Abstract
Purpose
To investigate the association of subjects with refractive error and diabetic retinopathy (DR) in the United States comparing results between different race groups.
Methods
All data were derived from National Health and Nutrition Examination Survey (NHANES) from 2005 to 2008. The data were divided into four groups (emmetropia, mild myopia, high myopia, hypertropia) according to the spherical equivalent (SE), and those who met the enrollment conditions were selected as the study subjects. Multivariable logistic regression analysis was used to evaluate the relationship between refractive error and diabetic retinopathy risk.
Results
A total of 1317 participants were included in the study, including 331 participants with diabetic retinopathy, and 986 without diabetic retinopathy. After adjustment for potential confounders, subjects with high myopia were associated with a lower risk of diabetic retinopathy. The odds ratio (OR) was 0.44, 95% confidence interval (CI): (0.20–0.96), P-value = 0.040 in the multivariate regression analysis. Subgroup analyses showed that subjects with high myopia in the non-Hispanic Black group were associated with decreased odds of diabetic retinopathy. (OR was 0.20, and 95% CI: 0.04–0.95, P-value = 0.042).
Conclusion
The results show that high myopia is associated with diabetic retinopathy in diabetic patients.
Similar content being viewed by others
Introduction
Diabetic retinopathy is one of the leading causes of blurred vision in middle-aged and elderly patients [1]. Irreversible central and peripheral vision loss can be triggered when effective treatment is not timely [2, 3]. Epidemiological studies have identified a variety of important systemic factors that influence the development of diabetic retinopathy, such as kidney damage, duration of diabetes mellitus, glycemic control, insulin use, hypertension, and cardiovascular disease [4,5,6]. Furthermore, several studies have mentioned that myopia is one of the factors that are protective against diabetic retinopathy. The correlation of these two eye diseases has been studied for over half a century [7,8,9,10,11,12,13,14]. Although the pathogeneses are different, the progressing development of high myopia and diabetic retinopathy both contribute to high risks of visual impairment. Through complete fundus examination (OCT, fundus photos), ophthalmologists can accurately determine the development of high myopia and diabetic retinopathy [15]. However, these studies focus on the analysis of the correlation between patients with diabetic retinopathy and those with low or moderate myopia, and rarely analyze patients with high myopia. In addition, there are far more Asian population studies than Western population studies. To more accurately explore the relationship between diabetic retinopathy and different refractive degrees in western different races, we analyzed the data from the NHANES dataset.
Materials and methods
Data source and study population
The National Health and Nutrition Examination Survey (NHANES) is a survey of the noninstitutionalized civilian US population conducted by the Centers for Disease Control since 1959. Representative participants were randomly selected through a multistage sampling design to assess their health and nutritional status. According to the 1975 Helsinki Declaration, all participants provided informed consent before enrollment.
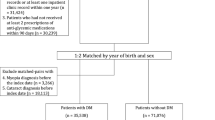
Two study protocols of NHANES (2005–2008) were collected in our analysis. The flow diagram of the participation is presented in Fig. 1. A total of 6797 participants aged ≥ 40 years had retinal photographs and were obtained. We excluded those with incomplete retinopathy information and vision data (n = 1198), no diabetes mellitus (n = 4109), and absence of covariates (n = 173). 1317 subjects were ultimately included in this study.
Definition of diabetic retinopathy
Participants sat in a room with no windows and lights off, and two images of the fundus exam were obtained using the Canon EOS 10D digital camera (Canon, Tokyo, Japan) and the Canon CR6-45N Ophthalmic Digital Imaging System. The pictures provided photographic documentation of the optic disc, macula, and substantial portions of the temporal arcades. Diabetic retinopathy was diagnosed by ophthalmologists at the University of Wisconsin. Researchers evaluated grading standards of diabetic retinopathy based on the Early Treatment for Diabetic Retinopathy Study (ETDRS). In the study, diabetic retinopathy was defined as the presence of retinal microaneurysms, blot hemorrhage, hard exudate, soft exudate, intraretinal microvascular abnormalities, venous beading, or fibrous proliferation. Also, clinically significant macular edema (CSME) on photographs in patients with diabetes was considered as diabetic retinopathy.
Assessment of refractive error
Objective refraction of both eyes was assessed using the Nidek Autorefractor Model ARK-760, without cycloplegia or pupillary dilation. The data of measurements were converted into SE calculated as the spherical value plus half of the astigmatic value. Emmetropia was defined as the average SE value from -1.0 D to 1.0 D, mild myopia from -1.0 D to -5.0 D, high myopia as less than or equal to -5.0 D, and hypertropia as more than 1.0 D.
Ascertainment of diabetes mellitus
The definition of Diabetic Mellitus in the NHANES study was described previously. According to the criteria, (1) Diabetic Mellitus was ascertained by the self-reported history of a physician diagnosis DIQ010 “Doctor told you to have diabetes” in the “Diabetes” questionnaire section in NHANES. The answer “yes” represented Diabetic Mellitus; (2) glycated hemoglobin A1c (HbA1c) ≥ 6.5%; (3) received antidiabetic treatments including insulin or oral hypoglycemic agents.
Other variables
Demographic characteristics were collected from a computer-assisted personal interview system including age, gender, race/ethnicity (non-Hispanic white, non-Hispanic Black, Hispanic, other), and education attainment (high school or below, any college). Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. The family poverty income ratio (PIR) compares family income to US census-defined poverty levels. The CVD-related information was assessed by a self-reporting questionnaire of coronary heart disease, angina, myocardial infarction, stroke, or congestive heart failure. Cigarette smoking status was attained by using the questions “Do you now smoke cigarettes?”, and “Smoked at least 100 cigarettes in life?”.
Statistical analysis
We obtained and merged the data from the 2005–2008 NHANES as mentioned previously. For the description of the baseline characteristics, categorical variables and continuous variables were performed using the chi-squared test and t-test for proportions and means, respectively.
Three logistic regression models were used to evaluate the relationship between high myopia and diabetic retinopathy, and the adjusted ORs and 95% CI were calculated. Model I was unadjusted regression. Next, Model II was adjusted for sex, age, and race/ethnicity. Finally, Model III was further adjusted for education level, BMI, PIR, CVD, hypertension, and smoking based on Model II. All statistical analyses were conducted using SAS (version 9.4). All tests were two-sided with a significance level of p < 0.05.
Result
A total of 1317 participants met the criteria after excluding missing data of gradable fundus photographs, incomplete vision data, and non-diabetics. Among them were 986 subjects with non-diabetic retinopathy, and 331 subjects with diabetic retinopathy. In addition, there were 610 subjects in the total study population with refractive errors (46.32%).
Characteristics of the study population
The demographic characteristics of subjects in the study population with and without high myopia are described in Table 1. Compared to the subjects in the non-diabetic retinopathy group, those with diabetic retinopathy tend to have lower PIR levels (2.57 ± 1.59 vs. 2.31 ± 1.44 kg/m2, P = 0.010). There were more Female subjects in the diabetic retinopathy group than in the non-diabetic retinopathy group (56.50% vs. 48.68%, P = 0.014). Participants with diabetic retinopathy were likely to have CVD (26.89% vs. 17.34%, P = < 0.001).
Associations of refractive error with diabetic retinopathy
Among the participants in the present study, diabetic retinopathy compared with non-diabetic retinopathy was associated with a lower risk of high myopia, and the association was not significant between other refractive degrees and diabetic retinopathy. The results from the multivariate logistic regression were shown in Table 2. In unadjusted analysis (Model I), subjects with high myopia had an OR of 0.39 (95% CI: 0.18–0.84, P-value = 0.016) for diabetic retinopathy. After adjusting for age, sex, and race/ethnicity (Model II), the results were significantly unchanged. The OR (95% CI) of diabetic retinopathy was 0.43 (95% CI: 0.20–0.93, P-value = 0.032) in the high myopia patients. After additional adjustments including education, BMI, PIR, CVD and smoke (Model III), the association between high myopia and diabetic retinopathy remained significant. (OR: 0.44, 95%CI: 0.20–0.96, P-value = 0.040).
Multivariate Analysis for diabetic retinopathy and the Risk of high myopia in different races
In this multivariable analysis (Table 3), three models were adjusted for the same variables as Table 2. The correlation between diabetic retinopathy and high myopia persisted in the non-Hispanic Black group, while there was no association in other races. The OR of the non-Hispanic Black group was 0.20 (95%CI: 0.04–0.95, P-value = 0.042) after adjusting additional covariate including education, BMI, PIR, CVD, and smoke by Model III.
Discussion
We used NHANES 2005–2008 data, which was collected from a public source with a complex multistage survey design for our cross-sectional study, and the results were consistent in different statistical models. After adjusting all the factors, we substantiated that the protective effect of high myopia was associated with a reduced likelihood of diabetic retinopathy (OR: 0.44, 95% CI: 0.18–0.96) In the stratified analyses, subjects with high myopia levels did have a significantly lower risk of diabetic retinopathy in the non-Hispanic Black group (OR: 0.20, 95%CI: 0.04–0.95).
The prevalence of people with high myopia from this screening data was 5.69%, which is lower than the U.K. population (9.5%), but higher than the Chinese (3.93%) and elder Indian population (< 1%) [16,17,18]. Many epidemiological surveys had proposed that an increase in refractive is a protective influence against diabetic retinopathy. However, some studies showed conflicting results in severe myopia in meta-analysis studies [19,20,21,22].
In recent years, axial length has been considered to be one of the most important eye measurement standards for diagnosing myopia, and more than 26 mm can be regarded as high myopia [23, 24]. Therefore, the relationship between severe myopia and diabetic retinopathy was also assessed based on the axial length in some studies. Two Singaporean cohort studies had described that the OR value of subjects with diabetic retinopathy were 0.86 and 0.68 per 1 mm increase in axis length, respectively [7, 9]. As for the Chinese population in Beijing, Xu et al. explored the incidence of diabetic retinopathy and its related factors in 2602 participants during a ten-year study. The results showed a total of 109 new patients with diabetic retinopathy during the ten years. These patients had a shorter eye axis length than the non-diseased person (OR: 0.48; 95% CI: 0.33–0.71) [25]. The prevalence of diabetic retinopathy was not related to refractive measurements, but the long axial length was associated with lower diabetic retinopathy [12]. This conclusion was similar to another study of Chinese populations [26]. In the cross-section study, Wang et al. measured axial lengths as an eye parameter for the prevalence and severity of diabetic retinopathy. A higher prevalence of diabetic retinopathy is associated with shorter axial lengths (OR: 0.81, 95% CI: 0.70–0.95) [13]. Unfortunately, although longer axial length is closely related to diabetic retinopathy, the structural component of participants was not measured in the NHANES datasets. Thus, we could not discuss the influence of axial length in our analysis even if it's an important diagnostic indicator.
According to the above-mentioned, Myopia is widely considered to be one of the protective factors for DR, but most studies have explored the situation in Asia. Few studies have explored the relationship between high myopia and DR in different Western populations based on large sample sizes. We found that high myopia has a significant negative relationship with DR in black people. There was a negative correlation between high myopia interval and diabetic retinopathy in univariate analysis (OR: 0.39, 95% CI: 0.18–0.84). After adjustment for age, gender, and race (Model II), high myopia might reduce the risk of diabetic retinopathy compared with those in the emmetropia group (OR: 0.43, 95% CI: 0.20–0.93). After further adjustment for education level, BMI, PIR, CVD, and smoking status (Model III), high myopia was still associated with a reduced diabetic retinopathy risk (OR: 0.44, 95% CI: 0.20–0.96).
To the best of our knowledge, there are no large-scale population-based studies that have focused on the relationship between high myopia and diabetic retinopathy in Western countries. Therefore, we investigated NHANES, a database with a complex sampling design in the United States population, and found high myopia is regarded as a factor influencing diabetic retinopathy in this public database. Moreover, the correlation between different races and diabetic retinopathy may be an influence factor. Nwanyanwu et al. described the relationship between race and the prevalence of diabetic retinopathy [27]. In the present study, High myopia is a protective factor for diabetic retinopathy in black populations.
Some limitations of this study should be acknowledged. First of all, the analysis was of cross-sectional design, thus our study cannot determine a causal relationship between two ocular diseases. Second, given the absence of data on the axial length of the eye in the NHANES dataset, we could not assess this main factor affecting refractive error. However, according to previous studies, some population-based studies also classify the degree of myopia solely based on SE value. If axial length assessment could be provided in later NHANES studies, combined with the SE classification method, it would provide more accurate measurements for myopia severity. Last, we had not analyzed the association between high myopia and proliferative diabetic retinopathy, which represents the last stage of this extremely complex retinal disease. This is because very few participants simultaneously suffered from high myopia and proliferative diabetic retinopathy in our analysis.
Conclusion
Based on the analysis for adjusting potential confounding variables, we concluded that participants with high myopia have a lower risk of diabetic retinopathy in the U.S. population, and such a conclusion was also statistically significant in the non-Hispanic Black group. Future longitudinal studies are needed to promote an understanding of the relationship between high myopia and the progression of diabetic retinopathy.
Availability of data and materials
The datasets generated and analyzed during the current study are available in the NHANES database. https://wwwn.cdc.gov/Nchs/Nhanes/.
References
Yang P, Xu W, Liu L, Yang G. Association of lactate dehydrogenase and diabetic retinopathy in US adults with diabetes mellitus. J Diabetes. 2023.
Stitt AW, Curtis TM, Chen M, et al. The progress in understanding and treatment of diabetic retinopathy. Prog Retin Eye Res. 2016;51:156–86.
Elman MJ, Aiello LP, Beck RW, et al. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2010;117(6):1064-1077.e1035.
Yin L, Zhang D, Ren Q, Su X, Sun Z. Prevalence and risk factors of diabetic retinopathy in diabetic patients: A community based cross-sectional study. Medicine (Baltimore). 2020;99(9): e19236.
Wong TY, Cheung N, Tay WT, et al. Prevalence and risk factors for diabetic retinopathy: the Singapore Malay Eye Study. Ophthalmology. 2008;115(11):1869–75.
Gui SY, Wang XC, Qiao JC, et al. Association of retinopathy with risk of all-cause and specific-cause mortality in the National Health and Nutrition Examination Survey, 2005 to 2008. Front Public Health. 2023;11:1200925.
Lim LS, Lamoureux E, Saw SM, Tay WT, Mitchell P, Wong TY. Are myopic eyes less likely to have diabetic retinopathy? Ophthalmology. 2010;117(3):524–30.
Ganesan S, Raman R, Reddy S, Krishnan T, Kulothungan V, Sharma T. Prevalence of myopia and its association with diabetic retinopathy in subjects with type II diabetes mellitus: A population-based study. Oman J Ophthalmol. 2012;5(2):91–6.
Man RE, Sasongko MB, Sanmugasundram S, et al. Longer axial length is protective of diabetic retinopathy and macular edema. Ophthalmology. 2012;119(9):1754–9.
Pan CW, Cheung CY, Aung T, et al. Differential associations of myopia with major age-related eye diseases: the Singapore Indian Eye Study. Ophthalmology. 2013;120(2):284–91.
Chao DL, Lin SC, Chen R, Lin SC. Myopia is Inversely Associated With the Prevalence of Diabetic Retinopathy in the South Korean Population. Am J Ophthalmol. 2016;172:39–44.
Man REK, Gan ATL, Gupta P, et al. Is Myopia Associated with the Incidence and Progression of Diabetic Retinopathy? Am J Ophthalmol. 2019;208:226–33.
Wang Q, Wang YX, Wu SL, et al. Ocular Axial Length and Diabetic Retinopathy: The Kailuan Eye Study. Invest Ophthalmol Vis Sci. 2019;60(10):3689–95.
Lin Z, Li D, Zhai G, et al. High myopia is protective against diabetic retinopathy via thinning retinal vein: A report from Fushun Diabetic Retinopathy Cohort Study (FS-DIRECT). Diab Vasc Dis Res Jul-Aug. 2020;17(4):1479164120940988.
Iglicki M, Busch C, Zur D, et al. Dexamethasone implant for diabetic macular edema in naive compared with refractory eyes: The International Retina Group Real-Life 24-Month Multicenter Study. The IRGREL-DEX Study. Retina. 2019;39(1):44–51.
Cumberland PM, Bountziouka V, Hammond CJ, Hysi PG, Rahi JS. Temporal trends in frequency, type and severity of myopia and associations with key environmental risk factors in the UK: Findings from the UK Biobank Study. PLoS ONE. 2022;17(1): e0260993.
Wang M, Gan L, Cui J, et al. Prevalence and risk factors of refractive error in Qinghai, China: a cross-sectional study in Han and Tibetan adults in Xining and surrounding areas. BMC Ophthalmol. 2021;21(1):260.
Hamati JN, Das AV, Prashanthi GS, Behera UC, Narayanan R, Rani PK. Factors protecting against diabetic retinopathy in a geriatric Indian cohort. Indian J Ophthalmol. 2021;69(11):3167–72.
Wang X, Tang L, Gao L, Yang Y, Cao D, Li Y. Myopia and diabetic retinopathy: A systematic review and meta-analysis. Diabetes Res Clin Pract. 2016;111:1–9.
Fu Y, Geng D, Liu H, Che H. Myopia and/or longer axial length are protective against diabetic retinopathy: a meta-analysis. Acta Ophthalmol. 2016;94(4):346–52.
He M, Chen H, Wang W. Refractive Errors, Ocular Biometry and Diabetic Retinopathy: A Comprehensive Review. Curr Eye Res. 2021;46(2):151–8.
Wang YM, Lu SY, Zhang XJ, Chen LJ, Pang CP, Yam JC. Myopia Genetics and Heredity. Children (Basel). 2022;9(3).
Du R, Xie S, Igarashi-Yokoi T, et al. Continued increase of axial length and its risk factors in adults with high Myopia. JAMA Ophthalmol. 2021;139(10):1096–103.
Lee MW, Lee SE, Lim HB, Kim JY. Longitudinal changes in axial length in high myopia: a 4-year prospective study. Br J Ophthalmol. 2020;104(5):600–3.
Xu J, Xu L, Wang YX, You QS, Jonas JB, Wei WB. Ten-year cumulative incidence of diabetic retinopathy. The Beijing Eye Study 2001/2011. PLoS One. 2014;9(10):e111320.
Jiang JJ, Li XX, Yuan L, Ji LN, Wu X. Ocular biological structures and relevant risk factors in the occurrence of diabetic retinopathy in diabetes mellitus patients. Zhonghua Yan Ke Za Zhi. 2012;48(10):898–902.
Nwanyanwu K, Nunez-Smith M, Gardner TW, Desai MM. Awareness of diabetic retinopathy: insight from the national health and nutrition examination survey. Am J Prev Med. 2021;61(6):900–9.
Acknowledgements
None.
Funding
This work was supported by Grant 2020YFC2003904 from National Key Research & Development Program, Grant 82070992 from National Natural Science Foundation, Grant YG2021ZD18 from Shanghai Jiaotong University Medical Engineering Cross Research, Grant CTCCR-2018B01 from Clinical Research Innovation Plan of Shanghai General Hospital, Grant 81770953 from National Natural Science Foundation.
Author information
Authors and Affiliations
Contributions
WT and BK designed the study, WT wrote the main manuscript, WZ provide statistical advice, and all authors (WT, YY, YW, WZ, BK) critically revised the manuscript for important intellectual content. All authors approved the final version of the manuscript and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The NHANES serial cross-sectional survey was conducted in accordance with ethical standards and regulations, including obtaining documented consent from participants. The dataset used in the present study had all individually identifiable information removed, making it suitable for non-human subjects research, which exempts it from requiring additional ethical approval or consent to participate.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ten, W., Yuan, Y., Zhang, W. et al. High myopia is protective against diabetic retinopathy in the participants of the National Health and Nutrition Examination Survey. BMC Ophthalmol 23, 468 (2023). https://doi.org/10.1186/s12886-023-03191-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-023-03191-x