Abstract
Purpose
We describe the management of a case of severe corneal melting after corneal cross-linking (CXL) treated with a staged approach using a conjunctival flap followed by deep anterior lamellar keratoplasty (DALK).
Methods
A 12-year-old male developed severe corneal melting with pending perforation after an accelerated epithelium-off CXL protocol. We initially treated the patient with a conjunctival flap to prevent perforation. Three months later, we performed DALK to restore vision.
Results
Conjunctival flap surgery allowed us to avoid corneal perforation and penetrating keratoplasty (PK) à chaud. Once the inflammation had resolved, we recessed the conjunctiva and performed DALK for optical purposes. Twelve months later, the graft was clear and the corrected visual acuity was 20/25 (Snellen). No complications occurred after surgery.
Conclusions
Although CXL is considered a safe procedure, in rare cases it can lead to serious complications, such as corneal haze, infectious and non-infectious keratitis, stromal melting and perforation. Corneal melting and perforation are usually managed by emergency PK. Herein we suggest a staged approach involving an emergency conjunctival flap followed by DALK at a later time that allowed us to avoid PK à chaud.
Similar content being viewed by others
Introduction
Keratoconus is a non-inflammatory ectatic disorder characterised by progressive corneal thinning and protrusion [1]; it usually affects both eyes and there is often asymmetrical involvement. The onset of keratoconus occurs at about the age of puberty, with a greater rate of progression in paediatric than adult patients [2].
Corneal cross-linking (CXL) is an effective treatment used to slow down or halt the progression of keratoconus [3]. The procedure combines riboflavin (vitamin B2), as a photosensitiser, and ultraviolet A (UVA) energy to induce reactive oxygen species to promote the formation of covalent bonds between collagen molecules. In this way, CXL increases the biomechanical stability of the cornea and reduces the probability of ectasia progression. Either the conventional technique or an accelerated “epithelium-off” protocol is successful for the management of paediatric keratoconus [4, 5]. The advantage of the latter approach is a shorter procedure that is more easily accepted by a young patient. Although CXL is a safe procedure with a low complication rate, a few side effects—such as corneal haze, infectious and non-infectious keratitis and stromal melting—have been reported. These mainly occur after epithelial debridement and may be related to pre-existing conditions, such as herpetic eye disease, vernal conjunctivitis, atopy, diabetes and other autoimmune conditions [6]. Herein, we report a case of corneal CXL, complicated by corneal melting, in a male paediatric patient, and its surgical management.
Case report
A 12-year-old Caucasian boy with progressive visual loss came to our attention. His best spectacle-corrected visual acuity (BCVA) was 20/25 in the right eye and 20/100 in the left eye. We performed corneal topography (Pentacam, Oculus Optikgeraete GmbH, Wetzlar, Germany), which revealed the presence of bilateral keratoconus, more accentuated in the left eye (Fig. 1A). The patient was negative for history of atopic dermatitis or allergies. Considering the young age of the patient, the referred worsening of visual symptoms and the high risk of progression, we decided to perform CXL in the left eye, using an accelerated epithelium-off protocol [7]. We administered topical pilocarpine 2% 10 min before treatment. After routine preparation with instillation of iodopovidone 5% and lidocaine 4% in the conjunctival sac, we debrided the corneal epithelium in the central 8–9 mm. Then, we applied riboflavin 0.1% (VibeX Rapid Avedro Inc., Waltham, MA, USA) for 10 min. Subsequently, we applied UVA irradiation, using a total energy dose of 7.2 J/cm2 delivered by 30 mW/cm2pulsed light (1 s on/1 second off) for 8 min, in accordance with literature [3, 8]. At the end, we positioned a sterile bandage contact lens (Relieve 7days, Safilens, Vision Innovation, Staranzano, Italy) and added betamethasone 0.2%/chloramphenicol 0.5% eye drops. Postoperatively, we prescribed unpreserved dexamethasone 0.15% and ofloxacin 0.3% eye drops four times a day, and an unpreserved lubricant eye drop eight times a day.
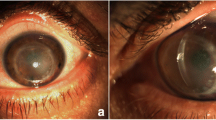
A Right eye preoperative corneal topography showing keratoconus. B Intraoperative photograph showing annular corneal infiltrate and melting with a pending perforation a few days after corneal cross-linking. C Intraoperative photograph showing the conjunctival flap covering the cornea surface at the end of the Gunderson procedure. D Anterior segment optical coherence tomography showing the conjunctival flap and corneal stromal integrity three months after surgery
Two days after treatment, the patient returned to our emergency room complaining of intense ocular pain, photophobia and drastically reduced visual function (20/500 Snellen) in the treated eye. Visual acuity was hand motion and slit-lamp examination showed annular corneal stromal infiltration measuring 8.00 mm in diameter, and a wide epithelial defect. We removed the contact lens and sent it for a microbiological investigation, which was negative for microbial growth. We commenced combined topical therapy with dexamethasone 0.1% to reduce the inflammatory stimulus, which was causing the corneal to melt, and levofloxacin 0.5% every 2 h. Intraocular pressure remained well controlled therefore there was no need to introduce anti-hypertensive therapy. It was recommended that the patient avoid any physical strain. After three days, the patient returned with worsening symptoms. Slit-lamp examination revealed severe central corneal thinning with impending perforation, which prompted surgical intervention (Fig. 1B). To prevent further stromal melting and perforation while avoiding penetrating keratoplasty (PK) à chaud, we decided to perform a conjunctival flap, using the Gundersen technique [9], and a temporary tarsorrhaphy (Fig. 1C). We sent corneal epithelium collected during the surgery for a microbiological investigation, which excluded an infectious aetiology. One month after the surgery, the conjunctival flap was well positioned and vascularised, the inflammation was controlled, the eye was quiet and pain was completely relieved. Meanwhile, the patient underwent dermatological evaluation to investigate the presence of an allergy to any of the compounds used during and after the surgery (contact lens, chloramphenicol/betamethasone drops, dexamethasone drops, monofloxacin and levofloxacin drops and riboflavin). However, no significant results emerged from the tests, so we excluded atopic dermatitis.
Three months later, the conjunctival flap was trophic, vascularised and uninflamed, and visual acuity was hand motion. Anterior segment optical coherence tomography (OCT) showed signs of stromal reconstitution (Fig. 1D) under the flap. At this time, we decided to attempt deep anterior lamellar keratoplasty (DALK) to restore vision. During surgery, we recessed the conjunctival flap by using blunt tip scissors (Fig. 2A). We performed a large 9 mm partial thickness trephination and then, under the guide of intraoperative OCT (Leica Proveo 8, Leica Microsystems, Wetzlar, Germany), we introduced a 27 G cannula into the deep stroma. We injected air to induce separation between the pre-Descemet layer and the posterior stroma. Air injection induced the formation of a type 3 bubble (a mixed type 1 and type 2 bubble) (Fig. 2B) that favoured exposure of the pre-Descemet layer in the central 6 mm, leaving a thin peripheral layer of stroma (Fig. 2C) that corresponded to the area of melting. Finally, we secured a donor stromal lenticule 9.0 mm in diameter and 400 μm in thickness, prepared with a microkeratome (Moria SA, Bourbon-l’Archambault, France) in place with 10 − 0 nylon sutures (Supplemental Digital Content, Video 1). At day 1, the corneal lenticule was clear, and the eye showed no signs of inflammation. Twelve months after surgery, the patient’s BCVA was 20/25 (Snellen), the graft was clear and corneal astigmatism was 2.9 D (Fig. 3).
A Intraoperative photograph showing removal of the conjunctival flap prior to keratoplasty. B Intraoperative optical coherence tomography (OCT) scan showing the formation of a mixed type 1 and type 2 bubble (type 3 bubble) during pneumatic dissection. C Intraoperative OCT scan showing the formation of a regular plane made of the pre-Descemet layer, the Descemet membrane and endothelial cells
Discussion
CXL is a technique employed in managing keratoconus and in association with refractive surgery, thanks to its property of strengthening the covalent bonds of stromal collagen. It is considered mainly a safe procedure [10], even though epithelial debridement is a risk factor for stromal haze, persistent epithelial defects, microbial infection, sterile inflammation, stromal melting and, ultimately, corneal perforation [6, 11].
Up to date, only a few cases of corneal melting and perforation have been reported in the literature after CXL (Table 1).
We conducted literature research in PubMed using the keywords “corneal cross-linking, CXL, corneal melting, corneal infection”. We included all the case reports that described the development of corneal melting with perforation or impending perforation. For each paper, we extracted the sex and age of the patients, the protocol of CXL used, the aetiology of corneal melting, and its management.
Infective keratitis was responsible for disruption of the stroma in some cases, which eventually led to corneal perforation. Both bacterial [15, 20] and fungal [22] keratitis have been described. Rama et al. [12] reported an atypical case of corneal perforation after CXL caused by Acanthamoeba keratitis related to improper use of contact lenses.
Abuse of nonsteroidal anti-inflammatory drug (NSAID) drops has also been identified as a cause of corneal melting in patients who underwent CXL. Gokhale et al. [21] reported a case of corneal melting and perforation that occurred 1 week after CXL in a 19-year-old patient treated with diclofenac sodium and proparacaine eyedrops. Noriega et al. [16] described another case of inappropriate use of NSAID eye drops, resulting in corneal melting, in a 50-year-old diabetic patient. Topical NSAIDs have been reported to cause corneal melting and perforation postoperatively, especially in the presence of epithelial breakdown [23]. Impairment of wound healing, resulting from the analgesic property of these drugs, alongside activation of matrix metalloproteinases (MMPs) are the suggested mechanisms [23, 24]. High levels of MMP-2, MMP-3, MMP-8 and MMP-9 have been found in the epithelium and stroma of melted and perforated corneas after topical NSAID use and in patients with diabetes [25]. Our patient did not use NSAID eye drops after the treatment and did not present any known risk factor related to the occurrence of postoperative corneal melting such as diabetes, Down syndrome, vernal keratoconjunctivitis, lagophthalmos and blepharitis [26, 27]. We performed a microbiological investigation; the results were negative for the corneal scraping and the corneal stroma excised at the time of keratoplasty.
In some cases, it is not possible to identify the causative agent of corneal melting [18]. Labiris et al. [13] described a case of a 23-year-old male who developed corneal melting and descemetocele a few days after CXL. They performed a complete laboratory examination for autoimmune and infectious diseases; the patient was also evaluated for hypersensitivity to riboflavin and other components of the B vitamin complex as well as a series of common allergens. However, all of the investigations were negative. Similarly, Tillmann et al. [20] and Angunawela et al. [14] described cases of corneal melting after CXL without a well-defined aetiology. They proposed atopia and hypersensitivity to Streptococcus pneumoniae antigens as possible triggers for the inflammation. Finally, Zhang et al. [17] identified a mutation in the ZNF469 gene, which encodes a protein involved in corneal extracellular matrix development and maintenance, as a predisposing factor for corneal perforation after CXL.
In our case, all allergy tests to the eye drops used and allergenic substances tested (contact lens, chloramphenicol/betamethasone drops, dexamethasone drops, monofloxacin and levofloxacin drops and riboflavin) were negative. Thus, what triggered the patient’s inflammatory response remains unclear. Moreover, our patient did not present signs and symptoms of atopic dermatitis. This condition is known to be associated with an immune dysregulation characterised by increased expression of Th17 and interferon gamma, increased circulating regulatory T cell and increased CLA-Th2 subsets [28], which could lead to an abnormal immune and inflammatory response.
We achieved something remarkable in managing our patient: we avoided PK à chaud and instead performed DALK, which has numerous safety advantages, including larger diameter grafts with a reduced risk of rejection, particularly in children and young patients [29]. Performing a conjunctival flap allowed us to turn off the inflammation and to avoid perforation, promoting healing of the stroma. It has been used successfully in cases with deep ulcers, descemetocele or corneal perforation [30, 31]. We used the technique described by Gundersen [9] in 1958, which involves covering the whole cornea with a conjunctival flap dissected from the upper bulbar conjunctiva and approximating and suturing the cut edges. The flap is capable of restoring ocular surface integrity while providing metabolic and mechanical support for corneal healing, allowing the chance to perform DALK at a later time. Most of the cases of corneal perforation after CXL reported in the literature were treated with PK à chaud (Table 1) [12, 13, 15, 16, 18, 20,21,22]. This procedure is effective in restoring eye integrity and vision but exposes patients to prolonged steroid therapy and the risk of graft rejection, endothelial failure, secondary glaucoma and cataract formation [20]. Sasaki et al. [19] described a case of amniotic membrane transplant (AMT), which allowed them to control the inflammation, to prevent perforation and to avoid PK. AMT may be considered an alternative option to a conjunctival flap for the treatment of acute stromal melting. In our opinion, a conjunctival flap offers a more effective tectonic support in cases with a high risk of perforation and its longer duration allows delaying surgery until the acute inflammatory phase has resolved. In the case of infective aetiology, AMT may impair treatment penetration and visualisation of the response to therapy. Therefore, it should be performed after the initial response to antimicrobials, or once the infectious component has been adequately controlled [32].
In conclusion, CXL is a safe and effective technique in the treatment of keratoconus in children and adults; however, it can have serious complications that could eventually lead to corneal perforation. While identification of the causative agent is essential in guiding the therapy, it is not always possible to define a certain aetiology. To our knowledge, this is the first case of severe non-infectious corneal melting that was managed with a conjunctival flap and subsequent DALK. A conjunctival flap is an excellent option to save the integrity and to promote healing of the cornea, with the purpose of performing subsequent reconstructive surgery in an elective setting. When possible, DALK allows preserving the host corneal endothelium, reducing the risk of rejection and late endothelial failure that are particularly relevant in young patients.
Availability of data and materials
Data is provided within the manuscript.
References
Gomes JAP, Donald T, Rapuano C, Belin MW, Ambròsio R, Guell JL, et al. Global consensus on keratoconus and ectatic diseases. Cornea. 2015;34(4):359–69.
Perez-Straziota C, Gaster RN, Rabinowitz YS. Corneal cross-linking for pediatric keratcoconus review. Cornea. 2018;37(6):802–9.
Moramarco A, Mastrofilippo V, Romano MG, Iannetta D, Braglia L, Fontana L. Efficacy and safety of accelerated corneal cross-linking for progressive keratoconus: a 5-year follow-up study. J Refract Surg. 2020;36(11):724–30.
Fard AM, Reynolds AL, Lillvis JH, Nader ND. Corneal collagen cross-linking in pediatric keratoconus with three protocols: a systematic review and meta-analysis. J AAPOS. 2020;24(6):331–6.
Randleman JB, Khandelwal SS, Hafezi F. Corneal cross-linking. Surv Ophthalmol. 2015;60(6):509–23.
Agarwal R, Jain P, Arora R. Complications of corneal collagen cross-linking. Indian J Ophthalmol. 2022;70(5):1466–74.
Ferdi AC, Nguyen V, Gore DM, Allan BD, Rozema JJ, Watson SL. Keratoconus natural progression: a systematic review and meta-analysis of 11 529 eyes. Ophthalmology. 2019;126(7):935–45.
Fung SSM, Mason M, Gore DM, Mireskandari K, Ali A. Technique for pediatric corneal crosslinking under general anesthesia. J APAPOS. 2020;24(3):162–4.
Gundersen T. Conjunctival flaps in the treatment of corneal disease with reference to a new technique of application. AMA Arch Ophthalmol. 1958;60(5):880–8.
Vinciguerra R, Bordignon N, Ferraro V, Mazzotta C, Rosetta P, Vinciguerra P. Corneal collagen cross-linking for progressive keratoconus in pediatric patients: up to 14 years of follow-up. Am J Ophthalmol. 2023;255:170–7.
Spoerl E, Mrochen M, Sliney D, Trokel S, Seiler T. Safety of UVA-riboflavin cross-linking of the cornea. Cornea. 2007;26(4):385–9.
Rama P, Di Matteo F, Matuska S, Paganoni G, Spinelli A. Acanthamoeba keratitis with perforation after corneal crosslinking and bandage contact lens use. J Cataract Refract Surg. 2009;35(4):788–91.
Labiris G, Kaloghianni E, Koukoula S, Zissimopoulos A, Kozobolis VP. Corneal melting after collagen cross-linking for keratoconus: a case report. J Med Case Rep. 2011;5(1):152.
Angunawela RI, Arnalich-Montiel F, Allan BDS. Peripheral sterile corneal infiltrates and melting after collagen crosslinking for keratoconus. J Cataract Refract Surg. 2009;35(3):606–7.
Rana M, Lau A, Aralikatti A, Shah S. Severe microbial keratitis and associated perforation after corneal crosslinking for keratoconus. Cont Lens Anterior Eye. 2015;38(2):134–7.
Mohamed-Noriega K, Butrón-Valdez K, Vazquez-Galvan J, Mohamed-Noriega J, Cavazos-Adame H, Mohamed-Hamsho J. Corneal melting after collagen cross-linking for keratoconus in a thin cornea of a diabetic patient treated with topical nepafenac: a case report with a literature review. Case Rep Ophthalmol. 2016;7(1):119–24.
Zhang W, Margines JB, Jacobs D, Rabinowitz YS, Hanser E, Chauhan T. Corneal perforation after corneal cross-linking in keratoconus associated with potentially pathogenic ZNF469 mutations. Cornea. 2019;38(8):1033–9.
Schear M, Ragam A, Seedor J, Udell I, Shih C. Rapid keratitis and perforation after corneal collagen cross-linking. J Ophthalmol Case Rep. 2020;18:100658.
Sasaki T, Ide T, Toda I, Kato N. Amnwiotic membrane transplantation as a treatment for sterile infiltration and corneal melting after corneal crosslinking for keratoconus. Case Rep Ophthalmol. 2018;9(1):185–9.
Tillmann A, Daniel K, Borrelli M, Seidl M, Menzel J, Seiler TG, et al. Acute corneal melt and perforation - A possible complication after riboflavin/UV-A crosslinking (CXL) in keratoconus. J Ophthalmol Case Rep. 2022;28:101705.
Gokhale NS, Vemuganti GK. Diclofenac-induced acute corneal melt after collagen crosslinking for keratoconus. Cornea. 2010;29(1):117–9.
Barut Selver O, Metin DY, Hilmioglu Polat S, Dogen A, Palamar M. Fungal keratitis and corneal perforation as a rare complication of corneal collagen cross-linking treatment. Cornea. 2023;42(9):1179–82.
Guidera AC, Luchs JI, Udell IJ. Keratitis, ulceration, and perforation associated with topical nonsteroidal anti-inflammatory drugs. Ophthalmology. 2001;108(5):936–44.
O’Brien TP, Li QJ, Sauerburger F, Reviglio VE, Rana T, Ashraf MF. The role of matrix metalloproteinases in ulcerative keratolysis associated with perioperative diclofenac use. Ophthalmology. 2001;108(4):656–9.
Gabison EE, Chastang P, Menashi S, Mourah S, Doan S, Oster M, et al. Late corneal perforation after photorefractive keratectomy associated with topical diclofenac: involvement of matrix metalloproteinases. Ophthalmology. 2003;110(8):1626–31.
Çakmak S, Sucu M, Yildrim Y, Kepez YB, Kirgiz A, Bektașo D, et al. Complications of accelerated corneal collagen cross-linking: review of 2025 eyes. Int Ophthalmol. 2020;40(12):3269–77.
Faschinger C, Kleinert R, Wedrich A. [Corneal melting in both eyes after simultaneous corneal cross-linking in a patient with keratoconus and down syndrome]. Ophthalmologe. 2010;107(10):951–2, 954–5.
Ramírez-Marín HA, Silverberg JI. Differences between pediatric and adult atopic dermatitis. Pediatr Dermatol. 2022;39(3):345–53.
Vanathi M, Raj N, Kusumesh R, Aron N, Gupta N, Tandon R. Update on pediatric corneal diseases and keratoplasty. Surv Ophthalmol. 2022;67(6):1647–84.
Jhanji V, Young AL, Mehta JS, Sharma N, Agarwal T, Vajpayee RB. Management of corneal perforation. Surv Ophthalmol. 2011;56(6):522–38.
Nizeyimana H, Zhou D, Liu X, Pan X, Liu C, Lu C, et al. Clinical efficacy of conjunctival flap surgery in the treatment of refractory fungal keratitis. Exp Ther Med. 2017;14(2):1109–13.
Singhal D, Nagpal R, Mahara P, Sinha R, Agarwal T, Sharma N, et al. Surgical alternatives to keratoplasty in microbial keratitis. Surv Ophthalmol. 2021;66(2):290–307.
Funding
All the Authors of this manuscript received no funding for this research.
Author information
Authors and Affiliations
Contributions
A.M., N.dG. and L.F wrote the main manuscript text and L.G. and A.G. prepared figures, table and video. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from the patient’s parents. This study was approved by the Institutional Review Board and performed in accordance with the tenets of Declaration of Helsinki.
Consent for publication
Written informed consent was obtained from the patient’s parents for the publication of this case report.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary Material 1.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Moramarco, A., di Geronimo, N., Gardini, L. et al. Management of corneal melting after collagen cross-linking for keratoconus: a case report and a review of the literature. BMC Ophthalmol 24, 131 (2024). https://doi.org/10.1186/s12886-024-03400-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-024-03400-1