Abstract
Background
Birth asphyxia is the major public health problem in the world. It is estimated that around 23% of all newborn deaths are caused by birth asphyxia worldwide. Birth asphyxia is the top three causes of newborn deaths in sub-Saharan Africa and more than one-third of deaths in Ethiopia. Therefore, the aim of this study was to identify determinants of birth asphyxia which can play a crucial role to decrease the death of newborns.
Methods
Unmatched case-control study design was implemented among 276 (92 cases and 184 controls) newborns from January 1st to March 30th, 2020. A systematic sampling technique was used to select the study participants. Data were collected by using a semi-structured interviewer-administered questionnaire and document review by trained nurses and midwives who work at the delivery ward of the hospitals. Bivariate logistic regression analysis was done to identify determinants of birth asphyxia. Adjusted odds ratios with 95% confidence intervals and p-value less than and equal to 0.05 were used to assess the level of significance.
Results
In this study, maternal education of being can’t read & write [AOR = 4.7, 95% CI: (1.2, 11.9)], ante-partum hemorrhage [AOR = 7.7, 95% CI: (1.5, 18.5)], prolonged labor [AOR =13.5, 95% CI: (2.0, 19.4)], meconium stained amniotic fluid [AOR = 11.3, 95% CI: (2.7, 39.5)], breech fetal presentation [AOR = 4.5, 95% CI: (2.0, 8.4)] and preterm birth [AOR: 4.1, 95% CI: (1.8, 9.2)] were factors which showed significantly associated with birth asphyxia among newborns.
Conclusions
In this study, maternal education can’t read & write, antepartum hemorrhage, prolonged labor, stained amniotic fluid, breech fetal presentation, preterm birth were significantly associated with birth asphyxia. So, educating mothers to enhance health-seeking behaviors and close monitoring of the labor and fetus presentation were recommended to reduce birth asphyxia.
Similar content being viewed by others
Introduction
Birth asphyxia is defined as the failure of the newborn to initiate and sustain adequate respiration after delivery [1]. It is also an existence of umbilical cord arterial pH < 7; APGAR score of 0–3 for longer than 5 min; neurological manifestations such as seizures, hypercapnia, metabolic acidosis and hypoxic-ischemic encephalopathy [2]. It is the major public health problem among under-five children in the world. Globally, 4 million or 23.0% of newborn deaths occur yearly due to birth asphyxia, representing the fifth (38.0%) largest cause of under-5 year’s children deaths [3]. The problem is severe in developing countries at which 120 million newborns develop birth asphyxia and the cause for 900,000 deaths every year. In sub-Saharan African countries 24.0% of newborn deaths were due to birth asphyxia [4].
In Ethiopia, birth asphyxia is the cause of more than one-third of newborn deaths [5]. The effect of birth asphyxia is not limited only to death but also has a short and long-term neurodevelopment squeal including cognitive and motor disabilities which are almost untreatable [6, 7]. In order to alleviate this problem, national newborn training and guidelines are well established for those health professionals who were attending labor at any health facility level. There is also a child survival strategy in Ethiopia that connects essential maternal, newborn, and child health packages throughout adolescence, pregnancy, childbirth, postnatal and newborn periods, and into childhood building upon their natural interactions throughout life. Even if such strategies were applied by Ethiopian health policy the problem of newborn death was still high in the country [5, 8].
Many studies in different parts of Ethiopia showed that parity [9], anemia [10, 11], antepartum hemorrhage [12], prolonged labor [9], preterm birth [12], meconium-stained liquor [12, 13], pregnancy-induced hypertension [10], and mode of delivery [14] were significant predictors of birth asphyxia. However, information related to determinants of newborn asphyxia in Debre Berhan referral hospitals is limited. Therefore, the aim of this study was to identify determinants of birth asphyxia among newborns in Debre Berhan Referral Hospital, Debre Behan, Ethiopia. The findings will help to improve health care providers’ and women’s knowledge on birth asphyxia during labor. This study also contributes for SGD goals 3 to reduce neonatal mortality by identifying the risk factors of birth asphyxia.
Methods
Study area and period
The study was conducted in Debre Berhan referral hospital at Debre Berhan town. It is located in North Shoa Zone, Amara regional state, North East part of Ethiopia. It is 130 km far from the capital city Addis Ababa, and 695 km far from the regional city Bahir Dar. It is one of the largest public referral hospitals in the zone, providing preventive, curative and rehabilitative services to about more 3 million people in the catchment area. It also provides delivery service 24 h a day, 7 days a week by 24 midwives, 3 general practitioners and 4 gynecologists who assist about 3366 deliveries annually. In NICU ward there are 22 nurses, 3 general practitioners and 2 pediatricians. The total admission of NICU wards from 2019 report 1056 neonates 313 by birth asphyxia. The study was conducted from January 1st to March 30th, 2020.
Study design
An institution-based unmatched case-control study design was employed to assess determinants of birth asphyxia among newborns in Debre Berhan Referral Hospital.
Population
All newborns delivered in Debre Berhan referral hospital were the source population and all newborns delivered in the hospital during the study period were the study population. Newborns that had heart deformity and more than one malformation were excluded from the study.
Sample size determination
The sample size was determined by Epi Info 7 version software package for the unmatched case control study. By considering, 29.4% proportion of controls exposed and odds ratio of 2 for low gestational age from a previous study conducted in Ethiopia Tigray region [12],with an assumption of, 95% confidence interval, 80% power of the study, two- to- one control to cases ratio, and 5% non-response rate. The final sample size was 276 (92 cases and 184 controls).
Sampling procedure
A systematic random sampling technique was used to select the study participants. Every third study subjects were included for both cases and controls. On the first day of data collection the first study participant was taken by using simple random sampling technique from the registration book.
Data collection tools and procedure
The data were collected by using interviewer administered structured questionnaire adapted from different literatures [7, 12], and document review. The socio-demographic and antepartum characteristics of the responder were collected by using interview and intra-partum and neonate characteristics were collected from medical records of the mother by using checklist. The questionnaire was first prepared in English and translated to local language Amhric and back translates to English to keep its consistency. The questionnaire was pre-tested in another health facilities and essential amendment were made based on the results. Data were collected by four midwives and two supervisors who have en experience of work on neonatal intensive care unit of the hospital.
Operational definition
Cases
When the newborn has at least one of the following signs, not breathing, gasping, < 30 breaths per minute or 5th minute APGAR score of < 7 [10].
Outcome variable
Birth asphyxia.
Independent variable
-
I.
Socio demographic determinants: age, marital status, residence, educational status, maternal occupation
-
II.
Ante partum determinants: parity, pregnancy induced hypertension, anemia, ante-partum hemorrhage, ANC follow up, chronic disease
-
III.
Intra-partum determinants: fetal presentation, duration of labor, amniotic fluid, type of labor, mode of delivery, labor attendant, PROM
-
IV.
Neonatal determinants: Sex, birth weight, gestational age
Data quality control
The quality of data was assured by using properly designed and validated questionnaire by those individuals who work more on the field of the study. Training was given for the data collectors and supervisors on how to collect the data for 3 days. Pre-testing was performed in another health facility and essential amendment was made on the questionnaire. The principal investigator and supervisors were made a day to day on site supervision and check the collected data for completeness, clarity and consistency.
Data processing and analysis
The data was coded and entered to Epi-data version 3.1 and exported to SPSS Version 21 for data analysis. Descriptive statistics were performed and presented in the form of means, standard deviations, frequencies and percentages. Binary logistic regression was computed to identify determinates of birth asphyxia. Variable which have p-value less than 0.25 in binary logistic regression analysis were transferred to multiple logistic regression model to see the relative effect of the confounder. Model goodness of fit test was checked by using Hosmer Lemeshow goodness of fit and Multicolinearity was assessed by variance inflation factor (VIF) among variables. Adjusted odd ratios with 95% confidence interval and P-value less than 0.05 was used to identify determinates of birth asphyxia.
Results
Socio-demographic characteristics of the study participants
A total of 276 (92 cases and 184 controls) were participated in the study with a response rate of 100%. About 52.2% of cases and 42.4% controls were live in rural resident and 42.4% of the mother of the cases and 6.0% controls were can’t read and write in their educational status. More mother of cases (48.9%) than controls (19.0%) were house wife by their occupational status. The majority of mother of cases (80.4%) and controls (95.1%) were married in their marital status (Table 1).
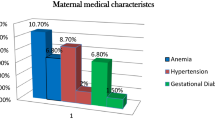
Ante partum related characteristics of the study participants
From the total study participants,46 (55.4%) mothers of the cases and 37 (44.6%) mothers of the controls were premipara, 39 (61.9%) mothers of the cases and 24 (38.1%) mothers of the controls were less than or equals to two ANC visits, 25 (78.1%) of the mothers of the cases and 7 (21.9%) mothers of the controls were APH during pregnancy, 21 (77.8%) mothers of the cases and 6 (22.2%) of the controls had anemia and 19 (73.1%) mothers of the cases and 7 (26.9%) of the controls were PIH during pregnancy (Table 2).
Intra partum related characteristics of the study participants
About 43.4% of the cases and 23.9% of the controls mother labor were attended by midwives. Majority 54.3% of the cases and 84.8% of the controls mother had spontaneous type labor and 50.0% of cases and 7.6% of controls mother delivered with stained amniotic fluid. Majority 73.9% of cases and 88.0% of controls were cephalic fetal presentation. About 14.1% of the cases and only 1.1% of controls were delivered with cored prolapsed (Table 3).
Newborn related characteristics of the study participants
This study revealed that 54 (58.7%) of cases and 107 (58.2%) of controls were male neonates. Twenty two (23.9%) of cases and only 6 (3.3%) of controls were preterm neonates. It was also observed that 39 (42.4%) of the cases and 34 (18.5%) of the controls were low birth weight (Table 4).
Determinants of birth asphyxia among newborns
Those variables which showed p-value < 0.05 in bivariate analysis were transferred to multivariate analysis to see the effect of confounders. In multivariate logistic regression analysis maternal education, ANC follow up, presence APH, prolonged labor, stained amniotic fluid, not cephalic fetal presentation and gestational age less than 37 weeks were identified as determinants of birth asphyxia among newborns. This study revealed that mother who can’t read and write [AOR = 4.7; 95%CI (1.2, 11.9)] were 4.7 times higher to develop birth asphyxia compared from mother who have college diploma and above. The odds of developing birth asphyxia among mothers who faced antepartum hemorrhage was 7.7 times higher compared from the counterparts [AOR = 7.7; 95%CI (1.5, 18.5)]. This study revealed that prolonged labor was the main predictor of birth asphyxia. A mother who had prolonged labor was more than 13 time higher risk compared from normal labor on the outcome of birth asphyxia [AOR = 13.5; 95%CI (2.0, 19.4)]. Preterm babies were 4.1 times higher risk than term babies to development birth asphyxia [AOR = 4.1; 95%CI (1.8, 9.2)] (Table 5).
Discussion
This study tried to identify the determinants of birth asphyxia among newborns in Debre Berhan referral hospital by including number of variables from different categories like socio-demographic, antepartum, intra partum and neonatal related characteristics of the newborns.
This study revealed that mothers who can’t read and write were 4.7 times higher risk to have asphyxiated newborns compared to mothers who have a college diploma and above. This finding was consistent with the study conducted in Sweden [15], Nepal [16], Pakistan [17] and Ethiopia [7, 12, 18]. This could indicate that poor literacy limits mothers from having independent decisions and good access to family resources that could restrict their health-seeking behaviour during the antepartum period and also it is an indicator of poor socio-economic status of the community and unplanned pregnancy.
Gestational age was significantly associated with birth asphyxia. Preterm (<37wks) was 4.1 times more likely asphyxiated than the term newborns. This finding was consistent with those of previous studies conducted in Pakistan [17], Nepal [16], and Ethiopia [9, 12, 19]. This may be due to the fact that preterm babies face multiple morbidities including organ system, immaturity especially lung immaturities causing respiratory failure.
Newborns with the breech presentation were 4.5 times the odds of developing birth asphyxia than the cephalic presentation. This finding was consistent with previous studies conducted in Uganda [20], Cameron [21], and Ethiopia [22]. Mal-presentation of foetus is associated with premature rupture of membrane; this premature rupture of membrane could leads to umbilical cord accidents occur with sub sequent asphyxia at birth [14]. But, the finding was inconsistent with previous studies conducted in Ethiopia [13, 23]. This difference might be due to the difference in the study population, both of the study was conducted in metropolitan city of Ethiopia at which the maternal healthcare services were more advanced than the study area.
Prolonged labour was significantly associated with birth asphyxia. This finding was consistent with studies conducted in India [24], Malawi [25], Cameron [21], Pakistan [17], and Ethiopia [11, 26,27,28]. This could be due to primary, secondary, or tertiary dalliance. This is in fact that, when labour is prolonged there was a high probability for the foetus to become distressed which can lead to birth asphyxia [28].
Less than or equals to two ANC follow up by the mothers were 4.6 times higher odds of developing asphyxiated newborns than mothers who have more than four ANC follow up. This finding was inconsistent with the study conducted in Ethiopia [13, 23, 27]. This difference may be due to the number of health facilities included in the study and study period. This ANC visit of the pregnant mother are very important to minimize adverse pregnancy outcomes including birth asphyxia as they provide chance for evaluating the foetal wellbeing and permit management soon by improving the health and wellbeing of the mother and preventing further complications by early detection and treatment of diseases.
In this study, induced labor doesn’t show an association with birth asphyxia when compared to Spontaneous labor. This result was congruent with the study conducted in West Shewa Zone, central Ethiopia [22]. But it was inconsistent with the Meta-analysis study conducted in Ethiopia [29]. This difference may be due to the difference in the study setting at which both this study and the central Ethiopia study were conducted in a single institution. This induction of labor may cause hyper-stimulation of the uterine constriction that could cause fetal heart rate changes. When constrictions are too fast and strong, the placenta, which helps carry oxygen-rich blood to the baby, often cannot recharge with an adequate supply of this blood for the baby [30].
In this study, we have limitations that should be noted. The study was done in single health facility therefore; it is difficult to generalize for the whole country with this small sample. This study also subjected to recalling bias of mothers when they remembered their previous history. The study also have other limitation that variables in intrapartum events like umbilical cord status, uterine rupture, placental abruption, shoulder dystocia and major maternal haemorrhage, trauma, cardiorespiratory arrest or maternal seizures immediately preceding delivery were not addressed.
Conclusions
In this study, maternal education can’t read & write, antepartum hemorrhage, prolonged labour, stained amniotic fluid, breech fetal presentation, preterm birth were significantly associated with birth asphyxia. So, educating mothers to enhance health seeking behaviors and close monitoring of the labor and fetus presentation were recommended to reduce birth asphyxia.
Availability of data and materials
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- ANC:
-
Antenatal Care
- AOR:
-
Adjusted Odd Ratio
- DDS:
-
Dietary Diversity Score
- FAO:
-
Food and Agriculture Organization
- NNP:
-
National Nutritional Program
- SD:
-
Standard Deviation
- SPSS:
-
Statistical Package for Social Science
- WHO:
-
World Health Organization
References
Spector JM, Daga S. Preventing those so-called stillbirths. Bull World Health Organ. 2008;86:315–6.
Solnes Miltenburg A. Quality of maternity Care in Rural Tanzania: understanding local realities and identification of opportunities for. Improvement. Dissertations submitted to the Faculty of Medicine, University of Oslo, Norway; 2019. ISBN 978-82-8377-422-1.
Organization WH. Newborn death and illness. Millennium Development goal (mdg). 2011;4.
Fekede A. Knowledge, attitude and practice towards Management of Birth Asphyxia among nurses and midwives working in labour Ward and Nicu in governmental hospitals, Addis Ababa, Ethiopia, 2017: Addis Ababa University; 2017.
Demographic E. Health survey, key indicators. Rockville: CSA, ICF; 2016.
Kiyani AN, Arshad Khushdil AE. Perinatal factors leading to birth asphyxia among term newborns in a tertiary care hospital. Iran J Pediatr. 2014;24(5):637.
Wosenu L, Worku AG, Teshome DF, Gelagay AA. Determinants of birth asphyxia among live birth newborns in University of Gondar referral hospital, Northwest Ethiopia: a case-control study. PLoS One. 2018;13(9):e0203763.
MoH F. National strategy for child survival in Ethiopia. Ethiopia: Addis Ababa; 2005.
Abdo RA, Halil HM, Kebede BA, Anshebo AA, Gejo NG. Prevalence and contributing factors of birth asphyxia among the neonates delivered at Nigist Eleni Mohammed memorial teaching hospital, southern Ethiopia: a cross-sectional study. BMC Pregnancy Childbirth. 2019;19(1):1–7.
Alemu A, Melaku G, Abera GB, Damte A. Prevalence and associated factors of perinatal asphyxia among newborns in Dilla University referral hospital, southern Ethiopia–2017. Pediatric Health Med Therapeut. 2019;10:69.
Gebregziabher GT, Hadgu FB, Abebe HT. Prevalence and associated factors of perinatal asphyxia in neonates admitted to ayder comprehensive specialized hospital, northern Ethiopia: a cross-sectional study. Int J Pediatr. 2020;2020.
Tasew H, Zemicheal M, Teklay G, Mariye T, Ayele E. Risk factors of birth asphyxia among newborns in public hospitals of central zone, Tigray, Ethiopia 2018. BMC Res Notes. 2018;11(1):1–7.
Mulugeta T, Sebsibe G, Fenta FA, Sibhat M. Risk factors of perinatal asphyxia among newborns delivered at public hospitals in Addis Ababa, Ethiopia: case–control study. Pediatr Health Med Therapeut. 2020;11:297.
Bayih WA, Yitbarek GY, Aynalem YA, Abate BB, Tesfaw A, Ayalew MY, et al. Prevalence and associated factors of birth asphyxia among live births at Debre Tabor general hospital, north Central Ethiopia. BMC Pregnancy Childbirth. 2020;20(1):1–12.
Odd D, Lewis G, Gunnell D, Rasmussen F. Risk of low Apgar scores and socioeconomic status over a 30-year period. J Matern Fetal Neonatal Med. 2014;27(6):603–7.
Lee AC, Mullany LC, Tielsch JM, Katz J, Khatry SK, LeClerq SC, et al. Risk factors for neonatal mortality due to birth asphyxia in southern Nepal: a prospective, community-based cohort study. Pediatrics. 2008;121(5):e1381–90.
Tabassum F, Rizvi A, Ariff S, Soofi S, Bhutta ZA. Risk factors associated with birth asphyxia in rural district Matiari, Pakistan: a case control study. Int J Clin Med. 2014;5(21):1430.
Desalew A, Semahgn A, Tesfaye G. Determinants of birth asphyxia among newborns in Ethiopia: a systematic review and meta-analysis. Int J Health Sci. 2020;14(1):35.
Yeshaneh A, Kassa A, Kassa ZY, Adane D, Fikadu Y, Wassie ST, et al. The determinants of 5th minute low Apgar score among newborns who delivered at public hospitals in Hawassa City, South Ethiopia. BMC Pediatr. 2021;21(1):1–10.
Kaye D. Antenatal and intrapartum risk factors for birth asphyxia among emergency obstetric referrals in Mulago Hospital, Kampala, Uganda. East Afr Med J. 2003;80(3):140–3.
Chiabi A, Nguefack S, Evelyne M, Nodem S, Mbuagbaw L, Mbonda E, et al. Risk factors for birth asphyxia in an urban health facility in Cameroon. Iran Journal of child neurology. 2013;7(3):46.
Kune G, Oljira H, Wakgari N, Zerihun E, Aboma M. Determinants of birth asphyxia among newborns delivered in public hospitals of west Shoa zone, Central Ethiopia: a case-control study. PLoS One. 2021;16(3):e0248504.
Woday A, Muluneh A, St Denis C. Birth asphyxia and its associated factors among newborns in public hospital, Northeast Amhara, Ethiopia. PLoS One. 2019;14(12):e0226891.
Kumar S, Akbar Nizamani M, Memon S. Risk factors in birth asphyxia at LIAQUAT UNIVERSITY hospital HYDERABAD. Med Channel. 2014;20(1).
Tewesa E, Chirwa E, Majamanda MD, Maluwa A, Chimwaza A. Associative factors for birth asphyxia at queen Elizabeth central hospital—Malawi. J Biosci Med. 2017;5(05):22.
Kibret Y, Hailu G, Angaw K. Determinants of birth-asphyxia among newborns in Dessie town hospitals. North-Central Ethiopia. 2018;2017.
Meshesha AD, Azage M, Worku E, Bogale GG. Determinants of birth asphyxia among newborns in referral hospitals of Amhara National Regional State, Ethiopia. Pediatr Health Med Therapeut. 2020;11:1.
Sendeku FW, Azeze GG, Fenta SL. Perinatal asphyxia and its associated factors in Ethiopia: a systematic review and meta-analysis. BMC Pediatr. 2020;20(1):1–11.
Ahmed R, Mosa H, Sultan M, Helill SE, Assefa B, Abdu M, et al. Prevalence and risk factors associated with birth asphyxia among neonates delivered in Ethiopia: a systematic review and meta-analysis. PLoS One. 2021;16(8):e0255488.
Sarathi S, Semmalar S. Complications of oxytocin in induction of labour. IOSR J Nurs Health Sci (IOSR-JNHS). 2015;4(2):29–32.
Acknowledgements
We would like to thank Debre Berhan Referral hospital medical directors for their collaboration during conducting this research. Our gratitude also goes to our data collectors and study participants for their willingness to participate in the study. At last but not least, we would like to forward our special thank and sincere appreciations to our friends who gave advice and comment throughout the whole research project activities.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
SST supervised the design of the study, writing and critically reviewed the drafts. YTG conceptualized and designed the study, obtain fund for the study, coordinate, and monitor the overall implementation of the project. She also participated in data extraction and analysis, interpreted the results and wrote the initial draft. SMA and AST contributed to the design and write of subsequent drafts of the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Consent to publication
Not applicable.
Ethics approval and consent to participate
This study was carried out after getting ethical clearance from Debre Berhan University, Institute of medicine and Health Science, College of Health Science, Department of Public Health research ethics review committee Ref. No./IOMHS/029/201/10/2020. Data collection was carried out after receiving ethical clearance letter from the district administrative health bureau. Informed written consent was obtained from each study participant prior to data collection. Each participant read the letter and explained further by the data collectors for easily understands the objective of the research. All methods were carried out in accordance with relevant guidelines and regulations of Helsinki declaration. Finally, the consent form was signed by each participant.
Competing interests
The Authors declare that we do not have any financial or non-financial competing interests in reference to this article for its publication.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tegegnework, S.S., Gebre, Y.T., Ahmed, S.M. et al. Determinants of birth asphyxia among newborns in Debre Berhan referral hospital, Debre Berhan, Ethiopia: a case-control study. BMC Pediatr 22, 165 (2022). https://doi.org/10.1186/s12887-022-03223-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-022-03223-3