Abstract
Purpose
To observe and understand the structural changes in choroidal vessels in eyes with hyperopic anisometropic amblyopia using swept-source optical coherence tomography angiography (SS-OCTA).
Methods
A total of 44 patients were enrolled in this study: 22 children with hyperopic anisometropic amblyopia and 22 age-matched controls. SS-OCTA was used to scan the 6*6 mm macular area of their eyes. The average choroidal thickness (CT) and choroidal capillary flow area (CC) in a 3 mm diameter area centered on the macular area were obtained. The choroidal vascularity volume (CVV) was automatically extracted and 3D reconstructed by inbuild software, and the three-dimensional choroidal vascularity index (3D-CVI) was calculated. The effect of amblyopia on the choroidal vessel structure was assessed using generalized linear estimating equations (GEEs) corrected for axial length, sex, age, and best-corrected visual acuity.
Results
The CC was greater in amblyopic eyes than in fellow eyes (P = 0.014) but was not significantly different from that in control eyes (P = 0.963). After correcting for sex, age, axial length, and visual acuity using GEEs, the mean CT in the amblyopic eyes was greater than that in the fellow eyes (P = 0.030) but was not significantly different from that in the control eyes (P = 0.160). The 3D-CVI in amblyopic eyes was higher than that in control eyes (P = 0.038) but was not significantly different from that in fellow eyes (P = 0.407). The three-dimensional choroidal vascularity volume (3D-CVV) was higher in amblyopic eyes than in fellow eyes (P = 0.046) and control eyes (P = 0.023).
Conclusions
We found that eyes with hyperopic anisometropic amblyopia demonstrated higher CT, CC and 3D-CVV values than the contralateral eyes after correction, while the 3D-CVI was unchanged. Compared with control eyes, amblyopic eyes had higher 3D-CVV and 3D-CVI values but similar CT and CC values. Amblyopic eyes may have different choroidal vascular structures from fellow and control eyes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Amblyopia is one of the leading causes of visual impairment in preschool children in China [1, 2], and untreated amblyopia can impact the academic lives of affected children [3]. According to previous studies, anisometropia is responsible for most cases of amblyopia [4]; this anisometropic amblyopia is caused by an abnormal interaction between the two eyes, resulting in amblyopia eyes having lower best-corrected visual acuities than the fellow eyes [5].
The amblyopic eye is usually considered free of ocular structural pathology. The normal structure and function of the choroid plays an important role in the nutrition and thermoregulation of the retina. In recent years, choroidal changes have been observed in a range of diseases, including amblyopia [6, 7]. Some studies have demonstrated thinner choroids in amblyopic eyes than in fellow and control eyes. However, studies investigating choroidal vascular structure changes have reached different conclusions [8, 9]. Furthermore, choroidal thickness and vascular structures are affected by a variety of factors, such as age, sex, axial length (AL), and refractive error [10,11,12,13]. AL and refractive error differences are common between amblyopic eyes and normal eyes, and ignoring these factors will affect the accuracy of the results. However, whether there are anatomical differences in the choroidal vascular structures between amblyopic and normal eyes remains to be understood.
With the development and widespread use of optical coherence tomography angiography (OCTA), it has become possible to understand the hierarchical structure of the retina and choroid in more detail. By using the variation in OCT signal caused by moving particles, such as red blood cells (RBCs), as the contrast mechanism for imaging blood flow, OCTA allows the visualization of functional blood vessels in the eye. In recent years, the use of swept-source OCTA (SS-OCTA) has become more beneficial for exploring deeper choroidal changes because of its faster scanning speed, clearer imaging quality, and greater scanning depth [14].
The choroidal vascularity index (CVI) is an OCT-based marker of choroidal vascularity that reflects the relationship between the choroidal vascular area and the total choroidal area. Previous studies have demonstrated differences in the CVI among patients with different refractive statuses [15], as well as amblyopia [16]. In previous studies, the CVI was typically obtained from a single B-scan image of the macula foveal region. Using one scan image covering the macula fovea to analyze changes in the CVI may not reveal the overall state of the choroidal vessels within a certain area. Choroidal vessel identification and 3D reconstruction can provide more information on the overall state of the choroid within a certain region and can provide a better understanding of the effect of disease on the choroidal vessels [13]. To our knowledge, there are no studies on the changes in 3D choroidal vessels between amblyopic and normal eyes.
In our research, we used SS-OCTA to scan the eyes of patients and age-matched normal controls and analyzed the differences in the mean choroidal thickness (CT), choroidal capillary flow area (CC), 3D-reconstructed choroidal vascular volume density (3D-CVI), and 3D-reconstructed choroidal vascular volume (3D-CVV) between amblyopic eyes, fellow eyes and control eyes. To assess and increase our understanding of the structural differences in the choroidal vasculature in the macula of hyperopic anisometropic amblyopia and clarify the effect of amblyopia on 3D choroidal vascular structure,
Methods
Demographic data
This was a retrospective study approved by the Peking University First Hospital Human Research Ethics Committee (2022Yan187). Data collection was performed in accordance with the Declaration of Helsinki.
The data were collected consecutively from February 2022 to June 2022. Children aged 4 to 12 years who attended the pediatric ophthalmology department of Peking University First Hospital and underwent OCTA examination to screen for hyperopic anisometropic amblyopia were initially included as the amblyopia group. The criteria for diagnosing hyperopic anisometropic amblyopia were determined according to the American Academy of Ophthalmology guidelines [17]. The inclusion criteria were as follows: 1, an equivalent spherical (SE) diopter (D) difference between both eyes > 1 D; 2, hyperopia in both eyes; and 3, two-line difference in best-corrected visual acuity (BCVA) between both eyes, with the more hyperopic eye having worse visual acuity. The exclusion criteria were as follows: 1, the presence of retinal or choroidal disease; 2, treatment with instruments that could potentially affect the retinal choroid; 3, esotropia or constant exotropia or vertical strabismus; 4, glaucoma; 5, previous internal eye surgery; 6, obstruction in the visual axis; 7, systematic disease; and 8, inability to cooperate with the examination for any reason.
We collected data from age-matched patients with mild hyperopia (< + 1.50 D), orthopia or mild myopia (> -0.50 D) who had no amblyopia and no ocular or systemic disease as the control group. All participants’ cycloplegia refraction, axial length, and BCVA values were also collected.
Image acquisition
SS-OCTA (VG100; SVision Imaging, Ltd., Luoyang, China) was used to scan the macular area of the eyes of the participants. The scan was centered at a wavelength of approximately 1050 nm and performed at a rate of 100,000 A-scans per second. The maximum axial and estimated lateral resolutions in the tissue were approximately 5 μm and 15 μm, respectively, and the scanning depth was 3 mm. Choroidal vascular distribution and CT data were obtained by a raster scanning protocol with 1024 × 1024 B scans covering a 6 mm × 6 mm area centered on the central macular fovea. Eye-movement artifacts during and between scans were minimized by using the built-in eye-tracking mode of the device based on the integrated confocal scanning laser detector lens.
Quantitative analysis was performed using a 6 mm × 6 mm OCTA scan (Fig. 1). When performing the examination, the software automatically scores the quality of the scan (1–10, with 10 being the highest score), and if the score for that scan is below 7, the scan will be performed again for the child. The scan with the highest quality was selected for analysis. Choroidal parameters were analyzed using built-in software (V 1.36.10), and all subjects' axial lengths were entered for image magnification correction. The software automatically performs layer segmentation and quantitative analysis [18] (Fig. 2). Data were reviewed by the researcher before extraction, and if there were errors in the stratification, manual changes were made to the segmentation to ensure accuracy. To avoid incomplete areas due to the magnification effect caused by hyperopia and the effect of retinal macrovascular occlusion, a circular area with a diameter of 3 mm centered on the central macular fovea was selected for analysis. To avoid interference of the circadian rhythm on the choroid, all subjects were examined from 9:00 am to 12:00 pm.
Definition of the choroid and choroidal capillaries. The inbuild software automatically performs layer segmentation. a. Choroid: the region spanning from the outer border of the retinal pigment epithelium-Bruch's membrane complex to the choroid-sclera junction. b. Choroidal capillaries: the area 10 μm above Bruch's membrane to 25 μm below it
The choroid was defined as the area from the outer border of the retinal pigment epithelium-Bruch's membrane complex to the choroid-sclera junction, and the thickness was recorded as the average choroidal thickness in this area (Fig. 2). The software automatically extracted the image of the scanned choroidal region and calculated the average choroidal thickness in that region.
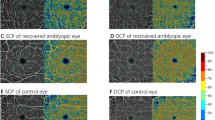
The choroidal capillaries were defined as those in the area 10 μm above Bruch's membrane to 25 μm below it. The inbuild software also automatically identifies this region, acquires the en face image (Fig. 2), selects the choroidal capillaries using the software's threshold function and automatically calculates the flow area (Fig. 3).
The images of large and medium vessels were also automatically extracted by the software (Fig. 4), and 3D reconstruction was performed to calculate the choroidal large and medium vessel volume (3D-CVV). The 3D-CVI was defined as the ratio of the choroidal vessel volume to the total choroidal volume (TCV), which reflects the choroidal vascular volume in the Sattler.
Statistical analyses
SPSS (version 26.0; IBM Corp., Armonk, NY, USA) was used for all statistical analyses. A chi-square test was used to compare the sex ratio between the two groups. The Kolmogorov–Smirnov test was used for normality testing. Normally distributed variables are expressed as the mean and standard deviation (mean ± SD), and nonnormally distributed variables are expressed as the median and interquartile range (IQR). The means of normally distributed quantitative variables were compared using a t test. For nonnormally distributed data, the Mann–Whitney U test was used for testing. The two eyes in the amblyopic group were compared using the paired test, and amblyopic eyes were compared with control eyes using the between-group test. Multivariable generalized estimating equation (GEE) models were used to adjust for the potential effects of axial length, sex and age on CT, 3D-CVI and 3D-CVV. P < 0.05 was considered to indicate statistical significance.
Results
Demographic data
A total of 44 children were included in this study, 22 with hyperopic anisometropic amblyopia and 22 in the control group. The clinical characteristics of each group are presented in Table 1. There were no significant differences between the amblyopic and normal control groups in terms of age or sex ratio. The mean axial length was 21.56 ± 1.06 mm, 22.26 ± 1.15 mm, and 22.96 ± 1.03 mm in the amblyopic, fellow, and control eyes, respectively, and the differences among them were significant (P < 0.001). The mean SE was + 5.09 ± 2.01 D, + 3.05 ± 1.98 D and + 0.25 ± 0.68 D in amblyopic, fellow and control eyes, respectively (P < 0.001). The mean logMAR BCVA was 0.343 ± 0.255, 0.104 ± 0.114 and 0.0029 ± 0.531 in the amblyopic, fellow and control eyes, respectively, and the differences among the groups were significant (P < 0.001).
Choroidal capillary flow area (CC)
The CC did not conform to a normal distribution (P = 0.032, P = 0.003, and P = 0.015 for amblyopic, fellow and control eyes, respectively). The median CC was 6.69 (0.103), 6.67 (0.167) mm2 and 6.72 (0.197) mm2 in the amblyopic, fellow, and control eyes, respectively. The CC was significantly higher in amblyopic eyes than in fellow eyes (P = 0.014), but there was no significant difference between amblyopic and control eyes (P = 0.963).
Choroidal thickness (CT)
The CT conformed to a normal distribution (P = 0.200). Within a 3 mm-diameter circle centered on the macular fovea, the mean CT was 388.6 ± 40.9 μm in the amblyopic eyes, 352.4 ± 56.6 μm in the fellow eyes, and 338.2 ± 70.2 μm in the control eyes (Table 2). The CT was significantly greater in amblyopic eyes than in fellow and control eyes (P < 0.001 and P = 0.006, respectively). After GEE analysis, the CT in the amblyopic eyes was significantly higher than that in the fellow eyes (P = 0.030) but was not significantly different from that in the control eyes (P = 0.160) (Table 3). There was a significant effect of axial length on CT; an increase in the AL was associated with an increase in the CT (P = 0.002). Age, sex, and BCVA had no effect on CT (Table 3).
3D-CVI and 3D-CVV
In the examination of the choroidal vasculature, the 3D-CVI and 3D-CVV conformed to a normal distribution (P = 0.200). The mean 3D-CVI was 0.400 ± 0.064 in the amblyopic eyes, 0.385 ± 0.048 in the fellow eyes, and 0.352 ± 0.087 in the control eyes; only the amblyopic and control eyes demonstrated a significant difference (P = 0.042; amblyopic vs. fellow eyes, P = 0.234). The 3D-CVV in amblyopic eyes was significantly higher than that in fellow eyes (P = 0.003) and control eyes (P = 0.027) (Table 2).
GEEs were used to adjust for the effects of axial length, age, sex, and BCVA on the 3D-CVI and 3D-CVV. The 3D-CVI in amblyopic eyes was significantly higher than that in control eyes (P = 0.038) but was not significantly different from that in fellow eyes (P = 0.407) (Table 4). There was no effect of axial length, age, sex, or BCVA on the 3D-CVI. Regarding 3D-CVV, amblyopic eyes had significantly higher values than fellow and control eyes (P = 0.023 and P = 0.046, respectively) (Table 5). There was no effect of axial length, age, sex, or BCVA on 3D-CVV (Table 5).
Discussion
The normal structure and function of the choroid plays an important role in the nutrition and thermoregulation of the retina. In recent years, there has been increasing focus on the role played by the choroid in various ophthalmic diseases [19, 20]. To clarify the effect of amblyopia on choroidal vascular structure, we conducted this study. We found that the choroidal capillary flow area was greater in amblyopic eyes than in fellow eyes but was not significantly different from that in control eyes. After correcting for age, sex, axial length, and BCVA using GEEs, the CT and 3D-CCV were greater in the amblyopic eyes than in the fellow eyes, while no significant differences were observed in the 3D-CVI. Amblyopia causes a thickening of the choroid and an increase in the flow area of choroidal capillaries and of large and medium vessels. Compared with the control eyes, amblyopic eyes had increased 3D-CVI and 3D-CVV but no significant differences in CT. Axial length remained the main causative effect of the changes relative to the control eyes, but the effect in amblyopia was not significant.
Changes in the choroidal structure of amblyopic eyes have been reported in numerous studies. A previous meta-analysis by Liu [21] yielded similar results to our study, with greater CT values observed in anisometropic amblyopic eyes than in fellow and control eyes, regardless of whether the axial length was matched. Some studies have reported thinner choroidal thickness in children with high myopic amblyopic eyes compared with high myopic eyes [22, 23]. Most of the subjects selected in previous studies were hyperopic or strabismic amblyopic children, suggesting that there are differences in choroidal structure changes in amblyopic eyes with different refractive types and that choroidal changes in amblyopic eyes may be due to a combination of amblyopia and refraction.
The study by Huang et al. [24] showed that the choroidal capillary flow area was higher in amblyopic eyes than in both fellow eyes and control eyes, similar to our findings. Terada’s [8] study found an increase in vascular perfusion area in amblyopic eyes compared to control eyes, which was also similar to the findings in our study. In recent years, an increasing number of studies have focused on refractive states and choroidal changes. Some studies have suggested that the choroid plays an important role in the process of emmetropization in children [25]. The choroid can adjust the position of the retina both by adjusting its thickness to the refractive state (choroidal modulation) and by releasing cytokines that regulate extracellular matrix remodeling in the sclera. In a study of patients with refractive parametric amblyopia treated with one year of refractive correction and/or masking, a decrease in the vascular component and an increase in the stromal component of the choroid in amblyopic eyes were observed after treatment, whereas no significant changes were observed in nonamblyopic eyes [26], suggesting that the effect of amblyopia on the choroid is associated with a delay in emmetropization.
Some studies have obtained different findings regarding the CVI. In the study by Baek et al. [27], which showed increased CVV in amblyopic eyes, the CVI was found to be higher in amblyopic eyes than in fellow eyes but was negatively correlated with CT, suggesting a relative decrease in choroidal vascularity and insufficient blood supply in amblyopic eyes. A similar conclusion was reached by Furundaoturan et al. [28], who found a decrease in the CVI and an increase in the stroma in patients with anisometropia amblyopia. The study by Cevher et al. [29] found a lower CVI in hyperopic anisometropia amblyopia eyes than in fellow and control eyes, suggesting that hyperopia affects choroidal structure. These studies, however, did not correct for the axial length and analyzed only a single layer of horizontal scans through the central macular sulcus that included only the blood vessels in a 750 μm or 1000 μm region. The differences in the image range of the scanning protocol could be the source of inconsistency between the conclusions drawn by that study and the present one.
In our study, before correction, the CT was higher in amblyopic eyes than in fellow and control eyes. After correction for axial length, age, sex and BCVA using the GEEs, the CT of the amblyopic eyes differed only from that of the fellow eyes and was not significantly different from that of the control eyes. Additionally, axial length significantly affected choroidal thickness (P = 0.002). Several previous studies have demonstrated [10, 11] that axial length has an effect on the choroid; specifically, there is a negative correlation between axial length and CT, with shorter axial lengths associated with thicker choroids. Therefore, it is necessary to correct the axial length in choroid-related studies to account for eyes with differences in axial length.
No relationship was identified between age and the choroidal vascular structure in our study. Some previous studies have shown that age also affects the choroid; a study by Xiong et al. [12], for example, showed that the CT in orthopic and mildly myopic children aged 6–19 years progressively decreased with age. Other studies have yielded different results, such as Read et al. [10], who showed a gradual thickening of the choroid with age during childhood. The CT is greater in children aged 10 to 12 years than in children aged 7–9 years and children aged 4–6 years. Zhou et al. [13] showed that CT, CVV, and choroidal stroma volume (CSV) all decreased with age in the macular subfovea region; however, the CVI was not affected by aging. In our study, no effect of age was found on the choroid because the patients were younger and had a relatively small age distribution.
The choroidal differences in amblyopia found in this study were mainly reflected with respect to the fellow eyes and not to the control eyes. Most likely due to the comparative study of both eyes from the same subjects, we were better able to control for the effects of age, sex, genetic and environmental factors. Vincent’s [30] study found that in refractive reference patients, differences in ocular biological parameters mainly originated in the posterior segment of the eye, such as vitreous cavity depth (VCD), axial length (AL), and CT. Patients showed similar characteristics in other ocular biometric parameters in both eyes, such as corneal curvature, anterior chamber depth (ACD), and crystalline lens power. Therefore, studies in patients with monocular amblyopia can better control for other unknown confounding factors and obtain relatively reliable conclusions.
There are limitations in our study. It is well-known that hyperopia affects the choroidal vascular structure. For instance, hyperopia causes thick choroids [16, 31]. To eliminate the effects of hyperopia on the choroid, it would be ideal to compare children with similar hyperopia grades (along with age- and sex-matched controls but with normal corrected visual acuity), but the mean refraction of the amblyopic eyes in our study was + 5.09 ± 2.01, and children with similar refraction but without amblyopia were difficult to find, so an ideal control group could not be found. To minimize the interference of refraction between different groups, the GEE equation was used in our study to correct for the effect of axial length age and sex on choroidal vascular parameters. The expectation is that the resulting results would yield the true effect of amblyopia on the choroid as much as possible.
The sample size of this study is small. This study included patients in different stages of treatment, which may have partially influenced the results. Some studies have shown that treatment in amblyopic eyes increases BCVA, decreases CVI, and increases stromal volume [26]. Further longitudinal studies are needed to clarify the effect of treatment on the choroid. Due to the need to conduct an SS-OCTA examination, only patients who could cooperate with the examination for acquiring high-quality images were included in this study. Some younger patients and those with poor visual acuity were excluded, which may have led to some degree of bias in the results. Therefore, future studies with larger populations and follow-up are needed to clarify the effects of amblyopia in the choroid.
In conclusion, in amblyopic eyes, the choroid was thicker and the capillary flow area and vascular volume were greater than those of normal eyes, which may be related to a delay in emmetropization. Future studies on amblyopia should focus on the mechanism underlying the causes of choroid changes in amblyopia. In the future, choroidal vascular changes may be used as a potential indicator for predicting and treating amblyopia.
Availability of data and materials
The data that support the findings of this study are available on reasonable request from the corresponding author [Liu Yang and Dehai Zhu]. The raw data are not publicly available due to [state restrictions, them containing information that could compromise research participant privacy/consent].
References
Pan CW, Chen X, Gong Y, Yu J, Ding H, Bai J, Chen J, Zhu H, Fu Z, Liu H. Prevalence and causes of reduced visual acuity among children aged three to six years in a metropolis in China. Ophthalmic Physiol Opt. 2016;36(2):152–7. https://doi.org/10.1111/opo.12249. (Epub 2015 Oct 2 PMID: 26432417).
Zhang X, Li R, Wang Y, Zhao X, Hao Q, Tong H, Chen P, Yu Y, Liu H. Prevalence, causes and risk factors of reduced VA and persistent reduced VA among preschool children in Eastern China. Ophthalmic Physiol Opt. 2020;40(4):452–62. https://doi.org/10.1111/opo.12692. (Epub 2020 May 28 PMID: 32462748).
Chua B, Mitchell P. Consequences of amblyopia on education, occupation, and long-term vision loss. Br J Ophthalmol. 2004;88(9):1119–21. https://doi.org/10.1136/bjo.2004.041863. (PMID:15317699;PMCID:PMC1772316).
Wang Y, Liang YB, Sun LP, Duan XR, Yuan RZ, Wong TY, Yi P, Friedman DS, Wang NL, Wang JJ. Prevalence and causes of amblyopia in a rural adult population of Chinese the Handan Eye Study. Ophthalmology. 2011;118(2):279–83. https://doi.org/10.1016/j.ophtha.2010.05.026. (Epub 2010 Sep 24 PMID: 20869774).
von Noorden GK. Amblyopia: a multidisciplinary approach. Proctor lecture Invest Ophthalmol Vis Sci. 1985;26(12):1704–16 (PMID: 3934105).
Borrelli E, Lonngi M, Balasubramanian S, Tepelus TC, Baghdasaryan E, Pineles SL, Velez FG, Sarraf D, Sadda SR, Tsui I. Increased choriocapillaris vessel density in amblyopic children: a case-control study. J AAPOS. 2018;22(5):366–70. https://doi.org/10.1016/j.jaapos.2018.04.005. (Epub 2018 Aug 2 PMID: 30009947).
Masri OS, Abiad B, Darwich MJ, Sarkis PA, El Mollayess GM, Nasser Z, Fares Y, Al Ahmar E, Estephan E. Morphological changes in amblyopic eyes in choriocapillaris and Sattler's layer in comparison to healthy eyes, and in retinal nerve fiber layer in comparison to fellow eyes through quantification of mean reflectivity: A pilot study. PLoS One. 2021;16(8):e0255735. https://doi.org/10.1371/journal.pone.0255735. PMID: 34358257; PMCID: PMC8345865.
Terada N, Miyata M, Muraoka Y, Hata M, Fujimoto M, Yokota S, Nakanishi H, Suda K, Yoshikawa M, Ooto S, Ohtsuki H, Tsujikawa A. Abnormal Outer Choroidal Vasculature in Amblyopia. J Ophthalmol. 2019;2019:2097087. https://doi.org/10.1155/2019/2097087. (PMID:30733871;PMCID:PMC6348855).
Araki S, Miki A, Goto K, Yamashita T, Yoneda T, Fujiwara A, Haruishi K, Ieki Y, Kiryu J, Maehara G, Yaoeda K. Choroidal vessel density in unilateral hyperopic amblyopia using en-face optical coherence tomography. BMC Ophthalmol. 2020;20(1):472. https://doi.org/10.1186/s12886-020-01735-z. (PMID:33267849;PMCID:PMC7709249).
Read SA, Collins MJ, Vincent SJ, Alonso-Caneiro D. Choroidal thickness in childhood. Invest Ophthalmol Vis Sci. 2013;54(5):3586–93. https://doi.org/10.1167/iovs.13-11732. (PMID: 23652485).
Qian Y, Ma Y, Lin Q, Xiang Z, Qiang J, Xu Y, Zou H. Retinal and Choroidal Changes in Children with Moderate-to-High Hyperopia. J Ophthalmol. 2021;2021:9971564. https://doi.org/10.1155/2021/9971564. (PMID:34646578;PMCID:PMC8505083).
Xiong S, He X, Deng J, et al. Choroidal Thickness in 3001 Chinese Children Aged 6 to 19 Years Using Swept-Source OCT. Sci Rep. 2017;7:45059.
Zhou H, Dai Y, Shi Y, Russell JF, Lyu C, Noorikolouri J, Feuer WJ, Chu Z, Zhang Q, de Sisternes L, Durbin MK, Gregori G, Rosenfeld PJ, Wang RK. Age-Related Changes in Choroidal Thickness and the Volume of Vessels and Stroma Using Swept-Source OCT and Fully Automated Algorithms. Ophthalmol Retina. 2020;4(2):204–215. https://doi.org/10.1016/j.oret.2019.09.012. Epub 2019 Oct 1. PMID: 32033714; PMCID: PMC7812781.
Copete S, Flores-Moreno I, Montero JA, Duker JS, Ruiz-Moreno JM. Direct comparison of spectral-domain and swept-source OCT in the measurement of choroidal thickness in normal eyes. Br J Ophthalmol. 2014;98(3):334–8. https://doi.org/10.1136/bjophthalmol-2013-303904. (Epub 2013 Nov 28 PMID: 24288394).
Cevher S, Üçer MB, Şahin T. How does anisometropia affect the choroidal vascularity index? Indian J Ophthalmol. 2022;70(6):2043–9. https://doi.org/10.4103/ijo.IJO_3092_21. (PMID:35647979;PMCID:PMC9359273).
Kaderli A, Acar MA, Ünlü N, Üney GÖ, Örnek F. The correlation of hyperopia and choroidal thickness, vessel diameter and area. Int Ophthalmol. 2018;38(2):645–53. https://doi.org/10.1007/s10792-017-0509-3. (Epub 2017 Apr 4 PMID: 28378149).
Wallace DK, Morse CL, Melia M, Sprunger DT, Repka MX, Lee KA, Christiansen SP; American Academy of Ophthalmology Preferred Practice Pattern Pediatric Ophthalmology/Strabismus Panel. Pediatric Eye Evaluations Preferred Practice Pattern®: I. Vision Screening in the Primary Care and Community Setting; II. Comprehensive Ophthalmic Examination. Ophthalmology. 2018;125(1):P184-P227. https://doi.org/10.1016/j.ophtha.2017.09.032. Epub 2017 Nov 4. PMID: 29108745.
Chen L, Yuan M, Sun L, Chen Y. Three-Dimensional Analysis of Choroidal Vessels in the Eyes of Patients With Unilateral BRVO. Front Med (Lausanne). 2022;9:854184. https://doi.org/10.3389/fmed.2022.854184. PMID: 35479961; PMCID: PMC9037087.
Cicinelli MV, Rabiolo A, Marchese A, de Vitis L, Carnevali A, Querques L, Bandello F, Querques G. Choroid morphometric analysis in nonneovascular age-related macular degeneration by means of optical coherence tomography angiography. Br J Ophthalmol. 2017;101(9):1193–200. https://doi.org/10.1136/bjophthalmol-2016-309481. (Epub 2017 Jan 5 PMID: 28057649).
Maruko I, Iida T, Sugano Y, Ojima A, Ogasawara M, Spaide RF. Subfoveal choroidal thickness after treatment of central serous chorioretinopathy. Ophthalmology. 2010;117(9):1792–9. https://doi.org/10.1016/j.ophtha.2010.01.023. (Epub 2010 May 15 PMID: 20472289).
Liu Y, Dong Y, Zhao K. A Meta-Analysis of Choroidal Thickness Changes in Unilateral Amblyopia. J Ophthalmol. 2017;2017:2915261. https://doi.org/10.1155/2017/2915261. Epub 2017 Jun 19. PMID: 28751980; PMCID: PMC5494565.
Shi T, Zhang W, Chen S, Xia H, Chen H. Reduced Photoreceptor Outer Segment Layer Thickness and Association with Vision in Amblyopic Children and Adolescents with Unilateral High Myopia. Curr Eye Res. 2021;46(12):1892–9. https://doi.org/10.1080/02713683.2021.1942072. (Epub 2021 Jul 20 PMID: 34112034).
Wan J, Zhang Z, Tian Y. Examination of Macular Retina and Choroidal Thickness in High Myopic Amblyopia Using Spectral-Domain Optical Coherence Tomography. Front Med (Lausanne). 2022;9:808409. https://doi.org/10.3389/fmed.2022.808409. PMID: 35419378; PMCID: PMC8996077.
Huang L, Ding L, Zheng W. Microvascular assessment of macula, choroid, and optic disk in children with unilateral amblyopia using OCT angiography. Int Ophthalmol. 2022;42(12):3923–31. https://doi.org/10.1007/s10792-022-02376-5. (Epub 2022 Jul 6 PMID: 35790661).
Summers JA. The choroid as a sclera growth regulator. Exp Eye Res. 2013;114:120–7. https://doi.org/10.1016/j.exer.2013.03.008. Epub 2013 Mar 23. PMID: 23528534; PMCID: PMC3724760.
Nishi T, Ueda T, Mizusawa Y, Semba K, Shinomiya K, Mitamura Y, Sonoda S, Uchino E, Sakamoto T, Ogata N. Effect of optical correction on choroidal structure in children with anisohypermetropic amblyopia. PLoS One. 2020;15(4):e0231903. https://doi.org/10.1371/journal.pone.0231903. PMID: 32324782; PMCID: PMC7179822.
Baek J, Lee A, Chu M, Kang NY. Analysis of Choroidal Vascularity in Children with Unilateral Hyperopic Amblyopia. Sci Rep. 2019;9(1):12143. https://doi.org/10.1038/s41598-019-48613-3.PMID:31434959;PMCID:PMC6704087.
Furundaoturan O, Değirmenci C, Akkın C, Demirkılınç Biler E, Üretmen Ö, Nalçacı S, Afrashi F. Evaluation of Choroidal Vascular Index in Amblyopic Patients. Turk J Ophthalmol. 2022;52(3):168–73. https://doi.org/10.4274/tjo.galenos.2021.48275. (PMID:35769903;PMCID:PMC9249111).
Guler Alis M, Alis A. Choroidal vascularity index in adults with different refractive status. Photodiagnosis Photodyn Ther. 2021;36:102533. https://doi.org/10.1016/j.pdpdt.2021.102533. Epub 2021 Sep 11. PMID: 34520880.
Vincent SJ, Collins MJ, Read SA, Carney LG. Retinal and choroidal thickness in myopic anisometropia. Invest Ophthalmol Vis Sci. 2013;54(4):2445–56. https://doi.org/10.1167/iovs.12-11434. (PMID: 23482471).
Lee GY, Yu S, Kang HG, Kim JS, Lee KW, Lee JH. Choroidal Thickness Variation According to Refractive Error Measured by Spectral Domain-optical Coherence Tomography in Korean Children. Korean J Ophthalmol. 2017;31(2):151–8. https://doi.org/10.3341/kjo.2017.31.2.151.
Acknowledgements
Not applicable.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
Yiwen Cao, Dehai zhu and Liu Yang designed and conducted the experiment. Yiwen Cao, Dehai Zhu, Liu Yang provided materials. Yiwen Cao, Xiaopeng Gu and Yadi Zhang collected the data. Yiwen Cao analyzed the data. Yiwen Cao, Dehai zhu and Liu Yang wrote and drafted the article. Yiwen Cao, Dehai zhu and Liu Yang reviewed the manuscript. Both Liu Yang and Dehai Zhu are co-corresponding authors of this article.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This was a retrospective study approved by Peking University First Hospital Human Research Ethics Committee (NO. 2022Yan187). The data collection procedure complied with the Declaration of Helsinki. Informed consent was exemption with the approval of Peking University First Hospital Human Research Ethics Committee.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cao, Y., Zhang, Y., Gu, X. et al. Choroid vascular changes in hyperopic anisometropia amblyopia using SS-OCTA. BMC Ophthalmol 23, 379 (2023). https://doi.org/10.1186/s12886-023-03121-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-023-03121-x