Abstract
Background
Good adherence to ocular hypotensive agents is important to control intraocular pressure and hence to prevent progressive glaucomatous optic nerve head damage. Periodic investigation of adherence is crucial in glaucoma treatment. The purpose of this study was to assess level of adherence to ocular hypotensive agents and to identify factors affecting adherence among glaucoma patients at a tertiary public eye care center.
Methods
The study was a hospital-based cross-sectional study that was conducted in Menelik II Referral Hospital from June 1, 2015 to July 31, 2015. A systematic random sampling technique was used to select 359 study participants from the source population. The study patients were interviewed and their medical charts were reviewed using a pretested structured questionnaire. Adherence was assessed using Morisky Medication Adherence Scale - 8 and adherence determinant factors were identified using multivariate binary logistic regression analysis. The association was declared statistically significant at p < 0.05.
Results
Among the 359 study glaucoma patients, 42.6 % were adherent to their prescribed hypotensive agents. Higher educational level (AOR = 4.60, 95 % CI: 1.01–21.03, p < 0.049), being self - employed (AOR = 6.14, 95 % CI: 1.37–27.50, p < 0.018) and taking lesser frequency of drops (AOR = 2.89, 95 % CI: 1.25–6.66, p < 0.013) were significantly associated with adherence, whereas being a farmer (AOR = 0.07, 95 % CI: 0.01–0.75, p < 0.028), having very low monthly family income (AOR = 0.22, 95 % CI: 0.06–0.77, p < 0.019) and self - purchasing of medications (AOR = 0.30, 95 % CI: 0.10–0.93, p < 0.036) were significantly associated with non-adherence.
Conclusions
The study has identified the adherence level to the prescribed ocular hypotensive agents to be sub-optimal and is influenced by different factors among glaucoma patients of the public tertiary center. We recommend glaucoma care providers to pay due attention on the importance of adherence.
Similar content being viewed by others
Background
Glaucoma is a progressive optic neuropathy which is caused by the death of the retinal ganglion cells and their fibers [1, 2]. It is a public health problem in developing countries, chiefly in sub-Saharan Africa, which is further compounded by poor awareness and low knowledge of glaucoma patients towards the disease [3, 4].
Adherence is the extent to which a patient’s behavior in taking medication corresponds with agreed recommendations from the provider [5]. Glaucoma medications are used over a long period or life-long that require long-term adherence to achieve the maximum intraocular pressure (IOP) lowering effect and prevent further progression of the disease [1, 6]. The major determinant for success in medical therapy of glaucoma is, therefore, the adherence of patients to their medications [7, 8].
Studies have documented that non-adherence is a significant problem among glaucoma patients which is further influenced by the asymptomatic nature of the disease [9, 10]. Reported adherence varies widely in different glaucoma studies [10] but a systematic review of 31 studies reported that 25 % of patients were found to be non-adherent [11]. Non-adherence potentially results in treatment failure, which is manifested as persistent elevation of IOP which, in turn, leads to progressive optic nerve damage and deterioration of the visual field [12–14]. Non-adherence is also associated with unnecessary prescription of drugs which add an extra burden on the health economy [15].
Glaucoma medication adherence could be measured through self-report, pharmacy refill reports, electronic monitoring and direct observation. To be clinically relevant, an ‘acceptable’ adherence level should be determined by its impact on clinical outcome [10]. Such evidence is lacking for ocular hypotensive agents due to the requirement for long-term follow-up and known inaccuracies in determining IOP control, visual field defects or optic nerve damage [16]. In the absence of any pre-existing gold standard measure, adherence to ocular hypotensive agents was measured using the Morisky Medication Adherence Scale – 8 (MMAS – 8) in this study [17]. The main purpose of this study was, therefore, to assess the level of adherence to ocular hypotensive agents and its determinant factors among glaucoma patients at a tertiary public referral hospital.
Methods
A hospital-based cross-sectional study was conducted at the glaucoma clinic of Menelik II Referral Hospital, Ethiopia from June 1, 2015 to July 31, 2015. At the clinic, glaucoma diagnosis was made based on the presence of elevated IOP (>20 mmHg), gonioscopy findings, characteristic optic nerve head damage (vertical cup-disc ratio greater than 0.4; diffuse or focal thinning or notching of the neuroretinal rim; or presence of asymmetry of the vertical cup-disc ratio of 0.2 between eyes) and/or visual field defect. The source population for this study was all glaucoma patients who received services at the glaucoma clinic of the hospital and the study population was all glaucoma patients who obtained services during the study period at the clinic.
Sample size determination and sampling technique
The sample size was calculated using a formula used to estimate the sample size for a single population [18]. Considering 1.96 for the standard normal variable with 5 % level of significance (α - value), 95 % confidence interval, 5 % margin of error and 10 % contingency, the sample size was calculated to be 359 from the 2120 study population. A systematic random sampling technique was employed to select the samples from the study population. The sampling interval was calculated to be 2120/359 = 6. A starting point was chosen randomly from numbers 1 to 6 and hence eligible individuals were chosen every sixth client at regular interval from the sampling frame.
Recruitment of research participants
Glaucoma patients enter the clinic’s triage and make a queue in the waiting area. The ophthalmic nurses measure both visual acuity and IOP and register these findings on the patient’s chart prior to getting services from physicians. While the patients were waiting at a waiting area during their appointment day, patients were screened for eligibility based on the inclusion and exclusion criteria. The study participants, who were selected from the sampling frame, were briefed about the purpose of the study and then requested for willingness for an interview at a nearby separate room.
Inclusion and exclusion criteria
Patients who were 18 years old and above, with the diagnosis of glaucoma or ocular hypertension, were on ocular hypotensive agents for one or both eyes for at least 6 months, had regular follow-up and had not undergone either laser or glaucoma surgery in the previous 3 months were enrolled in the study. Glaucoma patients with post-operative follow-up, on systemic glaucoma drugs only, on anti-inflammatory or anti-infective eye drops only, who were not willing to give informed written consent and those enrolled in the pretest were excluded from the study.
Data collection and analysis
Data were collected by three trained ophthalmic nurses through a face-to-face interview to collect socio-demographic characteristics (age, sex, educational level, residence, and occupation), medication-related characteristics (number, type, and side effects of medications) and adherence level. Medical charts of the patients were reviewed to abstract the type and severity of glaucoma, and visual acuity. Adherence to ocular hypotensive agents was measured using MMAS–8 which is a medication-taking behavior scale. MMAS–8 is the latest version of the scale and has a good internal consistency (Cronbach’s α = 0.83) [17]. This scale has been used for a wide variety of chronic medical conditions [19]. The study participant was deemed to be adherent when the MMAS – 8 score was < 2 and non-adherent when the MMAS – 8 score was ≥ 2 [20].
The questionnaire was translated to Amharic, a national language, and then translated back to English. To maximize quality of the data, the tool was pre-tested in 5 % of the study subjects (18 patients). The filled-in forms were checked for completeness of data and cleaned prior to data entry. Data were entered using Epi Info™ version 3.5.3. Data analysis was carried out using Statistical Package for Social Sciences (SPSS®Statistics) program version 21 (Chicago, IL, U.S.A.). Descriptive statistics such as frequency, percentage, mean and standard deviation were also employed to summarize patient’s characteristics.
Univariate binary logistic regression analysis was performed to assess the association of the variables to adherence. From the result of the univariate analysis, variables with p < 0.2 were selected for multivariate binary logistic regression analysis which was used to assess factors affecting adherence and to estimate the odds ratios (OR), 95 % confidence intervals (CI) and p - values. The association was declared statistically significant at p < 0.05.
Results
The socio-demographic and clinical characteristics of the study participants are summarized in Table 1. Among 359 eligible patients, about half of the patients (n = 181, 50.4 %) were in the age group of 61–80 years old (mean: 60.91, SD ± 12.34 years; range: 18 to 88 years). Large number of the patients were males (n = 247, 69.0 %). Concerning the educational level, 229 (63.9 %) patients had a lower education (elementary school and/or below). Majority of the study subjects were residing in urban areas (n = 322, 89.7 %) and about one-third (n = 115, 32.0 %) of the patients were retired (Table 1).
According to the medical records of the patients, the most prevalent type of glaucoma diagnosis was pseudoexfoliative glaucoma which accounted for 40.5 % (n = 138) followed by primary open angle glaucoma (n = 93, 27.3 %). The stage of glaucoma, based on the Canadian glaucoma strategy classification [21], was recorded as early, moderate and advanced in 32 (11.9 %), 173 (64.1 %) and 65 (24.1 %) patients respectively (Table 1).
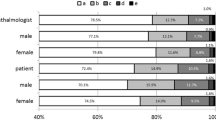
Almost all (n = 350, 97.5 %) of the patients were using one and/or two medications as depicted in Table 2. The combination of eye drops accounted for about half (n = 185, 51.5 %) of the prescribed medications followed by timolol as a monotherapy (n = 158, 44.0 %). Regarding eye drop administration, 123 (32.8 %) patients admitted that they were waiting more than five minutes to administer the second or consecutive drop. Above half (n = 200, 56.0 %,) of the patients also reported that they did not experience side effects (such as redness, itching, burning and blurring of vision) immediately after starting the medications (Table 2). According to the international council of ophthalmology’s classification of visual acuity [22], about one-third of the patients had (near-) normal vision (n = 122, 34.3 %), low vision (n = 130, 36.6 %) and (near-) blindness (n = 115, 32.3 %) on the better eye (Fig. 1). Regarding the level of adherence, assessment of patients’ response to the MMAS-8 revealed that 42.6 % (n = 153) of the study patients were adherent to their glaucoma medications (Fig. 2 and Table 3).
The results of logistic regression analysis for factors associated with medication adherence are summarized in Table 4. Variables with p - value less than 0.2 (marital status, educational level, occupation, monthly family income, follow-up, number of medications, type of medications, frequency of eye drop, time elapsed to administer the second drop, side effects, purchasing of the medications, and getting information about eye drop administration from the physicians) were incorporated into the multivariate logistic regression analysis (Table 4).
In this study, educational level, occupation, monthly family income, the frequency of eye drops and financial source to obtain the medications were found to be potential predictors of adherence to ocular hypotensive agents. Accordingly, the odds of being adherent for patients with higher educational level (diploma and/or above) were nearly five-fold (AOR = 4.60, 95 % CI: 1.01–21.03, p < 0.049) more compared to patients with lower educational status (Grade 1–8).
The odds of being adherent for farmer patients were 93 % (AOR = 0.07, 95 % CI: 0.01–0.75, p < 0.028) less compared to patients who were retired. In contrary to this, patients who were self-employed were approximately six-fold (AOR = 6.14, 95 % CI: 1.37–27.50, p < 0.018) more odds of being adherent compared to those participants who were retired. The odds of being adherent for patients with very low monthly family income were 78 % (AOR = 0.22, 95 % CI: 0.06–0.77, p < 0.019) less compared to patients with high monthly family income. It was also found that the odds of being adherent for patients who were taking fewer daily doses (two times per day) were approximately three-fold (AOR = 2.89, 95 % CI: 1.25–6.66, p < 0.013) more compared to those who were taking more frequent eye drops (four times per day). The odds of being adherent for patients who bought the medications by themselves were about 70 % (AOR = 0.30, 95 % CI: 0.10–0.93, p < 0.036) less compared to patients who obtained the medications free of charge.
Discussions
The study has assessed adherence to ocular hypotensive agents among glaucoma patients in Menelik II Referral Hospital. One hundred fifty-three (42.6 %) patients were found to be adherent which was similar to other studies that reported 40.0–45.0 % in USA [23–25]. This similarity might be evident owing to the use of a questionnaire for interviewing the patients. On the other hand, the level of adherence was found to be lower than 56.0 % in Greece [12], 72.1 % in Canada [26] and 72.7 % in Dutch [27] but higher than 30.7 % in England [28]. The wide variation might be partly attributable to inconsistency in the definition of non-adherence, subjectivity and heterogeneity in the assessment methods as well as differences in patient groups [29].
During multivariate logistic regression analysis, patients with higher educational level were more likely to be adherent compared to patients with lower educational level. This finding was similar to studies done in Canada [26], USA [30, 31] and Germany [32]. Patients who are more literate might have an updated information on the disease and its progression, and have a better understanding of the importance of adherence to the medications. On the other point, self-employed patients were more likely to be adherent compared to retired patients as the former might afford the medications easily. Moreover, retired patients are usually older than self-employed patients and might have greater cognitive and physical impairment associated with aging.
In contrary to the above, farmer patients were less likely to be adherent compared to retired patients. This could be illustrated as the majority of the farmers in developing countries like Ethiopia are illiterate with limited knowledge of the disease and have lower economic status.
Patients who applied eye drops less frequently were more likely to be adherent compared to patients who applied eye drops more frequently which corresponded with a previous study [12]. This is evident by the fact that increased daily frequency of eye drop is associated with increased complexity of the regimen. However, more emphasis should be given to the clinical importance of frequency of administration and available dosage preparations.
Patients with low monthly income were less likely to be adherent compared to patients with high monthly income. This finding was related to a previous study that revealed unaffordability considerably affects adherence [33]. Besides this, patients who purchased ocular hypotensive drops by themselves were less likely to be adherent compared to patients who obtained their medications free of charge. The plausible reason might also be related to an affordability issue of the medications.
In this study, age and sex of the participants were not significantly associated with the medication adherence during the multivariate logistic regression analysis. The absence of a relationship between adherence and most of the socio-demographic factors was supported by the previous findings [12, 23, 27, 29, 32, 34]. The absence of this association might be related to the characteristics of patients. The patients in the present study had a long history of glaucoma (for an average of 5.6 years) and a long duration of taking medication (mean duration of taking hypotensive agents was 5.35 years). Therefore, demographic factors might have less influence on the adherence behavior of the study participants.
Multivariate analysis of this study also indicated that medication adherence was not significantly associated with the type and severity of glaucoma, side effects (even though side effects were reported most commonly amongst those who were non-adherent), duration of glaucoma diagnosis, obtaining information about drug administration, intraocular pressure, and visual acuity. These results were comparable with different studies [12, 27, 33–35]. It remains unclear whether these clinical parameters might influence the adherence behavior of glaucoma patients in general.
The study had certain limitations. The cross-sectional nature of the study did not allow a follow-up, which could have provided a better design for identifying the factors associated with adherence. The results were also relied on patients’ response. It is known that patients tend to overestimate their ability to adhere to their therapy which necessities further objective assessment tools such as electronic medication monitoring system or biological assays in the future.
Conclusion
The study has identified the adherence level to the prescribed ocular hypotensive agents to be sub-optimal according to the Morisky Medication Adherence Scale-8, and influenced by different factors among glaucoma patients of the public tertiary center. We recommend glaucoma care providers to pay due attention to the importance of adherence and influencing factors to the prescribed medications.
Abbreviations
AOR, adjusted odds ratio; CI, confidence interval; COR, crude odds ratio; IOP, intraocular pressure; MMAS – 8, Morisky Medication Adherence Scale – 8; SD, standard deviation
References
McVeigh KA, Vakros G. The eye drop chart: A pilot study for improving administration of and compliance with topical treatments in glaucoma patients. Clin Ophthalmol. 2015;9:813–9.
Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;21:2081–90.
Kyari F, Abdull MM, Bastawrous A, Gilbert CE, Faal H. Epidemiology of glaucoma in sub-Saharan Africa: prevalence, incidence and risk factors. Middle East Afr J Ophthalmol. 2013;20:111–25.
Alemu AM, Nelson LA, Kruft B, Stewart JA, Stewart WC. Epidemiology of glaucoma in central Ethiopia. Int J Ophthalmol. 2009;2:168–73.
World Health Organization (WHO). Adherence to long-term therapies. Evidence for action. Geneva: World Health Organization; 2003.
Lee PP, Walt JW, Rosenblatt LC, Siegartel LR, Stern LS. Association between intraocular pressure variation and glaucoma progression: data from a United States chart review. Am J Ophthalmol. 2007;144:901–7.
Robert NW, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: a review. JAMA. 2014;311:1901–11.
Tsai T, Robin AL, Smith JP. An evaluation of how glaucoma patients use topical medications: a pilot study. Trans Am Ophthalmol Soc. 2007;105:29–35.
Schwartz GF. Adherence and persistence in glaucoma. In: Grehn F, Stamper R, editors. Glaucoma. Berlin: Heidelberg Platz; 2006. p. 91–105.
Olthoff CM, Schouten JS, van de Borne B, Webers CA. Noncompliance with ocular hypotensive treatment in patients with glaucoma or ocular hypertension an evidence - based review. Ophthalmology. 2005;112:953–61.
Lu VH, Goldberg I, Lu CY. Use of glaucoma medications: State of the science and directions for observational research. Am J Ophthalmol. 2010;150:569–74.
Konstas AGP, Maskaleris G, Gratsonidis S, Sardelli C. Compliance and viewpoint of glaucoma patients in Greece. Eye. 2000;14:752–6.
Stewart WC, Konstas AGP, Pfeiffer N. Patient and ophthalmologist attitudes concerning compliance and dosing in glaucoma treatment. J Ocular Pharmacol Ther. 2004;20:461–9.
Gupta R, Patil B, Shah BM, Bali SJ, Mishra SK, Dada T. Evaluating eye drop instillation technique in glaucoma patients. J Glaucoma. 2012;21:189–92.
Reeder CE, Franklin M, Bramley TJ. Managed care and the impact of glaucoma. Am J Manag Care. 2008;14:5–10.
Kulkarni SV, Damji KF, Buys YM. Medical management of primary open-angle glaucoma: Best practices associated with enhanced patient compliance and persistency. Patient Prefer Adherence. 2008;2:303–14.
Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive Validity of a Medication Adherence Measure in an Outpatient Setting. J Clin Hypertens. 2008;10:384–54.
Daniel WW, Cross LC. Biostatistics: A foundation for analysis in the health sciences. 8th ed. Hoboken, New Jersey: John Wiley and Sons Inc; 2005. p. 158–65.
Pedersini R, Vietri J. Comparison of the 4 - item and 8 - item Morisky Medication Adherence Scale in patients with type 2 diabetes. Kantar Health: Montreal; 2014.
Muntner P, Joyce C, Holt E, He J, Morisky D, Webber LS, et al. Defining the minimal detectable change in scores on the eight - item Morisky Medication Adherence Scale. Ann Pharmacother. 2011;45:569–75.
LeBlanc R. Canadian Glaucoma Strategy Forum. A Canadian glaucoma strategy. Can J Ophthalmol. 2007;42:60–5.
International Council of Ophthalmology (ICO). Visual Standards: Aspects and Ranges of Vision Loss. Sydney: International Council of Ophthalmology; 2002.
Okeke CO, Quigley HA, Jampel HD, Ying GS, Plyler RJ, Jiang Y, et al. Adherence with topical glaucoma medication monitored electronically the Travatan Dosing Aid study. Ophthalmology. 2009;116:191–9.
Stryker JE, Beck AD, Primo SA, Echt KV, Bundy L, Pretorius GC, et al. An exploratory study of factors influencing glaucoma treatment adherence. J Glaucoma. 2010;19:66–72.
Sleath B, Blalock S, Covert D, Stone JL, Skinner AC, Muir K, et al. The relationship between glaucoma medication adherence, eye drop technique, and visual field defect severity. Ophthalmology. 2011;118:2398–402.
Kholdebarin R, Campbell RJ, Jin YP, Buys YM. Multicenter study of compliance and drop administration in glaucoma. Can J Ophthalmol. 2008;43:454–61.
Olthoff CM, Hoevenaars JG, van de Borne B, Webers CA, Schouten JS. Prevalence and determinants of non-adherence to topical hypotensive treatment in Dutch glaucoma patients. Graefes Arch Clin Exp Ophthalmol. 2009;247:235–43.
Richardson C, Brunton L, Olleveant N, Henson DB, Pilling M, Mottershead J, et al. A study to assess the feasibility of undertaking a randomized controlled trial of adherence with eye drops in glaucoma patients. Patient Prefer Adherence. 2013;7:1025–39.
Cate H, Bhattacharya D, Clark A, Holland R, Broadway DC. Patterns of adherence behaviour for patients with glaucoma. Eye. 2013;27:545–53.
Boland MV, Chang DS, Frazier T, Plyler R, Friedman DS. Electronic monitoring to assess adherence with once - daily glaucoma medications and risk factors for nonadherence: The automated dosing reminder study. JAMA Ophthalmol. 2014;132:839–44.
Dreer LE, Girkin C, Mansberger SL. Determinants of medication adherence to topical glaucoma therapy. J Glaucoma. 2012;21:234–40.
Welge-lussen U, Weis S, Yu AL. Assessing the adherence behavior of glaucoma patients to topical eye drops. Patient Prefer Adherence. 2015;18:17–23.
Friedman DS, Okeke CO, Jampel HD, Ying GS, Plyler RJ, Jiang Y, et al. Risk factors for poor adherence to eye drops in electronically monitored patients with glaucoma. Ophthalmology. 2009;116:1097–105.
Ung C, Murakarui Y, Zhang E, Alfaro T, Zhang M, Seider MI, et al. Glaucoma severity and medication adherence in a county hospital population. Ophthalmology. 2013;120:1150–147.
Hoevenaars JG, Schouten JS, van den Borne B, Beckers HJ, Webers CA. Will improvement of knowledge lead to improvement of compliance with glaucoma medication? Acta Ophthalmol. 2008;86:849–55.
Acknowledgements
The authors would like to acknowledge all participants of the study. Dr. Yilkal Adamu and staff members of glaucoma clinic of Menelik II Referral Hospital are thanked for their unreserved support. Mekelle University is acknowledged for granting study leave to the first author.
Funding
The study was partly supported by Office of the Vice President for Research and Technology Transfer of the Addis Ababa University. The funding body did not have any role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
The datasets supporting the conclusions of the study are available publicly in server of Addis Ababa University as MSC Thesis of graduate student. Any additional data will be available on request.
Authors’ contributions
TM designed, conducted the study and prepared the manuscript. WS and ATG supervised the study and reviewed the manuscript. All authors read and approved the final manuscript.
Author’s information
TM is a lecturer of pharmacotherapy and clinical pharmacist at the Department of Pharmacy, College of Health Sciences, Mekelle University. ATG is an assistant professor and glaucoma consultant at the Department of Ophthalmology, School of Medicine, College of Health Sciences, Addis Ababa University. WS is an associate professor of pharmacology at the Department of Pharmacology and Clinical Pharmacy, School of Pharmacy, College of Health Sciences, Addis Ababa University.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable
Ethics approval and consent to participate
The study was undertaken after obtaining ethical clearance from School of Pharmacy’s Ethical Review Committee, Research and Publication Committee of the Department of Ophthalmology (Addis Ababa University) and the Research Committee of Addis Ababa City Health Bureau. Written informed consent was also obtained from patients. The study also adhered to the declarations of Helsinki.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Mehari, T., Giorgis, A.T. & Shibeshi, W. Level of adherence to ocular hypotensive agents and its determinant factors among glaucoma patients in Menelik II Referral Hospital, Ethiopia. BMC Ophthalmol 16, 131 (2016). https://doi.org/10.1186/s12886-016-0316-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-016-0316-z