Abstract
Background
Retinopathy of prematurity (ROP) is a disease that affects preterm infants born younger than 30 weeks of gestation. The pathophysiology of ROP involves an initial vaso-obliterative phase followed by vaso-proliferative phase that leads to disease progression. The use of supplemental oxygen during the vaso-proliferative phase of ROP has been associated with reduced disease progression, but how this impacts the need for ROP treatment is unclear. The goal of this study was to compare the rate of laser or intravitreal bevacizumab after implementation of a new supplemental oxygen therapy protocol in preterm infants with stage 2 ROP.
Methods
This is a retrospective chart review of preterm infants diagnosed with stage 2 ROP at Riley Hospital for Children between 1/2017 and 12/2022. Patients diagnosed between 1/2017 and 6/2020 were classified as Cohort A, preprotocol implementation. Patients diagnosed from 8/2020 to 12/2022 were classified as Cohort B, postprotocol implementation. In Cohort A, oxygen saturation was kept at 91-95% through the entire hospitalization. In Cohort B, oxygen saturation was increased to 97–99% as soon as Stage 2 ROP was diagnosed. Statistical analyses were performed using chi-square and Student’s T test, followed by multivariate analyses to determine the impact of the oxygen protocol on the need for ROP treatment.
Results
A total of 211 patients were diagnosed with stage 2 ROP between 1/2017 and 12/2022. Of those patients, 122 were before protocol implementation therapy (Cohort A), and 89 were after implementation of supplemental oxygen protocol (Cohort B). Gestational age was slightly higher in Cohort B (Cohort A 25.3 ± 1.9, Cohort B 25.8 ± 1.84, p = 0.04). There was no difference in birth weight, NEC, BPD, or survival. Cohort B had lesser need for invasive mechanical ventilation and higher days on CPAP during hospitalization. Notably, Cohort A had 67 (55%) patients treated with laser photocoagulation or intravitreal bevacizumab versus 20 (22%) patients in Cohort B (OR 0.19, 0.08–0.40).
Conclusion
The need for laser photocoagulation or intravitreal bevacizumab was significantly decreased in high-risk patients treated with the supplemental oxygen protocol. This result supports the idea that targeted supplemental oxygen therapy to keep saturations between 97 and 99% can reduce disease progression in infants with stage 2 ROP and potentially decrease the burden of additional procedures.
Similar content being viewed by others
Introduction
Retinopathy of prematurity (ROP) is a disease that primarily affects premature infants born before 30 weeks of gestation and is currently the leading cause of childhood blindness in the United States [1]. The pathophysiology of ROP consists of two phases: an initial vaso-obliterative phase followed by a vaso-proliferative phase. The initial vaso-obliterative phase is due to the transition from a hypoxic in-utero environment to a relatively hyperoxic ex-utero environment at birth. This phase usually occurs before the corrected gestation age (CGA) of 30 weeks, when the use of oxygen (O2) and higher target O2 saturations result in increased ROP severity [2]. The vaso-proliferative phase occurs after 30–32 weeks of CGA, and the pathophysiology is complex, involving a combination of factors including retinal hypoxia leading to increased angiogenic factors such as vascular endothelial growth factor (VEGF), as well as other nutrient regulated factors such as insulin-like growth factor 1 (IGF-1) [3, 4].
Current management of ROP involves limiting O2 during the first few weeks of life and serial ophthalmology retinal examinations beginning at 30 weeks CGA or later. ROP is classified based on zone, stage, and type as defined by ICROP criteria [5]. ROP deemed high risk for disease progression that could result in a poor visual or anatomic outcome (Type 1 ROP) is treated with laser photocoagulation and/or intravitreal anti-VEGF antibody (bevacizumab) [6]. Several studies have reported an association between laser photocoagulation and decreased visual acuity and a higher rate of myopia and astigmatism during childhood [7, 8]. Infants received intravitreal bevacizumab treatment may experience reactivation of ROP [9]. Intravitreal bevacizumab has also been reported to be associated with a higher risk of severe neurodevelopmental impairment and cerebral palsy [10, 11]. It is essential to note that these findings may be influenced by biases, as the associated morbidities may be partly attributed to the illness severity of the premature infants [7]. Therefore, there is a pressing need to explore alternative, less invasive approaches that can impede ROP progression and potentially avoid the need for laser or intravitreal bevacizumab.
Most of the efforts to prevent ROP are focused on limiting O2 delivery during the vaso-obliterative phase [12, 13]. Large, randomized control trials in the US, Australia, New Zealand, and United Kingdom found that lower oxygen saturations (85–89%) were associated with decreased rates of ROP in preterm infants compared to 91–95% target saturations [2, 14]. These studies randomized premature infants shortly after birth up until 36 CGA and therefore likely assessed the benefits of lower oxygen exposure during the vaso-obliterative phase, but unfortunately found a higher rate of mortality and necrotizing enterocolitis (NEC). Additional retrospective cohort studies also observed that infants managed with biphasic oxygen saturation targets (85–92% before, 92–97% after 34 weeks corrected gestational age), as opposed to static (91–95% throughout hospital stay) had lower ROP severity [12, 13]. To date, only one randomized control trial assessed oxygen supplementation in preventing ROP progression (STOP-ROP) after established ROP [15]. This study did not identify statistically significant benefits or harm of O2 supplementation on ROP. However, post hoc analysis suggested the benefits of O2 supplementation in prethreshold ROP without plus disease. To the best of our knowledge, small retrospective studies have also suggested potential benefits of supplemental O2 in preventing ROP progression [16, 17], but none have shown the direct impact of O2 supplementation after 32 weeks of CGA (during the vaso-proliferative phase) on the need for laser or intravitreal bevacizumab.
Taking these background studies into consideration, we implemented a protocol using supplemental O2 to prevent ROP progression in preterm infants with stage 2 ROP. We hypothesize that optimizing supplemental oxygen therapy in patients with stage 2 ROP can decrease the risk of progression to type I ROP and therefore reduce the need for treatment with either laser photocoagulation or intravitreal bevacizumab.
Methods
Study design
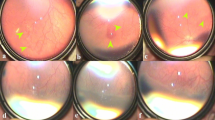
This is a retrospective chart review of neonates discharged from the neonatal ICU (NICU) at the Riley Hospital for Children between 1/1/2017 and 12/31/2022. Exemptions were obtained from the Indiana University School of Medicine (IUSM) Institutional Review Board (IRB), and the need for informed consent was waived because only deidentified clinical data was analyzed for this study. All data were deidentified and in compliance with the Healthcare Insurance Portability and Accountability Act (HIPAA). The new supplemental oxygen protocol was implemented in July 2019. We defined our cohorts as preprotocol implementation (Cohort A), which spanned from 1/2017 to 6/2020, and postprotocol implementation (Cohort B), which spanned 8/2019-12/2022 (Fig. 1). Preterm infants diagnosed in July 2020 were excluded to provide a washout period, thereby decreasing any confounding factors during the implementation of the new protocol. All neonates’ data were gathered from the duration of their inpatient stay. Neonates were screened and graded by the same two pediatric ophthalmologists (K. H and C. B) throughout the study.
Eligibility
Eligibility for inclusion in these data was classified as neonates discharged from the Riley Hospital for Children NICU between January 2017 and December 2022 who had a birthweight < = 1500 g, were < = 30 weeks gestation at birth, had no congenital abnormalities, and had Zone 1 Stage 2 w/o plus or Zone 2 Stage 2 w/o plus ROP. Preterm infants with type 1 ROP were immediately treated with laser photocoagulation or intravitreal bevacizumab [18].
Clinical data
All data were collected by the authors in compliance with the Indiana University School of Medicine IRB and HIPAA. Demographic data and clinical variables known to affect ROP (sex, race, birthweight, gestational age, diagnosis of necrotizing enterocolitis (NEC), interventricular hemorrhage (IVH), sepsis, bronchopulmonary dysplasia (BPD), and admission respiratory support) were retrieved from electronic records. The primary endpoint of this study was the need for invasive intervention via laser photocoagulation or intravitreal bevacizumab. Secondary endpoints were the duration of hospital stay and time on respiratory support.
Oxygen supplementation protocol
The Riley Hospital oxygen protocol was originally conceived based on the research of the STOP-ROP trial. Prior to protocol implementation, all preterm infants were treated with an oxygen saturation target of 91–95% during the duration of their hospitalization. After implementation, all neonates diagnosed with stage 2 ROP had a new target oxygen saturation of 97–99% (Fig. 1). Any adjustments in oxygen support modality or changes in FiO2 were managed by the bedside nurse. Given the potential risks of hyperoxia in neonates with chronic lung disease, neonates’ FiO2 was titrated based on their level of respiratory support. For infants requiring invasive mechanical ventilation (high-frequency ventilators (HFV), conventional mechanical ventilators (CMV) or any noninvasive mechanical ventilation providing continuous positive airway pressure (CPAP), a limit of 50% maximum FiO2 was allowed to avoid oxygen toxicity. Infants on ≤ 1 L per minute nasal cannula (NC) were placed on 100% FiO2. The decision to continue supplemental oxygen therapy was reassessed following weekly ophthalmology exams after initiation of oxygen treatment.
Statistical analysis
Descriptive statistics were obtained for demographic values at baseline for each cohort. To explore the differences between the two cohorts, chi-square tests were performed for categorical variables, and t tests were performed for continuous variables, which were first explored for normality. The main outcome of patients needing laser or bevacizumab was first explored unadjusted with chi-squared tests and later analyzed using a logistic regression adjusting for clinically or statistically significant covariates (sex, race, birthweight, gestational age, NEC status, IVH grade, history of sepsis, BPD, admission respiratory support need, and days on each respiratory modality). The outcomes, length of stay, time on CPAP, time on NC and time on any respiratory support, were analyzed with a linear regression adjusting for the same variables as the main outcomes. Assumptions for normality were checked and met. All data were analyzed using R v4.3.1 and RStudio v2023.09.1 + 494 software [19].
Results
Baseline demographics
A total of 212 patients met the criteria for inclusion, with 122 patients in Cohort A, preprotocol implementation, and 89 patients in Cohort B, postprotocol implementation. All demographic data are summarized in Table 1. Overall, there was no difference in the distribution of sex, Caucasian vs. non-Caucasian status, birthweight, diagnosis of NEC, BPD, or IVH, or sepsis. Patients from Cohort B had marginally higher gestational age at birth (Cohort A 25.3 ± 1.90, Cohort B 25.8 ± 1.84, p = 0.04), and a lower CMV use with higher CPAP use for respiratory support during admission (Table 1). We next assessed the days of respiratory support as a proxy for pulmonary health for both cohorts and compared the days on each respiratory support modality (Table 2). We found that Cohort A had a longer duration on HFV and CMV, and Cohort B had a longer duration on CPAP. Overall, Cohort B had lower days on any respiratory support. Given the statistical significance, we included days of ventilation as a covariate in subsequent logistic regression.
Implementation of the oxygen supplemental protocol is associated with a decreased need for laser photocoagulation or intravitreal bevacizumab
Overall, we found a significant reduction in the need for subsequent laser and/or intravitreal bevacizumab treatment in infants who developed stage 2 ROP after the implementation of supplemental O2 therapy (Table 3). In Cohort A, 55% (67/122) of infants with stage 2 ROP needed treatment, versus only 22% (20/89) of infants in Cohort B who needed further laser or intravitreal bevacizumab treatment (P < 0.001, univariate Pearson’s Chi-squared test). We next performed a logistic regression model adjusting for clinically important and significantly different covariates (sex, race, birthweight, gestational age, NEC status, IVH grade, sepsis, BPD, admission respiratory support need, and days on each respiratory modality). Compared to Cohort A, patients in Cohort B had a significantly decreased risk of needing laser and/or intravitreal bevacizumab treatment. (Table 4, OR = 0.19; 95% CI 0.09–0.41; P = 0.000). We also found that female sex, higher birthweight, sepsis, and longer time on conventional ventilation were factors associated with decreased need for laser or intravitreal bevacizumab. NEC was associated with higher odds of needing laser and/or intravitreal bevacizumab.
O2 protocol is associated with longer NC/O2 use but does not increase LOS
Finally, we assessed whether implementation of the supplemental O2 protocol in our population impacted the time on oxygen and length of stay in the hospital. After correcting for the same variables as the main treatment outcome, time on CPAP was increased (Beta = 18 [8.7,27], P = 0.000). However, the length of stay did not differ between the two cohorts (Beta = 12 [-0.58,24], P = 0.062)
Discussion
The survival of premature infants has steadily increased over the past few decades [20]. However, ROP remains a significant disease affecting surviving preterm infants born ≤ 30 weeks GA. Specifically, over 50% of these infants had a diagnosis of ROP, with 1 in 10 preterm infants developing severe (Stage 3) ROP [20]. Currently, the prevention of severe ROP development remains limited. Limiting oxygen exposure by targeting lower oxygen saturations (85–89%) during the vaso-obliterative phase is the only management shown to decrease the rate of severe ROP but is associated with a higher mortality rate in preterm infants [2, 12, 13, 15]. Other therapies during the early postnatal NICU course, such as aggressive parenteral nutrition, use of human milk, and several vitamin supplements, have been shown to decrease the risks of ROP of all stages, but the results on severe ROP needing intervention were mixed [21]. The aim of this study was to assess whether the use of supplemental oxygen to achieve a higher oxygen saturation target after the onset of the vaso-proliferative phase in preterm infants with ROP will dampen the conversion to Type 1 ROP and result in a lower rate of laser photocoagulation or intravitreal bevacizumab. Indeed, we found that after implementing the supplemental oxygen protocol, infants with Zone 1 or Zone 2 Stage 2 ROP without plus disease in Cohort B had lower rates of disease progression needing laser photocoagulation or intravitreal bevacizumab. This finding is consistent with benefits reported in a meta-analysis (2 RCTs, 1 prospective observation, and 2 retrospective cohorts with over 1600 patients) [22] as well as a retrospective cohort study by Colaizy et al. [16] Collectively, these studies found that higher oxygen saturation targets after 32 weeks of CGA are associated with decreased ROP disease progression.
We also assessed the duration of respiratory support and length of stay (LOS) in our patients to assess whether implementation of the supplemental oxygen protocol resulted in a longer duration of hospital stay or a longer duration of need for respiratory support. We found that Cohort B had lower number of days on HFV and CMV, higher number of days on CPAP, and lower number of days on any respiratory support with no increase in LOS. The difference in days on invasive mechanical ventilation and higher days on CPAP likely reflected changes in respiratory management (more proactive use of CPAP and extubation attempts), and the implementation of the protocol did not result in prolonged use of oxygen or LOS. Survival to discharge was not different in infants who were placed on supplemental oxygen protocol. These data also suggest that limiting FiO2 in high-risk infants to 50%, as we did in our protocol, does not increase adverse pulmonary events, as reported in the STOP-ROP trial. Nevertheless, our study is limited by the nature of its retrospective cohort design and therefore unable to control for nonsystematic changes in clinical practice. However, major clinical management (e.g., surfactant delivery, nutritional management) remained consistent. Furthermore, we had two pediatric ophthalmologists who had consistent ROP grading and management.
Conclusions
In conclusion, our results showed that the use of supplemental oxygen to target higher oxygen saturations in infants with Zone 1 and Zone 2 Stage 2 ROP without plus disease is safe and potentially decreases disease progression and the need for treatment with laser photocoagulation or intravitreal bevacizumab.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ROP:
-
Retinopathy of Prematurity
- NEC:
-
necrotizing enterocolitis
- IV:
-
intravitreal
- CGA:
-
corrected gestational age
- IVH:
-
intraventricular hemorrhage
- RA:
-
room air
- NC:
-
nasal cannula
- CPAP:
-
continuous positive airway pressure
- CMV:
-
conventional mechanical ventilation
- HFV:
-
high–frequency ventilation
References
Lim HW, Pershing S, Moshfeghi DM, Heo H, Haque ME, Lambert SR, Consortium IRAC. Causes of Childhood blindness in the United States using the IRIS(R) Registry (Intelligent Research in Sight). Ophthalmology. 2023;130:907–13. https://doi.org/10.1016/j.ophtha.2023.04.004
Network SS, Finer NN, Walsh MC, Rich W, Gantz MG, Laptook AR, Yoder BA, Faix RG, Das A, et al. Target ranges of oxygen saturation in extremely preterm infants. N Engl J Med. 2010;362:1959–69. https://doi.org/10.1056/NEJMoa0911781
Strube YNJ, Wright KW. Pathophysiology of retinopathy of prematurity. Saudi J Ophthalmol. 2022;36:239–42. https://doi.org/10.4103/sjopt.sjopt_18_22
Sapieha P, Joyal JS, Rivera JC, Kermorvant-Duchemin E, Sennlaub F, Hardy P, Lachapelle P, Chemtob S. Retinopathy of prematurity: understanding ischemic retinal vasculopathies at an extreme of life. J Clin Invest. 2010;120:3022–32. https://doi.org/10.1172/JCI42142
Molinari A, Weaver D, Jalali S. Classifying retinopathy of prematurity. Community Eye Health. 2017;30:55–6.
Good WV, Hardy RJ. The multicenter study of early treatment for retinopathy of Prematurity (ETROP). Ophthalmology. 2001;108:1013–4. https://doi.org/10.1016/s0161-6420(01)00540-1
Diggikar S, Gurumoorthy P, Trif P, Mudura D, Nagesh NK, Galis R, Vinekar A, Kramer BW. Retinopathy of prematurity and neurodevelopmental outcomes in preterm infants: a systematic review and meta-analysis. Front Pediatr. 2023;11:1055813. https://doi.org/10.3389/fped.2023.1055813
Yang CS, Wang AG, Shih YF, Hsu WM. Long-term biometric optic components of diode laser-treated threshold retinopathy of prematurity at 9 years of age. Acta Ophthalmol. 2013;91:e276–282. https://doi.org/10.1111/aos.12053
Lee CC, Chiang MC, Chu SM, Wu WC, Ho MM, Lien R. Clinical risk factors for retinopathy of Prematurity Reactivation after Intravitreal Anti-vascular endothelial growth factor injection. J Pediatr. 2024;113913. https://doi.org/10.1016/j.jpeds.2024.113913
Chou YB, Wang AG, Yang HY, Chen KJ, Yang CS. Refractive status, biometric components, and functional outcomes of patients with threshold retinopathy of prematurity: systemic review and a 17-year longitudinal study. Graefes Arch Clin Exp Ophthalmol. 2022;260:3809–16. https://doi.org/10.1007/s00417-022-05730-6
Baiad AA, Kherani IZ, Popovic MM, Katsnelson G, Muni RH, Mireskandari K, Tehrani NN, Zhou TE, Kertes PJ. A Meta-analysis of neurodevelopmental outcomes following Intravitreal Bevacizumab for the treatment of retinopathy of Prematurity. Neonatology. 2023;120:577–88. https://doi.org/10.1159/000531541
Shukla A, Sonnie C, Worley S, Sharma A, Howard D, Moore J, Rodriguez RJ, Hoppe G, Sears JE. Comparison of biphasic vs static oxygen saturation targets among infants with retinopathy of Prematurity. JAMA Ophthalmol. 2019;137:417–23. https://doi.org/10.1001/jamaophthalmol.2018.7021
Sears JE, Pietz J, Sonnie C, Dolcini D, Hoppe G. A change in oxygen supplementation can decrease the incidence of retinopathy of prematurity. Ophthalmology. 2009;116:513–8. https://doi.org/10.1016/j.ophtha.2008.09.051
Group BIUKC, Group BIAC, Group BINZC, Stenson BJ, Tarnow-Mordi WO, Darlow BA, Simes J, Juszczak E, Askie L, Battin M, et al. Oxygen saturation and outcomes in preterm infants. N Engl J Med. 2013;368:2094–104. https://doi.org/10.1056/NEJMoa1302298
Supplemental Therapeutic Oxygen for Prethreshold Retinopathy Of. Prematurity (STOP-ROP), a randomized, controlled trial. I: primary outcomes. Pediatrics. 2000;105:295–310. https://doi.org/10.1542/peds.105.2.295
Colaizy TT, Longmuir S, Gertsch K, Abramoff MD, Klein JM. Use of a Supplemental Oxygen Protocol to suppress progression of retinopathy of Prematurity. Invest Ophthalmol Vis Sci. 2017;58:887–91. https://doi.org/10.1167/iovs.16-20822
Cayabyab R, Arora V, Wertheimer F, Durand M, Ramanathan R. Graded oxygen saturation targets and retinopathy of prematurity in extremely preterm infants. Pediatr Res. 2016;80:401–6. https://doi.org/10.1038/pr.2016.98
Good WV. and Early Treatment for Retinopathy of Prematurity Cooperative, G. (2006). The Early Treatment for Retinopathy Of Prematurity Study: structural findings at age 2 years. Br J Ophthalmol 90, 1378–1382. https://doi.org/10.1136/bjo.2006.098582
Team RC. R: a Language and Environment for Statistical Computing. R Foundation for Statistical Computing; 2023.
Bell EF, Hintz SR, Hansen NI, Bann CM, Wyckoff MH, DeMauro SB, Walsh MC, Vohr BR, Stoll BJ, Carlo WA, et al. Mortality, In-Hospital morbidity, Care practices, and 2-Year outcomes for extremely Preterm infants in the US, 2013–2018. JAMA. 2022;327:248–63. https://doi.org/10.1001/jama.2021.23580
Fang JL, Sorita A, Carey WA, Colby CE, Murad MH, Alahdab F. Interventions to prevent retinopathy of Prematurity: a Meta-analysis. Pediatrics. 2016;137. https://doi.org/10.1542/peds.2015-3387
Chen ML, Guo L, Smith LE, Dammann CE, Dammann O. High or low oxygen saturation and severe retinopathy of prematurity: a meta-analysis. Pediatrics. 2010;125:e1483–1492. https://doi.org/10.1542/peds.2009-2218
Acknowledgements
This research was funded in part by an unrestricted grant from Research to Prevent Blindness Grant, Indiana Medical Student Program for Research, March of Dimes Basil O’Connor Award (K.L.K) and K08HD109636 (K.L.K).
Funding
This research was funded in part by an unrestricted grant from Research to Prevent Blindness Grant, Indiana Medical Student Program for Research, March of Dimes Basil O’Connor Award (K.L.K) and K08HD109636 (K.L.K).
Author information
Authors and Affiliations
Contributions
R.M. and K.H. performed chart review, data analysis, interpreted result, wrote the first draft and revised the manuscript. S.V. and C.B. interpreted the results if study and revised manuscript. L.G. performed statistical analysis and result interpretation. E.H. and E.L. performed chart review and revised manuscript. K.H. and K.L.K. designed the study, analyzed and interpreted the result, and revised manuscript. All authors approved the final version of manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This retrospective review was reviewed and considered as an exempt study by the Institutional Review Board (IRB) of Indiana University School of Medicine. Given that this is an exempted study that analyzed deidentified clinical data, informed consent to participate was waived. This study adhered to the tenants of the Declaration of Helsinki
Consent for publication
Not applicable.
Competing interests
None.
Commercial disclosures
Robert Minturn: none.Kelly Hartigan: none.Charline Boente: None.Lilian Golzarri-Arroyo: None.Elizabeth Hynes: none.Elleen Laughlin: none.Sravanthi Vegunta: None.Kathryn Haider: None.Kok Lim Kua: none.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Minturn, R., Hartigan, K., Vegunta, S. et al. Efficacy of supplemental oxygen in reducing the need for laser or intravitreal bevacizumab in preterm infants with stage 2 retinopathy of prematurity. BMC Ophthalmol 24, 220 (2024). https://doi.org/10.1186/s12886-024-03483-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-024-03483-w