Abstract
Background
To investigate the visual and refractive outcomes in patients with mild to moderate myopia after laser-assisted subepithelial keratectomy (LASEK) using the 500 Hz pulse rate of the Triple-A profile.
Methods
Thirty-six eyes of 20 patients (mean age, 27.5 ± 4.6 years) were included in this prospective, consecutive study. Uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), corneal topography, and corneal aberrations were measured preoperatively and 1 day, 1 week, 1, 3 and 6 months post-operation.
Results
At 1 week after surgery, UDVA was better than or equal to 20/25 in all eyes. At postoperative 6 months, the efficacy and safety index was 1.05 ± 0.13 and 1.12 ± 0.15, respectively; all eyes had a UDVA of 20/20 or better, and no eyes showed a loss in CDVA; 100% of the eyes were within ±1.00 D of the attempted spherical equivalent (SE) correction.
Conclusion
The postoperative results indicate that using the Triple-A ablation profile of the MEL 90 excimer laser with a 500 Hz pulse rate is a safe, efficient, and predictable method to correct mild to moderate myopia.
Similar content being viewed by others
Background
The excimer laser has the potential of producing tissue ablation with a high degree of precision and with minimal damage to the adjacent structures [1]. Laser-assisted subepithelial keratectomy (LASEK) was introduced in 1999 by Camellin for the correction of refractive error [2]. Treatment for myopia and myopic astigmatism using the MEL 80 excimer laser (Carl Zeiss Meditec AG, Jena, Germany) with the tissue saving ablation (TSA) and aberration smart ablation (ASA) profiles during LASEK has been reported to have excellent refractive outcomes in safety, efficacy, and predictability [3,4,5,6]. The use of ASA can induce a positive spherical aberration when correcting for high myopia and a relatively higher ablation depth when treating low myopia [7]. The advanced ablation algorithm (Triple-A) profile, developed by Carl Zeiss Meditec AG, is an ideal ablation profile to achieve better visual outcomes with a lower induction rate of higher-order aberrations (HOAs) while decreasing the ablation depth for the correction of myopia, especially for low myopia [7,8,9]. The MEL 90 excimer laser has two frequencies available for the correction of refractive error. The 250 Hz pulse rate has been recommended to treat refractive error for surface ablation, while the 500 Hz pulse rate has been used in laser-assisted in-situ keratomileusis (LASIK) procedures. Reinstein et al. demonstrated that the 500 Hz pulse rate achieved high efficacy for myopia up to −10.00 D and cylinder up to 5.00 D after LASIK [9]. For LASEK procedures, the refractive outcomes with the MEL 90 excimer laser have not yet been reported. Therefore, we conducted a prospective study to demonstrate the efficacy and safety after LASEK using a 500 Hz pulse rate.
Methods
Subjects
The research was conducted at the Ophthalmology Department of the Eye and ENT Hospital in Shanghai, China. In this prospective study, 36 eyes of 20 consecutive patients who received LASEK using the MEL 90 excimer laser (the MEL 90 group) for the correction of myopia and myopic astigmatism were enrolled. The follow-up time was 6 months.
For the control group (the MEL 80 group), we included 33 eyes of 17 patients who were treated with the TSA profile using the 250 Hz pulse rate of the MEL 80 with 6.5 mm for the optical zone (Carl Zeiss Meditec, Jena, Germany). Data were selected from our previously published data.
Inclusion criteria were a spherical refraction less than −6.00D, astigmatism from 0.00 to −3.75D, corrected distance visual acuity (CDVA) of 20/25 or better, stable refraction for 2 years before surgery, and an absence of other pathologic ocular conditions or relevant systemic diseases.
The research followed the tenets of the Declaration of Helsinki and was approved by the Ethics Committee of the EENT Hospital of Fudan University. All patients signed a consent inform.
Surgical technique
LASEK treatments began with 12 s of 20% alcohol-assisted epithelial flap creation, followed by standard excimer laser ablation using the MEL 90 with a 500 Hz pulse rate (Carl Zeiss Meditec, Jena, Germany, Triple-A profile, LASIK mode). The optical zone was 6.5 mm in all patients (Fig. 1). The epithelial flap was repositioned after laser ablation, and a bandage soft contact lens (ACUVUE OASYS; Johnson & Johnson, New Brunswick, NJ) was applied. The target refraction was plano for all patients.
The represented images showed the laser-assisted subepithelial keratectomy (LASEK) surgical procedures. The ablation center adjustment (a); the corneal epithelium was immersed in 20% alcohol (b); the epithelial flap was removed following immersion (c); the Corneal Bowman’s membrane and stroma were ablated with the MEL 90 excimer laser (d); the epithelial flap was repositioned after laser ablation (e); a bandage soft contact lens was applied (f)
Postoperative evaluation
Patients were instructed to wear the bandage soft contact lens for 1 week. Topical steroids (fluorometholone 0.1%; Santen Pharmaceutical Co., Ltd.) were initially administered 8 times/day and tapered over 75 days. Topical antibiotics (ofloxacin ophthalmic solution 0.5%; Santen Pharmaceutical Co., Ltd.) were administered 4 times/day for 7 days. Tears Naturale (hypromellose 2910, dextran 70, glycerol eye drops; Alcon Laboratories, Inc.) were administered 4 times/day for 3 months.
Patients were followed-up at postoperative 1 day, 1 week, 1, 3 and 6 months. All subsequent follow-up visits recorded uncorrected distance visual acuity (UDVA), CDVA, manifest refraction, corneal topography, and corneal aberrations. All postoperative examinations were conducted by the same experienced optometrists.
Measurement of corneal aberrations
Corneal HOAs were obtained using a rotating Scheimpflug Camera (Pentacam HR; Oculus, Wetzlar, Germany) in a dark room. The corneal HOAs of the anterior surface, posterior surface, and total cornea were analyzed over a 6.0 mm central diameter at pre-operation and at postoperative 6 months. We analyzed the root mean square values of the corneal HOAs including the third to sixth HOAs.
Data analysis
Statistical analyses were performed using SPSS software (version 13.0; SPSS Inc.). The mean ± standard deviation (SD) was calculated. A Student’s t-test was performed to determine the difference between pre-operation and post-operation and between the MEL 90 and MEL 80 groups. P values of less than 0.05 were considered statistically significant.
Results
Table 1 shows the demographic data of the two groups. All surgeries were uneventful without any intraoperative complications. No postoperative complications, such as corneal haze, wound dehiscence, inflammation and infection were observed in any eyes.
Refractive outcomes
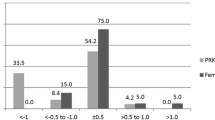
At postoperative 6 months, the efficacy and safety index after MEL 90 was 1.05 ± 0.13 and 1.12 ± 0.15, respectively. Figure 2 shows the distribution of UDVA and CDVA following LASEK. Table 2 shows the manifest refraction, logMAR CDVA and logMAR UDVA after use of the MEL 90 and MEL 80 excimer laser at 6 months after surgery.
Visual outcomes after the MEL 90 and MEL 80 at 6 months: Cumulative percentage of eyes with preoperative corrected distance visual acuity (CDVA) and postoperative uncorrected distance visual acuity (UDVA) results (a&b), percentage of eyes with various changes in postoperative UDVA and preoperative CDVA (c), and percentage of eyes with various changes in CDVA (d)
At postoperative 6 months, 81 and 85% of eyes were within ±0.50 D of the attempted spherical equivalent (SE) correction in the MEL 90 and MEL 80 groups, respectively, and 100% of eyes were within ±1.00 D of the attempted SE correction in both groups. Scatterplots of the achieved versus attempted spherical equivalent are shown in Fig. 3a and b . The percentage of eyes with the accuracy of SE to intended target is shown in Fig. 3c.
Figure 4a and b shows the percentage of eyes with refractive astigmatism. The distributions of absolute angle of error are presented in Fig. 4c.
Corneal aberrations
The mean change in anterior, posterior, and total corneal spherical aberration induction was 0.071 ± 0.112 μm, −0.005 ± 0.014 μm, and 0.094 ± 0.079 μm, respectively (Fig. 5).
Discussion
Although LASIK has gained widespread acceptance in corneal refractive surgery due to little pain and rapid visual rehabilitation, surface ablation including LASEK is also a valuable technique for patients with low myopia, a thinner cornea, or retinal pathology [10,11,12]. The main differences between the LASEK and LASIK procedures were the incidence rate of corneal haze and flap-related complications. The UDVA and CDVA could be reduced after LASIK due to flap-related complications including diffuse lamellar keratitis, epithelial ingrowth, flap traumatic shifting or avulsion [13]. Although several studies have reported corneal haze after surface ablation for the correction of high myopia [14, 15], there was no significant corneal haze between LASIK and LASEK for the treatment of low to moderate myopia [16, 17]. The MEL 90 has PRK and LASIK modes for laser ablation; the nomogram of PRK is different from the nomogram of LASIK, and PRK mode is more tissue saving than LASIK mode when treating the same refraction. Furthermore, there are the 250 Hz and 500 Hz pulse rates in LASIK mode, while PRK mode has only a 250 Hz pulse rate. In the current study, we have demonstrated it was feasible to perform LASEK procedures using the LASIK mode of the MEL 90 excimer laser with a 500 Hz pulse rate.
When compared to the MEL 80, the main differences of the MEL 90 were the pulse rate and ablation profile [9]. The treatment time of the 6 mm optical zone decreased from 3.2 s per diopter for the MEL 80 to 1.3 s per diopter for the MEL 90. A previous study found it to have a higher refractive predictability due to the faster ablation rate [9]. In the current study we further confirmed that predictability was higher after use of the MEL 90 when compared to the MEL 80, indicated by the higher R 2 value on the attempted versus achieved spherical equivalent scatter plot (Fig. 3a and b).
The MEL 90 offers a newly developed ablation profile called Triple-A, which consists of a basic profile in combination with a compensation algorithm for an enhanced energy correction. The enhanced energy correction in the Triple-A profile is stronger than that of ASA and TSA profiles. In two reports, this achieved better predictability compared with the ASA profile after LASIK and photorefractive keratectomy (PRK) [7, 8]. In our study we demonstrated better predictability achieved with the MEL 90 and Triple-A profile than with the MEL 80 and TSA profile after LASEK.
LASEK is the optimized mode for surface ablation, and several papers have reported good efficacy following LASEK for mild to moderate myopia [10, 18,19,20]. Since the MEL 90 was released, the safety and efficacy of the MEL 90 after LASIK has been reported by Reinstein et al. [9]. The safety, efficacy, and predictability of the MEL 90 after LASEK for mild to moderate myopia was worth investigation.
In our study all surgeries were uneventful and no definite intraoperative complications were observed. At postoperative 6 months, the safety index of the MEL 90 was 1.12 ± 0.15 and no eyes demonstrated a loss in CDVA, indicating the safety of LASEK with the MEL 90 Triple-A profile, which was consistent with the results after MEL 80 and previous studies [18, 19]. However, there were still some reports about postoperative complications such as haze, regression, and infection [21, 22]. Our research revealed that the epithelium survived and no patients complained of postoperative pain, which may be due to reduced dissociative time of the epithelial flap because of the faster pulse rate, and the activity of epithelial flap was retained to the greatest extent. This further increased safety and patient satisfaction following LASEK. The results in our study demonstrated the safety of using the Triple-A ablation profile with a 500 Hz pulse rate for a LASEK procedure.
The UDVA of all patients in the MEL 90 group at 1 week and 6 months was 20/25 or better and 20/20 or better, respectively, indicating the good efficacy of LASEK. The UDVA after LASEK was better than that after photorefractive keratectomy (PRK) in the early period after surgery [23, 24], which is characteristic of LASEK’s optimized surface ablation. Our results showed a faster recovery speed in UDVA when compared to the MEL 80 group (92% of eyes achieved 20/25 or better 1 week after surgery) and previous reports [20, 22, 25], which may be associated with the shorter ablation time, advanced ablation mode, and retained epithelial flap activity. PRK is no longer performed in our clinic in favor of LASEK, therefore the results following LASEK and PRK procedures were not compared in this study.
The SE diopter was 0.15 ± 0.41 D at 6 months after surgery with the MEL 90 excimer laser, which is similar to the results in the control group (0.19 ± 0.37 D, P = 0.613), and better than our previous results (−0.35 ± 0.41 D) [26], indicating the excellent predictability of the Triple-A ablation profile. Previous studies have reported regression and instability after LASEK [19, 21], while no such complications were observed in our study; this may be relative to the Triple-A ablation profile and a patient’s refraction. There are some limitations in this study. The refractive diopter was less than −6 D, and the follow-up period was relative short. Further studies with high myopia and a longer follow-up period will be conducted to demonstrate the outcomes after use of the MEL 90 excimer laser.
Conclusions
In conclusion, the MEL 80 excimer laser and the MEL 90 excimer laser used with a 500 Hz pulse rate and the Triple-A profile showed comparable results in terms of efficacy, safety, and predictability for mild to moderate myopia in a LASEK procedure.
Abbreviations
- ASA:
-
Aberration smart ablation
- CDVA:
-
Corrected distance visual acuity
- HOAs:
-
Higher-order aberrations
- LASEK:
-
Laser-assisted subepithelial keratectomy
- LASIK:
-
Laser-assisted in-situ keratomileusis
- PRK:
-
Photorefractive keratectomy
- SE:
-
Spherical equivalent
- TSA:
-
Tissue saving ablation
- UDVA:
-
Uncorrected distance visual acuity
References
Trokel SL, Srinivasan R, Braren B. Excimer laser surgery of the cornea. Am J Ophthalmol. 1983;96:710–5.
Camellin M. LASEK may offer the advantages of both LASIK and PRK. Ocul Surg News Int Edn. 1999;3:14–5.
Qian Y, Huang J, Chu R, Zhou X, Olszewski E. Influence of intraocular astigmatism on the correction of myopic astigmatism by laser-assisted subepithelial keratectomy. J Cataract Refract Surg. 2014;40:558–63.
Frings A, Vidic B, El-Shabrawi Y, Ardjomand N. Laser-assisted subepithelial keratomileusis with mitomycin C for myopic astigmatism ≥2.00 diopters using a Zeiss MEL 80 Excimer. Int Ophthalmol. 2014;34:225–33.
Qian Y, Huang J, Zhou X, Wang Y. Comparison of femtosecond laser small-incision lenticule extraction and laser-assisted subepithelial keratectomy to correct myopic astigmatism. J Cataract Refract Surg. 2015;41:2476–86.
Mastropasqua L, Toto L, Zuppardi E, Nubile M, Carpineto P, Di Nicola M, et al. Photorefractive keratectomy with aspheric profile of ablation versus conventional photorefractive keratectomy for myopia correction: six-month controlled clinical trial. J Cataract Refract Surg. 2006;32:109–16.
Dausch D, Dausch B, Wottke M, Sluyterman van Langeweyde G. Comparison of clinical outcomes in PRK with a standard and aspherical optimized profile: a full case analysis of 100 eyes with 1-year follow-up. Clin Ophthalmol. 2014;24:2251–60.
Meyer B, Sluyterman van Langeweyde G, Wottke M. Refractive outcomes of an advanced aspherically optimized profile for myopia corrections by LASIK: a retrospective comparison with the standard aspherically optimized profile. Clin Ophthalmol. 2015;23:379–92.
Reinstein DZ, Carp GI, Lewis TA, Archer TJ, Gobbe M. Outcomes for myopic LASIK with the MEL 90 excimer laser. J Refract Surg. 2015;31:316–21.
McAlinden C, Skiadaresi E, Moore JE. Visual and refractive outcomes following myopic laser-assisted subepithelial keratectomy with a flying-spot excimer laser. J Cataract Refract Surg. 2011;37:901–6.
Yee RW, Yee SB. Update on laser subepithelial keratectomy (LASEK). Curr Opin Ophthalmol. 2004;15:333–41.
Taneri S, Zieske JD, Azar DT. Evolution, techniques, clinical outcomes, and pathophysiology of LASEK: review of the literature. Surv Ophthalmol. 2004;49:576–602.
Estopinal CB, Mian SI. LASIK flap: postoperative complications. Int Ophthalmol Clin. 2016;56:67–81.
Lin N, Yee SB, Mitra S, Chuang AZ, Yee RW. Prediction of corneal haze using an ablation depth/corneal thickness ratio after laser epithelial keratomileusis. J Refract Surg. 2004;20:797–802.
Kim JK, Kim SS, Lee HK, Lee IS, Seong GJ, Kim EK, et al. Laser in situ keratomileusis versus laser-assisted subepithelial keratectomy for the correction of high myopia. J Cataract Refract Surg. 2004;30:1405–11.
Teus MA, de Benito-Llopis L, Sánchez-Pina JM. LASEK versus LASIK for the correction of moderate myopia. Optom Vis Sci. 2007;84:605–10.
de Benito-Llopis L, Teus MA, Sánchez-Pina JM, Hernández-Verdejo JL. Comparison between LASEK and LASIK for the correction of low myopia. J Refract Surg. 2007;23:139–45.
Yu M, Chen M, Wang B, Zou L, Zhu X, Dai J. Comparison of visual quality after SMILE and LASEK for mild to moderate myopia. J Refract Surg. 2015;31:795–800.
Kulkarni SV, AlMahmoud T, Priest D, Taylor SE, Mintsioulis G, Jackson WB. Long-term visual and refractive outcomes following surface ablation techniques in a large population for myopia correction. Invest Ophthalmol Vis Sci. 2013;54:609–19.
Al-Tobaigy FM. Efficacy, predictability, and safety of laser-assisted subepithelial keratectomy for the treatment of myopia and myopic astigmatism. Middle East Afr J Ophthalmol. 2012;19:304–8.
Fu D, Zhang ZY, Wang L, Zhou XT, Yu ZQ. Refractive regression and changes in central corneal thickness three years after laser-assisted Subepithelial keratectomy for high myopia in eyes with thin corneas: a retrospective study. Semin Ophthalmol. 2016;7:1–11.
Reilly CD, Panday V, Lazos V, Mittelstaedt BR. PRK vs LASEK vs Epi-LASIK: a comparison of corneal haze, postoperative pain and visual recovery in moderate to high myopia. Nepal J Ophthalmol. 2010;2:97–104.
Lee JB, Seong GJ, Lee JH, Seo KY, Lee YG, Kim EK. Comparison of laser epithelial keratomileusis and photorefractive keratectomy for low to moderate myopia. J Cataract Refract Surg. 2001;27:565–70.
Ghirlando A, Gambato C, Midena E. LASEK and photorefractive keratectomy for myopia: clinical and confocal microscopy comparison. J Refract Surg. 2007;23:694–702.
Wang D, Chen G, Tang L, Li Q. Comparison of postoperative pain following laser-assisted subepithelial keratectomy and transepithelial photorefractive keratectomy: a prospective, random paired bilateral eye study. Eye Sci. 2014;29:155–9.
Zou J, Zhou XT, Dai JH, Chu RY. Laser-assisted subepithelial keratectomy for low to moderate myopia. J Chinese Practical Ophthalmol. 2005;23:616–9.
Acknowledgements
Not applicable.
Funding
This work was supported by a grant from the National Natural Science Foundation of China: Grant No. 81570879 (Xingtao Zhou) and Grant No. 81500753 (Meiyan Li); and the ‘Yangfan’ Project of Science and Technology of Shanghai (Grant No. 15YF1401800) (Bing Qin).
Availability of data and materials
Available upon request from the co-first authors Yingjun Chen and Dong Yang.
Authors’ contributions
Concept and design (YC and XZ); analysis and interpretation (YC, DY and ML); writing the article (YC, and DY); critical revision of the article (YC, DY, TH, HX, ML and XZ); final approval of the article (YC, DY, TH, HX, ML and XZ); data collection (YC and TH); provision of materials, patients or resources (HX); statistical expertise (ML); literature research (DY); and administrative, technical or logistic support (YC, HT and HX). All authors have reviewed the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the Eye and ENT Hospital, Fudan University and was conducted with due regard to the tenets of the Declaration of Helsinki. Written informed consent was obtained from all participants.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Chen, Y., Yang, D., Han, T. et al. A pilot study: LASEK with the Triple-A profile of a MEL 90 for mild and moderate myopia. BMC Ophthalmol 17, 98 (2017). https://doi.org/10.1186/s12886-017-0493-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-017-0493-4