Abstract
Background
Globally more than 650,000 newborns died on their first day of life from birth asphyxia. The outcome of an asphyxiated newborn depends on the quality of care they received at birth. However, the quality of care newborns received at birth may be below the WHO resuscitation standard. The reason for the poor quality of care is unclear. The Donabedian model, according to the World Health Organization (WHO), is an appropriate framework for health care assessment that focuses on improving the quality of care. So this study aims to assess the quality of neonatal resuscitation, outcome, and its associated factors among newborns with birth asphyxia at public hospitals in the East Wollega zone, 2021.
Methods
An institution-based cross-sectional study was conducted to observe 410 asphyxiated newborns using consecutive sampling methods. Data was gathered using a pretested structured questionnaire and checklist. Epi-data version 3.1 was used to enter data, which was subsequently exported to Statistical Package for Social Sciences version 25 for analysis. A logistic regression model was employed to determine the variables associated with the outcome variable. The adjusted odds ratio with a 95% confidence interval was calculated, and all variables associated with the outcome variable with a p-value less than 0.05 in multivariable analysis were determined to be significant factors for the outcome of resuscitated newborns.
Result
A total of 410 asphyxiated newborns were included in this study with a response rate of 97%. From this 87.6% of resuscitated newborns survived. Keeping baby warm [AOR = 6.9; CI (3.1, 15.6)] is associated significantly with increased chances of survival while meconium presence in the airway [AOR = 0.26; CI (0.1, 0.6)], prematurity [AOR = 0.24; CI (0.12, 0.48)], and presence of cord prolapse [AOR = 0.08; CI (0.03, 0.19)] were factors significantly associated with decreased survival of resuscitated newborns at 1 h of life.
Conclusion
Newborns who were kept warm were more likely to survive compared to their counterparts. While the presence of meconium in the airway, preterm, and cord prolapse was associated with the decreased survival status of newborns. Facilitating referral linkage in the event of cord prolapse, counseling on early antenatal care initiation to decrease adverse outcomes (prematurity), and neonatal resuscitation refresher training is strongly recommended.
Similar content being viewed by others
Introduction
Worldwide, neonatal deaths account for about 4 million deaths with 99% of these happening in low- and middle-income nations [1, 2]. Furthermore, newborn mortality is still a major problem in most low- and middle-income countries (LMICs), with around 38% of all cases emerging from Sub-Saharan African countries. Ethiopia is one of the five countries responsible for half of the 2.6 million neonatal deaths worldwide in 2019. Birth asphyxia was responsible for about a quarter of these neonatal deaths [3,4,5]. Even though the mortality and morbidity from birth asphyxia may be preventable and treatable, birth asphyxia-related mortality still accounts for approximately quarter of neonatal mortality worldwide [6, 7].
Neonatal resuscitation is a set of techniques and life-saving interventions used to help newborns establish breathing and circulation at birth. Neonatal resuscitation includes different steps of establishing an airway, breathing, and sometimes circulation in the newborn with breathing difficulty [8, 9]. Simple investments in newborn resuscitation equipment supply and distribution, having Helping Babies Breathe (HBB) training is an important step to improve the survival of these babies from birth asphyxia [10,11,12]. It is anticipated that providing evidence-based service for all mothers and infant at the moment of birth in facilities may avert up to 531,000 stillbirths, 113,000 maternal deaths, and 1.3 million newborn deaths [13, 14].
Every year, 30 million infants require special or intensive newborn care in a hospital setting, requiring high-quality treatment at the appropriate time and in the right place to survive and thrive as members of society [14]. Resuscitation which is not performed in a timely and effective manner may be responsible for half of the 1.16 million neonatal deaths [15, 16]. Evidence from developing nations reveals that every 30 seconds delay in starting ventilation for up to the first 6 min increases the risk of death by 16%, and every minute delay in applying bag and mask ventilation (BMV) increases the risk of death by 6% [17]. To combat these problems high-quality resuscitation is very important [18, 19]. However, deaths from birth asphyxia occur due to a continuing lack of access to appropriate care in the hospital setting [19]. Also, research in low-income countries demonstrates that a high rate of infant mortality results from poor resuscitation given at birth [20].
Factors such as keeping the baby warm, suctioning before stimulation, mask ventilation, the ability to follow up labour properly, preparing equipment before delivery, with avoidance of meconium or prematurity, are the most effective factors associated with the survival of newborns [11, 21,22,23].
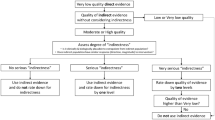
Even though effective neonatal resuscitation (NR) care has a role in reducing neonatal mortalities [24] still deaths occur as a result of poor quality of care given at birth [25]. Standardizing evaluations of clinical practices and infant services, who undergo resuscitation is currently needed to ensure quality care [10, 26]. To ensure this aim, many neonatal survival strategies including obstetric care and quality neonatal resuscitation in various contexts were established [5, 6, 27]. However, neonates with birth asphyxia still had a low survival rate, especially in a low resource setting [28]. Improved routine data collection focusing on quality of resuscitation and outcomes is required to accelerate progress [14]. The Donabedian model is one of the models recommended to assess the quality of care by WHO [29]. Three components of the model were used to assess the elements of quality of intrapartum care described as structure, process, and outcome [30]. The structure part was the human resource of the hospital, availability of equipment, and process part is neonatal resuscitation performed while survival or death of neonate is as an outcome of the study. So, this study aims to address quality neonatal resuscitation, its outcome, and associated factors by using the Donabedan model among resuscitated newborns with birth asphyxia at public hospitals in the East Wollega zone.
Methods
Study setting and design
From March 1 to June 30, an institution-based cross-sectional study was done at Wollega university referral hospitals, Nekemte specialized hospital, Gida Ayana district hospital, Jimma Arjo hospital, and Sire district hospitals in the East Wollega zone. During the study period, all asphyxiated newborns in public hospitals in the East Wollega zone were included, while congenital anomalies incompatible with life, mothers of newborn babies receiving opioids, and other depressive drugs were excluded.
Sampling and data collection
The sample size was estimated using the single population proportion formula, taking into account the following factors: The population proportion (P) is 50%, the confidence interval is 95%, the margin of error is 5%, and the response rate is 10%. As a result, 422 asphyxiated neonates from all governmental hospitals in the research area were evaluated. The previous 4 months’ data of asphyxiated newborns of all hospitals from the delivery registration book were observed as follows. The delivery registration book at the relevant institutions (Wollega University Referral Hospitals (102), Nekemte Specialized Hospital (121), Gida Ayana (88), Sire (80), and Arjo (85) revealed a total of 476 deliveries. The computed sample size was allocated proportionally for each hospital based on these data. Seventy-eight (78), seventy-five (75), and seventy-one (71) asphyxiated babies were observed from Nekemte specialized hospital, ninety-one (91) from Wollega University referral Hospital, and seventy-eight (78) from Gida Ayana, Arjo, and Sire district hospitals, respectively. Then, until the desired sample size was reached, asphyxiated newborns were observed consecutively.
Variables of the study
The Donabedian domains of structures and processes were the focus of the elements influencing the infant outcome. “Yes = 1” and “no = 0” were used to construct the independent process variables. The four sections of the NR process were used to categorize process variables. Drying/stimulation (drying, removing wet cloth, and keeping baby warm) airway maintenance (checked airway, suctioning, positioning baby’s head) bag and mask breathing, and possible cardiac resuscitation. NR equipment availability, health care professional characteristics such as training/qualifications and experience, and NR training were used to assess structural factors. The newborn’s survival status at 1 hour was the primary outcome. The outcome was either alive or dead [30, 31]. The outcome variable, survival or death of neonate was recorded starting from delivery time to till one hour post-partum. Newborns who survived past 1 h after delivery were recorded as survived and death was recorded as it was confirmed by physicians immediately after noting the time of death within 1 h of life. Newborns transferred to the neonatal intensive care unit (NICU) within 1 h for further care were evaluated at NICU by a neonatal nurse and death were immediately recorded and reported.
Study instrument and measurement
The data collection tool was developed and modified from a variety of studies undertaken in developing countries and then contextualized to Ethiopia [23, 32, 33]. The tool was then translated into Afan Oromo, the working language, and then retranslated back to English for consistency. These tools were divided into three parts: socio-demographic characteristics of the provider, a neonatal resuscitation process checklist, and neonatal-related data. First, at the delivery site where neonatal resuscitation is conducted is observed for equipment, and a checklist was used to check the neonatal resuscitation procedure. 10 data collectors, five BSc nurses and five BSc midwives were recruited for data collection, two BSc nurses supervised the total data gathering activity.
Operational/term definitions
Keeping baby warm is defined as sampling wrapping with cloth after drying and stimulation by placing near radiant heater.
Birth asphyxia in this context was defined as failure to initiate and sustain breathing at birth [16].
Prematurity: newborns with a gestational age of 28 weeks of gestation to 37 weeks of gestation.
Term: newborns with the gestational age of 37 weeks to 42 weeks.
Previous training: Any types of neonatal resuscitation training taken previously past 6 months.
Data quality control
Before the commencement of data collection for the study, a pilot was conducted in Bako hospital on 5% of the sample size to identify unclear phrasing and any uncertainty in the understanding of data collection instruments. The Chronbach alpha was determined to be 0.76. After the pretest, the Apgar score was modified to one, five, and 10 min. Additionally, data collectors and supervisors provided 2 days of training on how to obtain verbal consent, as well as informed consent from a mother under the age of 18, maintain confidentiality, and respect the rights of participants, as well as study purpose, methodology, how to conduct the interview, and how to observe the resuscitation process, including how to assess the Apgar score. 10 BSc (5 nurses and 5 midwifes) served as data collectors. To reduce bias during observation of neonatal resuscitation procedures, health care professionals were observed by B.Sc. nurses while performing resuscitation, but occasionally recruited midwives working in delivery rooms also collected data to reduce the hawthorn effect, which means that when data collectors were from other sites, they tried to perform resuscitation well because they knew they were under observation. The hawthorn effect was minimized when data collectors were viewed by a member of their team since they perform the technique as standard treatment. Furthermore, data collectors are constantly present in the labor ward to observe health care providers’ usual practices in the delivery room. To ensure the completeness, accuracy, and consistency of information collected during data collection, the supervisors supervise data collectors twice a week, and in the meantime, the principal investigator went to the hospitals and double-checked proper data collection.
Data analysis
Gathered data was then entered into Epidata version 3.1 before being exported to SPSS version 25 for further analysis. Data were cleaned, edited, categorized, and outliers were removed and prepared to be presented in the form of a table, chart, and percentage before analysis. To find factors that have been associated with the outcome variable, a logistic regression analysis was used. Factors that were associated with the outcome variable at a 25% (P-value ≤0.25) significant level in the bivariable analysis were prepared for final multivariable analysis after multicollinearity was checked with variance inflation factors, as well as backward logistic regression analysis was used to control confounding. In addition, model fitness was done by the Hosmer-Lemeshow goodness of fit test with a cut point of 0.5. Adjusted odds ratios (AOR) with 95% confidence intervals were computed and statistical significance was declared when it is significant at a 5% level (p-value < 0.05).
Results
Structural factors
Health care Provider’s background characteristics
A total of 75 health care professionals (HCP), with a mean age of 28.2 years gave care to the newborns. More than half of them, 39 (52%) were men. Midwives were the most common care providers of neonatal resuscitation, accounting for more than two-thirds, 61(84.4%) of the respondents. Nearly half of HCPs, 39 (52%) said they have ever attended NR training (Table 1).
Health facility characteristics
The resuscitation area had guidelines posted. All of the fundamental NR equipment is available in the delivery pack, suction devices such as (electric-powered suction machine and suction bulbs), term face masks (size = 1), and one clean dry towel for cleaning the newborn. The delivery room, on the other hand, lacked a wall clock and a flip chart that showed the procedure clearly.
Process factors
Overall neonatal Resuscitation processes performed
Drying or stimulation
The majority of babies, 338 (82.4%), were gently dried by massaging their backs with a dry towel. The wet cloth was removed from 347 (84.6%) of the neonates that were resuscitated, and 365 (89%) of the newborns were wrapped in a cloth to keep them warm.
Checked airway
More than two-thirds of newborns who did not respond to airway secretion stimulation had their airways checked and cleared. In 240 (58.5%) of the infants, meconium was found in the airway. In 230 (56%) of neonates with meconium present, proper head positioning to clear the airway was seen.
Bag and mask ventilation
Bag and mask ventilation (BMV) (n = 164) was initiated for all newborns who did not respond after airway clearance. However, of the babies who received BMV, 128 (78%) started ventilation within the first minute. The median time for BMV to start was 30 seconds (SD =29.2). All newborns who did not respond to initial bag and mask ventilation (n = 96) were initiated subsequent BMV.
Advanced care
Among newborns who received advanced care (n = 57), chest compressions with successful breaths were given to 54 (94.7%) neonates while 39 (68.4%) of them received supplemental oxygen. Adrenaline was administered in 9 (15.9%) newborns who needed advanced resuscitation (Table 2).
Outcome factors
General characteristics of newborns resuscitated
Nearly half of the neonates 222 (54.1%) who were resuscitated were females, with spontaneous vertex delivery (SVD) accounting for 227 (55.4%) of the deliveries. The median birth weight was 3500 g (SD 508.85). While 302 (73.7%) of the babies were over 37 weeks of gestational age. At 1, 5, and 10 minutes, the mean Apgar score was 5.5, 5.9, and 6.8 respectively (Table 3).
Final outcome of resuscitated newborns
The study revealed that among asphyxiated newborns undergoing neonatal resuscitation 359 (87.6%) of them survived the first hour of life (Fig. 1).
Factors associated with neonatal resuscitation outcome
Multivariable logistic regression analysis was conducted with those variables with p values < 0.25 in bivariable logistic regression analysis. Accordingly keeping the baby warm, absence of meconium in the airway, increased gestational age, and absence of cord prolapse were significantly associated with the survival of the newborn at 1 h of life.
Newborns kept warm (AOR, 95%CI; 6.9(3.1, 15.6)) were 6.9 times more likely to survive in comparison to those not kept warm. Newborns with meconium presence in the airway (AOR, 95%CI; 0.26(0.1,0.6)) had 26 times higher odds of death compared to counter parts. A premature infant (AOR, 95%CI; 0.24(0.12, 0.48)) is 76%less likely to survive compared to a term infant. Also, this study found that newborns with cord prolapse (AOR, 95%CI; 0.08(0.03, 0.19)) were 92% less likely to survive compared to those with no cord prolapse (Table 4).
Discussion
The goal of this study was to evaluate the quality of neonatal resuscitation and its outcomes and factors associated with mortality/survival at public hospitals in the East Wollega zone of Oromia, Western Ethiopia, in 2021. Among 410 newborns resuscitated, 359 (87.6%), [CI = 84.1, 90.7] survived the first hour of life. This result was similar to 87.7% survival found in a study conducted in northern Tanzania, [34], and 86.7% in South Africa [35]. Also supported by an 86.2% success rate in an institution-based study in Kenya on the practice and outcome of neonatal resuscitation among newborns with birth asphyxia [11]. However it was higher than a study conducted in Iran which reported 76.6% survival [36], but lower than the studies conducted in Tanzanian rural hospitals (93.6%) [6] and sub-Saharan Africa (90.9%) [37]. This variation may be due to the difference in design and sample size of the study conducted in these countries.
Survival of asphyxiated newborns after resuscitation may be affected by structural factors such as health care professional characteristics (year of experience, and previous training), availability of important equipment in the institution to give care as well as process factors such as the effective implementation of neonatal resuscitation procedure [29, 38, 39].
This study also revealed that some neonatal resuscitation equipment or materials such as availability of resuscitation guidelines (flow chart), and clock were absent in participating resuscitation areas. Absence of such equipment affects quality of resuscitation care given as well as neonatal outcome. Also study findings from low and middle-income countries demonstrate that facilities equipped to give better care to newborns improves the outcome of newborns with difficulty in breathing [40, 41].
Health care professionals performing neonatal resuscitation should be trained and sufficiently skilled to deliver quality care for newborns [40, 42, 43]. This study revealed that nearly half of HCP had no any type of previous training for neonatal resuscitation, nearly half of them had a duration of practice greater than 2 years, and more than one-third had a duration of more than 1 year of current training. Other studies have reported that health care professionals having any type of NR training compared to those not having it all, longer duration of practice, short duration of the training, or having immediate refresher training less than 6 weeks were associated with given better quality resuscitation for asphyxiated newborns [31, 43].
Proper resuscitation practice were linked to improved neonatal outcome. Greater attention to care given has proven to have a beneficial impact on the survival of newborns. Keeping a baby warm [AOR = 6.9; 95% CI (3.1, 15.6)], is one of the factors significantly associated with the survival of newborns at 1 h of life, which was similar to studies conducted in Kenya [11] and Sub-Saharan Africa [44]. This may be because keeping the baby warm reduces the risk of neonates developing hypothermia and is associated with improved survival of newborns. However, this study reports some health care professionals perform stimulation before suctioning. But, suctioning should be done before stimulation in case the airway is obstructed. This health care professional practice also contradicts different resuscitation guidelines [16, 39].
Also, this study reported that BMV was initiated for all newborns who did not respond after airway clearance. Subsequent BMV was continued in more than two-thirds. However, of the babies who needed assistance, one-third did not start ventilation within the first minute after birth. Immediate intervention within the first minute potentially reduces hypoxia and related complications. The practice of health care professionals in the first minute initiation was poor in this study. A delay in the application of BMV is associated with poorer neonatal outcomes due to decreased oxygen supply. This is revealed by several international studies [17, 28].
Among newborns who needed advanced care, chest compressions with successful breaths were given to neonates with supplemental oxygen. Newborns who got advanced care after application of continuing BMV had better outcomes to assist breathing and circulation. If breathing and circulation is not maintained after initial BMV, the newborn may end up with severe asphyxia and related complications [39]. However, this study reported that the majority of the newborn’s received chest compression rather than receiving subsequent BMV to support ventilation. This is contrary to different resuscitation guidelines [16, 39]. This misapplication of skills may worsen rather than improving the outcome. This may be due to nearly half of health care professionals in the study area having no training in neonatal resuscitation.
This study found that Premature infants (gestational age less than 37 weeks) [AOR = 0.24; 95% CI (0.12, 0.48)] were 76% less likely to survive than those with a gestational age of greater than 37 weeks. This is supported by the study conducted in Gonder [45], and Tanzania [6]. But contradicts studies from South Africa [35] and Nigeria [46]. This discrepancy may be due to differences in the care of premature newborns or the different setup of resuscitation areas.
The present study also found that newborns with the presence of meconium-stained liquor [AOR = 0.26; 95% CI (0.12, 0.57)], in the airway had reduced chances of survival within the first hour of life. This agreed with outcomes reported in Kenya [11], South Africa [35], India [47], and brazil [48]. This is may be due to meconium presence in the airway blocking air entry which leads to blockage of the airway resulting in the death of newborns.
The study found that newborns with Cord prolapse [AOR = 0.08; 95% CI (0.03, 0.19)] had 92% less likely to survive compared to those with no cord prolapse. Another study also reported cord prolapse as an independent risk factor for neonatal mortality [22]. The possible reason will be due to interference in blood supply to newborns while delivery which in turn decreases the oxygen supply to newborns resulting in hypoxia. The present study shares limitations of the cross-sectional study [22]., as well as limitations of the Donabedian model in which sociodemography is not considered as the main variable. The study also measures the survival of neonates at 1 h. But several studies measures neonatal mortality at 24 hours, 7 days and at 1 month. So this study may underestimate actual newborn survival.
Conclusion
At 1 h after being resuscitated, 87.6% of resuscitated neonates survived birth asphyxia. Keeping the baby warm was a factor that was associated with increased chances of survival while meconium presence in the airway, being premature, and having cord prolapse were all associated with a decreased chance of survival from birth asphyxia within the first hour of life. In comparison to other research, survival of resuscitated newborns is still poor after a short length of time. Health practitioners working in antenatal care clinics and labor and delivery wards should receive training to improve their resuscitation skills as well as the ability to recognize and detect early problems such as cord prolapse that affect the prognosis of resuscitated neonates. To intervene in cases of cord prolapse, strengthen formal referral links with peripheral health services. To avoid missing the neonatal resuscitation procedure steps, focus on following the neonatal resuscitation process guideline and charts accessible in resuscitation areas. More research on newborn resuscitation outcomes is needed, with a case-control study design being used to measure better neonatal resuscitation outcomes.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- EDHS:
-
Ethiopian Demographic Health Survey
- FDRE:
-
Federal Democratic Republic of Ethiopia
- FANC:
-
Focused Antenatal Care
- HBB:
-
Helping Baby Breath
- HCP:
-
Health Care Professional
- IMNCI:
-
Integrated Management of Newborn and Child Hood Illness
- MCNH:
-
Maternal Child and Neonatal Health
- MAS:
-
Meconium Aspiration Syndrome
- NICU:
-
Neonatal Intensive Care Unit
- NRFHRP:
-
None Reassuring Fetal Heart Rate pattern
- PPV:
-
Positive pressure ventilation
- SPSS:
-
Statistical Package for Social Science
- WHO:
-
World Health Organization
References
Lee AC, Waiswa P, Lalli M, Bhutta PZ, Barros AJ, Christian P, et al. Every newborn: progress, priorities, and potential beyond survival. Lancet (London, England). 2014;384(9938):189–205.
World Health Organization. World health statistics 2018: monitoring health for the SDGs, sustainable development goals. World Health Organization; 2018. https://apps.who.int/iris/handle/10665/272596.
Ethiopian Public Health Institute (EPHI) [Ethiopia] and ICF. Ethiopia Mini demographic and health survey:key indicators. Rockville: EPHI and ICF; 2019.
Abdurashid N. Prevalence of Birth Asphyxia and Associated Factors among Neonates Delivered in Dilchora Referral Hospital, in Dire Dawa, Eastern Ethiopia Clinics in Mother and Child Health. 2019;(March).
Mekonnen Y, Tensou B, Telake DS, Degefie T, Bekele A. Neonatal mortality in Ethiopia : trends and determinants. BMC Public Health. 2013;13(1):1.
Village EG. Birth Asphyxia : a major cause of early neonatal mortality in a Tanzanian Rural Hospital; 2012.
WHO. Every newborn: an action plan to end Preventable deaths: Executive summary. Geneva: World Health Organization. Who, Unicef; 2014. p. 12.
Textbook of Neonatal Resuscitation. 2006, American Academy of Pediatrics, 5
Organization WH. WHO technical specifications of neonatal resuscitation devices. Geneva: World Health Organization. Available from: https://apps.who.int/iris/handle/10665/206540
Tariq A. Journal of neonatal biology perinatal Mortality : a dissection of social myths. Socioeconomic Taboos and Psychosocial Stress. 2012;1(2):2–5.
Shikuku DN, Milimo B, Ayebare E, Gisore P, Nalwadda G. Practice and outcomes of neonatal resuscitation for newborns with birth asphyxia at Kakamega County General Hospital, Kenya: a direct observation study. BMC Pediatr. 2018;18(1):167. https://doi.org/10.1186/s12887-018-1127-6.
Haile-Mariam A, Tesfaye N, Otterness C, Bailey PE. Assessing the health system’s capacity to conduct neonatal resuscitation in Ethiopia. Ethiop Med J. 2012;50(1):43–55.
Kuruvilla S, Bustreo F, Kuo T, Mishra CK, Taylor K, Fogstad H, et al. The Global strategy for women’s, children’s and adolescents’ health (2016–2030): a roadmap based on evidence and country experience. Undefined. 2016;94(5):398–400.
World HealthOrganization. Survive and thrive: transforming care for every small and sick newborn. World Health Organization; 2019. https://apps.who.int/iris/handle/10665/326495.
World Health Orgnatization. Africa ’ s newborns – counting them and making them count. Geneva: World Health Orgnatization; 2010. Available from: https://www.google.com/url?esrc=s&q=&rct=j&sa=U&url=https://pmnch.who.int/docs/librariesprovider9/meeting-reports/opportunities-for-africa-s-newborn.pdf%3Fsfvrsn%3D8861b8a8_1%26download%3Dtrue&ved=2ahUKEwiK17SZm9_6AhWP_7sIHX3nDQ4QFnoECAoQAg&usg=AOvVaw2Ra68bQE0Hc0hVy6osP9tx.
WHO. Guide line on basic newborn Resuscitation. Geneva: World Health Organization; 2012.
Langli H, Mduma E, Svensen E, Perlman JM. Early initiation of basic resuscitation interventions including face mask ventilation may reduce birth asphyxia related mortality in low-income countries a prospective descriptive observational study. J Resusc. 2012;83(7):869–73.
Mukhtar-Yola M, Audu LI, Olaniyan O, et al. Decreasing birth asphyxia:utility of statistical process control in a low-resource setting. BMJ Open Quality. 2018;7(3):e000231. https://doi.org/10.1136/bmjoq-2017-000231.
Lawn JE, Manandhar A, Haws RA, Darmstadt GL. Health Research Policy and Systems Reducing one million child deaths from birth asphyxia – a survey of health systems gaps and priorities, vol. 10; 2007. p. 1–10.
Opiyo N, English M. In-service training for health professionals to improve care of seriously ill newborns and children in low-income countries. Cochrane Database Syst Rev. 2015;13(5):CD007071. https://doi.org/10.1002/14651858.CD007071.pub3.
Moshiro R, Ersdal HL, Mdoe P, Kidanto HL. Factors affecting effective ventilation during newborn resuscitation : a qualitative study among midwives in rural Tanzania. Glob Health Action. 2018;11(1):5–6.
Salustiano EM, Campos JA, Ibidi SM, Ruano R, Zugaib M. Low Apgar scores at 5 minutes in a low risk population: maternal and obstetrical factors and postnatal outcome. Rev Assoc Med Bras. 2012;58(5):587–93.
Yadav S, Shah GS, Poudel P, Mishra OP. Risk factors for adverse outcome in asphyxiated new born in Eastern Nepal. Int J Community Med Public Heal. 2016;3(6):1419–23.
Lulu C, Plotkin M, Currie S, Ugwi P, Louis H, Winani K, et al. Improvements in newborn care and newborn resuscitation following a quality improvement program at scale : results from a before and after study in Tanzania improvements in newborn care and newborn resuscitation following a quality improvement program at s. 2014;
Velaphi S, Rhoda N. Reducing neonatal deaths in South Africa - are we there yet, and what can be done? SAJCH South African J Child Heal. 2012;6(3):67–71.
Dalili H, Sheikh M, Hardani AK, Nili F, Shariat M. Comparison of the combined versus conventional apgar scores in predicting adverse neonatal outcomes; 2016. p. 1–11.
Tolessa BE. Factors determining neonatal mortality in Ethiopia and interventions to improve neonatal health; 2015.
Gobezie WA, Bailey P, Keyes E, Ruano AL, Teklie H. Readiness to treat and factors associated with survival of newborns with breathing difficulties in Ethiopia. BMC Health Serv Res. 2019;19(552):1–10.
WHO. Standards for improving quality of maternal and newborn care in health facilities. Geneva: World Health Organization; 2016. Available from: https://cdn.who.int/media/docs/default-source/mca-documents/qoc/quality-of-care/standards-for-improving-quality-of-maternal-and-newborn-care-in-health-facilities.pdf?sfvrsn=3b364d8_4.
Donabedian A. The quality of care: how can it be assessed? JAMA. 1988;260(12):1743–8.
Shikuku DN, Milimo B, Ayebare E, Gisore P, Nalwadda G. Practice and outcomes of neonatal resuscitation for newborns with birth asphyxia at Kakamega County General Hospital, Kenya : a direct observation study. BMC Pediatr. 2018;18(167):1–11.
MOH. Basic Paediatric protocols for ages upto 5 years - revised (Republic of Kenya): Government of Kenya; 2013. p. 38–9.
Annan GN, Asiedu Y. Predictors of neonatal deaths in Ashanti region of Ghana: a cross-sectional study. Adv Public Heal. 2018;2018:1–11.
Simiyu IN, Mchaile DN, Katsongeri K, Philemon RN, Msuya SE. Prevalence, severity and early outcomes of hypoxic ischemic encephalopathy among newborns at a tertiary hospital, in northern Tanzania. BMC Pediatr. 2017;17(1):1–7.
Padayachee N, Chb MB, Sa DCH, Ballot DE, Bch MB, Sa F. Outcomes of neonates with perinatal asphyxia at a tertiary academic hospital in Johannesburg, South Africa. 2014;(January).
Afjeh SA, Sabzehei MK, Esmaili F. Neonatal resuscitation in the delivery room from a tertiary level hospital: risk factors and outcome. Iran J Pediatr. 2013;23(6):675–80.
de Graft-Johnson J, Vesel L, Rosen HE, Rawlins B, Abwao S, Mazia G, et al. Cross-sectional observational assessment of quality of newborn care immediately after birth in health facilities across six sub-Saharan African countries. BMJ Open. 2017;7(3):e014680. https://doi.org/10.1136/bmjopen-2016-014680.
Biswas A, Ho SKY, Yip WY, Kader KBA, Kong JY, Ee KTT, et al. Singapore Neonatal Resuscitation Guidelines 2021. Singapore Med J. 2021;62(8):404–14. https://doi.org/10.11622/smedj.2021110.
Fawke J, May P. Newborn resuscitation and support of transition of infants at birth guidelines authors key points; 2021.
Weldearegay HG, Abrha MW, Hilawe EH. Quality of neonatal resuscitation in Ethiopia : implications for the survival of neonates; 2020. p. 1–9.
Woldu Abrha M, Gebreegziabher Gebru E, Weldemariam S, Gebrehiwot Weldearegay H. Exploring Factors Influencing Practice of Neonatal Resuscitation with Bag and Mask in Ethiopia: Analysis from 2016 National Emergency Obstetric and Newborn Care Survey. J Multidiscip Healthc. 2020;13:471–6. https:// doi. org/ 10. 2147/ JMDH. S2463 47.
Yoon SJ, Lim J, Han JH, Shin JE, Eun HS, Park MS. Impact of neonatal resuscitation changes on outcomes of very - low - birth - weight infants. Sci Rep. 2021:1–8. Available from: https://doi.org/10.1038/s41598-021-88561-5.
Bang A, Patel A, Bellad R, Gisore P, Goudar SS, Esamai F, et al. Helping Babies Breathe ( HBB ) training : What happens to knowledge and skills over time ? BMC Pregnancy Childbirth. 2016:1–12. Available from: https://doi.org/10.1186/s12884-016-1141-3.
Penfold S, Willey BA, Schellenberg J. Newborn care behaviours and neonatal survival: evidence from sub-Saharan Africa. Trop Med Int Heal. 2013;18(11):1294–316.
Yismaw AE, Tarekegn AA. Proportion and factors of death among preterm neonates admitted in University of Gondar comprehensive specialized hospital neonatal intensive care unit, Northwest Ethiopia. BMC Res Notes. 2018;11(1):867. Available from. https://doi.org/10.1186/s13104-018-3970-9.
Uleanya N, Aniwada E, Ekwochi U. Short term outcome and predictors of survival among birth asphyxiated babies at a tertiary academic hospital in Enugu , South East , Nigeria Short term outcome and predictors of survival among birth asphyxiated babies at a tertiary academic hospital in En. 2019;(May).
Saranappa SB, Nair CC, Madhu GN, Srinivasa S, Manjunath MN. Clinical profile and outcome of perinatal asphyxia in a tertiary care centre. Curr Pediatr Res. 2015;19:9–12.
Almeida MFB, Kawakami MD, Moreira LMO, Santos RMVD, Anchieta LM, Guinsburg R. Early neonatal deaths associated with perinatal asphyxia in infants ≥2500g in Brazil. J Pediatr (Rio J). 2017;93(6):576–84. https://doi.org/10.1016/j.jped.2016.11.008.
Acknowledgments
I am grateful to Research Directorate Office, Wollega University, for their cooperation. I want to thank Wollega university teaching hospital, Nekemete specialized hospital, Gida hospital, Arjo, and Sire hospital administration for their valuable support in providing necessary data. Finally, I want to thank data collectors and all study participants who participated in this research for their willingness to participate in the study.
Funding
The authors received no funding for this study.
Author information
Authors and Affiliations
Contributions
NM conceived the idea, drafted the proposal, analyzed collected data, prepared the final manuscript for publication, and read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the Institutional Review Board (IRB) of Wollega University, institute of health with a reference number of IHRWU\2012\2021. Then an official letter of support was written to East Wollega zone respective hospitals. Moreover, all the methods were performed following the relevant guidelines and regulations (Declaration of Helsinki). The study’s objective, benefits, and risks were explained to the participants before data collection and obtained written informed consent from all respondents. Also written informed consent was taken from parents of mother’s age below 18 years old. The study participants were assured of the attainment of confidentiality, and the information they give us will not be used for any purpose other than the study.
Consent for publication
Not applicable.
Competing interests
The author declare that he has no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Guta, N.M. Application of Donabedian quality-of-care framework to assess quality of neonatal resuscitation, its outcome, and associated factors among resuscitated newborns at public hospitals of East Wollega zone, Oromia, Western Ethiopia, 2021. BMC Pediatr 22, 605 (2022). https://doi.org/10.1186/s12887-022-03638-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-022-03638-y