Abstract
Background
Studies have shown that overweight and obesity conditions tend to be stable from childhood and adolescence to adulthood. Unfortunately, little is known about the evolution of abdominal obesity during childhood. The aim of this study was to evaluate the temporal variations and risk of general and abdominal obesity between 4, 6, and 9 years of age.
Methods
Measurements of children in the ELOIN study taken at the three follow-ups of 4, 6, and 9 years of age were included (N = 1,902). Body mass index and waist circumference were recorded via physical examination. General obesity was determined according to the criteria of the World Health Organization (WHO) and abdominal obesity according to the cut-off points proposed by the International Diabetes Federation (IDF). Prevalence ratios (PRs) were estimated by sex and family affluence using generalized estimating equation models and relative risks (RRs) of obesity were obtained via Poisson regression.
Results
The prevalence of general obesity was 5.1%, 9.1%, and 15.6% at 4, 6, and 9 years, respectively, yielding a PR of 3.05 (95%CI: 2.55–3.60) (9 years old relative to 4 years). The prevalence of abdominal obesity was 6.8%, 8.4%, 14.5% at 4, 6, and 9 years, respectively, and the PR was 2.14 (95%CI: 1.82–2.51) (9 years old relative to 4 years). An inverse correlation was observed between both general and abdominal obesity and socioeconomic status. Among participants with general or abdominal obesity at 4 years of age, 77.3% and 63.6% remained in their obesity classification at 9 years, respectively, and 3.4% and 3.5% presented general or abdominal obesity also at 6 and 9 years of age, respectively. The RRs of general and abdominal obesity at 9 years were 4.61 (95%CI: 2.76–7.72) and 4.14 (95%CI: 2.65–6.48) for children classified with obesity at 4 years of age, increased to 9.36 (95%CI: 7.72–11.35) and 9.56 (95%CI: 7.79–11.74) for children who had obesity at 6 years, and up to 10.27 (95%CI: 8.52–12.37) and 9.88 (95%CI: 8.07–12.11) for children with obesity at both 4 and 6 years, respectively.
Conclusions
General and abdominal obesity begin at an early age and increase over time, showing an inverse correlation with socioeconomic status. In addition, general and abdominal obesity at 9 years are strongly associated with being classified with obesity at 4 and 6 years, so preventive interventions should be established at very early ages.
Similar content being viewed by others
Background
Childhood obesity is a major public health problem in many countries [1]. Worldwide, 124 million children and 213 million children and teenagers between 5 and 19 years of age have been estimated to present obesity and overweight in 2016 [2], respectively. In Europe, the prevalence of overweight and obesity during childhood is high, with large variations between regions. A substantially higher prevalence has been observed in the Mediterranean countries, including Spain [3]. The estimated prevalence of overweight and obesity among the Spanish population aged 6 to 9 years in 2019 was 23.3% and 17.3%, respectively [4], and the prevalence of abdominal obesity in the Spanish population aged 3 to 11 years was between 21 and 26% in 2016 [5].
General obesity (GO) in childhood has been associated with higher blood pressure, myocardial dysfunction, dyslipidemia, insulin resistance, fatty liver, stigmatization, and poor school performance [6, 7]. Its tendency to persist over the years entails a greater risk of comorbidities in adulthood [8]. GO is frequently defined based on the body mass index (BMI), a parameter easy to calculate that helps diagnose overweight and obesity as well as their associations with mortality or morbidity [9, 10]. However, the use of BMI has limitations [11] since it does not allow for differentiating between lean and fat body mass and does not provide information on regional body fat distribution [12]. In children, the relationship between BMI and fat body mass varies with age and sex and must be compared with standard or reference populations [13].
Studies have shown that the waist circumference (WC), which is widely employed to define abdominal obesity (AO), is strongly associated with cardiometabolic risk factors and risk of chronic disease [14]. WC in childhood is considered an important predictor of cardiometabolic disorders, independently of BMI values [15].
In general, GO tends to appear at an early age and persists over time. Children with overweight/obesity are more likely to continue having obesity during their adolescence and adulthood. Tracking of BMI values and obesity during childhood has been well documented [16, 17]. Nevertheless, not much is known about the stability (i.e. tracking) of the AO during childhood, presumably because WC is not routinely measured in primary-care pediatric programs. Research increasingly suggests that combined measurements of BMI and WC could be a supplementary approach to detect weight fluctuations during childhood and determine the main relevant risk factors [18, 19].
The aim of this longitudinal study with a 5-year follow-up was to examine the evolution and tracking of GO and AO in the pediatric population at 4, 6, and 9 years of age and to estimate the risk of GO and AO at 9 years old relative to previous GO or AO occurrences.
Methods
Study design and participants
The Longitudinal Childhood Obesity Study (ELOIN for its acronym in Spanish) is a population-based cohort study in the Madrid region (6.7 million population), whose methods have been previously published [20].
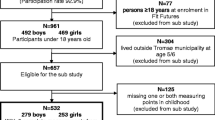
The sample size was calculated to be 3,000 children of 4 years of age at the baseline, assuming a prevalence of overweight/obesity of 12% and a precision level of about ± 2%. A total of 2,901 4-year-old children were finally recruited at the baseline. Of them, 1,902 participants were included in the present analysis that underwent three physical examinations for the recording of anthropometric measurements: the 4-year-old baseline measurements during 2012–2013, the 6-year-old follow-up during 2014–2015, and the 9-year-old follow-up during 2017–2018. The information was collected in two consecutive stages: 1) standardized physical examinations performed in the health center by pediatricians and primary care nurses of the sentinel network; and 2) completion of a structured questionnaire answered by the parents through a computer-assisted telephone interview (CATI) for the collection of data on sociodemographic variables and lifestyle.
Anthropometric measurements
The main outcome variables were abdominal obesity, measured via the WC, and general obesity, assessed with the BMI. Weight was measured with a digital scale (SECA® model 220, precision 0.1 kg), height was recorded using a telescopic stadiometer (SECA® model 220, precision 1 mm), and WC was obtained with an inextensible, locking, standardized measuring tape placed horizontally just above the iliac crest without tissue compression. All measurements were taken twice for each participant, and the mean of the two values was used for the analyses.
BMI (kg/m2) was adjusted by age (months) and sex according to the standardized tables of the WHO-2007 [13]. After obtaining BMI z-scores, normal weight was defined as zBMI ≤ 1 standard deviation (SD), overweight as 1 SD < zBMI ≤ 2 SD, and GO as zBMI > 2 SD [14]. WC was standardized by age (months) and sex based on reference tables of the International Diabetes Federation (IDF) for the consensus definition of metabolic syndrome. AO was defined setting the cut-off point at ≥ 90th percentile [21].
Four trajectories were defined based on the persistence or variation in obesity at 4, 6, and 9 years: 1) Stable without obesity: no obesity at any of the measurements; 2) Remitting obesity at 9 years: obesity at 4 and/or 6 years, but without obesity at 9 years; 3) Incidental obesity at 9 years: obesity only at 9 years, or at 4 and 9 years, or at 6 and 9 years; and 4) Stable with obesity: obesity at all three measurements. The same trajectories were used to assess changes in both GO and AO.
Covariates
The included sociodemographic variables, which were recorded at the baseline measurement of 4 years of age, were sex, age (months), and the household affluence estimated by the Family Affluence Scale (FAS) [22]. The FAS is a measure of family wealth and assets developed as an indicator of global socio-economic status. The FAS evaluates the following four items: ownership of a family car (0, 1, 2 or more), own bedroom (no = 0, yes = 1), family holidays during the past 12 months (0, 1, 2, 3 or more), and family computer(s) (0, 1, 2, 3 or more). The scores from these items are combined to produce a single index ranging from 0 (low affluence) to 9 (high affluence). The socio-economic status of respondents was classified as low (0–3 points), medium (4–5), or high (6–9), which is a categorization used in previous studies [23, 24].
Ethics
The Ethics Committee of the University Hospital Ramón y Cajal in Madrid approved the study (CIHURC- 122/11). Prior to their participation in the current study, all participants provided written informed consent. Written informed consent was obtained from the parents or legal guardians before participation in the ELOIN study.
Data analysis
An initial descriptive analysis was performed where the quantitative variables were summarized by their mean (SD) and the qualitative variables by percentages. Non-parametric tests were employed to determine whether the results reached statistical significance. Specifically, the Wilcoxon test was used for comparing two means while the Kruskal–Wallis test was used in cases where more than two means were compared.
The flow diagrams were represented in the form of Sankey diagrams to facilitate the visual interpretation of the tracking. The prevalence ratios (PRs) were calculated using generalized estimating equation (GEE) models under a binomial distribution. Poisson regression models were developed to estimate 1) the probability, as expressed by the relative risk (RR), of presenting GO and AO at 9 years based on the obesity status at 4 and 6 years of age, and 2) the risk of GO at 6 and 9 years relative to the presence of GO and/or AO at 4 years of age. GEE and Poisson regression models with robust variance were developed. The variables included in the models were sex, age (months), and family affluence (FAS index). The relationships of GO and AO indicators with sex and socioeconomic status were explored. Confidence intervals were established at 95% (95% CI) for all estimators. The statistical significance level was set at 0.05.
The analyses were performed using Stata v.16 (StataCorp, College Station. USA) software.
Results
A total of 1,902 participants who completed all three measurements were included, which represented 65.5% of the participation rate over time. Of them, 49.6% were boys and the mean (SD) age was 48.5 (1.8), 73.4 (3.3), and 110.9 (4.5) months at the 4-, 6-, and 9-year-old measurements, respectively. The mean follow-up period was 5.2 years.
Weight and height were greater in boys than in girls of all ages. The values obtained for the BMI at 9 years old and for the WC at all ages were greater in the participants with low household affluence than in those with high household affluence (Table 1).
Table 2 shows the evolution of the standardized prevalence of overweight, GO, and AO. The prevalence of overweight between 4 and 9 years of age increased from 16.8% to 21.8% (PR: 1.30; 95% CI: 1.16–1.46), with a similar evolution by sex (PR: 1.25 in boys and 1.35 in girls) and by family affluence (PR: low affluence 1.23; medium 1.31; high 1.31). GO increased from 5.1% to 15.6% between 4 and 9 years (PR: 3.05), from 5.5% to 19.3% in boys (PR: 3.50) and from 4.7% to 11.9% in girls (PR: 2.53). A similar over-time increase in obesity was observed in the population with low, medium, and high family affluence (PR: 2.81, 3.0, and 3.26, respectively). The prevalence of GO at 6 and 9 years of age was higher in boys (11.3% and 19.3%, respectively) than in girls (6.9% and 11.9%, respectively). The prevalence was also higher in participants with low household affluence compared to those with high affluence at 4, 6, and 9 years (8.7% vs 3.9%, 14.6% vs 7.1%, and 24.6% vs. 12.6%, respectively).
The AO prevalence increased between 4 and 9 years of age from 6.8% to 14.5% (PR: 2.14), with a fairly similar trend disaggregated by sex (PR: 2.43 in boys and 1.92 in girls) and family affluence, where the prevalence of AO was about two-fold higher in participants of low socioeconomic status versus those of high level.
Table 3 shows the variations observed in obesity at the 9-year-old follow-up. Of the included subjects, 82.4% and 82.1% were stable without GO or AO, respectively; incidental obesity was recorded in 12.1% (GO) and 11.0% (AO) of them; and 3.4% (GO) and 3.5% (AO) were stable with obesity. The prevalence of boys classified as stable without GO (78.6%) was lower than that of girls (86.1%). Participants of low socioeconomic status showed a higher prevalence of stable GO (6.2%) and AO (6.5%) than those of high status (2.3% for GO and 2.5% for AO), with children from medium-affluence households in an intermediate position.
The Sankey diagram (Fig. 1) displays the tracking of obesity throughout the three measurements (see also Figs. 1S and 2S in Supplementary material). Most of the children with GO or AO at 4 or 6 years old remained in the same condition at 9 years old; 77.3% and 63.6% of children with GO and AO at 4 years of age also showed GO or AO at 9 years, respectively. Only 3.1% and 0.6% of those who were classified with GO at 4 and 6 years, respectively, remitted to normal weight at 9 years. Of those classified with obesity at 9 years, nearly half were determined to be incidental cases.
Table 4 shows the RRs of GO and AO at 9 years old relative to participants stable without obesity. The RR of GO was 4.61 (95% CI: 2.76–7.72) for participants who presented obesity at the age of 4 but not at the age of 6, 9.36 (95% CI: 7.72–11.35) if they were classified with obesity at 6 years but not at 4, and 10.27 (95% CI: 8.52–12.37) if they presented obesity at both 4 and 6 years of age. Similar results were found for the risk of presenting AO at 9 years, with estimated RRs of 4.14 (95% CI: 2.65–6.48), 9.56 (95% CI: 7.79–11.74), and 9.88 (95% CI: 8.07–12.11) for participants with obesity at the age of 4 but not at 6, with obesity at 6 years but not at 4, or with obesity at both 4 and 6 years of age, respectively.
Finally, participants with combined obesity of GO and AO at 4 years old showed RRs of GO of 16.10 (95% CI: 12.41–20.87) at 6 years and 6.54 (95% CI: 5.40–7.91) at 9 years, relative to children without obesity at 4 years old. Children with only GO at 4 years old had RRs of a BMI representative of obesity of 12.37 (95% CI: 8.92–17.17) and 5.65 (95% CI: 4.29–7.43) at the ages of 6 and 9, respectively, relative to those who had AO but not GO (Table 5).
Discussion
This study describes the longitudinal changes in the GO and AO condition in children from 4 to 9 years of age. A high increase in GO and AO over time was evident from the large number of incidental cases at 6 and 9 years old and low remission percentage, with prevalence rates three-fold (GO) and two-fold higher (AO) at 9 years old than those observed at 4 years old and with similar tendencies across all socio-economic levels. Additionally, the children who were already classified with obesity at 4 or 6 years old presented a higher risk of maintaining their obesity condition at 9 years old. These results highlight the importance of the early detection of changes in obesity (general and abdominal) since its appearance at 4 or 6 years of age is highly determinant of obesity at 9 years.
This study estimated a prevalence of GO of 5.1%, 9.1%, and 15.6% at 4, 6, and 9 years, respectively. The present results were of a similar magnitude and trend to other cross-sectional studies in our setting. A greater prevalence of GO has also been observed in boys than in girls [4]. Our results are consistent with other studies that reported that childhood is a particularly susceptible period for the development of obesity, especially after 5 years of age [25, 26].
The prevalence of AO increased with age and was similar to that observed by Schröeder et al., which reported a prevalence of abdominal obesity of 13% among Spanish children aged 6 to 11 years [27], but lower than the estimated prevalence of 21.5% at 3 to 8 years recently reported by Aranceta-Bartrina et al. [5]. The different measurement methods and cut-off points for the WC used to define AO could explain these differences.
A clear correlation between socioeconomic status and childhood obesity is observed in Western countries, with higher prevalence associated with lower socioeconomic levels [28]. However, whether these differences remain stable or continue to increase is not clear, with some studies describing an increasing inequality while others note a fairly uniform evolution [29]. The present study found higher prevalence rates in children with low household affluence, with similar trends for both GO and AO over the ages of 4 to 9 years in low-, medium-, and high-affluence families. Highly disparate trends have been observed in Spain. The study by Albaladejo-Vicente et al. [30] examined the population aged 5–15 years based on the national health survey from 1997 to 2017 and showed a decreasing trend in obesity in children of parents of low socioeconomic status and an increasing trend in girls. A study in Andalusia in 2011–2012 observed a gradient of childhood obesity by socioeconomic indicators that disappeared by 2015–2016 [31]. In contrast, an ecological study conducted in Catalonia based on primary care electronic medical records noted an increase in inequality between 2006 and 2016 [32].
On the other hand, our study tracked GO from 4 to 6 to 9 years of age and the findings were consistent with several studies that also suggest the stability and persistence of GO throughout childhood [33, 34]. Children with or without GO at 4 or 6 years old tended to remain in the same category at 9 years. Furthermore, over 60% of participants who had GO at 4 or 6 years continued to have obesity at 9 years. As shown in the Sankey diagram and Figure S1, only 3% and 0.6% of the children who presented GO at 4 or 6 years of age, respectively, remitted to normal weight at 9 years.
The risk of GO at 9 years was also greater if they presented obesity at both 4 and 6 years of age than if they did so at only one of the previous measurement points. Other studies reported similar results. A study in Norway found that children with excess weight at 2–4 years of age had an 11-fold higher risk (odds ratio) of being overweight at 5–7 years than children with normal weight [35]. In a study in Australia, 5-year-old children who were classified with obesity were 25 times more likely to continue having obesity 3 years later than those who were not [36].
The information available for the assessed age group is insufficient to compare the variations and risk of AO, not only in Spain but also in other countries. Vogelezang et al. [37] found that the persistence of AO was very high as early as at 2 and 6 years of age. A recent study by Ochiai et al. [38] estimated that half of the children classified with AO remained in the same category during adolescence, and Chrzanowska et al. reported that 51% of children with AO at the age of 7 remained with AO at 15 years [39]. The present study observed an even greater persistence of AO: 60–80% of children who presented obesity at 4 or 6 years old remained in the same category at 9 years (see supplementary material) and the risk of AO at 9 years was ten times higher if they had obesity at both 4 and 6 years of age. These results are in agreement with other studies, but comparisons should be made with caution given the differences in the follow-up periods, ages, and classification methods used [40, 41].
An aspect of important public health implications is the greater probability of finding GO in children of 6 or 9 years of age who presented AO but not GO at the age of 4, which represented 3.4% of the analyzed sample. Considering the high cardiometabolic risk in children with normal weight and BMI but with AO, the combined measures of weight, height, and WC will improve the predictive power to detect this health problem [42].
To correctly interpret the results of this study, several limitations must be taken into consideration. On the one hand, no information was available on the weight status between birth and 4 years, which prevents the completion of the children’s obesity trajectories. In the constitution of the ELOIN cohort, a moderate bias was observed in the selection of the sample that could affect its population representativeness: children with low educational level and foreign parents had a lower response rate at the baseline [20]. However, the sociodemographic and anthropometric variables were quite similar between those who attended the three follow-up measurements and the characteristics of the cohort at the baseline (Table 1S in Supplementary material).
The longitudinal design must be highlighted among the strengths of the study. In addition, the sample is representative of the population of the Community of Madrid, even with the above-mentioned selection bias. The measurements of anthropometric variables were based on objective criteria and performed in a standardized way, hence minimizing validity errors, such as self-reported measures or those provided by parents [43].
Conclusions
The present study showed that both GO and AO begin at an early age, are associated with low socioeconomic status, and increase rapidly with age. The follow-up of the participants from 4 to 9 years of age revealed that, once instituted, GO and AO tend to persist strongly throughout early to middle childhood. Both forms of obesity at the age of 9 years are closely related to previous obesity conditions at 4 or 6 years of age. Therefore, prevention and management interventions should be established at very early ages. GO and AO are complementary indicators and their combined use could maximize the detection and control of this health problem.
Availability of data and materials
According to private and confidential clauses stated in the informed consent, the dataset generated and analyzed during the current study is restricted and not publicly available for ethical reasons.
Data will be available from Dr. Honorato Ortiz-Marrón (E-mail: honorato.ortiz@salud.madrid.org upon reasonable request.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- PR:
-
Prevalence ratio
- RR:
-
Relative risk
- SD:
-
Standard deviation
- WC:
-
Waist circumference
- AO:
-
Abdominal obesity
- GO:
-
General obesity
- WHO:
-
World Health Organization
- IDF:
-
International Diabetes Foundation
- ELOIN:
-
Longitudinal Childhood Obesity Study
References
Seidell JC, Halberstadt J. The global burden of obesity and the challenges of prevention. Ann Nutr Metab. 2015;66(Suppl 2):7–12.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–42.
Garrido-Miguel M, Cavero-Redondo I, Álvarez-Bueno C, Rodríguez-Artalejo F, Moreno LA, Ruiz JR, et al. Prevalence and Trends of Overweight and Obesity in European Children From 1999 to 2016: A Systematic Review and Meta-analysis. JAMA Pediatr. 2019;e192430. https://doi.org/10.1007/s00394-021-02540-0.
García-Solano M, Gutiérrez-González E, López-Sobaler AM, Ruiz-Álvarez M, Bermejo López LM, Aparicio A, et al. Weight status in the 6- to 9-year-old school population in Spain: results of the ALADINO 2019 Study. Nutr Hosp. 2021;38(5):943–53.
Aranceta-Bartrina J, Gianzo-Citores M, Pérez-Rodrigo C. Prevalence of overweight, obesity and abdominal obesity in the Spanish population aged 3 to 24 years The ENPE study. Rev Esp Cardiol (Engl Ed). 2020;73(4):290–9.
Han JC, Lawlor DA, Kimm SYS. Childhood obesity – 2010: progress and challenges. Lancet. 2010;375(9727):1737–48.
Puhl RM, Lessard LM. Weight stigma in youth: prevalence, consequences, and considerations for clinical practice. Curr Obes Rep. 2020;9(4):402–11.
Umer A, Kelley GA, Cottrell LE, Giacobbi P, Innes KE, Lilly CL. Childhood obesity and adult cardiovascular disease risk factors: a systematic review with meta-analysis. BMC Public Health. 2017;17(1):683. https://doi.org/10.1186/s12889.017.4691.z.
Llewellyn A, Simmonds M, Owen CG, Woolacott N. Childhood obesity as a predictor of morbidity in adulthood: a systematic review and meta-analysis. Obes Rev. 2016;17(1):56–67.
Di Angelantonio E, Bhupathiraju S, Wormser D, Gao P, Kaptoge S, Global BMI Mortality Collaboration, et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388(10046):776–86.
Freedman DS, Sherry B. The validity of BMI as an indicator of body fatness and risk among children. Pediatrics. 2009;124(Suppl 1):S23–34.
Kok P, Seidell JC, Meinders AE. The value and limitations of the body mass index (BMI) in the assessment of the health risks of overweight and obesity. Ned Tijdschr Geneeskd. 2004;148(48):2379–82.
de Onis M, Onyango AW. WHO child growth standards. Lancet. 2008;371(9608):204–2014.
Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich-Horvat P, Liu C-Y, et al. Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham heart study. Circulation. 2007;116(1):39–48.
Song Q, Huang T, Song J, Meng X, Li C, Wang Y, et al. Causal associations of body mass index and waist-to-hip ratio with cardiometabolic traits among Chinese children: a Mendelian randomization study. Nutr Metab Cardiovasc Dis. 2020;30(9):1554–63.
Simmonds M, Llewellyn A, Owen CG, Woolacott N. Predicting adult obesity from childhood obesity: a systematic review and meta-analysis. Obes Rev. 2016;17(2):95–107.
Bayer O, Krüger H, von Kries R, Toschke AM. Factors associated with tracking of BMI: a meta-regression analysis on BMI tracking. Obesity (Silver Spring). 2011;19(5):1069–76.
Grossman DC, Bibbins-Domingo K, Curry SJ, Barry MJ, Davidson KW, US Preventive Services Task Force, et al. Screening for obesity in children and adolescents: US preventive services task force recommendation statement. JAMA. 2017;317(23):2417–26.
Trandafir LM, Russu G, Moscalu M, Miron I, Lupu VV, Leon Constantin MM, et al. Waist circumference a clinical criterion for prediction of cardio-vascular complications in children and adolescences with overweight and obesity. Medicine (Baltimore). 2020;99(30):e20923. https://doi.org/10.1097/MD.0000000000020923.
Ortiz-Marrón H, Cuadrado-Gamarra JI, Esteban-Vasallo M, Cortés-Rico O, Sánchez-Díaz J, Galán-Labaca I. The Longitudinal Childhood Obesity Study (ELOIN): design, participation and characteristics of the baseline sample. Rev Esp Cardiol (Engl Ed). 2016;69(5):521–3.
Zimmet P, Alberti KGM, Kaufman F, Tajima N, Silink M, Arslanian S, et al. The metabolic syndrome in children and adolescents - an IDF consensus report. Pediatr Diabetes. 2007;8(5):299–306.
Currie C, Molcho M, Boyce W, Holstein B, Torsheim T, Richter M. Researching health inequalities in adolescents: the development of the Health Behaviour in School-Aged Children (HBSC) family affluence scale. Soc Sci Med. 2008;66(6):1429–36.
Torsheim T, Cavallo F, Levin KA, Schnohr C, Mazur J, Niclasen B, et al. Psychometric validation of the revised family affluence scale: a latent variable approach. Child Indic Res. 2016;9:771–84.
ter Bogt TFM, de Looze M, Molcho M, Godeau E, Hublet A, Kokkevi A, et al. Do societal wealth, family affluence and gender account for trends in adolescent cannabis use? A 30 country cross-national study. Addiction. 2014;109(2):273–83.
Fomon SJ, Haschke F, Ziegler EE, Nelson SE. Body composition of reference children from birth to age 10 years. Am J Clin Nutr. 1982;35(5 Suppl):1169–75.
Hughes AR, Sherriff A, Lawlor DA, Ness AR, Reilly JJ. Incidence of obesity during childhood and adolescence in a large contemporary cohort. Prev Med. 2011;52(5):300–4.
Schröder H, Ribas L, Koebnick C, Funtikova A, Gomez SF, Fíto M, et al. Prevalence of abdominal obesity in Spanish children and adolescents. Do we need waist circumference measurements in pediatric practice? PLoS One. 2014;9(1):e87549. https://doi.org/10.1371/journal.pone.0087549.
McLaren L. Socioeconomic status and obesity. EpidemiolRev. 2007;29(1):29–48.
Chung A, Backholer K, Wong E, Palermo C, Keating C, Peeters A. Trends in child and adolescent obesity prevalence in economically advanced countries according to socioeconomic position: a systematic review. Obes Rev. 2016;17(3):276–95.
Albaladejo-Vicente R, Villanueva-Orbaiz R, Carabantes-Alarcón D, Santos-Sancho J, Jiménez-García R, Regidor E. Reversal of the upward trend of obesity in boys, but not in girls, in Spain. Int J Environ Res Public Health. 2021;18(4). https://doi.org/10.3390/ijerph18041842.
Sánchez-Cruz J-J, de Ruiter I, Jiménez-Moleón JJ, García L, Sánchez M-J. Stabilization and reversal of child obesity in Andalusia using objective anthropometric measures by socioeconomic status. BMC Pediatr. 2018;18(1):322. https://doi.org/10.3390/ijerph18041842.
de Bont J, Díaz Y, Casas M, García-Gil M, Vrijheid M, Duarte-Salles T. Time trends and sociodemographic factors associated with overweight and obesity in children and adolescents in Spain. JAMA Netw Open. 2020;3(3):e201171. https://doi.org/10.1001/jamanetworkopen.2020.1171.
Wheaton N, Millar L, Allender S, Nichols M. The stability of weight status through the early to middle childhood years in Australia: a longitudinal study. BMJ Open. 2015;5(4):e006963. https://doi.org/10.1136/bmjopen-2014-006963.
Freedman DS, Goodman AB, King RJ, Blanck HM. Tracking of obesity among 2- to 9-year-olds in an electronic heath record database from 2006 to 2018. Obes Sci Pract. 2020;6(3):300–6.
Evensen E, Wilsgaard T, Furberg A-S, Skeie G. Tracking of overweight and obesity from early childhood to adolescence in a population-based cohort - the Tromsø Study. Fit Futures BMC Pediatr. 2016;16:64. https://doi.org/10.1186/s12887-016-0599-5.
Hesketh K, Wake M, Waters E, Carlin J, Crawford D. Stability of body mass index in Australian children: a prospective cohort study across the middle childhood years. Public Health Nutr. 2004;7(2):303–9.
Vogelezang S, Gishti O, Felix JF, van der Beek EM, Abrahamse-Berkeveld M, Hofman A, et al. Tracking of abdominal subcutaneous and preperitoneal fat mass during childhood. The Generation R Study. Int J Obes (Lond). 2016;40(4):595–600.
Ochiai H, Shirasawa T, Nishimura R, Yoshimoto T, Minoura A, Oikawa K, et al. Changes in overweight/obesity and central obesity status from preadolescence to adolescence: a longitudinal study among schoolchildren in Japan. BMC Public Health. 2020;20(1):241. https://doi.org/10.1186/s12889-020-8343-3.
Chrzanowska M, Suder A, Kruszelnicki P. Tracking and risk of abdominal obesity in the adolescence period in children aged 7–15. The Cracow longitudinal growth study. Am J Hum Biol. 2012;24(1):62–7.
Cunningham SA, Datar A, Narayan KMV, Kramer MR. Entrenched obesity in childhood: findings from a national cohort study. Ann Epidemiol. 2017;27(7):435–41.
Geserick M, Vogel M, Gausche R, Lipek T, Spielau U, Keller E, et al. Acceleration of BMI in early childhood and risk of sustained obesity. N Engl J Med. 2018;379(14):1303–12.
Gishti O, Gaillard R, Durmus B, Abrahamse M, van der Beek EM, Hofman A, et al. BMI, total and abdominal fat distribution, and cardiovascular risk factors in school-age children. Pediatr Res. 2015;77(5):710–8.
Esteban-Vasallo MD, Galán I, Ortiz-Pinto MA, Astray San Martín A, Cabrero López EM, Morales San José MT, Ortiz-Marrón H. Accuracy of anthropometric measurements and weight status perceptions reported by parents of 4-year-old children. Public Health Nutr. 2020;23(4):589–98. https://doi.org/10.1017/S1368980019003008.
Acknowledgements
To the participating families, to the health workers, and to the companies Demométrica, Sondaxe and Sigmados, which conducted the telephone interviews.
Funding
The ELOIN study was funded by the General Directorate of Public Health of the Ministry of Health of the Community of Madrid. The authors have not received financial support for the research, authorship, or publication of this article. This project received a grant for the translation and publication of this paper from the Foundation for Biosanitary Research and Innovation in Primary Care (FIIBAP).
Author information
Authors and Affiliations
Contributions
H. Ortiz-Marrón and I. Galán conceptualized and designed the study, drafted the initial manuscript with tables and figures, and checked and revised the final manuscript. H. Ortiz-Marrón, I. Galán, and MA. Ortiz-Pinto designed the instruments for data collection and initial analysis. MA. Ortiz-Pinto, G. Cabañas Pujadas, JG. Martinez Mosquera, M. Lorente Miñarro, F. Menchero Pinos, and M. Ordobás Gavín participated in the data collection and critically reviewed the manuscript making important contributions to its content. All authors gave their approval and agreed to the final manuscript and assume responsibility for all the aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ethics Committee of the Hospital Ramón y Cajal in Madrid approved the study (CIHURC- 122/11). Prior to their inclusion in the present study, all participants provided written informed consent. Written informed consent was obtained from the participants’ parents or legal guardians before their participation in the ELOIN study. The present study was conducted according to the Declaration of Helsinki and all methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interest
The authors declare that there are no potential conflicts of interest regarding the research, authorship, and/or publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Figure 1S. Weight status transitions (normal weight, overweight, and obesity) classified according to WHO-2007 criteria13: (A) from 4 to 9 years of age, and (B) from 6 to 9 years of age. Figure 2S. Abdominal obesity transitions based on waist circumference following the International Diabetes Federation consensus criteria21: (A) from 4 to 9 years of age, and (B) from 6 to 9 years of age.
Additional file 2:
Table 1S. Characteristics of children enrolled in the original cohort and in the study sample.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ortiz-Marrón, H., Ortiz-Pinto, M.A., Cabañas Pujadas, G. et al. Tracking and risk of abdominal and general obesity in children between 4 and 9 years of age. The Longitudinal Childhood Obesity Study (ELOIN). BMC Pediatr 22, 198 (2022). https://doi.org/10.1186/s12887-022-03266-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-022-03266-6