Abstract
Background
High-quality neonatal care requires sufficient functional medical devices, furniture, fixtures, and use by trained healthcare workers, however there is lack of publicly available tools for quantification and costing. This paper describes development and use of a planning and costing tool regarding furniture, fixtures and devices to support scale-up of WHO level-2 neonatal care, for national and global newborn survival targets.
Methods
We followed a systematic process. First, we reviewed planning and costing tools of relevance. Second, we co-designed a new tool to estimate furniture and device set-up costs for a default 40-bed level-2 neonatal unit, incorporating input from multi-disciplinary experts and newborn care guidelines. Furniture and device lists were based off WHO guidelines/norms, UNICEF and national manuals/guides. Due to lack of evidence-based quantification, ratios were based on operational manuals, multi-country facility assessment data, and expert opinion. Default unit costs were from government procurement agency costs in Kenya, Nigeria, and Tanzania. Third, we refined the tool by national use in Tanzania.
Results
The tool adapts activity-based costing (ABC) to estimate quantities and costs to equip a level-2 neonatal unit based on three components: (1) furniture/fixtures (18 default but editable items); (2) neonatal medical devices (16 product categories with minimum specifications for use in low-resource settings); (3) user training at device installation. The tool was used in Tanzania to generate procurement lists and cost estimates for level-2 scale-up in 171 hospitals (146 District and 25 Regional Referral). Total incremental cost of all new furniture and equipment acquisition, installation, and user training were US$93,000 per District hospital (level-2 care) and US$346,000 per Regional Referral hospital. Estimated cost per capita for whole-country district coverage was US$0.23, representing 0.57% increase in government health expenditure per capita and additional 0.35% for all Regional Referral hospitals.
Conclusion
Given 2.3 million neonatal deaths and potential impact of level-2 newborn care, rational and efficient planning of devices linked to systems change is foundational. In future iterations, we aim to include consumables, spare parts, and maintenance cost options. More rigorous implementation research data are crucial to formulating evidence-based ratios for devices numbers per baby. Use of this tool could help overcome gaps in devices numbers, advance efficiency and quality of neonatal care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Key findings
WHAT WAS KNOWN? |
• Scale-up of WHO level-2 care for small and sick newborns, which includes the provision of continuous positive airway pressure, is receiving increasing global and national attention. This effort has potential to save 747,000 lives annually, in line with Every Newborn Action Plan's fourth target. The target aims to have at least one unit providing level-2 care in 80% of sub-national districts by 2025 • Neonatal devices are lacking or may be donated or procured from high-income settings and hence often unfit for use in low-and middle-income countries (LMIC) due to missing parts and limited training • Health managers/planners are requesting evidence-based approaches to inform equipping newborn care units with appropriate types and quantities of devices and ward furniture • We aimed to co-design, with multi-disciplinary input, a costing tool for newborn care devices and furniture for planners to use at national or subnational levels |
WHAT WAS DONE THAT IS NEW? |
A systematic process was applied: • Review of relevant costing tools, including the UNICEF Oxygen System Planning Tool being the only one that was closely related to our tool’s remit, and we adopted its stepwise approach • Co-design with multi-disciplinary experts to develop a tool for estimating required quantities and incremental costs of ward furniture and devices • Operationalise this tool to estimate set-up costs in Tanzania for 146 Districts and 25 Regional Referral hospitals |
WHAT WAS FOUND? |
• A customisable tool based on activity-based costing approach was developed allowing quantification and costing for a default 40-bed neonatal unit (or multiples thereof), including a ten-bed level-2 (high-dependency) unit for small and sick newborn care. The tool includes three components: (1) ward furniture and fixtures (18 items as default with ratios and unit costs), (2) neonatal devices (16 items as default with ratios and unit costs), (3) device installation training cost estimates for a one-day, onsite face-to-face training • Hence automatically generating cost and procurement estimates are automatically generated into a result dashboard. In Tanzania, it was feasible to collect cost data and generate reports for inclusion in the annual budgeting cycles in less than a week by a non-economic expert user |
WHAT NEXT? |
• The tool provides policymakers with evidence-based cost information to guide budget allocation and catalyse resource mobilisation for scale-up of level-2 care for small and sick newborns • Future iterations of the tool aim to include quantities and costing for consumables, spare parts, and maintenance • There is a need for more robust data on device-to-baby ratios, case mix and more data on unit costs from regions beyond Africa to improve transferability |
Background
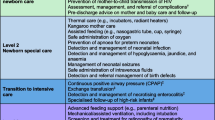
Hospital-based care for small and sick newborns has potential to avert approximately 750 000 neonatal deaths each year [1]. Despite the Sustainable Development Goals (SDGs) target for each country to reduce neonatal mortality to < 12 deaths per 1,000 live births by 2030, 63 countries remain off track [2]. To accelerate progress, the Every Newborn Action Plan (ENAP) calls for countries to establish at least one unit providing level-2 care plus respiratory support with continuous positive airway pressure (CPAP) (referred to as level-2 care in this paper) in 80% of sub-national units (e.g., districts) by 2025 [3]. Standard care at this level includes thermal care, kangaroo mother care (KMC), assisted feeding and intravenous fluids, safe administration of oxygen, neonatal sepsis management with injected antibiotics, management of neonatal jaundice with phototherapy, management of neonatal encephalopathy, detection of congenital abnormalities and referral or management of birth defects [1, 3]. In addition, the management of respiratory distress with CPAP during transition. Level-2 care alone is not sufficient; linking neonatal care from level-1 to level-3 is necessary to achieve a global neonatal mortality target [1]. Level-1 provides immediate and essential newborn care while level-3 provides intensive and advanced care for very sick babies (Table 1) [1, 4]. Achieving high coverage and high-quality requires the right physical space, the right people with the right training, and the right devices [1, 5, 6].
Low-and middle-income countries (LMIC) are increasingly prioritising small and sick newborn care (SSNC) in national plans and targets [3], but the devices, and system changes required to implement high-quality inpatient newborn care are challenging [5, 7, 8]. In high-income settings, care of an admitted newborn often involves more than 20 devices [9]. Analyses of bottlenecks to scale-up of high-quality care for mothers and newborns in 12 LMICs with most of the world’s newborn deaths found that lack of devices and ward furniture was a major challenge, and healthcare workers were often not confident in their ability to use devices effectively [10].
Many hospitals, especially those in resource-limited settings, have a shortage of functional medical devices and supplies. Historically, donated medical equipment has been relied on to meet this need, often without considering local constraints for training for use, maintaining, repairing, and decommissioning equipment. This has resulted in “equipment graveyards”, [11, 12]. While donations can help address acute shortages, they often come without user training, sustained consumable supply, compatible spare parts, or maintenance plans to ensure continuous functionality [13,14,15,16,17]. Additionally, context-specific considerations affecting device performance (e.g., dust, extreme temperatures, humidity, frequent power outages, etc.) are crucial to ensure value for money based on lifetime use [12, 18]. To ensure continuous device functionality, planners need to include distribution, maintenance, and consumable costs. On-site warranties, although these may increase the purchase price, may provide better value long-term [10, 12, 19]. In addition to procurement, onsite training of both clinicians and hospital biomedical technicians is fundamental to effective and safe use of devices.
Costing of medical devices requires determining the device types and quantities needed and unit cost data [5, 12]. There is a lack of global normative guidance for device-to-baby ratios and furniture specifications needed to provide level-2 care [20]. We were unable to find any open-source costing tool to inform budgeting for neonatal care ward furniture and devices. Costing that considers other health systems inputs, such as infrastructure and human resources is also crucial, but requires wider systems costing, often with economic expertise [21].
Aim and objectives
This paper is part of a supplement with the NEST360 Alliance, providing tools, analysis, and novel learning for implementing SSNC. In this paper, we aim to describe the development and refinement of a planning and costing tool. The intended audience is health planners at national, sub-national, or facility levels charged with planning and budgeting. The paper addresses three objectives:
-
Objective 1: Review relevant planning and costing tools to assess content, design and costing approaches.
-
Objective 2: Co-design content for a device and furniture planning and costing tool for a functional level-2 neonatal unit.
-
Objective 3: Refine and use tool to estimate cost of national scale-up in mainland Tanzania.
Methods
Methods by objectives
Objective 1: Review relevant planning and costing tools to assess content, design and costing approaches
We searched for open-source planning and costing tools relevant to maternal and child health, including grey literature due to limited results in international bibliographies databases. Data extraction was informed by an adapted ISPOR Criteria for Cost(-Effectiveness) Review Outcomes (CiCERO) Checklist [22] (Additional file 1) and was completed in two phases. In phase 1, we compared data inputs, tool’s features, and economic approaches of widely used costing tools with maternal and child health fields to inputs required for care of small and sick newborns specifically. In phase 2, we examined the activity-based costing approach to establish its inclusion in the tool design, and device-specific planning and costing tool, UNICEF Oxygen System Planning Tool, to gain insight into its underlying costing assumptions, outputs, and format.
Objective 2: Co-design content for a device and furniture planning and costing tool for a functional level-2 neonatal unit
We engaged a multidisciplinary group of newborn care implementers with professional experience in LMIC (including clinicians, biomedical technicians and engineers, national policymakers, trainers, economists, and researchers) to inform tool development and ensure a user-friendly design. We defined criteria for the tool a priori and designed the branching logic framework to guide content and data inputs.
A priori criteria included:
-
A default 40-bed neonatal unit, including a ten-bed level-2 unit for care of small and sick newborns, was adopted from the Tanzanian newborn unit floor plan for a District hospital. In Tanzania, this level-2 care unit is known as the high dependency unit (HDU). The floor plan includes five rooms: the HDU/ level-2 care (ten cots), a general, step-down neonatal ward (ten cots), an isolation room (five cots), a kangaroo mother care (KMC) room (ten adult beds) and a rooming-in area (five adult beds) [23] (Table 2). The default neonatal unit and level-2 care bed capacity can easily be adjusted up in multiples of ten.
-
Remit to include the following components: (1) ward furniture and fixtures (permanently installed equipment or furniture in the newborn unit), (2) neonatal devices, and (3) training for use (Fig. 1). The tool was structured based on these three components and built in Microsoft Excel. Additional components were identified (i.e., (4) consumables and spare parts, and (5) maintenance) but not possible to include in this version of the tool given cost data gaps. Quantities required for the ward furniture and fixtures (first component) and user training at device installation (third component) were determined based on a default 40-bed neonatal unit. On the other hand, quantities required for the devices (second component) were based on the ten-bed level-2 care unit only (Table 2).
Component 1: Ward furniture and fixtures (types, quantification, and costs)
A list of ward furniture and fixtures required for a newborn unit was compiled through a review of the World Health Organization (WHO) [24], the United nation international children’s emergency fund (UNICEF) guidelines [25] and Tanzanian national neonatal care manuals [26]. There were sparse data from these policy documents to inform the quantity of each item required, so we estimated quantities based on either number of beds or rooms as per the Tanzanian national floor plans for a District hospital newborn unit [23], supplemented by United Nations (UN) materials [25, 27, 28] and experts' opinion. To derive unit costs for furniture and fixtures we reviewed quotations (2022) from local government suppliers and private distributors (national or international distributor who supplies a range of neonatal items) tender documents from Tanzania, Kenya and Nigeria and calculated a median cost and range. Median costs from local government suppliers and private distributors were compared to assess variation. The local government suppliers’ median cost was used to derive the tool’s default point estimate.
Component 2: Neonatal devices (specification, quantification, and costs)
To identify types and quantities of devices to include in the tool for ten-bed level-2 care for small and sick newborns at District hospital, we reviewed several documentary sources [25, 27,28,29,30] and considered expert opinion. Device specifications, especially relevant for purchasers and procurement officials, were informed by UNICEF-NEST360 Target Product Profiles (TPP) [31]. A TPP is an outline of desired product characteristics aimed at addressing the needs of a particular disease(s)/medical condition [32]. The UNICEF-NEST360 TPP process involved a consensus-driven approach with 103 key stakeholders from 22 countries who voted on product characteristics for 16 types of technologies across six categories of care: hydration, nutrition, drug delivery, jaundice management, point of care diagnostics, infection prevention and control, respiratory support, and thermal management [31]. Of these 16 product categories, a minimum of two product options from different manufacturers of NEST360-qualified devices [33] were included in the tool to achieve brand neutrality.
To derive the price per device for a level-2 unit for the care of small and sick newborns, we followed a normative approach utilising market prices outlined by the government procurement agencies’ publicly available pricelists and requested quotes from private distributors in Kenya, Nigeria, and Tanzania. Median costs from government procurement agencies and private distributors were compared to assess variation. The government procurement agencies median cost was used as the tool’s default unit cost point estimate. Aside from government procurement agencies and private distributors, we identified the types of devices available from the UNICEF supply catalogue, though unit prices were not included due to variation in logistical costs e.g. freight across countries.
Component 3: User training at device installation
Training is crucial for safe use and troubleshooting of devices. Based on our experience of implementing a SSNC package through the NEST360 alliance in 67 newborn units across four countries, we costed a one-day, facility-based training combining local health providers (clinicians and nurses) and hospital biomedical engineers and technician(s). We reviewed user training logs to inform the number of participants and copies of necessary training materials. To derive unit costs, we reviewed current government reimbursement policies and prevailing market costs (i.e., cost of stationeries, meals, refreshments, etc.) across three countries (Kenya, Nigeria, and Tanzania). Malawi (the fourth implementing country with NEST360) was excluded as it had achieved a national scale-up to exceed ENAP target 4. The median value was calculated and used as the tool’s default estimate. Some sparse data inputs were refined through expert consultation.
Objective 3: Refine and use tool to estimate cost for national scale-up in mainland Tanzania
The tool was used in mainland Tanzania, one of the few countries that met the 2015 Millennium Development Goal target 4 of reducing under-5 mortality by two-thirds. However, from 2010 to 2015, the national neonatal mortality rate (NMR) remained almost unchanged [34]. This stagnation and in keeping with ENAP target 4, mainland Tanzania’s national health strategic plan and One Plan III prioritised the scale-up of level-2 care in 80% of District hospitals (146) and all (25) Regional Referral hospitals by 2025 [35].
To achieve this target, the Ministry of Health sought to develop a national investment case for scale-up to the 171 hospitals, incorporating infrastructure, human resources, and other system costs [21]. As part of the investment case development, this tool was customised to estimate furniture, fixture, and device costs (assuming all items would be purchased new) for both the District hospital and Regional Referral hospital scale-up. As per the guidelines Regional Referral hospital was defined to provide full level-2 care for sick babies and partial level-3 care for critically ill newborns awaiting referral to the intensive care unit (i.e., level-3 care) for further treatment and management.
Incremental costs for District and Regional Referral hospitals were estimated separately in the tool due to differences in unit size, types and quantities of devices needed. Incremental quantities were estimated based on Tanzania’s national neonatal floorplans, District hospital costing assumed a 40-bed size with a ten-bed level-2 unit for care of small and sick newborns (i.e., the tool’s default quantities), whilst Regional Referral hospital costing was customised from the default to an 80-bed neonatal unit with 20-bed level-2 care unit (i.e., tool’s default list of items with more quantities plus an estimate of devices for partial level-3 care) [23]. The additional neonatal devices and furniture and fixtures were multiplied by the unit costs derived from Tanzanian national medical agency pricelist (2022) [36] and local government suppliers respectively. The unit costs were converted to US dollars (2022 average exchange rate of 2324 TZS per USD) before being entered to the tool. The cost per capita at both levels of care was calculated using the mainland Tanzanian population (2022) of 60 million [37]; whilst cost per birth was estimated using annual total birth (2020) of two million [35].
Data collection and report generation were led by a purposively sampled team of ten Tanzanians, representatives from the Ministry of Health and the NEST360 country team, with economists' support. The Tanzanian team (consisting of six clinicians, three economists, and two qualitative researchers) were engaged through informal and formal interviews to understand their experiences on usability, time burden, and perceptions of the tool’s content.
Results
Our findings and learnings are summarised according to the three objectives:
Objective 1: Review relevant planning and costing tools to assess content, design and costing approaches
The widely used costing and impact estimation tools; the Lives Saved Tool (LiST) costing module [38] and One Health [39] were reviewed. Appraisal of Activity-Based costing approach [19, 40] was done to inform the tool’s design. We also identified a useful device-specific tool to learn from, the UNICEF Oxygen System Planning Tool [41, 42].
LiST estimates lives saved through reproductive, maternal, newborn, and child health (RMNCH) interventions, and has more approximate costs to inform return on investment (ROI) estimates [43, 44]. One Health is led by WHO and designed to inform health systems planning towards universal health coverage on a wide scale: national or sub-national levels [38, 39, 45] to generate estimates of health impact and cost, useful for developing broad investment cases. Both tools cover a broad remit of services and tend to be more focused on inputs for essential newborn care (level-1 care) than level-2 care. This is explained by the limited detail on neonatal care costs, for example, LiST costing module includes a bag and mask resuscitation and a few other items, mostly antibiotics. Costs in both tools are classified as set-up or recurrent, and calculated as either total or incremental, following an ingredients-based or bottom-up approach; where each resource required for an intervention is identified and valued using reliable cost estimates e.g., international price lists. Such an approach is suitable for costing interventions with defined guidelines but is less useful for interventions where various ‘ingredients’ lack normative quantity standards, as is the case for level-2 newborn care. Both LiST and One Health calculate the costs of the capital items of health systems components (e.g., infrastructure, furniture, devices and programmatic) as a percentage of total intervention costs, whereas we required a tool that identifies and quantifies key components e.g., type of ward furniture, fixtures, and neonatal devices for level-2 newborn unit and calculates their incremental costs thus adopting the activity-based costing approach for this tool. The activity-based costing approach is a principle that seeks to identify specific costs items and assign them to the health services delivered to better understand and manage total costs. Also, both One Health and LIST tools require skills and training for use whilst our remit was to develop a tool that can be used by a non-economic expert (Additional file 2).
The UNICEF Oxygen System Planning Tool was designed for a wider, non-specialist user group and focuses on incremental costs, primarily for set-up, and uses a stepwise approach, with easily customisable data input fields and a results dashboard [41, 42] (Additional file 2). This tool’s format was most applicable to our target audience and remit. However, the micro-costing approach of entering data in different sheets may be time-consuming and demanding, prolonging the planning process.
Objective 2: Co-design content for a device and furniture planning and costing tool for a functional level-2 neonatal unit
The user-designed tool follows the Activity-Based Costing (ABC) to provide quantification and cost based on three components (Fig. 1): (1) ward furniture/fixtures (18 default but editable items); (2) neonatal medical devices (16 product categories with minimum specifications for use in LMIC contexts); (3) user training at device installation. Results are displayed in summary dashboards. The procurement report auto-populates the summary of quantities per item to be procured and outlines minimally acceptable product specifications, including examples of device names and models that met an accepted qualification process. The cost report provides a summary of scale-up costs and costs per component, which enables assessment of cost drivers. Impact of the investment on the budget is also calculated and expressed as cost per capita (total costs divided by the county’s population) and cost per birth (total costs divided by the country’s annual total birth).
Component 1: Ward furniture and fixtures (types, quantification, and costs)
A total of eighteen default furniture items were identified based on UN guidelines and national policies. The quantities required are shown in (Table 3). Recommended quantities included one extra item of each type of fixture as a contingency in case of breakdown.
Unit costs were derived from local government suppliers' absolute price ranges across Kenya, Nigeria, and Tanzania. The costs were consistent for fifteen items except for voltage stabilisers and uninterrupted power supply (UPS) which were relatively higher in Kenya, and refrigerators with freezer compartments and emergency trolleys were expensive in Tanzania. Of the 18-ward furniture and fixtures items, 11 (61%) had greater median prices amongst private distributors compared to local government suppliers (Fig. 2a). The average relative percentage difference for the median cost of these 11 items was 17%, largely driven by the percentage difference in the cost of measuring tape between private distributors compared to local government suppliers (42%). On the other hand, seven (39%) items had lower median prices amongst private distributors compared to local government suppliers. The average relative percentage difference for the median cost of these seven items was 9% (Fig. 2a).
Relative percentage difference of median unit costsa for furniture, fixtures, and devices required for a level-2 neonatal unit A. Compares local supplier median unit cost to private distributor median unit cost per ward furniture/fixture B. Compares government procurement agency median unit cost to private distributor median unit cost per device Footnotes: aMedian from Kenya, Tanzania, and Nigeria (see Additional File 1 for further detail) Abbreviations: UPS, uninterrupted power supply, KMC, kangaroo mother care, L/Hr
Component 2: Neonatal devices (device type and specification, quantification, and costs)
A default list of 16 types of devices was reached through review and consensus agreement among a multi-disciplinary group (Table 4). This default device list is editable to add or remove and was informed particularly by UN publications. Priority medical devices for newborn health from the WHO inter-agency list of (26) included forty-three devices according to the level of health care delivery, and use for laboratory, anthropometric, or general hospital context. UNICEF country-specific guides listed neonatal devices per level of newborn care: special care newborn unit (level-2 care neonatal unit) and essential newborn care unit (level-1 care newborn unit). The multi-country health facility assessment reports itemised devices available at District (level-2 care) and Tertiary hospitals (level-3 care) (see Additional file 3).
Device quantification assumptions were based on a ten-bed level-2 unit with an option to customise. UNICEF neonatal care manuals provided guidance on number of devices based on the number of beds: UNICEF India for a 12-bed unit (22); UNICEF Bangladesh for a ten-bed unit (24); and UNICEF Sierra Leone for a ten-bed unit (25). The total number of devices ranged between 21 and 30 and were classified as either essential or desirable (Additional file 3). Out of the sixteen, 11 of the device types, minimally acceptable specifications were included, based on UNICEF/NEST360 target product profiles [31], as well as two to three examples of device names and models that conformed to specifications [33] (Additional File 4).
Unit price was derived from government procurement agencies as the tool’s default estimate with an option to customise. Government procurement agencies' unit prices across the three countries were remarkably consistent for all the devices. The lowest to the highest unit price per device ratio averaged 0.28. However, the price difference of glucometers and syringe pumps was high in Tanzania, whilst phototherapy units and CPAP prices were high in Kenya. According to the government sources the costs included logistic costs (i.e., freight, inspection, duty, and distribution). Installation was assumed to be done by government-salaried biomedical experts.
Across the 16 devices, the private distributor median unit cost for 12 (75%) devices were higher than that of the government procurement agencies (Fig. 2b). The average relative percentage difference for the median cost of these 12 items was 20%. There was minimal difference (< 10%) in the median unit costs between government procurement agencies and private distributors for radiant warmers, bilirubinometers, and oxygen concentrators. The median unit prices for four neonatal devices (i.e., weighing scales, glucometers, suction pumps, and oxygen flow splitters) were found to be higher through government procurement agencies than with private distributors (Fig. 2b). In addition, thirteen of the sixteen devices were listed in the UNICEF supply catalogue. The glucometer, hemoglobinometer, and bilirubinometer instruments were not available.
Component 3: User training at device installation
We costed for training a minimum of 25 healthcare workers, including nurses, clinical officers, medical doctors, and biomedical engineers and technicians; neonatologists and neonatal nurse(s) could be included if available. The training was delivered by two external facilitators – a nurse and a biomedical engineer/technician, government-salaried employees. Costed items were facilitator fees and travel reimbursement, refreshments and meals, and training materials (e.g., job aids, flip charts, booklets, etc.) (Additional 4). Government per diem rates across the three countries were relatively consistent with ratio of lowest to highest per diem rate averaging 0.8. There was no variation in training input costs across countries. Data from 20 hospitals implementing with NEST360 showed nurses made up 50–75% of installation trainees drawn from newborn units, paediatric, maternity, and labour wards.
Objective 3: Refine and use tool to estimate cost for national scale-up in mainland Tanzania
We estimated an incremental scale-up cost (assuming entirely new furniture and devices required for all categories) per District hospital at US$93,000 and US$346,000 per Regional Referral hospital. The higher cost of setting up a Regional Referral Hospital is attributed to increased unit capacity (10-bed to 20-bed level-2 care/HDU unit) that required more ward furniture, fixtures, and devices for level-2 care and additional devices for partial level-3 care. Partial level-3 care entails providing comprehensive inpatient special newborn care provided in secondary health facilities e.g., district hospitals plus some components of intensive newborn care services provided at the tertiary level of care, as defined by WHO (Table 1). Devices for partial level-3 care comprised a customised list of fourteen items (Table 5). The total cost to procure new furniture, fixtures, and devices and train users in the country's 171 hospitals was estimated to be US$22.2 million. Ward furniture and fixtures accounted for US$9.0 million (41%), neonatal devices for US$12.7 million (57%), and user training at device installation for US$0.5 million (2%). The incremental cost of the rollout to 146 District hospitals was US$13.6 million, with ward furniture and fixtures costing US$7.4 million (54%), neonatal devices costing US$5.8 million (43%), and user training costing US$0.3 million (3%) (Fig. 3). The total cost of scale-up for Regional Referral hospitals was slightly lower than District hospitals at US$8.6 million. District hospital national scale-up was estimated to cost an incremental US$0.23 per capita and US$6.30 per birth, while Regional Referral hospitals were estimated to cost US$0.14 per capita and US$4.10 per birth. The budget implications of scaling level-2 care to whole district coverage in the country estimated a 0.57% increase in government health expenditure per capita (from 40.62 in 2020). Adding 25 Regional Referral hospitals would be an additional 0.35%.
Tool users in Tanzania had positive feedback on the stepwise tool structure and default entries of quantities and unit cost. They cited the need for additional guidance notes next to the data input fields to aid prompt and accurate data entry. On the other hand, non-clinical users reported difficulty understanding certain device descriptions and specifications and needed additional clarification and support. These concerns were refined in the tool and validated via a virtual walk-through session with the users.
It took one week to collect and enter information (e.g., unit costs and demographic data) and generate the cost and procurement reports. All the users felt the reports were simple to interpret and could be incorporated into their budget planning processes.
Discussion
Implementing high-quality inpatient care for small and sick newborns requires sufficient, robust, context-appropriate devices and planning for user training and maintenance [5, 16]. We developed a novel newborn-specific planning and costing tool to support the national scale-up of SSNC and used the tool in Tanzania. The tool uses the ABC approach yet mirrors the stepwise approach of the UNICEF Oxygen System Planning Tool [16]. The tool's default costing estimates are based on publicly available government procurement agency pricelists, which are marginally lower on average than private distributor costs where available but may not be of comparable specification or post-distribution support.
Health system costing tools (i.e., the WHO One Health tool and the LiST costing module) had limited newborn-specific device inputs [39], which is unsurprising given the relatively recent global focus on SSNC. However, if countries are to achieve international standards for quality of care for small and sick newborns in health facilities [24], planners need to be enabled to more accurately budget and develop investment cases to mobilise resources. SSNC investment cases that used the LiST costing methodology had to add many specific items and cost assumptions to account for programme management and health system costs [43]. Our planning and costing tool is based on the activity-based costing approach, providing specific inputs for SSNC components, addressing a gap in existing tools. Incorporating newborn cost input data from this tool into existing health system tools (which may include estimates for components not included in our tool (e.g., human resources) could make costing estimates more comprehensive. On the other hand, the tool can also be used by a non-economic expert for standalone planning to refurbish an existing neonatal unit or estimate costs to fully fit out a new unit.
Use of the tool in mainland Tanzania revealed feasibility for use by a non-economic expert to generate reports and results were able to catalyse additional investment in care for small and sick newborns. To scale up SSNC nationally in Tanzania, the estimated incremental cost per capita was US$0.23 for 146 District hospitals and US$0.14 for 25 Regional Referral hospitals. These are modest estimates when compared to scaling up community-based maternal and newborn care interventions in Tanzania (US$1.30), Ghana (US$0.40), and Malawi (US$1.00) [46]. Similarly, when compared estimates of costs per capita to scale-up of mental health in low-income countries (US$1.85–2.60) [47] and malaria (US$1.20–5.70) services [48], the indicative SSNC estimates are relatively lower, suggesting it may be an affordable investment. Advocating and prioritising for sustained investment in SSNC requires tools that provide evidence-based cost estimates and impact on budget. However, many countries still rely on short-term donor investment for maternal and child health interventions, making planning for activities that span over several years challenging [49, 50], and newborns have been historically under-represented in health budgeting decisions [51]. Despite the disproportionately high neonatal mortality burden, and the potential return on investment in SSNC (between US$8 –12 for every US$1 invested) [21], the percentage of RMNCH donor aid that specifically mentions newborns remains small [52]. Costing estimates from the tool may help to catalyse more funding, from government sources and non-traditional donors.
Strengths of this work include the user-centric approach, systematic development of the tool, and transparency of the data sources. The tool’s customisability to reflect the local guidelines and costs, given the observed price variability and step-by-step approach with guidance notes, makes it feasible for use by individuals without an economics background. Reports generated by the tool, include minimum technical specifications of devices with corresponding product examples which can be useful to inform tender documents and budget cycle discussions. Procuring context-appropriate devices (i.e., those qualified for low-resourced settings) can increase the lifetime of a device and avoid exacerbating “equipment graveyards” [33]. These reports are possible to generate within a week, as found in Tanzania.
There are also limitations, inherent to data gaps for evidence-based newborn-to-device ratios. These gaps reflect the recent rise of SSNC on the global agenda – the first WHO norms and standards were only published in 2020 [24]. Whilst we reviewed existing information, device ratios in the past have tended to rely on expert opinion – highlighting crucial implementation research questions. The current version of the tool is focused on the set-up costs for a level-2 neonatal unit with device quantities based on a default ten-bed capacity. While the ten-bed option is pragmatic, most district hospitals will likely require more data on the need versus population or case mix to inform their decisions on the cots and bed capacity and device ratios. Important cost components (Fig. 1) such as device consumables, spare parts, and maintenance are not included yet and require more data. Ongoing data collection in hospitals implementing with NEST360, and in other regions and countries, may provide better quality data to assess device and staffing ratios and optimal unit size, including appropriate number of cots and beds. While we recognize that the current Excel version is user-centred, it may crash as more data is added; moving to a user-friendly platform may increase use.
We assumed a constant unit cost, whilst economies of scale and other cost-saving opportunities might exist, so the costs may be lower than we report. The tool default cost estimates may underestimate costs as the government procurement agencies, whilst mostly consistent across these three African countries, were generally lower than private distributors. Cost differences may be attributable to more stringent device specifications and explicit add-ons (e.g., installation, one-year warranty costs, starter packs of consumables, etc.) included in private distributor costs. The government procurement agency pricelists do not give minimum specifications for devices. Instead, some provide a list of companies from which health facilities can procure devices [53]. Research comparing actual costs incurred and default estimates beyond the three countries will improve the reliability and transferability of default estimates.
Conclusion
Use of data to guide budget allocation and catalyse resource mobilisation is crucial in all contexts, but even more so in high-burden settings with relatively low per capita expenditures on health. The review revealed gaps for systematic planning tools notably for devices for small and sick newborn care. Our new tool provides practical evidence-based guidance to countries scaling up care for small sick newborns to accelerate progress toward ENAP and the SDG 3.2 target for neonatal survival. Systematic planning and costing could prevent costly mistakes that can arise from incorrect estimations (e.g., not enough devices procured, or devices not adequately maintained). To provide high-quality newborn care, the use of appropriate devices, furniture, and fixtures must be coupled with effective implementation including infrastructure, health workforce and data to drive change, reaching every district in every country.
Availability of data and materials
Data used was available in the public domain. The Excel-based tool is available on www.newborntooolkit.org.
Abbreviations
- ABC:
-
Activity-Based Costing
- CiCERO:
-
Criteria for Cost(-Effectiveness) Review Outcomes
- ENAP:
-
Every Newborn Action
- HDU:
-
High Dependency Unit
- ISPOR:
-
The Professional Society for Health Economics and Outcomes Research
- KMC:
-
Kangaroo Mother Care
- LiST:
-
Lives Saved Tool
- LMIC:
-
Low- and Middle-Income Countries
- NEST360:
-
Newborn Essential Solutions and Technologies
- RMNCH:
-
Reproductive Maternal Newborn and Child Health
- ROI:
-
Return on Investment
- SDG:
-
Sustainable Development Goal
- SSNC:
-
Small and Sick Newborn Care
- TPP:
-
Target Product Profile
- TZS:
-
Tanzania Shilling
- UN:
-
United Nations
- UNICEF:
-
United Nations Children’s Fund
- US:
-
United States
- WHO:
-
World Health Organization
References
World Health Organization. Survive and Thrive: Transforming Care for Every Small and Sick Newborn. Geneva; 2019. Available from: https://www.who.int/publications/i/item/9789241515887. [cited: 2022 Nov 12].
United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development. 2015 . Available on: https://sdgs.un.org/2030agenda. [cited 2023 Feb 4].
World Health Organization. Ending Preventable Newborn Deaths and Stillbirths by 2030: Moving Faster Towards High-Quality Universal Health Coverage in 2020–2025. 2020 Jul 01. Available from: https://www.unicef.org/media/77166/file/Ending-preventable-newborn-deaths-and-stillbirths-by-2030-universal-health-coverage-in-2020%E2%80%932025.pdf. [cited: 2023 Jan 03].
World Health Organization. Born Too Soon: Decade of Action on Preterm Birth. 2023 . Available from: https://www.who.int/publications/i/item/9789240073890. [cited: 2023/05/23].
Dickson KE, Kinney MV, Moxon SG, Ashton J, Zaka N, Simen-Kapeu A, et al. Scaling up Quality Care for Mothers and Newborns around the Time of Birth: An Overview of Methods and Analyses of Intervention-Specific Bottlenecks and Solutions. BMC Pregnancy Childbirth. 2015;15(S2):S1.
Lawn JE, Blencowe H, Oza S, You D, Lee ACC, Waiswa P, et al. Every Newborn: Progress, Priorities, and Potential Beyond Survival. The Lancet. 2014;384(9938):189–205.
Moxon SG, Lawn JE, Dickson KE, Simen-Kapeu A, Gupta G, Deorari A, et al. Inpatient Care of Small and Sick Newborns: A Multi-Country Analysis of Health System Bottlenecks and Potential Solutions. BMC Pregnancy Childbirth. 2015;15(S2):S7.
Ginsburg AS, Macharia W, Ansermino JM. Evaluating Neonatal Medical Devices in Africa. Lancet Digit Health. 2021;3(4):e211–2.
Li Q, Li X, Zhang Q, Zhang Y, Liu L, Cheng X, et al. A Cross-Sectional Nationwide Study on Accessibility and Availability of Neonatal Care Resources in Hospitals of China: Current Situation, Mortality and Regional Differences. Lancet Reg Health West Pac. 2021;14:100212.
Dickson KE, Simen-Kapeu A, Kinney MV, Huicho L, Vesel L, Lackritz E, et al. Every Newborn: Health-Systems Bottlenecks and Strategies to Accelerate Scale-up in Countries. Lancet. 2014;384(9941):438–54.
Perry L, Malkin R. Effectiveness of Medical Equipment Donations to Improve Health Systems: How Much Medical Equipment Is Broken in the Developing World? Med Biol Eng Compu. 2011;49(7):719–22.
World Health Organization. Medical Devices: Managing the Mismatch an Outcome of the Priority Medical Devices Project. 20 Avenue Appia,1211 Geneva 27: WHO Press; 2010 Jul 01. Available from: https://www.who.int/publications/i/item/9789241564045. [cited: 2023 Jan 03].
Marks IH, Thomas H, Bakhet M, Fitzgerald E. Medical Equipment Donation in Low-Resource Settings: A Review of the Literature and Guidelines for Surgery and Anaesthesia in Low-Income and Middle-Income Countries. BMJ Glob Health. 2019;4(5):e001785.
Diaconu K, Chen Y-F, Cummins C, Jimenez Moyao G, Manaseki-Holland S, Lilford R. Methods for Medical Device and Equipment Procurement and Prioritization within Low- and Middle-Income Countries: Findings of a Systematic Literature Review. Globalization and Health. 2017;13(1).
World Health Organization. Medical Device Donations: Considerations for Solicitation and Provision. 20 Avenue Appia,1211 Geneva 27: WHO press; 2011. Available from: https://www.who.int/publications/i/item/9789241501408. [cited: 2023 Jan 6].
Reddy M, Samprathi M, Bhatia V. Medical Equipment Donation: An End in Itself or a Mean to an End? Indian J Crit Care Med. 2022;26(3):399–400.
Thairu L, Wirth M, Lunze K. Innovative Newborn Health Technology for Resource-Limited Environments. Tropical Med Int Health. 2013;18(1):117–28.
WHO. Medical Devices: Managing the Mismatch: An Outcome of the Priority Medical Devices Project. 2010. Available from: https://www.who.int/publications/i/item/9789241564045. [cited: 2023 Jan 15].
Narayanan I, Nsungwa-Sabiti J, Lusyati S, Rohsiswatmo R, Thomas N, Kamalarathnam CN, et al. Facility Readiness in Low and Middle-Income Countries to Address Care of High Risk/ Small and Sick Newborns. Maternal Health, Neonatology and Perinatology. 2019;5(1).
Keene CM, Aluvaala J, Murphy GAV, Abuya N, Gathara D, English M. Developing Recommendations for Neonatal Inpatient Care Service Categories: Reflections from the Research, Policy and Practice Interface in Kenya. BMJ Glob Health. 2019;4(2):e001195.
Kamuyu R, Tarus A, Bundala F, Msemo G, Shamba D, Paul C, et al. Investment case for small and sick newborn care in Tanzania: systematic analyses. BMC Pediatr. 2023.
Mandrik O, Severens JL, Bardach A, Ghabri S, Hamel C, Mathes T, et al. Critical appraisal of systematic reviews with costs and cost-effectiveness outcomes: An Ispor good practices task force report. Value Health. 2021;24(4):463–72.
Ministry of Health Tanzania. Proposed neonatal unit plan for district and regional referral hospitals. 2022. [cited 2023 Jan 10]. Available from: https://www.moh.go.tz/.
World Health Organization. Standards for improving quality of care for small and sick newborns in health facilities. Geneva. 2020. [cited 2023 Mar 20]. Available from: https://www.who.int/publications/i/item/9789240010765.
UNICEF. Toolkit for setting up special care newborn units, stabilisation units and newborn care corners. 2010. [cited 2021 Nov 23]. Available from: https://www.healthynewbornnetwork.org/hnn-content/uploads/UNICEF_Toolkit-for-Setting-Up-Special-Care-Newborn-Units-Stabilisation-Units-and-Newborn-Care-Corners.pdf.
Ministry of Health Tanzania. The national guideline for neonatal care and establishment of neonatal care unit. 2019. [cited 2023 Mar 12]. Available from: https://www.moh.go.tz/.
Ministry of Health and Family Welfare (MOH&FW) and UNICEF Bangladesh. Standard operating procedure (Sop) for newborn care services at primary and secondary level hospitals in Bangladesh. 2019. [cited 2022 Dec 10]. Available from: https://platform.who.int/docs/default-source/mca-documents/policy-documents/guideline/BGD-CC-37-01-GUIDELINE-2011-eng-BAN-SOP-Newborn-care-2012.pdf.
Ministry of Health and Sanitation and UNICEF. Setting up special care baby units in Sierra Leone. 2021. [cited 2022 Dec 15]. Available from: https://mohs.gov.sl/.
World Health Organization. Interagency list of priority medical devices for essential interventions for reproductive, maternal, newborn and child health. 2016. [cited 2022 Mar 10]. Available from: https://www.who.int/publications/i/item/9789241565028.
Penzias RE, Bohne C, Ngwala SK, Zimba E, Lufesi N, Rashid E, et al. Health facility assessment of small and sick newborn care in low- and middle-income countries: systematic tool development and operationalisation with NEST360 and UNICEF. BMC Pediatr. 2023.
Kirby RP, Molyneux EM, Dube Q, McWhorter C, Bradley BD, Gartley M, et al. Target product profiles for neonatal care devices: systematic development and outcomes with NEST360 and UNICEF. BMC Pediatr. 2023.
World Health Organization. Target product profile. 2022. [cited 2023 Mar 6]. Available on: https://www.who.int/observatories/global-observatory-on-health-research-and-development/analyses-and-syntheses/target-product-profile/who-target-product-profiles.
Asma E, Heenan M, Banda G, Kirby R, Mangwiro L, Acemyan CZ, et al. Avoid equipment graveyards: rigorous process to improve identification and procurement of effective, affordable, and usable newborn devices in low-resource hospital settings. BMC Pediatr. 2023.
Ministry of Health Community Development Gender Elderly and Children Tanzania. The national road map strategic plan to improve reproductive, maternal, newborn, child and adolescent health in Tanzania (2016 - 2020). 2016. [cited 2022 Dec 07]. Available from: https://www.moh.go.tz/.
Ministry of Health Tanzania. National plan for reproductive, maternal, newborn, child and adolescent health & nutrition (2021/2022 - 2025/2026). 2021. [cited 2022 Dec 01]. Available from: https://www.moh.go.tz/.
Medical Stores Department. Price cataloque 2022/2023. Tanzania: MSD; 2022. [cited 2023 Jan 31]. Available from: https://www.msd.go.tz/.
Tanzania national bureau of statistics. Population and housing census - preliminary report (2022). 2022. [cited 2023 Mar 12]. Available from: https://www.nbs.go.tz/index.php/en/census-surveys/population-and-housing-census.
Bollinger LA, Sanders R, Winfrey W, Adesina A. Lives Saved Tool (List) costing: A module to examine costs and prioritize interventions. BMC Public Health. 2017;17(S4).
Avenir Health. Onehealth tool. 2020. [updated 2022 May 6; cited 2023 Jan 12]. Available on: https://www.avenirhealth.org/software-onehealth.php.
Rajabi A, Dabiri A. Applying activity based costing (Abc) method to calculate cost price in hospital and remedy services. Iran J Public Health. 2012;41(4):100–7.
UNICEF. Oxygen System Planning Tool. 2020. Available on: https://www.unicef.org/innovation/oxygen-system-planning-tool. [cited 2022 Dec 28].
UNICEF. Oxygen System Planning Tool: Quick Reference Guide and Faq. 2020. [cited 2022 Dec 28]. Available on: https://www.unicef.org/innovation/media/13711/file/UNICEF%20Oxygen%20Planning%20Tool.pdf.
UNICEF Regional Office for South Asia. Investment case for newborn survival in South Asia. 2021. [cited 2023 Apr 21]. Available from: https://www.unicef.org/rosa/reports/investing-newborn-health-south-asia.
Bhutta ZA, Das JK, Bahl R, Lawn JE, Salam RA, Paul VK, et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost?. Lancet. 2014;384(9940):347–70.
Wong JQ, Haw NJ, Uy J, Bayani DB. Reflections on the use of the World Health Organization’s (WHO) Onehealth Tool: implications for health planning in low and middle-income countries (LMIC). F1000Research. 2018;7:157.
Nishimwe C, McHunu GG, Mukamusoni D. Community- based maternal and newborn interventions in Africa: systematic review. J Clin Nurs. 2021;30(17–18):2514–39.
Chisholm D, Lund C, Saxena S. Cost of scaling up mental healthcare in low-and middle-income countries. Br J Psychiatry. 2007;191(6):528–35.
Conteh L, Shuford K, Agboraw E, Kont M, Kolaczinski J, Patouillard E. Costs and cost-effectiveness of malaria control interventions: a systematic literature review. Value Health. 2021;24(8):1213–22.
Borghi J, Munthali S, Million LB, Martinez-Alvarez M. Health Financing at district Level in Malawi: an analysis of the distribution of funds at two points in time. Health Policy Plan. 2018;33(1):59–69.
Dingle A, Schäferhoff M, Borghi J, Lewis Sabin M, Arregoces L, Martinez-Alvarez M, et al. Estimates of aid for reproductive, maternal, newborn, and child health: findings from application of the Muskoka2 method, 2002–17. Lancet Glob Health. 2020;8(3):e374–86.
Pitt C, Grollman C, Martínez-Álvarez M, Arregoces L, Lawn JE, Borghi J. Countdown to 2015: An analysis of donor funding for prenatal and neonatal health, 2003–2013. BMJ Glob Health. 2017;2(2):e000205.
Kumar MB, Bath D, Binyaruka P, Novignon J, Lawn JE, Pitt C. Donor aid for newborns and stillbirths: analyses of levels, trends, and equity, 2002–19. Lancet Glob Health. 2023.
Bureau of Public Procurement and Federal Ministry of Health Nigeria. Policy for procurement of health and medical equipment, list of manufacturers and equipment for tertiary hospitals 2022–2024. 2022. [cited 2023 Jan 29]. Available from: https://www.bpp.gov.ng/wp-content/uploads/2022/07/APPROVED-POLICY-FOR-PROCUREMENT-OF-HEALTH-AND-MEDICAL-EQUIPMENT-LIST-OF-MANUFACTURERS-AND-EQUIPMENT-2022-2024.pdf.
Acknowledgements
We thank those involved as part of the multidisciplinary team led by the Ministry of Health Tanzania whose inputs provided data and helped to shape the tool. We are also grateful to organizations involved in the NEST360 alliance. Many thanks to the relevant administrative staff for their support. We are also very grateful to fellow researchers and guest-editors who peer-reviewed this paper, and for the input from the managing editors at BMC and within NEST360 including Caroline Noxon, Sarah Murless-Collins, and Joy E. Lawn.
About this supplement
This article has been published as part of BMC Pediatrics, Volume 23 Supplement S2, 2023: NEST360 Small and sick newborn care: learning for implementation across Africa and beyond. The full contents of the supplement are available at https://bmcpediatr.biomedcentral.com/articles/supplements/volume-23-supplement-2.
Funding
This work is funded through the NEST360 Alliance with thanks to John D. and Catherine T. MacArthur Foundation, the Bill & Melinda Gates Foundation, ELMA Philanthropies, The Children’s Investment Fund Foundation UK, The Lemelson Foundation, The Sall Family Foundation, and the Ting Tsung and Wei Fong Chao Foundation under agreements to William Marsh Rice University.
Author information
Authors and Affiliations
Contributions
The ABC device planning and costing tool was conceptualized by the NEST360 Alliance team, facilitated by JEL. All co-authors contributed to the design of the tool. AT with JEL, RRK and MO developed a detailed outline of the tool and concept for this paper. Clinical insights and context data from three countries to model default estimates in the tool were provided by GM, RK, DS, EG, SLM, CB and AM. Analysis was undertaken by AT in collaboration with MBK, TPJ and JEL. RK and KMP enabled the tool’s further development in MS Excel. DS, GM, RK, RK, AM and KMP, helped with tool refinement. AT, SMC, JEL and RKK collaborated on the first draft of the manuscript. All authors reviewed the tool and helped to revise the manuscript. All authors reviewed and agreed on the final version. The authors' views are their own, and not necessarily from any of the institutions they represent.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was received in each country from respective ethical review committees and the London School of Hygiene and Tropical Medicine ethics committee (no. 21892). The NEST360 Alliance data sharing agreement covered data sharing between sites. Where applicable, national data transfer agreements were acquired. No individual consent was required for the study.
Consent for publication
“Not applicable”.
Competing interests
Authors are inventors on patents for CPAP (MO, RRK) and for bilirubinometry (RRK) that have been licensed to 3rd Stone Design at zero percent royalty in GAVI eligible countries; these inventors have donated their share of all royalties to Rice University to support global health research and education. Remaining authors have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Adapted ISPOR Criteria for Cost(-Effectiveness) Review Outcome (CiCERO) checklist.
Additional file 2.
Review on planning and costing tools.
Additional file 3.
Review on type and quantity of neonatal devices.
Additional file 4.
ABC planning and costing tool for ward furniture and neonatal devices.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tarus, A., Msemo, G., Kamuyu, R. et al. Devices and furniture for small and sick newborn care: systematic development of a planning and costing tool. BMC Pediatr 23 (Suppl 2), 566 (2023). https://doi.org/10.1186/s12887-023-04363-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-023-04363-w