Abstract
Background
The study was designed to investigate microvascular and morphological changes in retinal vein occlusion (RVO) using multimodal imaging after intravitreal ranibizumab (IVR) with or without triamcinolone acetonide (IVTA) injections.
Methods
This was a retrospective and observational study. Fifty patients (52 eyes) diagnosed with RVO were enrolled. Best corrected visual acuity (BCVA), ophthalmoscopy, fundus fluorescein angiography (FFA), spectral domain optical coherence tomography (SDOCT), and optical coherence tomography angiography (OCTA) were employed sequentially both before treatment and at the last visit after treatment.
Results
The mean logMAR VAs in BRVO eyes decreased significantly after treatment (P = 0.029). OCTA showed there was a significant difference in foveal avascular zone (FAZ) in BRVO eyes (P = 0.024), superificial foveal vessel density in both CRVO (P = 0.0004) and BRVO eyes (P = 0.02155). OCT showed the foveal thickness had significant differences after treatment in both CRVO (P < 0.0001) and BRVO eyes (P = 0.0001). BCVA was associated most commonly with ellipsoid zone integrity (P = 0.022). The BCVA in eyes treated with IVR and IVTA was significantly decreased compared with IVR only in BRVO group (P = 0.021). However, the combination of IVR + IVTA significantly improved intraocular pressure (IOP) compared with IVR only in BRVO group (P = 0.037).
Conclusion
Both IVR and IVR + IVTA can significantly improve the central vision, macular structure, and functions in BRVO group. Simultaneous IVR with IVTA can significantly increase BCVA compared with IVR only in BRVO group.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Retinal vein occlusion (RVO) is the second most common retinal vascular disease [1]. Obstruction can occur in the central trunk or its branches and it occurs more commonly with branch retinal vein occlusion (BRVO). The main cause of vision loss is persistent macular edema (ME). The first line treatment for ME caused by RVO is anti-vascular endothelial growth factor (VEGF) therapy. Anti-VEGF therapy has been shown to be effective in restoring visual function and macular morphology.
However, there are some RVO patients who do not respond sensitively to anti-VEGF drugs. Multiple studies have shown that levels of inflammatory factors, such as VEGF, interleukin-1 β, and interleukin-6, are associated with the severity of ME [2]. Dexamethasone treatment reduces proinflammatory cytokine levels in the aqueous humor of patients with RVO [3]. An intravitreal steroid injection may be beneficial for these RVO patients who do not respond sensitively to anti-VEGF drugs. Intravitreal triamcinolone acetonide has been used to treat ME secondary to RVO for many years [4]. Its mechanisms include anti-inflammatory effects [5, 6], inhibition of VEGF [7], improvement of diffusion [8], and reconstruction of the blood-retinal barrier by reducing permeability [9, 10]. Due to well-known complications such as cataracts and increased intraocular pressure (IOP), intravitreal steroid administration is reserved as second-line therapy if anti-VEGF is ineffective [11,12,13].
The cost of repeated anti-VEGF therapy is high, which brings an economic burden to patients. Due to financial limitations, in general clinical practice in China, ophthalmologists aim to improve the therapeutic effect by reducing the number of anti-VEGF injections. Retinal specialists suggest that it is important to develop a multimodal approach to the treatment and management of ME. These multi-mode therapies mainly focus on anti-VEGF therapy combined with triamcinolone acetonide injection, laser photocoagulation, or vitrectomy [14]. Previous studies have reported that the combination of ranibizumab and triamcinolone acetonide injection in the treatment of central branch retinal vein occlusion (CRVO) induced ME can reduce the number of repeated injections [15]. Intravitreal ranibizumab (IVR) and triamcinolone acetonide injections (IVTA) have also been used clinically to treat ME caused by RVO.
Recently, multimodal imaging has been used to show the morphology and structure of the retina blood vessels at different levels and to quantify blood flow density [16,17,18]. On the one hand, multimodal imaging technology contributes to the diagnosis of fundus diseases. On the other hand, in the process of exploring the nature of diseases, it can provide a new understanding of the pathological mechanism of diseases, which contributes to accurate diagnosis and dynamic monitoring of ophthalmic diseases, and provides a good reference for the selection of treatment for ophthalmic diseases. However, there was little report about using multimodal imaging to evaluate the efficacy of IVR with or without IVTA. In our study, multimodal imaging was used to observe the microvascular and foveal changes before treatment, and at the last visit after IVR with or without IVTA in patients with RVOs.
Methods
This study was a retrospective cohort study and it was approved by the Second.
Xiangya Hospital Ethics Committee. Patients undergoing IVR (0.5 mg) and IVTA (1 mg) injections for RVO were included in the study. The diagnosis of RVO was confirmed with fundus fluorescein angiography (FFA), spectral domain optical coherence tomography (SDOCT), and optical coherence tomography angiography (OCTA). Exclusion criteria included previous treatment for RVO, previous retinal surgery, age-related macular degeneration, diabetic retinopathy, and other retinal vascular diseases. Visual acuity, central foveal thickness, duration of edema, severity of inflammation, personal experience of the physician, and patient’s treatment preference are all key considerations in choosing IVR with or without IVTA. All patients received at least once IVR with or without IVTA. Additional IVR with or without IVTA were required when any of the following conditions occurred: (1) macular effusion; and (2) central retinal thickness increased greater than 100 μm compared with previous measurements. All patients were followed up at 1 day, 1 week, and 1 month after the first intravitreal injection. Postoperative follow-up was performed once a month. The best corrected visual acuity (BCVA), IOP, slit lamp, and indirect ophthalmoscopy, fundus photography, FFA (Optos 200Tx Imaging System; Optos PLC, Dunfermline, Scotland), SDOCT (Carl Zeiss Meditec, Jena, Germany), and OCTA (RTVue XR Avanti, AngioVue; Optovue, Inc., Fremont, CA, USA) were performed before the intravitreal injection and at the last visit. All patients were followed up monthly from the beginning of the first treatment to at least 6 months after the first treatment.
Optical coherence tomography angiography
OCTA works with Avanti RTVue XR AngioVue software (Optovue Inc., Fremont,
CA, USA). The scanning area of macular angiography was 6 × 6 mm, and four.
images were automatically generated by the instrument. They were of the shallow retina, deep retina, outer retina, and choroid capillary layer. The FAZ area was measured with the non-flow function in OCTA software. The mesh consisted of two circles: an inner circle and an outer circle. The foveal thickness was calculated from the inner circle with a diameter of 1 mm.
Spectral domain optical coherence tomography
SDOCT was used to detect the foveal thickness, macular foveal hyperreflective dots (near the fovea, less than 50 microns in size, with reflectivity similar to that of the retinal nerve fiber layer and without background shadows), epimacular membrane or vitreomacular traction, ellipsoid zone interrupted, disorganization of the retinal inner layers (DRIL), external limiting membrane interrupted.
Fluorescein angiography
FFA was used to evaluate disruption of the perifoveolar capillary arcade, late macular leakage, macular ischemia, and peripheral ischemia.
Statistical analysis
SPSS 27.0 software was used for statistical analysis. The BCVA was converted to logMAR for statistical evaluation. A lower logMAR vision was a better Snellen equivalent. Multivariable regression (α in = 0.05, α out = 0.10) was used to identify the most critical factors for BCVA. The injection number, changes of.
logMAR VA, FAZ, foveal thickness, and superficial foveal vessel density between IVR and IVR with IVTA were compared with t-test. The changes of OCT features, OCTA features, and FFA features between IVR and IVR with IVTA were compared with chi-square test. P < 0.05 was considered statistically significant.
Results
The basic clinical information for the included patients is shown in Table 1. A total of 50 patients with a history of RVO were enrolled in this study (27 females, 23 males, mean age 56.54 ± 13.594 years). Twenty-eight patients had hypertension, thirteen had hyperglycemia. There were no significant differences in age, sex, hypertension, and diabetes between the CRVO and BRVO groups.
The mean logMAR visual acuities in BRVO eyes decreased significantly after treatment (0.904 ± 0.574 vs. 0.585 ± 0.464, P = 0.029, Table 2). OCTA revealed significant differences in the FAZ (0.411 ± 0.126 vs. 0.505 ± 0.168, P = 0.024) in the BRVO group. Foveal vessel density decreased in both the CRVO (30.875 ± 7.313 vs. 23.091 ± 7.142, P = 0.0004) and BRVO (33.289 ± 8.66 vs. 28.047 ± 7.557, P = 0.02155) groups after treatment. OCT scans showed a significant decrease in foveal thickness in both the CRVO (530.92 ± 132.249 vs. 332.84 ± 94.848, P < 0.0001) and BRVO (429 ± 131.833 vs. 309.926 ± 65.365, P = 0.0001) groups post-treatment; interruption of the ellipsoid zone was significantly different in the CRVO group after treatment (P = 0.046), while DRIL decreased significantly in the BRVO group (P = 0.018). FFA demonstrated significant improvement in late macular leakage after treatment in both the CRVO (P < 0.001) and BRVO (P < 0.001) groups. All initial and final data obtained from OCTA, SD-OCT, and FFA are presented in Table 2. Figure 1 depicts the enlargement of the FAZ, the reduction in foveal vessel densities, and the decrease in foveal thickness in a representative patient.
OCTA and OCT images of a typical case of ME secondary to RVO before therapy and final visit after therapy are shown. The upper row represents the enlargement of FAZ and the reduction of foveal vessel densities; the lower row represents the decrease of foveal thickness. OCTA, optical coherence tomography angiography; OCT, optical coherence tomography; ME, macular edema; RVO, Retinal Vein Occlusion; FAZ, foveal avascular zone
As show in Table 3, this study confirmed that patients with ellipsoid zone or external limiting membrane integrity had lower BCVA values compared to those without an ellipsoid zone or external limiting membrane integrity (0.663 ± 0.344 vs. 1.182 ± 0.524 logMAR, P < 0.001; 0.809 ± 0.505 vs. 1.138 ± 0.505 logMAR, P = 0.024). Patients with DRIL had higher BCVA values (0.955 ± 0.429 vs. 0.608 ± 0.223 logMAR, P = 0.01). The effects of macular foveal hyperreflective dots, an epimacular membrane, or vitreomacular traction and serous retinal detachment on visual acuity were not statistically significant (1.004 ± 0.679 vs. 0.983 ± 0.378 logMAR, P = 0.892; 1.217 ± 0.542 vs. 0.963 ± 0.524 logMAR, P = 0.272; 1.12 ± 0.454 vs. 0.941 ± 0.551 logMAR, P = 0.27, respectively). Figure 2 showed alleviated macular edema, reduced foveal thickness, and rebuilt ellipsoid zone in three typical cases after treatment.
The OCT images of three typical cases before therapy and final visit after therapy showed macular microstructure. OCT images of RVO (a, c, e) manifested macular edema, increased foveal thickness and ellipsoid zone interrupted. IVR and IVTA treatment (b, d, f) successfully alleviated macular edema, reduced foveal thickness, and rebuilt ellipsoid zone. OCT, optical coherence tomography; RVO, Retinal Vein Occlusion; IVR, intravitreal ranibizumab; IVTA, intravitreal triamcinolone acetonide
The multivariable regression identified the factors most relevant to BCVA (Table 4). BCVA was associated most commonly with ellipsoid zone integrity (P = 0.022).
The BCVA in eyes treated with IVR and IVTA was significantly decreased compared with IVR only in BRVO group (P = 0.021). However, the combination of IVR + IVTA significantly improved intraocular pressure (IOP) compared with IVR only in BRVO group (P = 0.037). The combination of IVR + IVTA significantly decreased macular foveal hyperreflective dots compared with IVR only in BRVO group (P = 0.02). There were no significant differences in secondary catract between the IVR and IVR + IVTA groups in both CRVO and BRVO. The details were shown in Table 5.
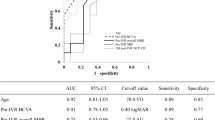
Supplemental Fig. 1 showed the mean change of BCVA and IOP over time for the groups treated.
Discussion
In this study, we chose ranibizumab as an anti-VEGF agent. Ranibizumab has been approved by the State Medical Products Administration for the treatment of visual impairment caused by ME secondary to RVO, including BRVO or CRVO, and has become the only anti-VEGF drug with indication for RVO in China. By choosing ranibizumab as the treatment for RVO, patients can enjoy certain medical insurance reimbursement in China. Previous studies have reported that some RVO patients do not respond sensitively to anti-VEGF drugs [19]. For RVO patients who are not sensitive to anti-VEGF drugs, intravitreal steroid injections may be beneficial. Triamcinolone acetonide has been widely used in the treatment of ME [20]. Previous studies have shown that IVTA 0.4 mg had little difference in visual acuity improvement in patients with ME, while 4 mg had an increased risk of ocular hypertension [21]. We chose 1 mg as the therapeutic dose. In addition, no patient had elevated intraocular pressure in our study, so 1 mg is a relatively safe dose that is not likely to cause elevated IOP. Our study confirmed that the effectiveness of IVR with or without IVTA in the treatment of ME caused by RVO, and visual acuity and the macular structure were significantly improved after treatment.
In the current study, we measured the FAZ area and foveal vessel densities with OCTA in RVO patients to evaluate the effect of IVR with or without IVTA on retinal vascular perfusion. The FAZ area was enlarged after IVR with or without IVTA. This was similar to other reports. Suzuki et al. reported enlargement of the FAZ region after 6 months of intravitreal bevacizumab or aflibercept treatment [22]. We speculated that FAZ remodeling might indicate the dynamic changes of intraocular vascular flow in BRVO patients, but the mechanism of FAZ enlargement after anti-VEGF therapy has not been definitively determined. After anti-VEGF therapy, intravitreal anti-VEGF drugs can only delay the release of VEGF, but the situation of retinal ischemia and hypoxia and retinal vessel reperfusion still exists, so even after anti-VEGF therapy, the FAZ is still expanded. Campochiaro et al. [23] also found that monthly injections of anti-VEGF drugs could only delay the release of VEGF, but could not prevent the process in the long term. This also suggested that blood perfusion in the macular area may also be a feature of RVO’s transition to hypoxia with the progression of RVO [24].
We also found that the foveal vessel density was decreased after treatment. This result is similar to previous reports, which reported that anti-VEGF therapy may aggravate retinal ischemia due to decreased superficial blood flow density [25, 26]. However, some studies have shown that anti-VEGF therapy has a positive effect on retinal vascular perfusion and can slow down the retinal deterioration of vascular hyperfusion [27], but there is no unified conclusion on the effect of anti-VEGF therapy on the blood flow state of the posterior pole of the retina. RVO causes retinal ischemia and induces increased release of VEGF factors, which in turn aggravates retinal ischemia and hypoxia, which is also a positive feedback loop in the pathological process of RVO. Anti-VEGF therapy can block the positive feedback loop, slow down the progression of anperfusion, and stabilize the macular blood flow state, but it does not significantly improve the macular blood flow state in most RVO patients. Mane et al. [28] showed that although capillaries existing above the cystic space could appear in OCTA after edema subsided, it was unlikely that capillaries in the macular area would undergo reperfusion after anti-VEGF treatment. Winegarner et al. [29] also showed that the retinal capillary perfusion status would not be restored in patients with RVO, even if ME was recovered.
In addition, SSADA software is able to detect red blood cells of blood vessels, but only those that move within a certain range of speed. If the blood flow is too slow or too fast, the vessels will not show up in OCT images. The blood flow rate in these non-perfused areas is very slow and is lower than the detection limit of OCTA 0.3 mm/s. Therefore, a partial vascular signal was not detected [23, 25, 30, 31].
With SD-OCT, some structural improvements in the retina were detected after IVR with or without IVTA. The foveal thickness decreased after IVR with or without IVTA. The structure of retinal inner layers, ellipsoid zone, and external limiting membrane were also significantly improved. Previous studies have shown that the retinal inner layers, the ellipsoid zone, and the external limiting membrane are predictive factors for visual outcomes after anti-VEGF therapy for RVO [32].
Our study found significant improvement in visual acuity after treatment and further confirmed that these structural improvements were closely related to visual outcomes. The influence of ME on visual function is mainly due to the damage to photoreceptors, the damage to neurons in the retinal inner layers, and the impairment of light signal transmission caused by ME itself. The state of macular anperfusion is related to vision, and the state of photoreceptors is also involved in the process of visual impairment [33]. Severe BRVO-ME can lead to a breakdown of the retinal blood barrier, increased fluid leakage, and irreversible photoreceptor damage. Therefore, anti-VEGF treatment will not improve visual acuity even after a decrease in ME. DRIL refers to the inability to recognize the ganglion cell-inner plexus complex and any boundary between the inner and outer plexus layers. DRIL is a useful biomarker for visual acuity in patients with RVO-ME.
On FFA, disruption of the perifoveal capillary arcade and macular ischemia was not significantly decreased after treatment, which was consistent with the enlarged FAZ and decreased foveal vessel densities. Treatment with ranibizumab and triamcinolone acetonide injections was not sufficient to completely prevent the progression of posterior retinal ischemia. Peripheral ischemia was not significantly decreased after treatment, which suggested that retinal photocoagulation was necessary.
In the present study, the result of multivariable regression demonstrated that BVCA post IVR + IVTA was associated with ellipsoid zone integrity. Previous studies have reported that the close relationship between ellipsoid zone integrity and BCVA in various ocular diseases including proliferative diabetic retinopathy, macular hole and epiretinal membrane [34,35,36]. The restoration of ellipsoid zone integrity suggested that the improvement of photoreceptor cells and visual acuity.
Our research has identified that patients with CRVO and BRVO exhibit different responses to treatment. The main differences in the pathological mechanisms between BRVO and CRVO lie in the sites and severity of onset, as well as the way and extent to which they affect different regions of the retina. CRVO involves the blockage of the central retinal vein, leading to restricted blood circulation in a wide area of the retina. This can result in extensive retinal edema, hemorrhage, and ischemia, ultimately causing severe impairment of retinal function. On the other hand, BRVO typically occurs at the branching points between the central retinal artery and one or multiple branches of the retinal vein, obstructing blood flow in that specific region. BRVO often manifests as retinal hemorrhage, edema, and ischemic changes at the bifurcation of the central retinal artery and vein, leading to functional impairment in the affected retinal area. Therefore, the pathology induced by CRVO is more severe, resulting in a poorer response to treatment with intravitreal anti-VEGF injections with or without intravitreal triamcinolone acetonide compared to BRVO. In our study, the IOP of the eyes after intraocular injection did not rise (≥ 25mmHg) and required immediate treatment.
The combination of IVR + IVTA significantly improved visual acuity compared with IVR only in BRVO group. Fan C et al. reported that there was no significant difference of mean BVCA between IVR + IVTA group and IVR group in CRVO patients [15]. The findings of our study differ from previous research, and we believe the potential reasons for this discrepancy are as follows: firstly, our study is retrospective in nature, which may introduce some selection bias in the choice of patients who received intravitreal ranibizumab with or without triamcinolone acetonide. Secondly, the sample size is relatively small, which might not be representative enough and could impact the accuracy of the study’s conclusions. We found there were no significantly difference in the changes of OCT features, OCTA features, and FFA features between IVR and IVR with IVTA. In terms of the lens status in patients at baseline and the last visit, we have taken into account the potential impact of corticosteroid treatment, specifically triamcinolone acetonide (TA), on cataract progression. We have assessed the lens status at both baseline and the last visit for all patients in our study. Some patients had pre-existing cataracts to a certain extent before treatment. During the six-month follow-up treatment period, no significant worsening of cataracts was observed in any of the patients.
In conclusion, both IVR and IVR + IVTA can significantly improve the central vision, macular structure, and functions. Simultaneous IVR with IVTA can significantly decrease the injection number compared with IVR only. There was no significant difference in efficacy between the two treatments group.
The limitations of this study were the small number of patients enrolled and the limited flow density and FAZ analysis area (6 × 6 mm). In addition, signal blocking due to retinal surface hemorrhaging, motion artifacts due to solid vision dysplasia, projection artifacts, and failure to completely eliminate segmentation errors may affect the results of the observation indicators. In addition, we evaluated only superificial foveal vessel density related parameters, but not the deep and intermediate capillary plexuses. Therefore, studies using different devices and algorithms as well as larger sample sizes are needed to further verify the results of this study, so there can be a more comprehensive understanding of the microvascular changes in RVO patients.
Conclusions
In summary, our research found that both IVR and IVR + IVTA can significantly enhance central vision, macular anatomy, and function. Simultaneous IVR with IVTA can significantly reduce the number of injections compared to IVR alone. There was no significant difference in effectiveness between the two treatment groups.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- RVO:
-
Retinal vein occlusion
- BRVO:
-
Branch retinal vein occlusion
- ME:
-
Macular edema
- VEGF:
-
Vascular endothelial growth factor
- IOP:
-
Intraocular pressure
- CRVO:
-
Central branch retinal vein occlusion
- IVR:
-
Intravitreal ranibizumab
- IVTA:
-
Triamcinolone acetonide injections
- FFA:
-
Fundus fluorescein angiography
- SDOCT:
-
Spectral domain optical coherence tomography
- OCTA:
-
Optical coherence tomography angiography
- BCVA:
-
Best corrected visual acuity
- DRIL:
-
Disorganization of the retinal inner layers
References
Khayat M, Williams M, Lois N. Ischemic retinal vein occlusion: characterizing the more severe spectrum of retinal vein occlusion. Surv Ophthalmol. 2018;63(6):816–50.
Noma H, Mimura T, Eguchi S. Association of inflammatory factors with macular edema in branch retinal vein occlusion. JAMA Ophthalmol. 2013;131(2):160–5.
Rezar-Dreindl S, Eibenberger K, Pollreisz A, Bühl W, Georgopoulos M, Krall C, et al. Effect of intravitreal dexamethasone implant on intra-ocular cytokines and chemokines in eyes with retinal vein occlusion. Acta Ophthalmol. 2017;95(2):e119–27.
Zhang S, An N, Ha W, Zhang S, Hu X, Ma A, et al. Factors correlated with the resolution of macular oedema after one dose injection of intravitreal triamcinolone acetonide treatment in branch retinal vein occlusion. J Int Med Res. 2016;44(3):685–97.
Floman N, Zor U. Mechanism of steroid action in ocular inflammation: inhibition of prostaglandin production. Invest Ophthalmol Vis Sci. 1977;16(1):69–73.
Ishibashi T, Miki K, Sorgente N, Patterson R, Ryan SJ. Effects of intravitreal administration of steroids on experimental subretinal neovascularization in the subhuman primate. Arch Ophthalmol. 1985;103(5):708–11.
Bandi N, Kompella UB. Budesonide reduces vascular endothelial growth factor secretion and expression in airway (Calu-1) and alveolar (A549) epithelial cells. Eur J Pharmacol. 2001;425(2):109–16.
Sze PY, Iqbal Z. Glucocorticoid action on depolarization-dependent calcium influx in brain synaptosomes. Neuroendocrinology. 1994;59(5):457–65.
Wilson CA, Berkowitz BA, Sato Y, Ando N, Handa JT, de Juan E. Jr. Treatment with intravitreal steroid reduces blood-retinal barrier breakdown due to retinal photocoagulation. Arch Ophthalmol. 1992;110(8):1155–9.
Penfold PL, Wen L, Madigan MC, King NJ, Provis JM. Modulation of permeability and adhesion molecule expression by human choroidal endothelial cells. Invest Ophthalmol Vis Sci. 2002;43(9):3125–30.
Kiddee W, Trope GE, Sheng L, Beltran-Agullo L, Smith M, Strungaru MH, et al. Intraocular pressure monitoring post intravitreal steroids: a systematic review. Surv Ophthalmol. 2013;58(4):291–310.
Veritti D, Di Giulio A, Sarao V, Lanzetta P. Drug safety evaluation of intravitreal triamcinolone acetonide. Expert Opin Drug Saf. 2012;11(2):331–40.
Hida T, Chandler D, Arena JE, Machemer R. Experimental and clinical observations of the intraocular toxicity of commercial corticosteroid preparations. Am J Ophthalmol. 1986;101(2):190–5.
Terasaki H, Ogura Y, Kitano S, Sakamoto T, Murata T, Hirakata A, et al. Management of diabetic macular edema in Japan: a review and expert opinion. Jpn J Ophthalmol. 2018;62(1):1–23.
Fan C, Wang Y, Ji Q, Zhao B, Xie J. Comparison of clinical efficacy of intravitreal ranibizumab with and without triamcinolone acetonide in macular edema secondary to central retinal vein occlusion. Curr Eye Res. 2014;39(9):938–43.
Hirano Y, Suzuki N, Tomiyasu T, Kurobe R, Yasuda Y, Esaki Y et al. Multimodal Imaging of Microvascular Abnormalities in retinal vein occlusion. J Clin Med. 2021, 10(3).
Cicinelli MV, Sadiq SA, Mishra S, Jampol LM, Mirza RG. Multimodal Imaging Characterization of Arteriolosclerotic Plaques in retinal vein occlusion. Ophthalmic Surg Lasers Imaging Retina. 2021;52(12):650–7.
Remolí Sargues L, Montero Hernández J, Navarro Palop C, Monferrer Adsuara C, Castro Navarro V, Cervera Taulet E. Multimodal imaging of two cases of retinal vein occlusion secondary to Waldenstrom macroglobulinemia. Eur J Ophthalmol. 2022;32(3):Np50–5.
Sun Z, Zhou H, Lin B, Jiao X, Luo Y, Zhang F, et al. Efficacy and Safety of Intravitreal Conbercept Injections in Macular Edema Secondary to retinal vein occlusion. Retina. 2017;37(9):1723–30.
Dikmetas O, Kuehlewein L, Gelisken F. Rebound Phenomenon after Intravitreal Injection of Triamcinolone Acetonide for Macular Edema. Ophthalmologica. 2020;243(6):420–5.
Ip MS, Scott IU, VanVeldhuisen PC, Oden NL, Blodi BA, Fisher M, et al. A randomized trial comparing the efficacy and safety of intravitreal triamcinolone with observation to treat vision loss associated with macular edema secondary to central retinal vein occlusion: the Standard Care vs corticosteroid for retinal vein occlusion (SCORE) study report 5. Arch Ophthalmol. 2009;127(9):1101–14.
Suzuki N, Hirano Y, Tomiyasu T, Esaki Y, Uemura A, Yasukawa T, et al. Retinal hemodynamics seen on Optical Coherence Tomography Angiography before and after treatment of retinal vein occlusion. Invest Ophthalmol Vis Sci. 2016;57(13):5681–7.
Campochiaro PA, Bhisitkul RB, Shapiro H, Rubio RG. Vascular endothelial growth factor promotes progressive retinal nonperfusion in patients with retinal vein occlusion. Ophthalmology. 2013;120(4):795–802.
Hayreh SS, Zimmerman MB, Podhajsky P. Incidence of various types of retinal vein occlusion and their recurrence and demographic characteristics. Am J Ophthalmol. 1994;117(4):429–41.
Shimura M, Yasuda K. Macular ischaemia after intravitreal bevacizumab injection in patients with central retinal vein occlusion and a history of diabetes and vascular disease. Br J Ophthalmol. 2010;94(3):381–3.
Huang ZL, Lin KH, Lee YC, Sheu MM, Tsai RK. Acute vision loss after intravitreal injection of bevacizumab (avastin) associated with ocular ischemic syndrome. Ophthalmologica. 2010;224(2):86–9.
Mir TA, Kherani S, Hafiz G, Scott AW, Zimmer-Galler I, Wenick AS, et al. Changes in Retinal Nonperfusion Associated with suppression of vascular endothelial growth factor in retinal vein occlusion. Ophthalmology. 2016;123(3):625–e341.
Mané V, Dupas B, Gaudric A, Bonnin S, Pedinielli A, Bousquet E, et al. Correlation between Cystoid spaces in Chronic Diabetic Macular Edema and Capillary Nonperfusion detected by Optical Coherence Tomography Angiography. Retina. 2016;36(Suppl 1):S102–10.
Winegarner A, Wakabayashi T, Fukushima Y, Sato T, Hara-Ueno C, Busch C, et al. Changes in Retinal Microvasculature and Visual Acuity after Antivascular endothelial growth factor therapy in retinal vein occlusion. Invest Ophthalmol Vis Sci. 2018;59(7):2708–16.
Sabet-Peyman EJ, Heussen FM, Thorne JE, Casparis H, Patel SJ, Do DV. Progression of macular ischemia following intravitreal bevacizumab. Ophthalmic Surg Lasers Imaging. 2009;40(3):316–8.
Mansour AM, Bynoe LA, Welch JC, Pesavento R, Mahendradas P, Ziemssen F, et al. Retinal vascular events after intravitreal bevacizumab. Acta Ophthalmol. 2010;88(7):730–5.
Chatziralli I, Dimitriou E, Lambadiari V, Kazantzis D, Kapsis P, Theodossiadis G et al. The impact of Laboratory findings and Optical Coherence Tomography biomarkers on response to Intravitreal Anti-VEGF Treatment in patients with Diabetic Macular Edema. Semin Ophthalmol. 2022:1–8.
Ghashut R, Muraoka Y, Ooto S, Iida Y, Miwa Y, Suzuma K, et al. Evaluation of Macular Ischemia in eyes with central retinal vein occlusion: an Optical Coherence Tomography Angiography Study. Retina. 2018;38(8):1571–80.
Iacono P, Parodi MB, Scaramuzzi M, Bandello F. Morphological and functional changes in recalcitrant diabetic macular oedema after intravitreal dexamethasone implant. Br J Ophthalmol. 2017;101(6):791–5.
Sevgi DD, Yee PS, Srivastava SK, Le TK, Abraham JR, Reese J, et al. Longitudinal Ellipsoid Zone dynamics after Macular Hole Repair in the Discover Study. Structure-Function Assess Retina. 2021;41(5):915–20.
Tuifua TS, Abraham JR, Srivastava SK, Kaiser PK, Reese J, Ehlers JP. Longitudinal ellipsoid zone and Outer Retinal Integrity Dynamics after Epiretinal membrane surgery. Retina. 2022;42(2):265–73.
Acknowledgements
Not Applicable.
Funding
This work was supported by the Natural Science Foundation of Hunan Province (No.2023JJ30748, No.2023JJ30003), Scientific Research Project of Hunan Provincial Health Commission (No.C202307027337, No.D202307028349), the Science and Technology Program of Changsha (No.kh2302036), the Natural Science Foundation of Changsha (No. kq2208494).
Author information
Authors and Affiliations
Contributions
Chun Ding conceived and designed the study. Xianghui Deng collected the patient’s data. Shengguo Li, Jun Zeng reviewed the patient data. Nan Wang, Jingling Zou analyzed the data and provided interpretation. Nan Wang, Jingling Zou wrote the main manuscript. Chun Ding revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This was a retrospective study conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Second Xiangya Hospital, which waived the written informed consent because of the study’s retrospective design.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, N., Zou, J., Li, S. et al. Multimodal imaging to distinguish microvascular and morphological changes in retinal vein occlusion after intravitreal ranibizumab with or without triamcinolone acetonide injection. BMC Ophthalmol 24, 354 (2024). https://doi.org/10.1186/s12886-024-03619-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-024-03619-y