currently controversial, and it is believed that the optimal strain, optimal dose and duration of probiotics for the prevention of NEC have not been determined [82]. Our study found that probiotics reduced the risk of NEC, which is consistent with previously published meta-analysis [83]. Prophylactic supplementation with probiotics increases the deposition and growth of normal flora, enhances the barrier function of the intestinal mucosa, prevents the migration of bacteria or curative factors, and activates protective receptors to balance the intestinal flora [84]. The 2020 European Society of Pediatric Gastroenterology and Hepatology and Nutrition recommends that probiotics such as Bifidobacterium bifidum, when safe to do so, can be given to preterm infants to reduce the risk of NEC in preterm infants [85]. A multicenter randomized controlled study found that early administration of Bifidobacterium bifidum (BBG-001) did not reduce the risk of NEC in preterm infants [86]. The use of probiotics for the prevention of NEC in preterm infants is controversial and further studies are needed to demonstrate the effect.
In this meta-analysis, prenatal application of glucocorticoids was a protective factor for NEC in preterm infants, which is consistent with the results of a previous meta-analysis [17]. A Cochrane systematic evaluation documented that antenatal glucocorticoid use in women at risk of preterm labor reduced the incidence of RDS in preterm infants and also reduced the risk of NEC [87]. It was found that the proinflammatory factors interleukin-1β and interleukin-8 play an important role in the pathogenesis of NEC, and glucocorticoids significantly inhibit the proinflammatory effects of both and promote the maturation of the gastrointestinal tract while reducing the absorption of macromolecules by the intestinal mucosa and avoiding intestinal necrosis [88]. The clinical guidelines for the management of neonatal necrotizing small bowel colitis, published in China in 2020, recommend that glucocorticoids should be applied prenatally in mothers at risk of preterm delivery [89].
Breastfeeding has been shown to reduce the risk of NEC. In this study, breastfeeding was a protective factor for NEC in preterm infants, and a review by Nolan et al. [90] indicated that immune components in breast milk have a protective effect against NEC. A prospective study found that breastfeeding reduced the risk of NEC in preterm infants compared with formula feeding [91]. Breast milk, with its lower osmolality compared to formula, alleviates the osmotic load of food, relieving intestinal pressure. In addition, breast milk is rich in secretory IgA, lactoferrin and other antimicrobial active substances, which enhance the body’s immune defense and effectively prevent the occurrence of infectious diseases of the gastrointestinal tract [92].
Limitations
Our study had several limitations. First, we only included published literature, and potential publication bias should not be ignored. Second, the quality of the included articles was limited and the heterogeneity among studies was high, and we need to be cautious in interpreting the findings. We only included NEC premature infants hospitalized in neonatal intensive care units (NICUs) in China, and there was some bias in the selection of the study population and region, which may limit the generalizability of the findings. In addition, this study also found that cesarean section and the use of pulmonary surfactant are protective factors against NEC in premature infants, but due to the limited number of included studies, meta-analysis was not performed on these factors. Although this study only analyzed the factors influencing NEC in Chinese preterm infants, it may provide a valuable foundation for future research and interventions to enhance infants’ health related to NEC.
Conclusion
In summary, our study suggests that septicemia, blood transfusion, neonatal asphyxia, pneumonia, infection, congenital heart disease, ICP, GDM, RDS, hypoproteinemia, PDA, respiratory failure, severe anemia, antibiotic use history and MSAF are risk factors for NEC in premature infants in China. Breastfeeding, oral probiotics and prenatal use of glucocorticoids are protective factors. This is the first meta-analysis of the factors influencing NEC in preterm infants in China, further expanding our knowledge in this subject area.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ANS:
-
Antenatal steroid
- CI:
-
Confidence interval
- CNKI:
-
China National Knowledge Infrastructure
- CBM:
-
China Biomedical Literature Database
- IVIG:
-
Intravenous Immunoglobulin
- ICP:
-
Intrahepatic cholestasis of pregnancy
- MSAF:
-
Meconium-stained amniotic fluid
- NEC:
-
Necrotizing enterocolitis
- NOS:
-
Newcastle-Ottawa Scale
- NICU:
-
Neonatal intensive care unit
- OR:
-
Odds ratio
- PDA:
-
Patent ductus arteriosus
- RDS:
-
Respiratory distress syndrome
- GDM:
-
Gestational diabetes mellitus
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- AMSTAR2:
-
A Measurement Tool to Assess Systematic Reviews 2
- VLBW:
-
Very low birth weight
- WHO:
-
World health organization
- GA:
-
Gestational age
- BW:
-
Birth weight
References
Neu J, Walker W. Medical progress: necrotizing enterocolitis. N Engl J Med. 2011;364:255–64.
Hull MA, Fisher JG, Gutierrez IM, Jones BA, Kang KH, Kenny M, et al. Mortality and management of surgical necrotizing enterocolitis in very low birth weight neonates: a prospective cohort study. J Am Coll Surg. 2014;218(6):1148–55.
Miller RJ, Sullivan MC, Hawes K, Marks AK. The effects of perinatal morbidity and environmental factors on health status of preterm children at age 12. J Pediatr Nurs. 2009;24(2):101–14.
Fitzgibbons SC, Ching Y, Yu D, Carpenter J, Kenny M, Weldon C, et al. Mortality of necrotizing enterocolitis expressed by birth weight categories. J Pediatr Surg. 2009;44(6):1072–5. discussion 1075–1076.
Kong X, Xu F, Wu R, Wu H, Ju R, Zhao X, Tong X, Lv H, Ding Y, Liu F, et al. Neonatal mortality and morbidity among infants between 24 to 31 complete weeks: a multicenter survey in China from 2013 to 2014. BMC Pediatr. 2016;16(1):174.
Jiang S, Yan W, Li S, Zhang L, Zhang Y, Shah PS, Shah V, Lee SK, Yang Y, Cao Y. Mortality and morbidity in infants < 34 weeks’ Gestation in 25 NICUs in China: a prospective cohort study. Front Pediatr. 2020;8:33.
Cao X, Zhang L, Jiang S, Li M, Yan C, Shen C, Yang Y, Lee SK, Cao Y. Epidemiology of necrotizing enterocolitis in preterm infants in China: a multicenter cohort study from 2015 to 2018. J Pediatr Surg. 2022;57(3):382–6.
Jones IH, Hall NJ. Contemporary Outcomes for Infants with necrotizing Enterocolitis-A systematic review. J Pediatr. 2020;220:86–92e83.
Ellsbury DL, Clark RH, Ursprung R, Handler DL, Dodd ED, Spitzer AR. A Multifaceted Approach to improving outcomes in the NICU: the Pediatrix 100 000 babies campaign. Pediatrics. 2016;137(4):e20150389.
Dong HM, Song J, Wang Y, Zhang XL, Jue ZZ, Wei LL. Clinical characteristics and risk factors for necrotizing small intestinal colitis in extremely premature infants. Chin J Child Health Care. 2021;29(09):1012–6.
Liu X, Liu LJ, Jiang HY, Zhao CL, He HY. Establishment of a line graph model for predicting the risk of necrotizing small bowel colitis in very preterm infants. Chin J Contemp Pediatr. 2022;24(07):778–85.
Yu ZY, Xu SJ, Sun HQ, Li MC, Xing S, Cheng P, et al. Clinical characteristics and risk factors of premature necrotizing small bowel colitis in extremely/ultra-low birth weight preterm infants. Chin J Contemp Pediatr. 2023;25(02):147–52.
Campos-Martinez AM, Expósito-Herrera J, Gonzalez-Bolívar M, Fernández-Marin E, Uberos J. Evaluation of risk and preventive factors for necrotizing enterocolitis in premature newborns. A systematic review of the literature. Front Pediatr. 2022;10:874976.
Rose AT, Patel RM. A critical analysis of risk factors for necrotizing enterocolitis. Semin Fetal Neonatal Med. 2018;23(6):374–9.
Chen D, Huang XL, Li X. Meta-analysis of risk factors for necrotizing small bowel colitis in newborns. Chin J Clin Phys (Electronic Edition). 2010;4(05):563–7.
Lu CY, Liu KF, Qiao GX, Luo Y, Cheng HQ, Du SZ. Meta-analysis of risk factors for necrotizing small bowel colitis in preterm infants. Chin J Contemp Pediatr. 2022;24(08):908–16.
Su Y, Xu RH, Guo LY, Chen XQ, Han WX, Ma JJ, et al. Risk factors for necrotizing enterocolitis in neonates: a meta-analysis. Front Pediatr. 2022;10:1079894.
Gephart SM, Effken JA, McGrath JM, Reed PG. Expert consensus building using e-Delphi for necrotizing enterocolitis risk assessment. Journal of obstetric, gynecologic, and neonatal nursing. JOGNN. 2013;42(3):332–47.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (Clinical Res ed). 2021;372:n71.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, Brotherton T. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978;187(1):1–7.
Wells G, Shea B, O’Connell J. The Newcastle-Ottawa Scale (NOS) for assessing the quality of Nonrandomised studies in Meta-analyses. Ottawa Health Research Institute Web site; 2014. p. 7.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ (Clinical Res ed. 2017;358:j4008.
Cheng SP, Lu Q, Zhou M, Yu JL. A case–control study on risk factors for necrotizing enterocolitis in premature infants with gestational age less than 34 weeks. Chin J Evidence- Based Pediatr. 2016;11(02):122–5.
Zeng SY, Deng C. Analysis of risk factors for necrotizing small bowel colitis in very low birth weight children. J Chongqing Med Univ. 2021;46(03):335–40.
Liu YC. Risk factor analysis of low and very low birth weight neonates with necrotizing small bowel colitis in a hospital from 2012–2018. J Practical Med. 2019;36(11):985–8.
Shang Y, Yang J. Clinical analysis of risk factors for the development of necrotizing small bowel colitis in preterm infants. Jilin Med. 2014;35(31):6920–2.
Sun HX, Gao RR, Zheng JF, Sun LS, Liu W, Wang XJ, Zhong YQ, Zhang LM. Clinical analysis of risk factors for necrotizing small bowel colitis in premature infants. J Weifang Med Univ. 2017;39(01):60–2.
Lu Y, Pan S. Analysis of risk factors for necrotizing small bowel colitis in preterm infants. Chin Mod Phys. 2022;60(02):60–3.
Wang YP, Zheng MY, Xiao YY, Qu YM, Wu H. Analysis of factors influencing necrotizing small intestinal colitis in preterm infants and construction of a predictive model for its development. Chin J Contemp Pediatr. 2022;24(01):41–8.
Li XH. Analysis of clinical characteristics and influencing factors of necrotizing small bowel colitis in preterm infants. China Matern Child Health Care. 2019;34(24):5673–5.
Lu H, Zhou HY, He YB. Analysis of risk factors for necrotizing small bowel colitis in premature neonates. Youjiang Med. 2018;46(01):79–82.
Lu XY, Tan W. Clinical analysis of factors affecting 54 cases of necrotizing small bowel colitis in premature infants. Jiangxi Med. 2013;48(07):610–2.
Lu M, Liu DL, Lu YD, Li YB. A retrospective analysis of factors influencing necrotizing small bowel colitis in preterm infants. Chin Maternal Child Health Care. 2015;30(15):2397–400.
Qu XL, Zhang SE, Fang Y, Wan GB. Analysis of clinical characteristics and risk factors for preterm infants with necrotizing small bowel colitis. China Maternal Child Health Res. 2018;29(08):995–9.
Shi Y. Analysis of factors influencing necrotizing small bowel colitis in preterm infants. Mod Diagnosis Therapy. 2019;30(19):3416–8.
Wang RJ, Kong XY, Cai N, Cheng Y, Feng ZC. A case–control study of perinatal high-risk factors for necrotizing small bowel colitis in preterm infants. Chin J Contemp Pediatr. 2014;16(04):414–7.
Yu M, Xu H, Lu YJ, Zhu ZF, Shi BZ. Analysis of factors influencing necrotizing small bowel colitis and surgical efficacy in low birth mass children. Anhui Med. 2018;22(10):1949–52.
Zhu MY, Gu MZ. Analysis of the incidence and risk factors of necrotizing small bowel colitis in very low birth weight infants. Chin J Neonatology. 2012;27(2):78–81.
Hou AN, Li X, Fu JH. Analysis of high-risk factors in 76 cases of neonatal necrotizing small bowel colitis. Chin J Practical Pediatr. 2017;32(8):611–4.
Song J, Dong H, Xu F, Wang Y, Li W, Jue Z, Wei L, Yue Y, Zhu C. The association of severe anemia, red blood cell transfusion and necrotizing enterocolitis in neonates. PLoS One. 2021;16(7):e0254810.
Zhang LP, Lei XP, Luo LJ, Dong WB. Risk factors for necrotizing enterocolitis in very preterm infants: a case-control study in southwest China. J Maternal Fetal Neonatal Med. 2019;32(6):896–901.
Lu Q, Cheng S, Zhou M, Yu J. Risk factors for necrotizing enterocolitis in neonates: a retrospective case-control study. Pediatr Neonatol. 2017;58(2):165–70.
Zhu K, Li-ping Y, Gao H, Wang X, Wang J, Wang L, Deng F. The role of probiotics prophylaxis duration in preventing necrotizing enterocolitis: a single-center retrospective study. Iran J Pediatr. 2021, In Press.
Huang D, Jiang YJ, Zhang ZY, Li LQ. Risk factors for the development of necrotizing small bowel colitis in children younger than fetal age. J Clin Pediatr. 2022;40:661–5678.
Yang J, Liu E, Yang L. Clinical characterization of necrotizing small bowel colitis in 78 neonates. J Mol Diagn Ther. 2022;14(02):309-311+316.
Yang LR, Li H, Zhang T, Zhao RC. Correlation between vitamin D deficiency and necrotizing small bowel colitis in preterm infants. Chin J Contemp Pediatr. 2018, 20(03):178–83.
Zhuang XY, Li LQ, Gao XX, Su LD. Etiology of necrotizing small bowel colitis in preterm infants and the preventive effect of microecological agents. Clin J Pract Pediatr. 2007(18):1392–3.
Li ZT, Xu N, Li H, Qiao LX, Qian LJ. Characteristics of the pathogens of necrotizing small bowel colitis in preterm infants in Nanjing and the effect of probiotic intervention and prognostic factors. Chin J Microecol. 2020;32(07):789–93.
Ma SJ, Zheng TT. Correlation between maternal risk factors and necrotizing small bowel colitis in preterm infants during preconception and early pregnancy. World J Chin Gastroenterol. 2021;29(10):557–62.
Deng X. Analysis of risk factors for necrotizing small bowel colitis in preterm infants. Chin Comm Phys. 2017;33(29):35–6.
Zhu JL, Zhu XG, Ma LY, Zhou LX, Duan CS. Analysis of factors associated with necrotizing small bowel colitis in neonates and preventive measures. Chin J Prev Med. 2020;21(09):990–4.
Wang XQ, Li ZB, Lian J. A case-control study of risk factors for necrotizing small bowel colitis in preterm infants. Zhongguo Nguo Kang Med. 2017;29(14):65–7.
Wang P P, Huang N N, Wang GZ, Yu FQ. Analysis of high-risk influencing factors and response to necrotizing small bowel colitis in preterm infants. Clin Res. 2020;28(09):23–4.
Zhang L, Xu YL, Li MX. Analysis of risk factors for necrotizing small bowel colitis in preterm very low birth weight infants. China Matern Child Health Care. 2017;32(15):3515–17.
Chen S, Wang XQ, Hu XY, Guo L, He Y, Wang ZL, et al. Meconium-stained amniotic fluid as a risk factor for necrotizing enterocolitis in very low-birth weight preterm infants: a retrospective cohort study. J Matern Fetal Neonatal Med. 2020;33(24):4102–7.
Tan X, Zhou Y, Xu L, Zhang L, Wang J, Yang W. The predictors of necrotizing enterocolitis in newborns with low birth weight: A retrospective analysis. Medicine. 2022;101(7):e28789.
Tian M, Fan XQ, Dong Y.Risk factors and preventive measures for the occurrence of NEC in preterm combined very low birth weight infants. Int J Nurs. 2023;42(2):231–4.
Shao XM, Ye HM, Qiu XS.Publication of the fourth edition of practical neonatology. Chin J Pract Pediatr. 2011;26(11):880.
Shao, XM, Ye HM, Qiu XS. Practical Neonatology 5th ed. Beijing: People's Health Publishing House, 2019.
Walsh MC, Kliegman RM. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North America. 1986;33(1):179–201.
Avery's diseases of the newborn. In. Edited by Gleason CA, Devaskar SU, Avery ME, 9th ed. / edn. Philadelphia, PA: Elsevier/Saunders; 2012.
van Druten J, Khashu M, Chan SS, Sharif S, Abdalla H. Abdominal ultrasound should become part of standard care for early diagnosis and management of necrotising enterocolitis: a narrative review. Arch Dis Childhood Fetal Neonatal Ed. 2019;104(5):F551–9.
Chen XH, Yu ZB, Li YQ, Han SP. Guidelines for the management of necrotizing small bowel colitis in very low birth mass children in the United States. Pract Pediatr. 2012;27(14):1134–6.
Samuels N, van de Graaf RA, de Jonge RCJ, Reiss IKM, Vermeulen MJ. Risk factors for necrotizing enterocolitis in neonates: a systematic review of prognostic studies. BMC Pediatr. 2017;17(1):105.
Salvesen B, Stenvik J, Rossetti C, Saugstad OD, Espevik T, Mollnes TE. Meconium-induced release of cytokines is mediated by the TRL4/MD-2 complex in a CD14-dependent manner. Mol Immunol. 2010;47(6):1226–34.
Greenwood C, Morrow AL, Lagomarcino AJ, Altaye M, Taft DH, Yu Z, Newburg DS, Ward DV, Schibler KR. Early empiric antibiotic use in preterm infants is associated with lower bacterial diversity and higher relative abundance of Enterobacter. J Pediatr. 2014;165(1):23–9.
Cotten CM, Taylor S, Stoll B, Goldberg RN, Hansen NI, Sánchez PJ, Ambalavanan N, Benjamin DK, Jr. Prolonged duration of initial empirical antibiotic treatment is associated with increased rates of necrotizing enterocolitis and death for extremely low birth weight infants. Pediatrics. 2009;123(1):58–66.
Esaiassen E, Fjalstad JW, Juvet LK, van den Anker JN, Klingenberg C: Antibiotic exposure in neonates and early adverse outcomes: a systematic review and meta-analysis. Journal Antimicrob Chemother. 2017;72(7):1858–70.
Gagliardi L, Bellù R, Cardilli V, De Curtis M. Necrotising enterocolitis in very low birth weight infants in Italy: incidence and non-nutritional risk factors. J Pediatr Gastroenterol Nutrition. 2008;47(2):206–10.
Flidel-Rimon O, Friedman S, Lev E, Juster-Reicher A, Amitay M, Shinwell ES. Early enteral feeding and nosocomial sepsis in very low birthweight infants. Arch Dis Childhood Fetal Neonatal Ed. 2004;89(4): F289–92.
Li LQ, Wu B, Gao XX, Wang SX, Zheng ZS, Xu JL. A case-control study of microecological agents for the prevention and treatment of necrotizing small bowel colitis in neonates. Chin J Contemp Pediatr. 2006(06);464–6.
PHay S, Zupancic JA, Flannery DD, Kirpalani H, Dukhovny D. Should we believe in transfusion-associated enterocolitis? Applying a GRADE to the literature. Semin Perinatol. 2017;41(1):80–91.
Wan-Huen P, Bateman D, Shapiro DM, Parravicini E. Packed red blood cell transfusion is an independent risk factor for necrotizing enterocolitis in premature infants. J Perinatol. 2013;33(10):786–90.
Rai SE, Sidhu AK, Krishnan RJ. Transfusion-associated necrotizing enterocolitis re-evaluated: a systematic review and meta-analysis. J Perinatal Med. 2018;46(6):665–76.
Patel RM, Knezevic A, Shenvi N, Hinkes M, Keene S, Roback JD, Easley KA, Josephson CD. Association of red blood cell transfusion, anemia, and necrotizing enterocolitis in very low-birth-weight infants. Jama. 2016;315(9):889–97.
Neu J. The 'myth' of asphyxia and hypoxia-ischemia as primary causes of necrotizing enterocolitis. Biol Neonate. 2005;87(2):97–8.
Sankaran K, Puckett B, Lee DS, Seshia M, Boulton J, Qiu Z, Lee SK. Variations in incidence of necrotizing enterocolitis in Canadian neonatal intensive care units. J Pediatr Gastroenterol Nutrition. 2004;39(4):366–72.
Gan X, Mao J, Li J. Clinical characteristics and outcomes of neonatal necrotizing small bowel colitis. Clinical characteristics and outcome analysis of necrotizing small bowel colitis in neonates. Chin J Contemp Pediatr. 2019;21(10):1028–32.
Benitz WE. Committee on fetus and newborn, American academy of pediatrics. Patent ductus arteriosus in preterm infants. Pediatrics. 2016;137(1):10.1542/peds.2015–3730.
Mitra S, Florez ID, Tamayo ME, Mbuagbaw L, Vanniyasingam T, Veroniki AA, Zea AM, Zhang Y, Sadeghirad B, Thabane L. Association of placebo, indomethacin, ibuprofen, and acetaminophen with closure of hemodynamically significant patent ductus arteriosus in preterm Infants: A systematic review and meta-analysis. Jama. 2018;319(12):1221–38.
Beghetti I, Panizza D, Lenzi J, Gori D, Martini S, Corvaglia L, Aceti A. Probiotics for preventing necrotizing enterocolitis in preterm infants: A network meta-analysis. Nutrients. 2021;13(1).
D'Angelo G, Impellizzeri P, Marseglia L, Montalto AS, Russo T, Salamone I, Falsaperla R, Corsello G, Romeo C, Gitto E. Current status of laboratory and imaging diagnosis of neonatal necrotizing enterocolitis. Ital J Pediatr. 2018;44(1):84.
Patel RM, Underwood MA. Probiotics and necrotizing enterocolitis. Semin Pediatr Surg. 2018;27(1):39–46.
oindexter B. Use of probiotics in preterm infants. Pediatrics. 2021;147(6):e2021051485.
Bi LW, Yan BL, Yang QY, Li MM, Cui HL. Probiotic strategies to prevent necrotizing enterocolitis in preterm infants: a meta-analysis. Pediatr Surg Int. 2019;35(10):1143–62.
Costeloe K, Hardy P, Juszczak E, Wilks M, Millar MR. Bifidobacterium breve BBG-001 in very preterm infants: a randomised controlled phase 3 trial. Lancet (London, England). 2016;387(10019):649–60.
Roberts D, Brown J, Medley N, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2017;3(3):Cd004454.
Nanthakumar NN, Young C, Ko JS, Meng D, Chen J, Buie T, Walker WA. Glucocorticoid responsiveness in developing human intestine: possible role in prevention of necrotizing enterocolitis. American journal of physiology Gastrointestinal and liver physiology. 2005; 288(1):G85–92.
Huang L, Xiong T, Tang J, Feng ZC, Mu DZ. Clinical guidelines for the treatment of neonatal necrotizing small bowel colitis (2020). Chin J Contemp Pediatr.2021;23(1):1–11.
Nolan LS, Parks OB, Good M. A Review of the immunomodulating components of maternal breast milk and protection against necrotizing enterocolitis. Nutrients. 2019;12(1):14.
Sisk PM, Lovelady CA, Dillard RG, Gruber KJ, O'Shea TM. Early human milk feeding is associated with a lower risk of necrotizing enterocolitis in very low birth weight infants. Journal of perinatology: official journal of the California Perinatal Association. 2007;27(7):428–33.
Herrmann K, Carroll K. An exclusively human milk diet reduces necrotizing enterocolitis. Breastfeeding medicine: the official journal of the Academy of Breastfeeding Medicine. 2014;9(4):184-90.
Acknowledgements
Not applicable.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
SZ, HJ and YM conceptualized and designed the study, drafted the initial manuscript, reviewed and revised the manuscript; SZ, YM, WL and YL designed the collection instruments and collected data; HJ, HL performed quality assessment; SZ and YM performed the statistical analysis and participated in its design; AW, YZ and XC coordinated and supervised data collection, and critically reviewed the manuscript for important intellectual content. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethics approval for this study was not required.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 2:
Supplementary Information Table 2. Text database search criteria.
Additional file 3.
AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non- randomised studies of healthcare interventions, or both
Additional file 4: Table S3.
Assessment of methodological quality by NOS.
Additional file 5: S figure1.
Forest plot of the analysis regarding blood transfusion as a risk factor for NEC preterm infants. S figure2. Forest plot of the analysis regarding neonatal asphyxia as a risk factor for NEC preterm infants. S figure 3. Forest plot of the analysis regarding pneumonia as a risk factor for NEC preterm infants. S figure 4. Forest plot of the analysis regarding infection occurs as a risk factor for NEC preterm infants. S figure 5. Forest plot of the analysis regarding breastfeeding as a protective factor for NEC preterm infants. S figure 6. Forest plot of the analysis regarding congenital heart disease as a risk factor for NEC preterm infants. S figure 7. Forest plot of the analysis regarding meconium-stained amniotic fluid as a risk factor for NEC preterm infants. S figure 8. Forest plot of the analysis regarding mechanical ventilation as a risk factor for NEC preterm infants. S figure 9. Forest plot of the analysis regarding gestational diabetes mellitus as a risk factor for NEC preterm infants. S figure 10. Forest plot of the analysis regarding respiratory distress syndrome as a risk factor for NEC preterm infants. S figure 11. Forest plot of the analysis regarding prenatal application of glucocorticoids as a protective factor for NEC preterm infants. S figure 12. Forest plot depicting the analysis of intravenous immunoglobulin as a non-influencing factor for NEC preterm infants. S figure 13. Forest plot of the analysis regarding hypoalbuminemia as a risk factor for NEC preterm infants. S figure 14. Forest plot of the analysis regarding patent ductus arteriosus as a risk factor for NEC preterm infants. S figure 15. Forest plot of the analysis regarding respiratory failure as a risk factor for NEC preterm infants. S figure 16. Forest plot of the analysis regarding severe anemia as a risk factor for NEC preterm infants. S figure 17. Forest plot of the analysis regarding history of antibiotic use as a risk factor for NEC preterm infants. S figure 18. Forest plot of the analysis regarding intrahepatic cholestasis of pregnancy as a risk factor for NEC preterm infants.
Additional file 6: S figure19.
Funnel plot of breastfeeding. S figure20. Funnel plot of blood transfusion. S figure21. Funnel plot of oral probiotics. S figure22. Funnel plot of septicemia.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhao, S., Jiang, H., Miao, Y. et al. Factors influencing necrotizing enterocolitis in premature infants in China: a systematic review and meta-analysis. BMC Pediatr 24, 148 (2024). https://doi.org/10.1186/s12887-024-04607-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-024-04607-3