Abstract
Background
Although school screenings identify children with vision problems and issue referrals for medical treatment at an ophthalmic hospital, the effectiveness of this approach remains unverified.
Objective
To investigate the impact of ophthalmic clinical services on the onset and progression of myopia in preschool children identified with vision impairment.
Methods
Using data from the Shanghai Child and Adolescent Large-scale Eye Study (SCALE), this retrospective cohort study evaluated the visual development of children from three districts—Jing’an, Minhang, and Pudong—which are representative of geographic diversity and economic disparity in Shanghai’s 17 districts. Initially, in 2015, the study encompassed 14,572 children aged 4–6 years, of whom 5,917 needed a referral. Our cohort consisted of 5,511 children who had two or more vision screenings and complete personal information over the follow-up period from January 2015 to December 2020. We divided these children into two groups based on their initial spherical equivalent (SE): a High-risk group (SE > -0.5 D) and a Myopia group (SE ≤ -0.5 D). Within each of these groups, we further categorized children into Never, Tardily, and Timely groups based on their referral compliance to compare the differences in the occurrence and progression of myopia. Cox proportional models were applied to estimate hazard ratios (HRs) for myopia incidence per person-years of follow-up in High-risk group. Generalized additive models(GAM) was used to calculating the progression for annual spherical equivalent changes in all children.
Results
Of the 5,511 preschool children (mean age, 5.25 years; 52.24% male) who received a referral recommendation, 1,327 (24.08%) sought clinical services at an ophthalmic hospital. After six years of follow-up, 65.53% of children developed myopia. The six-year cumulative incidence of myopia in the Never, Tardily, and Timely groups was 64.76%, 69.31%, and 57.14%, respectively. These percentages corresponded to hazard ratios (HRs) of 1.31 (95% CI, 1.10–1.55) for the Tardily group and 0.55 (95% CI, 0.33–0.93) for the Timely group, compared with the Never group. The HRs were adjusted for age, sex, and SE at study entry. Interestingly, the Timely group showed significantly less SE progression than the other groups (P < 0.001), and SE progression was higher in the High-risk group (-0.33 ± 0.37D/year) than in children with myopia (-0.08 ± 0.55D/year).
Conclusion
Timely utilization of ophthalmic clinical services among children aged 4 to 6 years who fail school vision screenings can significantly reduce the incidence of myopia and slow SE progression.
Similar content being viewed by others
Introduction
Myopia, broadly accepted as one of the most prevalent ocular diseases, presents a concern of international magnitude [1,2,3]. A predictive study suggests that by the year 2050, myopia will afflict approximately 4758 million individuals, constituting nearly 49.8% of the global population [4]. There is a high prevalence of myopia, 80–90%, in young adults in East Asia [5]. Particularly in China, forecasts indicate that by the year 2050, the prevalence of myopia is expected to reach an estimated 84% among children and adolescents ages 3 to 19 years [6]. The foremost strategies to prevent the onset and slow the progression of myopia primarily involve public health initiatives, pharmacological approaches, and optical devices [7], such as increased outdoor time [8,9,10,11], reducing activities done at a short working distance [12,13,14], Chinese eye exercises [15, 16], low-dose atropine [17, 18], and repeated low-level red-light (RLRL) [19]. In China, the primary focus of prevention strategies lies in curbing the incidence of myopia, with secondary and tertiary prevention measures aimed at decelerating the progression of the condition enforced as a governmental imperative. Given the escalating prevalence of high myopia and subsequent severe complications, the deployment of primary prevention tactics are of utmost importance and are privileged within the existing national myopia control plan in China [20]. The distinct features of the myopia epidemic underscore the principal challenges: ensuring timely correction for myopic children during their developmental phase. This necessitates the implementation of efficacious school screening programs and expedited referrals for optical correction and myopia management [21].
The Shanghai Child and Adolescent Large-scale Eye Study (SCALE) is a citywide, prospective survey conducted throughout schools, aimed at addressing ocular health concerns in children aged between 4 and 14 years across Shanghai. In instances where school vision screenings detected abnormal visual acuity or refraction, a referral was initiated. This enabled children, under parental guidance, to visit hospitals for more intensive re-examinations of visual acuity, cycloplegia, and subjective refraction. These assessments were performed by experienced ophthalmologists or optometrists skilled in the diagnosis and treatment of ocular conditions within Shanghai, China. All pertinent study data were diligently compiled within an electronic database [22]. The utilization of health services has been proved to be effective in controlling of many diseases, such as smoking [23], early cancer [24], and chronic disease [25]. Nonetheless, only a handful of studies have influence of referral on the occurrence and progression of myopia. Myopia progression is irreversible and there is no cure [26]. The significance of curbing and managing myopia during early childhood cannot be understated. It is also well recognized that myopia occurring at an earlier age in childhood is associated with a faster myopia progression and higher degree of myopia in adult life [5, 27,28,29]. Hence, our study aims to investigate the impact of utilizing ophthalmic clinical health services post-school vision screening, on mitigating the onset and progression of myopia among preschool children.
Methods
Data source and study population
Our research was based on the SCALE study. SCALE represents the most extensive investigation into the prevalence of myopia among the Shanghai children and adolescent population aged 4–14. Since 2012, community doctors have annually examined children and adolescents from all 17 districts and counties in Shanghai, China. The Detailed methods of the study were previously reported [22]. In brief, if a child’s visual acuity or refraction was determined to be abnormal during the school vision screening, the child would fail the screening and would be recommended for further evaluation. Students who failed the screening would receive a paper referral notice, but they were not compelled to do so, nor did they receive further phone calls or text message reminders.
According to the referral criteria in the SCALE study, children meeting the following conditions were encouraged to visit the designated hospital for further examination and, if necessary, management:1) The uncorrected visual acuity of either eye is abnormal(for ages 4–5 years, UCVA < 0.6, and for age 6 years, UCVA < 0.8). 2)The uncorrected visual acuity is normal but have a high risk of myopia according to the spherical equivalent (SE). These children have normal UCVA of both eyes (for 4–5 years, UCVA ≥ 0.6, for 6 years, UCVA ≥ 0.8) and SE of either eye < 0.00D. These children will also need regular referrals.
Since 2015, the data quality of the Shanghai Child and Adolescent Large-scale Eye Study (SCALE) has significantly improved. Owing to the extensive size of the database, we selected Jing’an, Minhang, and Pudong districts for our study. These districts represent the geographic location and economic disparities amongst Shanghai’s 17 districts. Figure 1 represents the process of selecting the study subjects.
Definition
Spherical equivalent (SE) was defined as the sum of the spherical power and half of the cylinder. Myopia was determined as a SE of -0.5D or less without cycloplegia. Based on the initial SE, children were categorised into two groups for a six-year observational study on visual development: the High-risk group (SE > -0.5D) and the Myopia group (SE ≤ -0.5D). As per the guidelines in Shanghai, students failing school vision screenings are recommended to seek ophthalmic clinical referral services within three months. Accordingly, we further bifurcated each subgroup into three groups, based on the compliance with this referral recommendation: Never group—children who did not seek ophthalmic clinical referral services during the six-year follow-up period; Tardily group—children who sought such services one or more times between three months post the initial vision screening and the end of the follow-up period; and Timely group—children who promptly sought ophthalmic clinical referral services within three months post referral recommendation issuance.
Data analysis
The statistical analyses for this study were performed using SAS version 9.4, and Sigmaplot 14.0 was employed for generating graphical figures. Normality of the data sets was assessed using the Kolmogorov-Smirnov test. Despite some variables conforming to the normal distribution, due to the large sample size, we expressed results as mean ± standard deviation (SD) or as a percentage. Depending on the data type and distribution, the age and sex among the groups were compared employing the Kruskal-Wallis test, Fisher’s exact test, and the χ2 test. The screening frequency and spherical equivalent (SE) were compared using the Kruskal-Wallis test and analysis of variance. In this cohort study, the incidence of myopia was calculated per person-years of follow-up. Cox proportional hazard models were utilized to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for the incidence of myopia per referral compliance group, with non-referred children serving as the reference. Initially, unadjusted models were calculated, followed by fully adjusted models accounting for age, sex, and initial SE. The dependent variable of this study is non normal data, the mean rate of change in SE was compared among children with different initial age, sex and SE by using generalized additive models(GAM). The utilization of Generalized Additive Models (GAM) facilitated error pattern specification and proved an adequate fit for datasets with non-normal distributions, yielding lower and more reliable p-values [30]. Since our data is non-normal and the relationship between dependent and independent variables is also not linear, GAM provides a more effective analytical method than traditional linear models.
Results
Baseline characteristics
Table 1 presents the baseline characteristics of the 5,511 preschool children included in this study, categorized according to referral compliance. While the compliance rate was 24.08%, the proportion of timely referrals stood at a mere 2.03% (112 out of 5,511). There was no significant difference in compliance rates between the High-risk and Myopia groups (χ2 = 0.14, P = 0.71). The study children had a mean age of 5.25 ± 0.75 years, with 52.24% being boys. The mean spherical equivalent (SE) was − 0.87 ± 1.29D. At the outset of the follow-up period, there were differences in age and SE among children in each subgroup. However, the sex distribution within the Myopia group showed no significant difference.
Risk estimates of the association between referral compliance and incident myopia
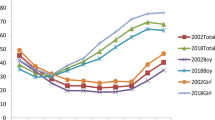
Among children at high risk for myopia, the mean follow-up period was 5.00 ± 0.94 years, with each child undergoing an average of 4.17 ± 1.25 examinations. Over the course of six years, 65.53% of children developed myopia. The six-year cumulative incidence of myopia was lowest in the Timely group (57.14%), compared to the Never (64.76%) and Tardily (69.31%) groups (Fig. 2, Picture A). The median survival times for the Never, Tardily, and Timely groups were 4.92 years (95% CI, 4.83–4.92), 4.50 years (95% CI, 4.00-4.92), and 5.83 years (95% CI, 4.42–5.92), respectively. A total of 1,597 incidences of myopia were recorded over 12,185 person-years. The incidence of myopia (per 1,000 person-years) differed according to referral compliance: 129.53 for the Never group, 138.34 for the Tardily group, and 118.42 for the Timely group (Table 2). When compared with children who never sought a referral, the hazard ratios (HRs) for cumulative incidence of myopia were 1.31 (95% CI, 1.10–1.55; P < 0.001) in the Tardily group and 0.67 (95% CI, 0.33–0.93; P < 0.05) in the Timely group.
Risk estimates of the association between referral compliance and progression of myopia
Among all 2,437 participants at high risk of myopia, the average rate of change in the spherical equivalent (SE) was − 0.33 ± 0.37D/year. The annual SE progression in the Timely group (-0.28 ± 0.37D/year) was significantly lower than that of the Never group (-0.32 ± 0.37D/year) and the Tardily group (-0.36 ± 0.37D/year) at later ages (P = 0.006) (Fig. 2, Picture B). There was a rapid increase in SE among children at high risk of myopia, indicating a severe trend (Fig. 2, Picture C). Conversely, children in the Myopia group experienced an initial rebound followed by a decline over the six-year follow-up period (Fig. 2, Picture D). The mean SE progression in children who promptly utilized ophthalmic clinical services after school vision screening (0.07 ± 0.60D/year) was significantly slower compared to those who never sought referral (-0.06 ± 0.57D/year) or were tardy in doing so (-0.14 ± 0.50D/year) at later ages (P = 0.005) (Table 2).
Discussion
In this extensive, prospective, school-based cohort study, we discovered that a timely utilization of ophthalmic clinical services post school vision screenings in preschool children aged 4 to 6 years with vision disorders can mitigate the onset and progression of myopia.
During the 2015–2020 period, 24.08% of the 5,511 preschool children who received referral notice following failed school vision screenings attended follow-up appointments at the hospital for additional examinations at least once within the six-year follow-up period. However, only a meagre 2.03% of children required to seek ophthalmic clinical services did so within the stipulated three months. To our knowledge, no other cohort studies have examined the correlation between ophthalmic clinical service utilization in preschool children and the subsequent development and progression of myopia. In our follow-up study, we found that student age, visual health status, family annual income, and the presence of referral prompts in schools or community health centers all impact the utilization of ophthalmic clinical health services. The primary factor contributing to the current low compliance is the absence of a robust referral system [31].
We found that children who were referred for eye examinations at preschool, but did so tardily, presented the highest risk for developing myopia—even outstripping those who never sought a referral. Generally, these children sought medical treatment after a long interval—on average, 555 days—following their referral recommendations. We hypothesize that although these children had previously utilized ophthalmic clinical services, their vision issues by that time were severe, resulting in higher myopia incidence and progression rates compared to other children.
Constrained by the challenge of insufficient cooperation and a low follow-up rate among young children, only a handful of studies have undertaken a longitudinal observation to evaluate the likelihood of myopia in preschool children [32]. Our study’s results provide groundwork for comparing myopia prevalence rates in preschool children. Myopia is commonly seen among school-aged children, whereas its prevalence is relatively low in children aged 6 years or younger. However, congruent with other longitudinal studies, we identified a higher rate of vision disorders among preschool children. In this study, we discovered that 35.08% of children aged between 4 and 6 years exhibited visual abnormalities at the commencement of the follow-up period. Further, 13.98% were in high-risk groups and 21.1% already had myopia. The prevalence rate of an Vision In Preschoolers (VIP) study-targeted vision disorders among all children aged 3–5 years with sampling weights incorporated was 21.4% [33]. There were 17.0% children aged 3 to 6 years identified in having the visual abnormalities in Hong Kong preschool and 6.32% were myopes [34]. The prevalence of myopia under 6 years in Germany was lower than 5.0%, and remained virtually unchanged over a period of approximately 10 years [35]. Among children with high risk of myopia, 65.53% develop myopia during 6 years of follow-up. A 6-year follow-up of the Sydney Myopia Study revealed a mean annual incidence of myopia of 2.2% in the younger cohort among 1765 children with a mean age of 6.7 years at baseline [36]. In previous reports, the myopia rate in China was generally higher than that of other countries [6, 37], and the subjects of this study were children who were already visually impaired. It has been reported that early achievement of emmetropia is a risk factor for subsequent progression to myopia [38]. Most importantly, the refractive data in this study are all obtained without cycloplegia. One current study limitation is the likelihood of overestimating myopia prevalence due to children’s refractive status being assessed without cycloplegia. Administering cycloplegia in children requires substantial effort and resources, which were unavailable in our protocol. Furthermore, significant parental resistance to cycloplegia exists in this region, making it unrealistic to execute the study within the preset timeframe and resource allocation required for cycloplegia. The focus of this study isn’t to pinpoint an accurate diagnosis of myopia, but to review the significance of using commonplace health services to control and prevent myopia during large population mass screenings. Despite the potential for overestimating myopia prevalence, the application of noncycloplegic refraction for school screenings is fitting, given its inherent capability to effectively identify all instances of myopia [39].
In this study, we documented the longitudinal shifts in spherical equivalent (SE) refractive errors among Chinese preschoolers diagnosed with visual impairments. The mean rate of SE change in high-risk children and those with myopia were − 0.33 ± 0.37D/year and − 0.08 ± 0.55D/year, respectively. The Northern Ireland Childhood Errors of Refraction (NICER) reported that the estimated annual median change of participants with 6–7 years old was − 0.23D over the six-year period [40]. Hu Y et al. [41] reported that the mean rate of SE change in the children aged 5.12 years(IQR, 4.12–5.76 years) with myopia was − 0.59-0.47D/year. Some studies have revealed that younger children or children with greater initial myopic refractive errors are at a greater risk of myopia progression [41,42,43,44], especially in school-aged children [45, 46]. In our study, the myopia progression rate was lower among children referred timely, and children with myopia at study entry. The research results of Hu Y et al. [41] and Shih YF, et al. [47] also showed that the risk of myopia progression does not increase with the severity of initial SE in preschool children. The refractive development of human eyes represents a dynamic process, as ocular biometric parameters undergo changes from birth, resulting in corresponding alterations in the refractive state [48]. These results may not be exactly comparable to our study findings because the age and refraction distributions of the study populations were different. Nonetheless, the findings suggest that preschool myopia likely follows a distinct evolutionary course. Undeniably, further study is required to fully understand the mechanism of myopic regression [47].
The mitigated occurrence and progression of myopia in the Timely referred group might be attributed to their timely utilization of ophthalmic health services. Such services encompass not only health education initiatives like enhancing outdoor activities and maintaining proper reading and writing posture but also corrective interventions including eyeglasses prescription and medication usage. Moreover, physicians often require perpetual vigilance and frequent follow-ups from parents. This study, along with several other population-based researches, conveys that children with elevated risk should receive preventative guidance and close monitoring for the onset of myopia, so that necessary therapeutic interventions can be timely introduced [2, 7].
Compared to the school vision screening program, the referral mechanism has not been given sufficient attention in Shanghai. Our results provide strong evidence for regions to continue promoting and implementing referral work, demonstrating the necessity of promoting the utilization rate of ophthalmic clinical health services. Additionally, population screening, clinical early diagnosis, and early treatment are all extremely important aspects of disease prevention strategies in the secondary prevention stage. This study confirms that both school vision screening and early utilization of clinical health services are indispensable for children’s visual development, and the utilization of ophthalmic clinical health services after school vision screening is time-sensitive. Therefore, this study suggests that Shanghai should further enhance its well-established community-based school vision screening and referral systems to create a comprehensive and advanced primary pediatric eye care system, similar to those found in countries with more refined models [49,50,51].
There have been several cross-sectional studies of prevalence of myopia in school-aged children [52,53,54,55,56], but few longitudinal studies on the incidence and progression of myopia in China. In this large-scale, prospective, school-based cohort study, we attempted to evaluate the effectiveness of ophthalmic clinical health services on myopia prevention and control in preschool children, which is highly innovative. We also acknowledge several weaknesses in this study. This study focuses on preschool children afflicted with visual disorders, perhaps not depicting a true representation of the preschool population with healthy vision. Irregularities were present in terms of the frequency and intervals of monitoring among children, which could potentially lead to the inaccurate recording of myopia onset during the follow-up period. Moreover, this retrospective cohort study was based on the observation and analysis of child and adolescent visual development data obtained from certain areas of Shanghai from 2015 to 2020. The results of school vision screenings and hospital reviews of the study subjects represented the past situation in Shanghai. However, during the follow-up period from 2015 to 2020, there might have been unknown influences (such as the COVID-19 pandemic) affecting the study results, which remained uncertain.
Conclusion
The timely utilization of ophthalmic clinical services following school vision screenings demonstrated a significantly reduced incidence rate of both myopia and spherical equivalent (SE) progression among preschool children with vision disorders. While the prevalence of vision disorders displays some variation, this study underscores the importance of uplifting the degree of ophthalmic clinical health services utilized by preschool children.
Data availability
The datasets generated and analyzed during the current study are available. The materials used in this study are available. Requests for access to the data and materials should be directed to the corresponding author (Huijing Shi, hjshi@fudan.edu.cn).
References
Bullimore MA, Ritchey ER, Shah S, Leveziel N, Bourne RRA, Flitcroft DI. The risks and benefits of myopia control. Ophthalmology. 2021;128(11):1561–79. https://doi.org/10.1016/j.ophtha.2021.04.032
Jonas JB, Ang M, Cho P, Guggenheim JA, He MG, Jong M, et al. IMI prevention of myopia and its progression. Invest Ophthalmol Vis Sci. 2021;62(5):6. https://doi.org/10.1167/iovs.62.5.6
Baird PN, Saw SM, Lanca C, Guggenheim JA, Smith EL, Zhou XT, et al. Myopia. Nat Rev Dis Primers. 2020;6(1):99. https://doi.org/10.1038/s41572-020-00231-4
Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–42. https://doi.org/10.1016/j.ophtha.2016.01.006
Wu PC, Huang HM, Yu HJ, Fang PC, Chen CT. Epidemiology of myopia. Asia Pac J Ophthalmol (Phila). 2016;5(6):386–93. https://doi.org/10.1097/APO.0000000000000236
Dong L, Kang YK, Li Y, Wei WB, Jonas JB, PREVALENCE AND TIME TRENDS OF, MYOPIA IN CHILDREN AND ADOLESCENTS IN CHINA. A systemic review and meta-analysis. Retina. 2020;40(3):399–411. https://doi.org/10.1097/IAE.0000000000002590
Németh J, Tapasztó B, Aclimandos WA, Kestelyn P, Jonas JB, De Faber JHN, et al. Update and guidance on management of myopia. European Society of Ophthalmology in cooperation with International Myopia Institute. Eur J Ophthalmol. 2021;31(3):853–83. https://doi.org/10.1177/1120672121998960
He M, Xiang F, Zeng Y, Mai J, Chen Q, Zhang J, et al. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA. 2015;314(11):1142–8. https://doi.org/10.1001/jama.2015.10803
Wu PC, Tsai CL, Wu HL, Yang YH, Kuo HK. Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology. 2013;120(5):1080–5. https://doi.org/10.1016/j.ophtha.2012.11.009
Wu PC, Chen CT, Lin KK, Sun CC, Kuo CN, Huang HM, et al. Myopia prevention and outdoor light intensity in a school-based cluster randomized trial. Ophthalmology. 2018;125(8):1239–50. https://doi.org/10.1016/j.ophtha.2017.12.011
He X, Sankaridurg P, Wang J, Chen J, Naduvilath T, He M, et al. Time outdoors in reducing myopia: a school-based cluster randomized trial with objective monitoring of outdoor time and light intensity. Ophthalmology. 2022;129(11):1245–54. https://doi.org/10.1016/j.ophtha.2022.06.024
French AN, Morgan IG, Mitchell P, Rose KA. Patterns of myopigenic activities with age, gender and ethnicity in Sydney schoolchildren. Ophthalmic Physiol Opt. 2013;33(3):318–28. https://doi.org/10.1111/opo.12045
Jones LA, Sinnott LT, Mutti DO, Mitchell GL, Moeschberger ML, Zadnik K, et al. Parental history of myopia, sports and outdoor activities, and future myopia. Invest Ophthalmol Vis Sci. 2007;48(8):3524–32. https://doi.org/10.1167/iovs.06-1118
French AN, Morgan IG, Mitchell P, Rose KA. Risk factors for incident myopia in Australian schoolchildren: the Sydney adolescent vascular and eye study. Ophthalmology. 2013;120(10):2100–8. https://doi.org/10.1016/j.ophtha.2013.02.035
Kang MT, Li SM, Peng X, Li L, Ran A, Meng B, et al. Chinese eye exercises and myopia development in school age children: a nested case-control study. Sci Rep. 2016;6:28531. https://doi.org/10.1038/srep28531. Published 2016 Jun 22.
Lin Z, Vasudevan B, Fang SJ, Jhanji V, Mao GY, Han W et al. Eye exercises of acupoints: their impact on myopia and visual symptoms in Chinese rural children. BMC Complement Altern Med. 2016;16(1):349. Published 2016 Sep 6. https://doi.org/10.1186/s12906-016-1289-4
Jethani J. Efficacy of low-concentration atropine (0.01%) eye drops for prevention of axial myopic progression in premyopes. Indian J Ophthalmol. 2022;70(1):238–40. https://doi.org/10.4103/ijo.IJO_1462_21
Fang PC, Chung MY, Yu HJ, Wu PC. Prevention of myopia onset with 0.025% atropine in premyopic children. J Ocul Pharmacol Ther. 2010;26(4):341–5. https://doi.org/10.1089/jop.2009.0135
He X, Wang J, Zhu Z, Xiang K, Zhang X, Zhang B, et al. Effect of repeated low-level red light on myopia prevention among children in China with premyopia: a randomized clinical trial. JAMA Netw Open. 2023;6(4):e239612. https://doi.org/10.1001/jamanetworkopen.2023.9612. Published 2023 Apr 3.
Jan C, Li L, Keay L, Stafford RS, Congdon N, Morgan I. Prevention of myopia, China. Bull World Health Organ. 2020;98(6):435–7. https://doi.org/10.2471/BLT.19.240903
Morgan IG, Jan CL. China turns to school reform to control the myopia epidemic: a narrative review. Asia Pac J Ophthalmol (Phila). 2022;11(1):27–35. https://doi.org/10.1097/APO.0000000000000489. Published 2022 Jan 18.
He X, Zhao R, Sankaridurg P, Zhu J, Naduvilath T, Ma Y, et al. Design and methodology of the Shanghai child and adolescent large-scale eye study (SCALE). Clin Exp Ophthalmol. 2018;46(4):329–38. https://doi.org/10.1111/ceo.13065
Chen C, Anderson CM, Babb SD, Frank R, Wong S, Kuiper NM, et al. Evaluation of the Asian smokers’ quitline: a centralized service for a dispersed population. Am J Prev Med. 2021;60(3 Suppl 2):S154–62. https://doi.org/10.1016/j.amepre.2020.01.033
Fouladi N, Pourfarzi F, Daneshian A, Alimohammadi S. Mediating factors in early diagnosis of breast cancer: from initial changes in health to breast cancer detection. Asian Pac J Cancer Prev. 2018;19(10):2751–5. https://doi.org/10.22034/APJCP.2018.19.10.2751. Published 2018 Oct 26.
Hu H, Jian W, Fu H, Zhang H, Pan J, Yip W. Health service underutilization and its associated factors for chronic diseases patients in poverty-stricken areas in China: a multilevel analysis. BMC Health Serv Res. 2021;21(1):707. Published 2021 Jul 18. https://doi.org/10.1186/s12913-021-06725-5
Poonam, Manjusha R, Vaghela DB, Shukla VJ. A clinical study on the role of Akshi Tarpana with Jeevantyadi Ghrita in Timira (myopia). Ayu. 2011;32(4):540–5. https://doi.org/10.4103/0974-8520.96130
Goss DA. Variables related to the rate of childhood myopia progression. Optom Vis Sci. 1990;67(8):631–6. https://doi.org/10.1097/00006324-199008000-00014
Lin LL, Shih YF, Hsiao CK, Chen CJ. Prevalence of myopia in Taiwanese schoolchildren: 1983 to 2000. Ann Acad Med Singap. 2004;33(1):27–33.
Zadnik K, Sinnott LT, Cotter SA, Jones-Jordan LA, Kleinstein RN, Manny RE, et al. Prediction of juvenile-onset myopia. JAMA Ophthalmol. 2015;133(6):683–9. https://doi.org/10.1001/jamaophthalmol.2015.0471
Ravindra K, Rattan P, Mor S, Aggarwal AN. Generalized additive models: building evidence of air pollution, climate change and human health. Environ Int. 2019;132:104987. https://doi.org/10.1016/j.envint.2019.104987
Lyu P, Shi J, Hu J, et al. Barriers and facilitators to using ophthalmic clinical health services following school vision screening: a mixed-methods study. BMJ Paediatrics Open. 2024;8:e002459. https://doi.org/10.1136/bmjpo-2023-002459
Liu L, Li R, Huang D, Lin X, Zhu H, Wang Y, et al. Prediction of premyopia and myopia in Chinese preschool children: a longitudinal cohort. BMC Ophthalmol. 2021;21(1):283. https://doi.org/10.1186/s12886-021-02045-8. Published 2021 Jul 21.
Ying GS, Maguire MG, Cyert LA, Ciner E, Quinn GE, Kulp MT, et al. Prevalence of vision disorders by racial and ethnic group among children participating in head start. Ophthalmology. 2014;121(3):630–6. https://doi.org/10.1016/j.ophtha.2013.09.036
Fan DS, Lai C, Lau HH, Cheung EY, Lam DS. Change in vision disorders among Hong Kong preschoolers in 10 years. Clin Exp Ophthalmol. 2011;39(5):398–403. https://doi.org/10.1111/j.1442-9071.2010.02470.x
Schuster AK, Krause L, Kuchenbäcker C, Prütz F, Elflein HM, Pfeiffer N, et al. Prevalence and time trends in myopia among children and adolescents. Dtsch Arztebl Int. 2020;117(50):855–60. https://doi.org/10.3238/arztebl.2020.0855
French AN, Morgan IG, Burlutsky G, Mitchell P, Rose KA. Prevalence and 5- to 6-year incidence and progression of myopia and hyperopia in Australian schoolchildren. Ophthalmology. 2013;120(7):1482–91. https://doi.org/10.1016/j.ophtha.2012.12.018
Tang Y, Chen A, Zou M, Liu Z, Young CA, Zheng D, et al. Prevalence and time trends of refractive error in Chinese children: a systematic review and meta-analysis. J Glob Health. 2021;11:08006. https://doi.org/10.7189/jogh.11.08006. Published 2021 Jul 17.
Morgan IG, Rose KA, Ellwein LB, Refractive Error Study in Children Survey Group. Is emmetropia the natural endpoint for human refractive development? An analysis of population-based data from the refractive error study in children (RESC). Acta Ophthalmol. 2010;88(8):877–84. https://doi.org/10.1111/j.1755-3768.2009.01800.x
Li SM, Wei S, Atchison DA, Kang MT, Liu L, Li H, et al. Annual incidences and progressions of myopia and high myopia in Chinese schoolchildren based on a 5-year cohort study. Invest Ophthalmol Vis Sci. 2022;63(1):8. https://doi.org/10.1167/iovs.63.1.8
McCullough SJ, O’Donoghue L, Saunders KJ. Six year refractive change among white children and young adults: evidence for significant increase in myopia among white UK children. PLoS ONE. 2016;11(1):e0146332. https://doi.org/10.1371/journal.pone.0146332. Published 2016 Jan 19.
Hu Y, Ding X, Long W, He M, Yang X. Longitudinal changes in spherical equivalent refractive error among children with preschool myopia. Invest Ophthalmol Vis Sci. 2019;60(1):154–60. https://doi.org/10.1167/iovs.18-24862
Saw SM, Tong L, Chua WH, Chia KS, Koh D, Tan DT, et al. Incidence and progression of myopia in Singaporean school children. Invest Ophthalmol Vis Sci. 2005;46(1):51–7. https://doi.org/10.1167/iovs.04-0565
Wong K, Dahlmann-Noor A. Myopia and its progression in children in London, UK: a retrospective evaluation. J Optom. 2020;13(3):146–54. https://doi.org/10.1016/j.optom.2019.06.002
McCullough S, Adamson G, Breslin KMM, McClelland JF, Doyle L, Saunders KJ. Axial growth and refractive change in white European children and young adults: predictive factors for myopia. Sci Rep. 2020;10(1):15189. https://doi.org/10.1038/s41598-020-72240-y. Published 2020 Sep 16.
Verkicharla PK, Kammari P, Das AV. Myopia progression varies with age and severity of myopia. PLoS ONE. 2020;15(11):e0241759. https://doi.org/10.1371/journal.pone.0241759. Published 2020 Nov 20.
Saw SM, Nieto FJ, Katz J, Schein OD, Levy B, Chew SJ. Factors related to the progression of myopia in Singaporean children. Optom Vis Sci. 2000;77(10):549–54. https://doi.org/10.1097/00006324-200010000-00009
Shih YF, Ho TC, Hsiao CK, Lin LL. Long-term visual prognosis of infantile-onset high myopia. Eye (Lond). 2006;20(8):888–92. https://doi.org/10.1038/sj.eye.6702035
Brown NP, Koretz JF, Bron AJ. The development and maintenance of emmetropia. Eye (Lond). 1999;13(Pt 1):83–92. https://doi.org/10.1038/eye.1999.16
Blows SJ, Murphy EP, Martin FJ, Davies RM. Vision screening in preschoolers: the New South Wales statewide eyesight preschooler screening program. Med J Aust. 2014;200(4):222–5. https://doi.org/10.5694/mja13.10594
Hemptinne C, La Grange N, Yüksel D. Vision screening in Belgian children: too much or not enough? Ophthalmic Epidemiol. 2020;27(5):364–75. https://doi.org/10.1080/09286586.2020.1767151
Hered RW, Wood DL. Preschool vision screening in primary care pediatric practice. Public Health Rep Wash DC 1974. 2013;128(3):189–97. https://doi.org/10.1177/003335491312800309
He X, Sankaridurg P, Xiong S, Li W, Naduvilath T, Lin S, et al. Prevalence of myopia and high myopia, and the association with education: Shanghai child and adolescent large-scale eye study (SCALE): a cross-sectional study. BMJ Open. 2021;11(12):e048450. https://doi.org/10.1136/bmjopen-2020-048450. Published 2021 Dec 23.
Matsumura S, Dannoue K, Kawakami M, Uemura K, Kameyama A, Takei A, et al. Prevalence of myopia and its associated factors among Japanese preschool children. Front Public Health. 2022;10:901480. https://doi.org/10.3389/fpubh.2022.901480. Published 2022 Jun 22.
Li M, Tan CS, Xu L, Foo LL, Yap F, Sun CH, et al. Sleep patterns and myopia among school-aged children in Singapore. Front Public Health. 2022;10:828298. https://doi.org/10.3389/fpubh.2022.828298. Published 2022 Mar 25.
Jing S, Yi X, Lei Y, Hu L, Cheng W, Wen T, et al. Prevalence and risk factors for myopia and high myopia: a cross-sectional study among Han and Uyghur students in Xinjiang, China. Ophthalmic Physiol Opt. 2022;42(1):28–35. https://doi.org/10.1111/opo.12907
Mukazhanova A, Aldasheva N, Iskakbayeva J, Bakhytbek R, Ualiyeva A, Baigonova K, et al. Prevalence of refractive errors and risk factors for myopia among schoolchildren of Almaty, Kazakhstan: a cross-sectional study. PLoS ONE. 2022;17(6):e0269474. https://doi.org/10.1371/journal.pone.0269474. Published 2022 Jun 3.
Funding
This study was funded by the Key Discipline Program of Sixth Round of the Three-Year Public Health Action Plan (Year 2023–2025) of Shanghai, China (GWVI-11.1-32), and the Shanghai three-year action plan to strengthen public health project(NO: GWV−9.1).
Author information
Authors and Affiliations
Contributions
Pingping Lyu had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: Huijing Shi, Pingping Lyu, Jingwen Hu, Yujie WangAcquisition, analysis, or interpretation of data: Pingping Lyu, Huijing Shi, Jingjing Wang2, Xiangui He2Drafting of the manuscript: Pingping Lyu. Critical revision of the manuscript for important intellectual content: Huijing Shi, Pingping Lyu, Jingwen Hu, Yujie WangStatistical analysis: Pingping LyuObtained funding: Huijing Shi, Xiangui HeAdministrative, technical, or material support: Xiangui He, Jingjing WangSupervision: Huijing Shi.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study conformed to the principles of the Declaration of Helsinki, and informed consent was signed by the participants’ parents. The Ethics Committee of the School of Public Health, Fudan University, approved this study (approval number IRB#2020-07-0836).
Furthermore, this study does not involve any human or animal experiments and does not include any information or images that may lead to the identification of research participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lyu, P., Hu, J., Wang, Y. et al. Impact of ophthalmic clinical service use in mitigating myopia onset and progression in preschool children: a retrospective cohort study. BMC Ophthalmol 24, 221 (2024). https://doi.org/10.1186/s12886-024-03488-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-024-03488-5