Abstract
Purpose
To investigate early changes in the intraocular pressure (IOP) and macular microvascular structure in eyes with branch retinal vein occlusion (BRVO) treated with intravitreal Ranibizumab injection.
Methods
This study enrolled 30 patients (one eye per patient) who received intravitreal injections (IVI) of ranibizumab for macular edema secondary to BRVO. IOP were measured before, 30 min (min) and 1 month following IVI. Changes in macular microvascular structure were examined via assessment of foveal avascular zone (FAZ) parameters, vascular density (VD) of superficial vascular complex (SVC), and deep vascular complex (DVC) in whole macula, central fovea and parafovea area which were measured automatically by optical coherence tomography angiography (OCTA) on the same time as IOP examinations. Paired t test and Wilcoxon test were used to compare pre- and post-injection values. The correlation between IOP and OCTA findings was assessed.
Results
IOP Measurements at 30 min post-IVI (17.91 ± 3.36 mmHg) increased significantly from baseline (15.07 ± 2.58 mmHg, p < 0.001), then became similar with baseline after 1 month (15.00 ± 3.16 mmHg, p = 0.925). 30 min past the injection, the parameters of VD of the SCP significantly decreased in comparison to baseline, then became similar with baseline after one month, while there were no significant changes in other OCTA parameters, including parameters of VD of the DCP and the FAZ. At 1 month after IVI, in comparison to baseline, no significant changes were observed in all of the OCTA parameters (P > 0.05). There were no significant correlations between IOP and OCTA findings no matter 30 min or 1 month post-IVI (P > 0.05).
Conclusions
Transient IOP elevation and decreased superficial macular capillary perfusion density were detected 30 min post-IVI, however, no potential continual macular microvascular damage was suspected.
Similar content being viewed by others
Introduction
Branch retinal vein occlusion (BRVO) is a relatively common retinal vascular disorder in elderly patients that can lead to visual impairments [1]. Macular edema (ME) secondary to BRVO is considered the main cause of visual impairment [2]. At present, intravitreal anti-vascular endothelial growth factor (VEGF) therapy, such as ranibizumab, is the standard of care of ME associated with BRVO [3]. The usefulness and convenience of IVI of anti-VEGF has been widely recognized [4,5,6,7]. However, concerns about the effect of the IVI of anti-VEGF on intraocular pressure (IOP) have arisen in the last few years. It is already known that there is a transient elevation of IOP immediately after any intravitreal injection, which normalizes over minutes to hours [8,9,10,11,12]. Until now, few studies were reported about the acute and subacute post-IVI changes of macular microvascular structure [13]. Whether the acute and subacute post-IVI IOP changes are associated with macular microvascular structure changes is still controversial [14,15,16]. In this study, we aimed to quantitatively investigate the acute and subacute changes in the IOP and macular microvascular structure in a cohort of patients undergoing intravitreal ranibizumab injection for ME following BRVO, to better understand retinal perfusion changes associated with IVI and also the correlation with the post-IVI IOP changes.
Materials and methods
Subjects
This prospective observation study was performed from September, 2016 to October, 2017. The research protocols were approved by the Ethics Committee of Beijing Hospital, carried out in accordance with the tenets of the Declaration of Helsinki. Written informed consent was obtained from each participant. Thirty eyes of 30 patients (one eye per patient) who were ultimately diagnosed with ME due to BRVO were enrolled.
All patients underwent an ophthalmological examination with best-corrected visual acuity (BCVA), IOP measurements, slit lamp examination, fluorescein fundus angiography (FFA), dilated fundoscopic examinations and OCTA. Additionally, vital signs, such as systolic and diastolic blood pressures were also acquired. IOP, OCTA, and blood pressure, including systolic blood pressure (SBP)and diastolic blood pressure (DBP) were acquired at baseline, 30 min, and 1-month post-injection.
Patients were excluded if they met the following criteria: (1) hemi-CRVO or CRVO; (2) diabetic maculopathy and/or retinopathy; (3) any other BCVA compromising ocular disease; (4) any prior intravitreal anti-VEGF or corticosteroid injections; (5) any prior retinal laser photocoagulation; (6) IOP higher than 21 mmHg; (7) history of vitrectomy; (8) history of myocardial infarction or stroke within three months; and (9) other major systemic disorders. The inclusion and exclusion criteria were similar to Song’s study [17].
Treatments
Each patient received intravitreal ranibizumab injection at a dose of 0.5 mg/ 0.05 ml. After instilling topical 0.4% oxybuprocaine chloride eye drops for topical anesthesia, the eye was irrigated with 5% povidone-iodine and opened using a lid retractor, and the drug was injected through the pars plana 3.5 mm posterior to the limbus in the inferotemporal quadrant in pseudophakic eyes and 4.0 mm posterior to the limbus in phakic eyes using a 30 G needle. The treatment protocol was similar to Song’s study [17].
IOP
IOP was measured with Goldmann applanation tonometry(Haag-Streit AT 900) at least twice in each eye at each visit. The average of the measurements wastaken. The baseline IOP was measured at the visit before the injection. We also examined the IOP 30 min and 1 month after the injection.
Optical coherence tomography angiography (OCTA)
All patients had macular OCT-A performed before and 30 min, and 1-month post-IVI treatment by spectral-domain OCT (RTVue XR Avanti, Optovue, Inc., Fremont, CA, USA). We only chose OCTA images with an image quality score of 6 or more. For each patient, 3 × 3 mm scans centered on the fovea were acquired. Macular scans were segmented into superficial and deep OCT-A layers. The OCT system’s Angio Analytics software (version 2017.1.0.151, Optovue, Inc.) performs automatic segmentation of vessel layers. Based on the default setting of the OCTA system, the SCP of the retina included blood vessels from the internal limiting membrane (ILM) to − 10 μm below the inner plexiform layer (IPL). DCP of the retina included blood vessels from − 10 μm below the IPL to 10 μm below the outer plexiform layer (OPL). The SCP, DCP as described as the whole macula, the fovea and parafovea which were measured automatically by OCTA built-in software. The fovea was defined as the area within the central 1-mm ring of the Early Treatment Diabetic retinopathy Study (ETDRS) grid. Parafovea was considered as the area between the central 1- and the 3-mm ring of the ETDRS grid. (Fig. 1) FAZ was defined as a capillary-free area in the central macular region on traditional FFA analysis of the retina. FAZ measurements include the following parameters: the FAZ area; the FAZ perimeter (PERIM); the acircularity index (AI), which is defined as the ratio of the perimeter of the FAZ and the perimeter of a circle with equal area, AI = PERIM/equal area standard circumference; and the FD300, which refers to the blood vessel density within a 300 μm wide ring around the FAZ. The FAZ area, PERIM, AI, and FD-300 were used to evaluate the hemodynamics of the FAZ [17]. We recorded the VD of the whole macula, fovea, parafovea of the SCP and DCP, FAZ area, perimeter (PERIM), FD-300 and AI and also their relationships with IOP were observed.
Statistical analysis
Continuous variables with normal distribution were presented as mean ± standard deviation and with nonnormal distribution were presented as median (interquartile range). Paired t-test and Wilcoxon paired signed rank test were used to compare changes pre- and post-IVI of ranibizumab in BRVO eyes. Normality of errors (residuals) was checked while modeling (histograms and P–P plots). Pearson correlation analyses were adopted to study the correlations among IOP and OCTA findings 30 min and 1 month post-injection. Statistical analyses were performed with the IBM SPSS Statistics for Windows, Version 28.0 (IBM Corp., Armonk, NY, USA), and statistical significance was established at two-tailed P < 0.05.
Results
30 eyes of 30 patients over age 18 (Mean 57.5 years, Std. Deviation 7.61) were studied. The mean pre-injection IOP was 15.07 ± 2.58 mmHg. The mean IOP at 30 min past the IVI was 17.91 ± 3.36 mmHg with the statistically significant increase of 2.85 mmHg compared with the baseline (p < 0.001). The IOP measurements 1 month post-IVI was 15.00 ± 3.16 mmHg, which decreased significantly compared with 30 min past the injection (mean difference 2.91, p = 0.001), thus became similar with the baseline (mean difference 0.07, p = 0.925). No significant changes were found among the SBP and ABP measurements before, 30 min and 1 month after the IVI(p > 0.05). (Tables 1 and 2).
30 min past the injection, statistically significant decreases were found in VD of SVC, as we could see the decreases of VD of SVC in macula (mean difference 3.10, p < 0.001), in fovea (mean difference 2.74, p = 0.006), in parafovea (mean difference 2.68, p = 0.002). 1 month later, the parameters we observed in VD of SVC increased significantly compared with 30 min past the injection, with macula (mean difference 4.41, p < 0.001), fovea (mean difference 1.52, p = 0.007), parafovea (mean difference 3.56, p = 0.009), thus all the superficial parameters became similar with the baseline(p > 0.05). (Tables 1 and 2).
The VD of DVC had no significant changes. No Changes were seen in the VD of DVC in the area of macula, fovea or parafovea no matter 30 min or 1 month after the injection. (p > 0.05) (Tables 1 and 2).
All the FAZ parameters including FAZ area, FAZ perimeter, FAZ AI and FD-300 had no significant changes no matter 30 min or 1 month after the injection. (p > 0.05) (Tables 1 and 2).
Unfortunately, IOP increase had no significant correlation with the decrease in the parameters of VD of SVC, including macula, fovea and parafovea.
Discussion
IOP elevations are likely to occur in post-IVI cases [8,9,10,11,12]. However, the impact of these transient IOP elevations on retinal physiology is poorly understood. Some authors have shown that IOP spikes and changes in OCTA parameters can be observed post-IV, however, the results are still controversial [14,15,16]. In this study, we analyzed the acute and subacute alterations in IOP and macular microvascular changes in OCTA parameters in patients with BRVO post-IVI.
In agreement with previous reports, our study shows a transient IOP elevation 30 min after ranibizumab injection. We found the mean pre-injection IOP was 15.07 ± 2.58 mmHg; the mean IOP at 30 min past the IVI was 17.91 ± 3.36 with the significant increase of 2.85 mmHg. The result was similar with many previous studies which have been conducted to assess short-term IOP changes after intravitreal injection [9, 18, 19]. The pathogenesis of short-term increases in IOP after anti-VEGF IVIs is still controversial, but has been presumably due to the transiently increased intraocular fluid volume after injection, thus increases the pressure of the intraocular contents to the eyeball. [9]
The IOP measurements 1 month after the IVI were 15.00 ± 3.16 mmHg, thus became similar with the baseline. Previous studies supported our result. Gado and Macky [20] reported a maximum IOP of 21 mmHg in treated patients over a 3 to 6-month follow-up; Güler et al. [21] reported a mean IOP of 13.2 ± 4.4 mmHg at 1-month follow-up.
In summary, intravitreal injection of anti-VEGF agents generally resulted in acute post-injection elevations of IOP, and in the majority of patients, returned to normal within a short period of time.
Meanwhile, we found that 30 min past the injection, statistically significant decreases were found in VD of SVC, as we could see the decreases of VD of SVC in macula (mean difference 3.10, p < 0.001), in fovea (mean difference 2.74, p = 0.006), in parafovea (mean difference 2.68, p = 0.002), while no changes were seen in the VD of DVC. The result is similar with Barash et al. [15] Recently, Takusagawa et al. [22] found that glaucoma affected the SVC to a much greater degree than DVC. It is not surprising that the SVC VD was greatly reduced in glaucomatous eyes, as it supplies the nerve fiber layer (NFL), the ganglion cell layer (GCL) and part of the inner plexiform layer (IPL), [23,24,25] which are the anatomic layers most affected by glaucoma [26, 27]. The DCP was minimally affected by glaucoma, as it supplies the middle retinal layers that do not include the retinal ganglion cells.
These changes match with the acute perfusion effects of intravitreal injections observed in our study, where the VD of SVC decreased significantly compared with the VD of DVC, which had no changes. It is possible that we are seeing the ischemic effects of increased IOP. This lends credence to the idea that intravitreal injections may stress the same structures that get damaged in glaucomatous eyes. Since glaucoma damages retinal ganglion cells (RGC) and approximate 1/3 of RGCs resides in the macula, so macular perfusion is theoretically a good place to detect glaucoma and assess disease severity [28, 29].
We also found that no matter superficial or deep retinal capillary perfusion density measured 1 month after IVI of ranibizumab remain unchanged. The result is similar with Falavarajni et al. [30], suggesting that changes like those measured in our study are short term effects more likely to be IOP related than medication related. This study also agrees with other reports that overall FAZ parameters does not change significantly following acute IOP elevation due to intravitreal injections [16].
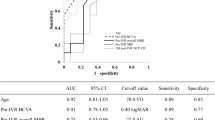
In the current study, unfortunately, IOP increase had no significant correlation with the decrease in the parameters of VD of SVC, including macula, fovea and parafovea. In our study, the IOP measurements were taken approximately 30 min after injection, whereas the OCT-A imaging followed approximately 1 min thereafter [8,9,10, 18, 19, 31]. In a study in our department, we measured the IOP of 292 patients 10 min, 30 min after injection and found similar results. The mean IOP was 23.8mmHg at 10 min, and 20.5mmHg at 30 min [32]. In our series, we did not check IOP and OCT-A at 1 min, 5 min or 10-min post-IVI. According to the literature review, we suspect quite possibly, if the OCT-A images and IOP measurements had been taken closer to the time of injection, they may have shown even greater changes in perfusion density and IOP, then maybe we can find the better correlation. As a result, angiographic changes likely correlate to elevated intraocular pressures already in the process of equilibration.
In conclusion, this study of 30 eyes shows that intravitreal injections induce acute changes in IOP and retinal angiographic perfusion density. The superficial layers of the macula are more affected than deep layers by these changes, while after one month, no changes in quantitative OCTA parameters, including, FAZ and VD were observed, thus no potential continual macular microvascular damage was suspected.
The main limitations of this study included the small sample size, the diagnosis with inclusion of only the patients affected by BRVO, the absence of measurements immediately post-IVI. Thus, further randomized controlled studies with a longer follow-up and a larger sample size are highly warranted.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Rogers SL, McIntosh RL, Lim L et al. “Natural history of branch retinal vein occlusion: an evidence-based systematic review, “Ophthalmology, vol. 117, no. 6, pp.1094–1101, 2010.
Ho M, Liu DTL, Lam DSC, Jonas JB. Retinal vein occlusions, from basics to the latest treatment. Retina. 2016;36(3):432–48.
Gerding H, Mones J, Tadayoni R, Boscia F, Pearce I, Priglinger ´S. Ranibizumab in retinal vein occlusion: treatment recommendations by an expert panel. Br J Ophthalmol. 2015;99(3):297–304.
Song S, Yu X, Dai H. The efficacy of combination of intravitreal ranibizumab with triamcinolone or laser photocoagulation for macular edema secondary to branch retinal vein occlusion. Chin J Ocular Fundus Dis. 2015;31:18–21.
Rabena MD, Pieramici DJ, Castellarin AA, Nasir MA, Avery RL. “Intravitreal bevacizumab (Avastin) in the treatment of macular edema secondary to branch retinal vein occlusion,”Retina, vol. 27, no. 4, pp.419–425,2007.
Campochiaro PA, Heier JS, Feiner L, et al. Ranibizumab for macular edema following branch retinal vein occlusion: sixmonth primary end point results of a phase III study. Ophthalmology. 2010;117(6):1102–12.
Campochiaro PA, Clark WL, Boyer DS, et al. Intravitreal aflibercept for macular edema following branch retinal vein occlusion: the 24-week results of the VIBRANT study. Ophthalmology. 2015;122(3):538–44.
Hong SW, Jee D. Effect of the Honan intraocular pressure reducer to prevent vitreous reflux after intravitreal bevacizumab injection. Eur J Ophthalmol. 2012;22(4):615–9.
Murray CD, Wood D, Allgar V, et al. Short-term intraocular pressure trends following intravitreal ranibizumab injections for neovascular age-related macular degeneration-the role of oral acetazolamide in protecting glaucoma patients. Eye (Lond). 2014;28(10):1218–22.
Kim KS, Jee D. Effect of the Honan intraocular pressure reducer on intraocular pressure increase following intravitreal injection using the tunneled scleral technique. Jpn J Ophthalmol. 2011;55(6):632–7.
Pang CE, Mrejen S, Hoang QV, et al. Association between needle size, postinjection reflux, and intraocular pressure spikes after intravitreal injections. Retina. 2015;35(7):1401–6.
Cacciamani A, Oddone F, Parravano, et al. Intravitreal injection of bevacizumab: changes in intraocular pressure related to ocular axial length. ”Jpn J Ophthalmol. 2013;57(1):63–7.
Lisa T, Federica E, Pasquale V et al. “ Changes in Ocular Blood Flow after Ranibizumab Intravitreal Injection for Diabetic Macular Edema Measured Using Laser Speckle Flowgraphy,” Biomed Res Int, vol. 2020, 9496242,2020.
Chui Ming Gemmy Cheung. Kelvin Yi Chong Teo, Sai Bo Bo Tun, “Differential reperfusion patterns in retinal vascularplexuses following increase in intraocular pressure an oct angiography study,” Sci. Rep, vol. 10, no.1, pp. 16505, 2020.
Barash A, Chui TYP, Garcia P, Rosen RB. Acute macular and peripapillary angiographic changes with intravitreal injections. Retina. 2020;40(4):648–56.
Nadhini Arumuganathan MRobertJ, Wiest M, DamianoToro, et al. Acute and subacute macular and peripapillary angiographic changes in choroidal and retinal blood flow postintravitreal injections. Sci Rep. 2021;11(1):19381.
Shuang Song X, Yu P, Zhang et al. “ Changes in Macular Microvascular Structure in Macular Edema Secondary to Branch Retinal Vein Occlusion Treated with Antivascular Endothelial Growth Factor for One Year,”J Ophthalmol, May 17, 6645452,2021.
Knip MM, Välimäki J. Effects of pegaptanib injections on intraocular pressure with and without anterior chamber paracentesis: a prospective study. Acta Ophthalmol. 2012;90(3):254–8.
Theoulakis PE, Lepidas J, Petropoulos IK, et al. Effect of brimonidine/timolol fixed combination on preventing the short-term intraocular pressure increase after intravitreal injection of ranibizumab. Klin Monbl Augenheilkd. 2010;227(4):280–4.
Gado AS, Macky TA. Dexamethasone intravitreous implant versus bevacizumab for central retinal vein occlusion-related macular oedema: a prospective randomized comparison. Clin Exp Ophthalmol. 2014;42(7):650–5.
Güler M, Capkin M, Simsek A, et al. Short-term effects of intravitreal bevacizumab on cornea and anterior chamber. Curr Eye Res. 2014;39(10):989–93.
Takusagawa HL, Liu L, Ma KN. Projection-resolved Optical Coherence Tomography Angiography of Macular Retinal circulation in Glaucoma. Ophthalmology. 2017;124(11):1589–99.
Snodderly DM, Weinhaus RS, Choi JC. Neural-vascular relationships in central retina of macaque monkeys (Macaca fascicularis). J Neurosci. 1992;12(4):1169–93.
Snodderly DM, Weinhaus RS. Retinal vasculature of the fovea of the squirrel monkey, Saimiri sciureus: three-dimensional architecture, visual screening, and relationships to the neuronal layers. J Comp Neurol. 1990;297(1):145–63.
Provis JM. Development of the primate retinal vasculature. Prog Retin Eye Res. 2001;20(6):799–821.
Tan O, Chopra V, Lu AT, et al. Detection of macular ganglion cell loss in glaucoma by Fourier domain optical coherence tomography. Ophthalmology. 2009;116(12):2305–14.
Mwanza JC, Durbin MK, Budenz DL, et al. Glaucoma diagnostic accuracy of ganglion cell-inner plexiform layer thickness: comparison with nerve fiber layer and optic nerve head. Ophthalmology. 2012;119(6):1151–8.
Quigley HA, Dunkelberger GR, Green WR. Retinal ganglion cell atrophy correlated with automated perimetry in human eyes with glaucoma. Am J Ophthalmol. 1989;107(5):453–64.
Curcio CA, Allen KA. Topography of ganglion cells in human retina. J Comp Neurol. 1990;300(1):5–25.
Ghasemi Falavarjani K, Iafe NA, Hubschman JP, Tsui I, Sadda SR, Sarraf D. Optical coherence tomography angiography analysis of the Foveal Avascular Zone and Macular Vessel Density after Anti-VEGF therapy in eyes with Diabetic Macular Edema and retinal vein occlusion. Invest Ophthalmol Vis Sci. 2017;58(1):30–4.
Katayama BY, Bonini-Filho MA, Messias AM, et al. Comparison of acetazolamide, brimonidine, and anterior chamber paracentesis for ocular hypertension control after initial intravitreal bevacizumab injection: a randomized clinical trial. J Glaucoma. 2014;23(7):461–3.
Song Shuang Z, Peng Gu, Xiaoya, et al. Analysis of factors associated with short-term elevation of intraocular pressure after ranibizumab intravitreal injection. Chin J Ocul Fundus Dis. 2018;34(5):432–5.
Acknowledgements
Not applicable.
Funding
This work was supported financially by Beijing Hospital under 121 Projects (121–2016001 and BJ-2020-167).
Author information
Authors and Affiliations
Contributions
Dr Xiaoyu Li: methodology, formal analysis, and writing of the manuscript. Dr Qin Chen: contributed to the preparations of the manuscript. Professor Xiaobing Yu: review & editing of the manuscript and also the Funding acquisition. And all authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study approved by the Ethics Committee of Beijing Hospital, carried out in accordance with the tenets of the Declaration of Helsinki. Written informed consent was obtained from each participant.
Consent for publication
Not applicable.
Competing interests
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, X., Chen, Q. & Yu, X. Acute and subacute intraocular pressure and macular microvascular structure changes after intravitreal ranibizumab injection in eyes with branch retinal vein occlusion. BMC Ophthalmol 23, 160 (2023). https://doi.org/10.1186/s12886-023-02889-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-023-02889-2