Abstract
Rationale
Nd:YAG (neodymium:yttrium-aluminum-garnet) capsulotomy (Nd:YAG-caps) is the gold standard for the treatment of PCO (Posterior Capsule Opacification). There is a lack of real-world data about Nd:YAG-caps use.
Purpose
This study’s objectives were to estimate Nd:YAG-caps incidence in France, to describe the patient characteristics, and to analyze the time between surgeries and capsulotomies. Setting: The study was based on data extracted from the EGB database, a 1/97th sample representative of the French population. Design: observational, retrospective, cohort study using national claims data.
Methods
French adult patients who underwent Nd:YAG-caps between 2014 and 2017 were selected. Main outcomes were the number of patients and procedures performed and the risk factors associated with early Nd:YAG-caps. Results: During the study period, Nd:YAG-caps were performed in 8,425 patients accounting for 10,774 procedures. The extrapolation to the French population led to estimate that 253.103 patients had Nd:YAG-caps, representing 312.103 procedures in 2017. The mean age at Nd:YAG-caps was 75.1 (± 10.2) years. About 36% of patients presented at least one ocular comorbidity. Nd:YAG-caps was performed within 2 years after surgery in 33.0% of patients and within one year in 9.8% of patients. Patients with Nd:YAG-caps within the first year (OR CI95 0.721 [0.673–0.772]) or in the first two years (OR CI95 0.721 [0.673–0.772]) were younger than patients with later Nd:YAG-caps and had a more frequent history of treated ocular diseases (OR 1.516 and 1.178, respectively).
Conclusions
This study brought new real-world and large-scale data regarding Nd:YAG-caps use and gave an updated insight into the patients’ characteristics.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
More than 940.103 cataract surgeries were performed in France in 2021, making cataract surgery the most frequent ophthalmological procedure [1, 2]. Secondary posterior capsular opacification (PCO) is a common complication, occurring within months after surgery, with an estimated 5-year rate between 30% and 50% [3,4,5]. PCO is managed by performing a capsulotomy with a Nd:YAG (neodymium:yttrium-aluminum-garnet) laser [6], allowing patients to regain satisfying vision within hours. Post-operative treatment can include anti-inflammatory and/or hypotonizing eyedrops for several days [7, 8].
With a significant proportion of cataract surgeries ultimately resulting in treated PCO, these ophthalmic procedures represent a substantial economic burden and public health impact. In addition, other potential adverse events due to cataract surgery or capsulotomy may increase this burden and deteriorate patients’ quality of life, in a population mostly consisting of elderly and comorbid patients [9, 10]. Recent and exhaustive knowledge on the most frequent complication of cataract surgery, as well as on the potential factors influencing its occurrence, is crucial for health authorities decision-making, even more with the global aging of the population.
There is a lack of real-world data about the epidemiology of Nd:YAG capsulotomy (Nd:YAG-caps). Few databases allow to access patient-level data with both sufficient representativeness and data granularity to ensure results generalizability. The French national representative sample (Echantillon Généraliste des Bénéficiaires – EGB), satisfies both conditions and exhaustively captures patients’ reimbursed healthcare resources and can complement the clinical studies carried on smaller populations, notably focusing on the risk of Nd:YAG-caps by type of implant. This FreYAG1 study aimed at estimating the up-to-date number of Nd:YAG-caps performed in France, describing patients’ characteristics, analyzing the delay between surgery and capsulotomy, and assessing risk factors of earlier YAG, notably regarding age.
Materials and methods
General design
This was an observational, retrospective, cohort study performed among patients who underwent Nd:YAG-caps between January 1st, 2014, and December 31st, 2017. This study used reimbursement data from the EGB, based on healthcare claims from the French national health data system.
Study population
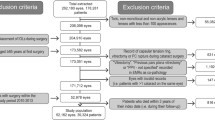
Adults who underwent Nd:YAG-caps between January 1st, 2014, and December 31st, 2017 (study period), were identified in EGB to assess overall and annual use of Nd:YAG-caps. Among them, patients with complete coverage (continuous affiliation to an insurance scheme) from January 1st, 2012, were considered for characteristics description. Nd:YAG-caps were identified using a specific code from French procedure classification. The date of Nd:YAG-caps was defined as the index date. In case of multiple Nd:YAG-caps, the first one was considered. Comorbidities and medical history of interest were assessed over a 2-year period before index date.
Data source
The EGB is a 1/97th sample of insured individuals and gathers ≈ 700.103 persons. It is an exhaustive pseudonymized patient-level collection of claims data, representative of the French population in terms of age, gender, and geographical area [11,12,13]. It exhaustively gathers patients’ healthcare reimbursements, using specific coding systems for procedures, laboratory tests, medical devices, diagnoses (hospitalizations), or drugs [14,15,16,17]. Only expensive drugs and medical devices are captured during hospitalizations, as others are part of the hospital stay fee (Diagnosis Related Groups [DRG]). Beneficiary data include age, gender, city of residence, date of care, care settings, as well as date and cause of death.
Outcomes
The primary outcome was the number of patients undergoing Nd:YAG-caps and the number of procedures performed. They have been estimated overall and by year over study period. Data from EGB were extrapolated to the national scale for each year, adjusted on age and gender based on the French population census for the same year [18].
The secondary outcomes were the description of the patients’ characteristics. The sociodemographic characteristics were analyzed at index date and included age, gender, and district of residence. The comorbidities were assessed using validated algorithms based on hospital diagnoses and outpatient reimbursed treatments and were split into 3 categories. The non-ocular comorbidities included cardiovascular diseases, diabetes, malignant neoplasms, assessed over a 2-year period before index date. The ocular comorbidities included retinal vein occlusion (RVO), uveitis, diabetic retinopathy, prior Nd:YAG-caps, and cataract surgery, assessed over the same period. Finally, known Nd:YAG-caps complications were analyzed over a 1-year period before the index date and included Ocular hypertension (OHT) or glaucoma, retinal detachment (RD), vitrectomy, and treated diabetic macular edema (DME), age-related macular degeneration (ARMD), uveitis, or RVO [19]. Detailed algorithms are available as supplementary material. Patients’ characteristics were also analyzed according to the time between surgery and Nd:YAG-caps, which was categorized as very early (≤ 1 year post-surgery), early (between 1 and 2 years post-surgery), and late (> 2 years post-surgery).
Statistical methods
All analyses were performed using the SAS® version 9.4 (SAS Institute Inc. Cary, NC, USA). Quantitative variables were described as means, standard deviations, medians, first (Q1) and third (Q3) quartiles, and extreme values; qualitative variables as absolute frequencies and percentages by category. Logistic regression models were developed including characteristics of interest, using a backward method with preliminary selection. Interactions with a p-value threshold ≤ 0.10 were included in the final models. The covariables of interest were the age at the index date; gender; ocular and non-ocular comorbidities, as well as known Nd:YAG-caps complications.
Ethical considerations
Prior to data management, access to SNDS data was granted by the French national health data institute (Institut National des Données de Santé – INDS), implying the protocol validation by the French expert committee for health research and evaluation (Comité d’Expertise pour les Recherches, les Études et les Évaluations dans le domaine de la Santé - CEREES), as well as by the French national data protection agency (Commission Nationale de l’Informatique et des Libertés – CNIL). Once approved, EGB data were analyzed on the SNDS secure portal by data managers and statisticians trained to patient-related data securization. No individual data was extracted from the SNDS portal. This study was conducted in compliance with the French Data Protection Act and in accordance with applicable ethical principles set out in the Declaration of Helsinki.
Results
Nd:YAG laser capsulotomy
During the study period, 8,425 patients underwent Nd:YAG-caps, accounting for 10,774 procedures, as bilateral capsulotomy can occur (Fig. 1).
More than 2,000 patients had Nd:YAG-caps each year, ranging from 2,006 (2,312 procedures) in 2014 to 2,550 (3,141 procedures) in 2017. In 2017, the EGB extrapolation [CI95%] to the French population estimated that 253.103 [252.103; 254.103] patients had a Nd:YAG-caps, corresponding to 312.103 [311.103; 313.103] procedures. In 2017, 9 districts (out of 100) accounted for > 20% of patients with Nd:YAG-caps. Among them, Gironde (n = 282), Bouches-du-Rhône (n = 269) and Nord (n = 257) each represented > 3% of overall patients (Fig. 2). For the same year, 4 French districts had > 800 Nd:YAG-caps performed per 100,000 inhabitants, all of them in the south of France (Table 1 – Fig. 2).
Patient characteristics
Among the 8,425 patients with a Nd:YAG-caps, 7,462 patients (9,560 procedures) had no discontinuation in healthcare coverage. The sex ratio was 0.55 with 4,817 (64.6%) women. The mean (SD) age at index date was 75.1 (10.2) years, with most patients being aged ≥ 75 years (n = 4,409; 59.1%), while patients aged < 40 years accounted for 0.6% (Table 2).
About 15% of patients had a history of diabetes (n = 1,390, 18.6%) or malignant neoplasm (n = 1,041, 14.0%). Almost 75% of patients (n = 5,576, 74.5%) had a cardiovascular disease. Ocular comorbidities were identified in 35.6% (n = 2,654) of patients. Treated diabetic retinopathy accounted for fewer than 2% of the patients with ocular comorbidities (n = 49), while RVO and uveitis were almost never encountered. Among known Nd:YAG-caps complications, 1,049 (14.1%) patients had a history of OHT/glaucoma, 277 (3.7%) patients received a treatment for either ME, ARMD or RVO, and < 1% of patients had a history of RD (n = 44, 0.6%) or vitrectomy (n = 19, 0.3%).
Time to nd:YAG posterior capsulotomy
Among the 7,462 patients included, 2,466 (33.0%) had a cataract surgery 2 years before Nd:YAG-caps, of whom 732 (29.7%) were performed within the year before the index date while 1734 (70.3%) surgeries were performed between one and two years before it. More than half of them (n = 1,354, 54.9%) had two cataract surgeries within 2 years before Nd:YAG-caps, with a median (Q1 – Q3) delay between surgeries of 21.0 (7.0–49.0) days. Logistic regression model showed that patients who had a very early Nd:YAG-caps (i.e. <1 year post-surgery) were younger (OR 0.721 [0.673–0.772] for a 10-year increase) than those having a late one. They also had a more frequent history of glaucoma (OR 1.516 [1.240–1.855]) or other treated ocular diseases (OR 2.224 [1.610–3.072]). Moreover, patients who had a non-late Nd:YAG-caps (within 2 years) were younger than those having a later one. The odds ratio for a 10-year increase were 0.794 [0.757–0.833] and 0.587 [0.454–0.759] either without or with a history of treated ocular disease, respectively. Age and history of treated ocular disease had a significant interaction, making it impossible to analyze these covariates independently. The patients with non-late Nd:YAG-caps also had a more frequent history of treated ocular disease compared to those with late Nd:YAG-caps (Table 3). Each of the models analyzed in this study showed areas under curve of ≈ 0.60 and Hosmer Lemeshow test p-value of < 0.001, implying that other variables could impact these models.
The impact of young age on time to Nd:YAG-caps was highlighted by the proportion of patients aged < 65 years in each subgroup. This proportion was 22.4% among patients with very early Nd:YAG-caps. It decreased to 13.7% and 13.0% among patients with early and late Nd:YAG-caps, respectively. A similar trend was observed for patients with a history of glaucoma, as proportions decreased from 20.6 to 13.8% and 13.2%, for the same periods (Fig. 3).
Discussion
Our study estimated the epidemiology and the characteristics of patients undergoing Nd:YAG-caps, using an innovative approach taking Nd:YAG-caps as a starting point and analyzing prior cataract surgeries in a backward way.
Demographics
The mean age at Nd:YAG-caps was in line with the literature with mean ages at cataract surgery being between 74 and 77 years [5, 20, 21]. The proportion of women was 64.6% in this study, also in line with Daien et al’s study, with 59% of the cataract surgeries being among women, while the National Ophthalmology Database (NOD) audit from United Kingdoms showed that women seemed slightly more at risk of developing PCO (NOD audit-appendix 8) [5, 20].
According to the EGB data extrapolation, ≈ 253.103 patients have undergone Nd:YAG-caps in 2017, accounting for ≈ 310.103 procedures. During the same year, the French national health insurance database for reimbursed procedures (Open-CCAM) recorded 277.103Nd:YAG-caps [22]. As Open-CCAM does not exhaustively includes Nd:YAG-caps performed among outpatients in public hospitals, it seems acceptable to assess that 290.103 to 300.103Nd:YAG-caps are performed each year in France. The geographical distribution of Nd:YAG-caps seemed unsurprisingly linked to that of cataract surgeries, with the South being the most frequent region for cataracts and Nd:YAG-caps, as described in the 2019 French health authority report [23]. As shown in supplementary material displaying the geographic distribution of Nd:YAG-caps, cataract surgeries, and the density of ophthalmologists in France for the year 2017, these 3 components are highly correlated. Over our study’s 4 years (2014–2017), the increase in capsulotomies (+ 19.1%) appeared to have been slightly greater than the increase in cataract surgeries (+ 11.5%) [24]. It cannot be ruled out that the postoperative visual expectations of patients have increased over time, with an earlier request for capsulotomies.
Clinical characteristics and medical history
The proportion of patients with a history of diabetes was 18.6%, close to that from the French public health organism Santé Publique France in 2013, with around 16% of diabetic patients among subjects aged ≥ 70 years [25]. The most frequent comorbidities were cardiovascular impairments (75%). This is in line with the literature and might be mainly represented by high blood pressure (HBP). According to Yazdanyar et al. 2009 study, the prevalence of cardiovascular diseases in the United States was between 70% and 85% among patients aged ≥ 60 years [26]. The global burden of disease project estimated that non-HBP cardiovascular disease prevalence was around 43% among patients aged ≥ 75 years, while Esteban’s study estimated HBP prevalence in France at almost 70% among patients aged between 65 and 74 years [27, 28]. Hence, controlled HBP might not be of major risk for cataract or Nd:YAG-caps, despite being captured in this study.
In this study, 14.1% of patients had a history of OHT/glaucoma, in line with Delcourt et al. study from 2010, with a prevalence [CI 95%] of treated OHT and Glaucoma among elderly patients being 9.8 [6.7%; 12.9%] and 5.3% [3.0% ; 7.6%], respectively [29]. Similarly, OHT rates were estimated at 15.5% and 7.5% among men and women aged ≥ 60 years, respectively, by Bron et al. in 2006 [30].
This study is the first to highlight a potential link between several ocular pathologies and earlier Nd:YAG-caps. Despite young age and history of uveitis being risk factors already identified in daily practice, macular diseases and glaucoma were not known as such. A recent study based on 2008 to 2018 SNDS data showed that diabetic maculopathies and retinopathies were encountered among 0.1% and 0.2% of the overall French population, respectively. In the same study, the prevalences of treated DME and ARMD were about 0.1% and 1.0%, respectively [31]. In our study, the proportion of severe diabetic retinopathy reached 0.7%, while treated DME, ARMD, and RVO represented almost 4% of the patients. It seems that patients with an active macular disease were over-represented in Nd:YAG-caps population when compared to the overall French population. In spite of the greater frequencies of these pathologies observed in patients with earlier Nd:YAG-caps, a causal link with PCO remains unproven. Indeed, patients with chronic ocular disorders might simply have more regular scheduled ophthalmological visits. Hence, Nd:YAG-caps might be performed as soon as PCO is observed and before significant visual symptoms are recorded.
Time to nd:YAG posterior capsulotomy
More than half of patients with a Nd:YAG-caps within 2 years post-surgery had both eyes operated on, with an interval of 21 days, in line with Daien et al. EPISAFE study, with 29 days [20]. In the same study, cataract was performed on both eyes among 51.2% of patients, which seemed also in line with our results, even though surgery laterality cannot be assessed in EGB. In this study, most patients had Nd:YAG-caps > 2 years after cataract surgery, with 33.0% of patients having Nd:YAG-caps procedures performed within 2 years. It is comparable to the French observational studies from Ton Van et al. and Bourdiol Ducasse et al., which showed a mean time to Nd:YAG-caps of 32.17 months and around 25 months, respectively, in smaller cohorts [32, 33].
Unsurprisingly, elderly patients appeared to be less likely to have non-late Nd:YAG-caps than younger ones. A similar pattern was highlighted by Miller et al. US cohort which showed that older age was a protective factor for early Nd:YAG-caps (OR: 0.95 [0.92; 0.98]) [34]. On the other hand, patients with ocular comorbidities seemed more likely to undergo Nd:YAG-caps earlier than those without, potentially due to a closer ophthalmological follow-up, allowing an earlier detection of PCO. As models in this study did not exhaustively include all factors, this study cannot be used to assess whether a specific group of IOL results in earlier or more frequent capsulotomies, nor to assess Nd:YAG-caps-free survival. The NOD study brought substantial information on the probability of Nd:YAG-caps and the time between cataract and Nd:YAG-caps according to the type of IOL used. In fact, it showed that PCO rates can widely vary with material and design, at equivalent time points. According to the IOL material used (e.g. hydrophobic or hydrophilic IOL), the 2-year proportion of patients with subsequent Nd:YAG-caps varied from 2.2 to 7.0% and from 9.2 to 25.4% after 5 years, showing a threefold increase of Nd:YAG-caps procedures with hydrophilic IOLs [5].
Strengths and limitations
Overall, the French medico-administrative databases do not allow to control the data validity and quality. Some studies have reported that diagnoses coded in the French hospitalization database (PMSI) are not always reliable, leading to a risk of information bias related to coding errors. However, considering the large number of patients included, this bias is expected to have a limited impact. Similarly, it is not possible to ensure the completeness of the SNDS data, particularly regarding comorbidities. To improve data quality, algorithms combining inpatient and outpatient data (diagnoses, reimbursed drugs…) are an effective solution to optimize the identification of pathologies within the SNDS. The study results have been compared to the literature when available. The algorithms used in this study were reviewed by an independent scientific committee and are adapted from validated sources such as French national health insurance (Cnam) mapping of diseases, and literature [35]. A laterality bias can also be highlighted, as no specific clinical data is available in EGB to distinguish which eye has been operated on. However, an important proportion of patients seemed to undergo bilateral cataract surgery, as shown in the Schweitzer et al. FEMCAT study in France, with 63% of patients undergoing bilateral cataract surgery within a short interval. These findings mitigate the importance of the laterality bias [21]. Finally, the medico-administrative nature of claims databases such as EGB leads to a lack of clinical information, limiting the granularity of analyses undergone. For instance, no data is available on the surgeon performing the cataract surgery, the technique used per se, or the type of IOL implanted, which is billed as part of the diagnosis-related group. As specified above, and as shown in NOD audit, these factors can change the outcomes of a surgery, notably in terms of PCO rate [5]. However, the FEMCAT economic study showed that FLACS technique remains rarely used due to a relative lack of medico-economic advantage; and Monnet et al. multicentric analysis showed that multifocal implants represented around 6% of the IOLs in 2021 [36, 37]. These results tend to limit the potential biases due to the differences in practices.
Also, patients with ocular comorbidities could schedule more frequent visits with their ophthalmologists and may benefit from an earlier detection and Nd:YAG-caps for PCO. Similarly, health literacy can increase patients’ sensitivity to cataract-related ocular complications and lead to more frequent ophthalmologist appointments on patient’s initiative. Lin et al. Chinese cross-sectional study assessed the link between health literacy and patient-physician communication among patients with cataract, showing a threefold increased probability of poor patient-physician communication if inadequate health literacy (OR 3.6 [1.6; 8.1]) [38].
The main strength identified in this study is the source of data used. EGB is a nationwide population-representative sample of French health insurance beneficiaries, exhaustively gathering every reimbursed healthcare resource used by patients. When considering frequent diseases or procedures, as is the case with Nd:YAG-caps, the EGB brings a very high level of evidence, strong external validity, and good data generalizability, reinforced by the availability of a specific Nd:YAG-caps code. This study gave a good and informative estimate of the current use of Nd:YAG-caps in France, as well as an overview of the profiles of patients undergoing this procedure. Furthermore, the association of results from national claims database with that of clinical studies focused on the ophthalmological risk factors of PCO (e.g., type of IOL, use of coaxial I/A…) could provide important information to the health authorities on which techniques and technologies to promote in order to decrease the number of PCO [5, 39].
Conclusion
This study allowed us to fill the informational gap regarding real-world data about Nd:YAG-caps and give an updated insight into patients’ characteristics and main comorbidities. This study estimated that more than 250.103 patients undergo Nd:YAG-caps each year in France, accounting for more than 300.103 procedures in 2017. More than 30% of Nd:YAG-caps were performed within 2 years after the cataract surgery. When analyzing the patients’ characteristics at the date of Nd:YAG-caps, it appeared that patients with a history of ocular disease were more likely to undergo non-late Nd:YAG-caps. In the meantime, despite cataract surgery being mainly performed among older patients, younger ones seemed to have a shorter period between cataract and Nd:YAG-caps. This data must be considered as refractive cataract procedures are mostly undergone among younger patients.
Data Availability
Complete list of algorithms is available as Supplementary data. No additional data is available.
References
Caisse Nationale d’Assurance Maladie. Actes techniques de la CCAM en 2021 | L’Assurance Maladie. https://assurance-maladie.ameli.fr/etudes-et-donnees/actes-techniques-ccam-2021. Accessed 5 Oct 2022.
Agence Technique de l’Information sur l’Hospitalisation. Open CCAM 2021 | Stats ATIH. https://www.scansante.fr/mco-actes-ccam-par-etablissements/open-ccam-2021. Accessed 5 Oct 2022.
Ayed T, Rannen R, Naili K, Sokkah M, Gabsi S. [Risk factors for secondary cataract: a case-control study with multivariate analysis]. J Fr Ophtalmol. 2002;25:615–20.
Benzerroug M, Milazzo S. La cataracte secondaire. EMC Ophtalmologie. 2014;11.
Royal College of Ophthalmologists. RCOphth NOD PCO Report 2021.pdf. https://www.nodaudit.org.uk/u/docs/20/rijbxkcubs/RCOphth%20NOD%20PCO%20Report%202021.pdf. Accessed 5 Dec 2022.
Aron-Rosa D, Aron JJ, Griesemann M, Thyzel R. Use of the neodymium-YAG laser to open the posterior capsule after lens implant surgery: a preliminary report. J - Am Intra-Ocul Implant Soc. 1980;6:352–4.
Findl O, Buehl W, Bauer P, Sycha T. Interventions for preventing posterior capsule opacification. Cochrane Database Syst Rev. 2010;:CD003738.
Ling R, Borkenstein E-M, Borkenstein AF. Evaluation of nd:YAG Laser Capsulotomy Rates in a Real-Life Population. Clin Ophthalmol Auckl NZ. 2020;14:3249–57.
Dot C, Schweitzer C, Labbé A, Lignereux F, Rozot P, Goguillot M, et al. Incidence of retinal detachment, Macular Edema, and ocular hypertension after Neodymium:Yttrium-Aluminum-Garnet Capsulotomy: a Population-Based Nationwide Study-The french YAG 2 study. Ophthalmology. 2023;130:478–87.
de Juan-Marcos L, Blanco-Blanco JF, Hernández-Galilea E. Visual function and quality of life in pseudophakic patients before and after capsulotomy. Eur J Ophthalmol. 2012;22:943–9.
Bezin J, Duong M, Lassalle R, Droz C, Pariente A, Blin P, et al. The national healthcare system claims databases in France, SNIIRAM and EGB: powerful tools for pharmacoepidemiology. Pharmacoepidemiol Drug Saf. 2017;26:954–62.
Tuppin P, Rudant J, Constantinou P, Gastaldi-Ménager C, Rachas A, de Roquefeuil L, et al. Value of a national administrative database to guide public decisions: from the système national d’information interrégimes de l’Assurance Maladie (SNIIRAM) to the système national des données de santé (SNDS) in France. Rev Epidemiol Sante Publique. 2017;65(Suppl 4):149–67.
Roquefeuil LD, Studer A, Neumann A, Merlière Y. L’échantillon généraliste de bénéficiaires: représentativité, portée et limites. Prat Organ Soins. 2009;40:213–23.
Caisse Nationale d’Assurance Maladie. CCAM en ligne - CCAM. https://www.ameli.fr/accueil-de-la-ccam/index.php. Accessed 2 Jun 2021.
Caisse Nationale d’Assurance Maladie. Nomenclatures: NGAP et LPP. https://www.ameli.fr/infirmier/exercice-liberal/facturation-remuneration/nomenclatures-ngap-lpp/nomenclatures-ngap-lpp. Accessed 22 Sep 2021.
World Health Organization. ICD-10 Version:2019. https://icd.who.int/browse10/2019/en#/. Accessed 2 Jun 2021.
World Health Organization. WHOCC - ATC/DDD Index. https://www.whocc.no/atc_ddd_index/. Accessed 2 Jun 2021.
INSEE. Évolution de la population entre 2013 et 2018 et estimation de la population au 1er janvier 2021 | Insee. https://www.insee.fr/fr/statistiques/2012730. Accessed 9 Sep 2021.
O’Boyle D, Perez Vives C, Samavedam S, Ender F, deHaan J, Shaikh J, et al. PMD1 - POST-ND:YAG LASER COMPLICATIONS IN CATARACT PATIENTS TREATED FOR POSTERIOR CAPSULAR OPACIFICATION: A SYSTEMATIC LITERATURE REVIEW. Value Health. 2018;21:243.
Daien V, Korobelnik J-F, Delcourt C, Cougnard-Gregoire A, Delyfer MN, Bron AM, et al. French Medical-Administrative Database for Epidemiology and Safety in Ophthalmology (EPISAFE): the EPISAFE collaboration program in cataract surgery. Ophthalmic Res. 2017;58:67–73.
Schweitzer C, Brezin A, Cochener B, Monnet D, Germain C, Roseng S, et al. Femtosecond laser-assisted versus phacoemulsification cataract surgery (FEMCAT): a multicentre participant-masked randomised superiority and cost-effectiveness trial. Lancet Lond Engl. 2020;395:212–24.
Agence Technique de l’Information sur l’Hospitalisation. Open CCAM 2017 | Stats ATIH. https://www.scansante.fr/open-ccam/open-ccam-2017. Accessed 18 Aug 2021.
Haute autorité de Santé. Indications et contre-indications de la chirurgie de la cataracte liée à l’âge. https://www.has-sante.fr/upload/docs/application/pdf/2019-02/app_151_rapport_elaboration_cataracte_vf_2019-02-26_15-03-47_723.pdf.
Agence Technique de l’Information sur l’Hospitalisation. MCO actes CCAM par établissements (Open CCAM) | Stats ATIH. https://www.scansante.fr/opendata/pmsi-mco/ccam. Accessed 17 Feb 2022.
Santé Publique France. Prévalence et incidence du diabète. https://www.santepubliquefrance.fr/maladies-et-traumatismes/diabete/prevalence-et-incidence-du-diabete. Accessed 8 Sep 2021.
Yazdanyar A, Newman AB. The burden of cardiovascular disease in the elderly: morbidity, mortality, and costs. Clin Geriatr Med. 2009;25:563–77. vii.
Global Burden of Disease Collaborative Network. Global Burden of Disease Collaborative Network. Global Burden of Disease Study – 2019. 2021.
Perrine A-L, Lecoffre C, Olié V. Prévalence de l’hypertension artérielle chez les adultes en France en 2015, étude ESTEBAN. Rev DÉpidémiologie Santé Publique. 2018;66:50.
Delcourt C, Korobelnik J-F, Barberger-Gateau P, Delyfer M-N, Marie-Bénédicte R, Le Goff M, et al. Nutrition and Age-Related Eye Diseases: the ALIENOR (Antioxydants, LIpides Essentiels, Nutrition et maladies OculaiRes) study. J Nutr Health Aging. 2010;14:854–61.
Bron A, Baudouin C, Nordmann J-P, Rouland J-F, Thomas F, Bean K, et al. [Prevalence of intraocular hypertension and glaucoma in a nonselected french population]. J Fr Ophtalmol. 2006;29:635–41.
Creuzot-Garcher CP, Srour M, Baudin F, Daien V, Dot C, Nghiem-Buffet S, et al. Incidence and prevalence of Neovascular Age-Related Macular Degeneration in France between 2008 and 2018: the LANDSCAPE study. Ophthalmol Sci. 2022;2:100114.
Ton Van C, Tran THC. Incidence of posterior capsular opacification requiring nd:YAG capsulotomy after cataract surgery and implantation of enVista® MX60 IOL. J Fr Ophtalmol. 2018;41:899–903.
Bourdiol Ducasse A-M, Guerzider V, Velasque L, Dominguez M, Lafuma A, Robert J. Comparison of clinical efficacy: nd:YAG laser rates after implantation of AcrySof® SN60WF, Akreos® AO-MI60 and Hoya® YA-60BB. J Fr Ophtalmol. 2013;36:575–82.
Miller VJ, Patnaik JL, Lynch AM, Taravella M, Palestine AG, Nagaraj RH. Risk factors predisposing to early nd:YAG Capsulotomy in a Colorado Cohort. Invest Ophthalmol Vis Sci. 2018;59:4797–7.
Caisse. Nationale d’Assurance Maladie. 2020_methode-reperage-pathologies_cartographie.pdf.
Bénard A, Sitta R, Brezin AP, Cochener B, Monnet D, Denis P, et al. Cost utility and value of information analysis of Femtosecond Laser-Assisted cataract surgery. JAMA Ophthalmol. 2023;141:625–9.
Monnet D. To better understand and delineate indications for the use of multifocal implants in cataract surgery: A French Multicentric Study. https://escrs.conference2web.com/?from_contentsession=840#!users/287691. Accessed 4 Aug 2023.
Lin X, Wang M, Zuo Y, Li M, Lin X, Zhu S, et al. Health literacy, computer skills and quality of patient-physician communication in chinese patients with cataract. PLoS ONE. 2014;9:e107615.
Eggermont RL, Witteman AM, van Erkelens JA, Vermeulen K, Vunderink L, Reus NJ. Nd:YAG laser capsulotomy rates in the Netherlands: practice variation and association with physician practice styles. J Cataract Refract Surg. 2023;49:373–7.
Acknowledgements
The authors thank Louis Chillotti (stève consultants) for his assistance in the development of this manuscript.
Funding
This study was granted by Alcon laboratories.
Author information
Authors and Affiliations
Contributions
All authors participated in the interpretation of the data, provided critical feedback and final approval for submission, and took responsibility for the accuracy, completeness, and protocol adherence of data and analyses. FB had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.Concept and design: all authorsAcquisition, analysis, or interpretation of data: all authorsDrafting of the manuscript: AB and CDCritical revision of the manuscript: AL, CS, FL, PRStatistical analysis: MG and FBAdministrative, technical, or material support: FB, CDSupervision: all authors.
Corresponding author
Ethics declarations
Competing interests
A Brézin is a consultant for Alcon; A Labbé is a consultant for Alcon, Allergan, Bausch & Lomb, Glaukos, Santen, Théa and Horus Pharma; C Schweiter has had advisory and honoraria for lecturing with Alcon, Allergan, Bausch & Lomb, Glaukos, Horus, Johnson & Johnson, Nicox, Théa; F Lignereux is consultant for Alcon and J&J; P Rozot is consultant for Alcon, Carl Zeiss Meditec, Horus Pharma, Hoya, Johnson & Johnson, Thea; M Goguillot and F Bugnard are employees of stève consultants, which has a research consultancy contract with Alcon; C Dot is consultant for Abbvie, Alcon, Bayer, Horus Pharma, Hoya, Novartis, Roche, Zeiss.
Ethics approval and consent to participate
Prior to data management, access to SNDS data was granted by the French national health data institute (Institut National des Données de Santé – INDS). This study has been granted scientific and ethical approval by the French expert committee for health research and evaluation (Comité d’Expertise pour les Recherches, les Études et les Évaluations dans le domaine de la Santé – CEREES), dossier n° 1119683 on December 19th, 2019. Also, this study received the authorization for claims data analyses from the French national data protection agency (Commission Nationale de l’Informatique et des Libertés – CNIL), dossier DR2020-096 on February 28th, 2020. This study was conducted in compliance with the French Data Protection Act and in accordance with applicable and with the ethical principles set out in the Declaration of Helsinki.
Granted ethical approval by the CEREES and data access authorization by CNIL (see ethical approval), no informed consent required as per Decree no. 2021 − 848 of June 29, 2021, of French Public Health Code. However, the patients have the right to be informed about ongoing studies and re-use of data and the opportunity to exercise their right to withdraw or object by contacting their local insurance service.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work was presented in part at the Oct 8–11, 2021 ESCRS meeting in Amsterdam.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Brézin, A.P., Labbe, A., Schweitzer, C. et al. Incidence of Nd:YAG laser capsulotomy following cataract surgery: a population-based nation-wide study – FreYAG1 study. BMC Ophthalmol 23, 417 (2023). https://doi.org/10.1186/s12886-023-03134-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-023-03134-6