Abstract
Background
Information regarding incidence of treatment plan changes may be useful when discussing postoperative treatment plans for patients. Moreover, it may help establish a standardized postoperative treatment plan. This study aimed to evaluate the incidence of early complications requiring treatment plan changes in patients following vitreoretinal surgery and investigate its risk factors.
Methods
This single-center retrospective study included 465 patients who had undergone vitreoretinal surgery. The reasons, incidence, and timing of treatment plan changes within 14 days of surgery were identified. Potential factors associated with the changes, such as patient demographics, surgeon’s experience, diagnoses, and type of surgery were also analyzed.
Results
The treatment plan was changed in 76 patients (16.3%) at a mean of 4.0 ± 3.2 days after vitreoretinal surgery. The reasons for the plan changes were increased intraocular pressure (IIOP) in 66(86.8%), intraocular inflammation in 2(2.6%), corneal edema in 3(3.9%), leakage from the sclerotomy wound in 3(3.9%) patients, and combined IIOP and intraocular inflammation in 2(2.6%). The date of discharge was postponed because of treatment plan changes in 17 patients (22.4%). The incidence of plan changes was higher in patients who underwent gas or oil tamponade (P < 0.001) and those who underwent surgery performed by less experienced surgeons (P = 0.034).
Conclusions
Treatment plan was changed in 16.3% of patients after vitreoretinal surgery. The risk of treatment plan changes was associated with the surgeon’s experience in vitreoretinal surgery and the type of surgery. These results should be considered when establishing standardized care plans for patients who require vitreoretinal surgery.
Similar content being viewed by others
Intruduction
Modern vitreoretinal surgery is safe and effective in treating various retinal disorders, including rhegmatogenous retinal detachment (RRD), [1] complications of diabetic retinopathy, [2] macular hole (MH), [3] and epiretinal membrane (ERM) [4]. However, since vitreoretinal surgery is invasive, postoperative complications, such as increased (2.5–61.5%) or decreased (1.8–13.1%) intraocular pressure (IOP), [5,6,7,8,9,10] corneal edema (0.80–1.1%) [7, 11], intraocular inflammation (0.25–26%) [5, 12], or retinal detachments (1.2–1.7%) may occur in patients [11]. Therefore, the postoperative care plan for patients may be changed according to the type and severity of these complications [12].
The incidence of postoperative complications varies substantially among patients who undergo different surgical procedures [13]. Accordingly, the incidence of changes in treatment plans may also differ. Information regarding these changes may be useful when discussing postoperative treatment plans for patients. In addition, it may help establish a standardized postoperative care system [14]. To date, there is limited knowledge regarding this topic.
Herein, we investigated the incidence of early complications requiring changes in the treatment plan in patients who had undergone vitreoretinal surgery. Additionally, the factors associated with the risk of plan changes were evaluated.
Methods
This retrospective study was conducted at a single center (Kim’s Eye Hospital, Seoul, South Korea, #2022-05-009). The study was approved by the Institutional Review Board of Kim’s Eye Hospital and conducted in accordance with the tenets of the Declaration of Helsinki. The need for informed consent was waived by the Institutional Review Board (Kim’s Eye Hospital IRB).
Patients
We secured a list of patients who underwent vitrectomy with or without gas or silicone oil tamponade, scleral buckling, scleral encircling, or scleral fixation of intraocular lens (IOL) at our institution between January 2021 and December 2021. Patients with the following diagnoses were included: RRD, ERM, MH, DR, vitreous hemorrhage (VH) other than DR, IOL dislocation, or lens dislocation. All vitrectomies were performed with transconjunctival sutureless vitrectomy technique using 23-gauge or 25-gauge device.
Outcome measures
Patients who experienced changes in the treatment plan within 14 days after surgery due to postoperative complications were identified. The timing, reasons, and details of these changes were also identified. The incidence of the changes in treatment plan was compared among the following categories: (1) age; (2) sex; (3) diabetes mellitus; (4) hypertension; (5) surgeon’s experience in vitreoretinal surgery (≥ 6 vs. < 6 years); (6) diagnosis: RRD vs. ERM vs. MH vs. DR vs. VH other than DR vs. IOL dislocation or lens dislocation; (7) type of surgery: vitrectomy without tamponade vs. vitrectomy with tamponade vs. scleral buckling or encircling only vs. scleral fixation; and (8) combined cataract surgery. When there was more than one episode of plan change, only the first episode of plan change was included in this study.
Statistical analysis
Data are presented as the mean ± standard deviation or number (%), where applicable. Statistical analyses were performed using the IBM SPSS Statistics for Windows (version 21.0; IBM Corp., Armonk, NY, USA). The visual acuities were represented as logarithm of the minimum angle of resolution (logMAR) values. The visual acuities for counting finger and hand motion were converted to logMAR values of 2 and 3, respectively. Between patients with and without treatment plan changes, the age was compared using the independent samples t-test. Diabetes mellitus, hypertension, history of vitreoretinal surgery, surgeon’s experience in vitreoretinal surgery, diagnosis, type of surgery, and combined cataract surgery were compared between the two groups using the chi-square test. The incidence of complications among patients requiring treatment plan changes according to the type of surgery and the timing at which the complications occurred was analyzed using the chi-square or Fisher’s exact test. Statistical significance was set at P < 0.05.
Results
Demographics
A total of 465 patients were included in the study (Table 1). Two hundred and seventy-three patients were men (58.7%) and 192 were women (41.3%). Their mean age was 58.20 ± 13.52 years; 15 (3.2%) of them had a history of vitreoretinal surgery, 133 (28.6%) had diabetes mellitus, and 205 (44.1%) had hypertension. The logMAR preoperative best-corrected visual acuity was 0.98 ± 1.01 and the mean axial length was 24.42 ± 1.80 mm.
The diagnosis was ERM in 86 patients (18.5%), diabetic retinopathy in 76 patients (16.3%), MH in 53 patients (11.4%), RRD in 158 patients (34.0%), VH other than DR in 26 patients (5.6%), and IOL dislocation or lens dislocation in 66 patients (14.2%). One hundred seventy-four patients underwent vitrectomy without tamponade, 184 underwent vitrectomy with tamponade using either gas (n = 156) or silicone oil (n = 28), 62 underwent vitrectomy with IOL scleral fixation, and 45 underwent scleral buckling or encircling only. Fifteen surgeons performed the surgery. Three hundred thirty-four cases (71.8%) were operated on by surgeons with ≥ 6 years of experience in vitreoretinal surgery. Surgeons with < 6 years of experience performed the procedure in the remaining 131 cases (28.2%).
Treatment plan changes
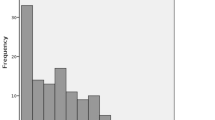
Among the 465 patients, the treatment plan was changed within 14 days after surgery in 76 patients (16.3%). The mean period between the surgery and plan changes was 4.0 ± 3.2 days (Fig. 1). The plan was changed 1 day after the surgery in 33 patients (43.4%), between 2 and 7 days in 29 patients (38.1%), and between 8 and 14 days in 14 patients (18.4%). The reasons for the plan changes were increased intraocular pressure in 66 (86.8%), intraocular inflammation in 2 (2.6%), corneal edema in 3 (3.9%), leakage from the sclerotomy wound in 3 (3.9%) patients, and combined increased intraocular pressure and intraocular inflammation in 2 (2.6%). Table 2 summarizes the reasons for the plan changes according to the type of surgery.
The specific contents of the treatment plan changes were as follows: changes in the frequency of administration of topical drugs only = 4, adding another topical drug = 66, changes in the usage of systemic drugs with or without changes in the usage of topical drugs = 10, and performing invasive procedures, such anterior chamber tapping or intravitreal injection = 5 with or without changes in drug therapy. All four intraocular inflammation cases were well-controlled after changes in the frequency of administration of topical drugs or the addition of other topical drugs. None of the patients had infectious endophthalmitis. Table 3 summarizes the timing of the treatment plan changes according to the reasons. Among the 76 patients, the date of discharge was postponed owing to treatment plan changes in 17 patients (21.8%). The reason was an increase in IOP in 13 patients, intraocular inflammation in 1, hypotony in 1, and combined increased intraocular pressure and intraocular inflammation in 2.
Factors associated with treatment plan changes
Table 4 summarizes the results of comparisons between patients with and without changes in the treatment plan. A history of vitreoretinal surgery (P = 0.001), surgeon’s experience in vitreoretinal surgery (P = 0.034), diagnosis (P < 0.001), and type of surgery (P < 0.001) were associated with different incidences of plan changes. More specifically, the incidence was relatively higher in patients with a history of vitreoretinal surgery (46.7%), those operated on by surgeons with < 6 years of experience in vitreoretinal surgery (22.1%), those diagnosed with RRD (23.4%) or MH (26.4%), and those who underwent vitrectomy with tamponade (30.4%).
Discussion
In the present study, changes in the treatment plan after vitreoretinal surgery were noted in 16.3% of patients at a mean of 4.0 days after surgery. The most prevalent reason was an increase in IOP, followed by intraocular inflammation, hypotony due to leakage from the sclerotomy wound, and corneal edema. In most patients, the events causing plan changes were well-controlled with the modulation of topical or systemic drug administration.
Increase in IOP is a frequently noted phenomenon after vitreoretinal surgery [15]. Various mechanisms, including gas expansion, anterior chamber inflammation, and iris-lens diaphragm shifting, are suspected causes of acute increase in IOP [15]. In the present study, increase in IOP was the primary reason of treatment plan changes. This was most frequently observed after vitrectomy with tamponade. Similar to previous studies, [8, 16] most increases in IOP were noted within one week after the surgery. Although most cases were well-controlled after administration of IOP-lowering agents, an increase in IOP was the most prevalent reason for prolonged hospitalization. Patients in whom tamponade is planned should be informed that the treatment plan can be changed because of a postoperative increase in IOP.
Sutureless vitrectomy has revolutionized vitreoretinal surgery. Compared to previous technique, it provided more convenient surgery with shortening of operating time and minimizing surgically induced trauma [17]. However, one limitation of this technique is that tight wound apposition is sometimes not made [18]. Therefore, leakage of vitreous fluid from unclosed wound lead postoperative IOP decrease [18]. In some instances, additional procedures, such as sclerotomy sutures, were necessary to control the leakage [12]. In the present study, hypotony was noted in 3 of the patients who underwent vitrectomy and leakage from sclerotomy wound was noted in one of them. Although the incidence was low, discharge was postponed in one-third of patients with hypotony.
Intraocular inflammation is a rare but important complication of vitreoretinal surgeries. In particular, postoperative endophthalmitis is a grave condition that may lead severe vision loss [19]. In the present study, treatment plan was changed in four patients because of intraocular inflammation, and the date of discharge was postponed in three (75.0%) of them for close follow-up.
An interesting finding of the present study is that the surgeon’s experience can influence treatment plan changes. It is well-known that there is a learning curve in vitreoretinal surgery. [20] In the study by Mazinani et al., a learning effect was noted in most surgeons. The learning effect was correlated with the total number of procedures, suggesting the importance of the surgeon’s experience in successful surgery [21]. In a more recent study investigating the redetachment rates after retinal detachment surgery, the rate was approximately 20% in beginners. The redetachment rates steadily decreased and stabilized under 10% after approximately 200 surgeries [20]. In the study of Yamakiri et al., surgeons with a higher average annual number of surgeries had significantly better surgical outcomes in scleral buckling procedure [22]. In the present study, we first evaluated the influence of the surgeon’s experience on the incidence of treatment plan changes. We observed that the incidence was higher in less experienced surgeons than in experienced surgeons, suggesting that inexperienced surgeons should anticipate treatment plan changes before surgery.
The previously reported types and incidence of postoperative complications in patients who had undergone vitreoretinal surgery are summarized in Table 5. The incidence of postoperative complications reported in our study were generally lower than those reportedly [5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25]. However, this study only analyzed cases where treatment plan changes were deemed necessary. Therefore, the incidence of actual complications might have been higher.
The strengths of the present study are as follows. Firstly, we first evaluated the incidence of changes in the duration of hospitalization after vitreoretinal surgery owing to treatment plan changes. Although hospitalization was prolonged in only a limited number of patients, the postoperative care plan and subsequent cost of treatment could be markedly changed in these patients. Recently, the number of centers accredited by the Joint Commission International has increased worldwide, [26] suggesting an increasing need for standardization of patient care. In the treatment of a certain disease, predicting the hospitalization period is an important part of establishing a standardized care plan for a patient. Second, we identified incidence, timing, and factors related to changes in treatment plans, which can provide valuable information for establishing treatment plans and discussing them with patients in advance.
The present study had some limitations. Firstly, this retrospective study was conducted at a single institution. Secondly, since patients with certain diagnoses were included, the results of the present study may not be valid for patients who underwent vitreoretinal surgery for other reasons. Thirdly, analysis was performed based on the data obtained within 2 weeks after surgery. Thus, complications that may occur after a longer period, such as open-angle glaucoma, [27] could not be evaluated. Fourth, no strict guidelines were available for surgery, and our results included surgeries performed by multiple surgeons. Therefore, the results of this study require confirmation via further studies with a more controlled design. Finally, detailed postoperative anatomical or functional changes [28] were not evaluated. Subsequent evaluations may be necessary to assess the impact of such changes on the risk of treatment plan changes.
In summary, treatment plan were changed due to postoperative complications in 16.3% of patients within 14 days following vitreoretinal surgery. The most prevalent complication was an increase in IOP. The incidence was higher in patients who underwent gas or oil tamponade and those who underwent surgery performed by less experienced surgeons. In some patients, the discharge date was delayed because of changes in the treatment plan. When establishing a standardized care plan for patients requiring vitreoretinal surgery, the possibility of treatment plan changes and subsequent prolongation of hospitalization should be considered. Further studies are needed to elucidate the specific burdens that treatment plan changes may impose on individual patients.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Popovic MM, Muni RH, Nichani P, Kertes PJ. Pars plana vitrectomy, scleral buckle, and pneumatic retinopexy for the management of rhegmatogenous retinal detachment: a meta-analysis. Surv Ophthalmol 2021.
Glassman AR, Beaulieu WT, Maguire MG, et al. Visual acuity, vitreous hemorrhage, and other ocular outcomes after vitrectomy vs aflibercept for vitreous hemorrhage due to Diabetic Retinopathy: a secondary analysis of a Randomized Clinical Trial. JAMA Ophthalmol. 2021;139:725–33.
Elhusseiny AM, Schwartz SG, Flynn HW Jr, Smiddy WE. Long-term outcomes after Macular Hole surgery. Ophthalmol Retina. 2020;4:369–76.
Far PM, Yeung SC, Ma PE et al. The effect of internal limiting membrane peel for idiopathic epiretinal membrane surgery: a systematic review of randomized controlled trials. Am J Ophthalmol 2021.
Arikan Yorgun M, Toklu Y, Mutlu M, Ozen U. Clinical outcomes of 25-gauge vitrectomy surgery for vitreoretinal diseases: comparison of vitrectomy alone and phaco-vitrectomy. Int J Ophthalmol. 2016;9:1163–9.
Bamonte G, Mura M, Stevie Tan H. Hypotony after 25-gauge vitrectomy. Am J Ophthalmol. 2011;151:156–60.
Chen HF, Yeung L, Yang KJ, Sun CC. Persistent corneal epithelial defect after Pars Plana Vitrectomy. Retina. 2016;36:148–55.
Jabbour E, Azar G, Antoun J, et al. Incidence and risk factors of ocular hypertension following Pars Plana Vitrectomy and Silicone Oil Injection. Ophthalmologica. 2018;240:129–34.
Moussa G, Jalil A, Ivanova T, et al. Expansile gas concentration in primary pseudophakic retinal detachment repair, effect on intraocular pressure and outcomes; the Manchester Pseudophakic Retinal Detachment Study. Graefes Arch Clin Exp Ophthalmol; 2023.
Patel D, Borkar DS, Madhava M, et al. Incidence of management changes at the postoperative Day one visit after Pars Plana Vitrectomy for Retinal detachment. Am J Ophthalmol. 2021;222:271–6.
Rizzo S, Belting C, Genovesi-Ebert F, di Bartolo E. Incidence of retinal detachment after small-incision, sutureless pars plana vitrectomy compared with conventional 20-gauge vitrectomy in macular hole and epiretinal membrane surgery. Retina. 2010;30:1065–71.
Gupta OP, Ho AC, Kaiser PK, et al. Short-term outcomes of 23-gauge pars plana vitrectomy. Am J Ophthalmol. 2008;146:193–7.
Znaor L, Medic A, Binder S, et al. Pars plana vitrectomy versus scleral buckling for repairing simple rhegmatogenous retinal detachments. Cochrane Database Syst Rev. 2019;3:CD009562.
Okumura Y, Inomata T, Iwagami M, et al. Shortened cataract surgery by standardisation of the perioperative protocol according to the Joint Commission International accreditation: a retrospective observational study. BMJ Open. 2019;9:e028656.
Rossi T, Ripandelli G. Pars Plana Vitrectomy and the risk of ocular hypertension and Glaucoma: where are we? J Clin Med 2020;9.
Kanclerz P, Grzybowski A. Complications Associated with the use of expandable gases in vitrectomy. J Ophthalmol. 2018;2018:8606494.
Fujii GY, De Juan E Jr, Humayun MS, et al. Initial experience using the transconjunctival sutureless vitrectomy system for vitreoretinal surgery. Ophthalmology. 2002;109:1814–20.
Chen D, Lian Y, Cui L, et al. Sutureless vitrectomy incision architecture in the immediate postoperative period evaluated in vivo using optical coherence tomography. Ophthalmology. 2010;117:2003–9.
Dave VP, Pathengay A, Basu S, et al. Endophthalmitis after Pars Plana Vitrectomy: clinical features, risk factors, and Management Outcomes. Asia Pac J Ophthalmol (Phila). 2016;5:192–5.
Radeck V, Helbig H, Barth T, et al. The learning curve of retinal detachment surgery. Graefes Arch Clin Exp Ophthalmol. 2021;259:2167–73.
Mazinani BA, Rajendram A, Walter P, Roessler GF. Does surgical experience have an effect on the success of retinal detachment. surgery? Retina. 2012;32:32–7.
Yamakiri K, Sakamoto T, Koriyama C, et al. Effect of surgeon-related factors on outcome of retinal detachment surgery: analyses of data in Japan-retinal detachment registry. Sci Rep. 2022;12:4213.
Al-Hinai AS. Corneal epithelial defect after pars plana vitrectomy. Oman J Ophthalmol. 2017;10:162–6.
Ben Ghezala I, Mariet AS, Benzenine E, et al. Incidence of acute postoperative endophthalmitis following macular surgery in France between 2006 and 2016. Acta Ophthalmol. 2020;98:e333–e8.
Desai A, Rubinstein A, Reginald A, et al. Feasibility of day-case vitreoretinal surgery. Eye (Lond). 2008;22:169–72.
Mehta A, Goldstein SD, Makary MA. Global trends in center accreditation by the Joint Commission International: growing patient implications for international medical and surgical care. J Travel Med 2017;24.
Chang S. LXII Edward Jackson lecture: open angle glaucoma after vitrectomy. Am J Ophthalmol. 2006;141:1033–43.
Lyssek-Boroń A, Wylęgała A, Krysik K et al. Assessment of vascular changes in patients after Pars Plana vitrectomy surgery due to Macula-Off Rhegmatogenous Retinal detachment. J Clin Med 2021;10.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
Study conception and design (J.H.K.); acquisition of data (J.H.Y., J.H.K., C.G.K., J.W.K.); analysis and interpretation of data (J.H.Y., J.H.K., C.G.K., J.W.K.); drafting the article (J.H.Y., J.H.K.); revising the article critically for important intellectual content (J.H.K.); final approval of the article (J.H.Y., J.H.K., C.G.K., J.W.K.).
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Board of Kim’s Eye Hospital and was conducted in accordance with the tenets of the Declaration of Helsinki. Due to the retrospective nature of this study, the need for an informed consent was waived off (Kim’s Eye Hospital IRB, Seoul, South Korea).
Consent for publication
Consent for publication was not obtained since no identifying information of the participants was presented in this study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yoon, J.H., Kim, J.H., Kim, C.G. et al. Incidence of early complications requiring treatment plan changes after vitreoretinal surgery: a single-center study in South Korea. BMC Ophthalmol 23, 282 (2023). https://doi.org/10.1186/s12886-023-03030-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-023-03030-z