Abstract
Objective
The aim of this study was to investigate the incidence and risk factors of new-onset hypopituitarism after gamma knife radiosurgery (GKRS) for pituitary adenomas in a single center.
Methods
In this retrospective study, 241 pituitary adenoma patients who underwent GKRS from 1993 to 2016 were enrolled. These patients had complete endocrine, imaging, and clinical data before and after GKRS. The median follow-up time was 56.0 (range, 12.7–297.6) months.
Results
Fifty patients (20.7%) developed new-onset hypopituitarism after GKRS, including hypogonadism (n = 22), hypothyroidism (n = 29), hypocortisolism (n = 20), and growth hormone deficiency (n = 4). The median time to new-onset hypopituitarism was 44.1 (range, 13.5–141.4) months. The rates of new-onset hypopituitarism were 7%, 16%, 20%, 39%, and 45% at 1, 3, 5, 10, and 15 years, respectively. For those patients treated with a single GKRS, sex (p = 0.012), suprasellar extension (p = 0.048), tumor volume (≥ 5 cm3) (p < 0.001), tumor progression (p = 0.001), pre-existing hypopituitarism (p = 0.011), and previous surgery (p = 0.009) were significantly associated with new-onset hypopituitarism in univariate analysis. In the multivariate analysis, tumor volume (≥ 5 cm3) and tumor progression were associated with new-onset hypopituitarism (hazard ratio [HR] = 3.401, 95% confidence interval [CI] = 1.708–6.773, p < 0.001 and HR = 3.594, 95% CI = 1.032–12.516, p = 0.045, respectively). For patients who received 2 or more times GKRS, no risk factors associated with new-onset hypopituitarism were found.
Conclusion
New-onset hypopituitarism was not uncommon after GKRS for pituitary adenomas. In this study, large tumor volume (≥ 5 cm3) and tumor progression were associated with new-onset hypopituitarism after a single GKRS.
Similar content being viewed by others
Introduction
Pituitary adenomas (PAs) are one of the most common intracranial neoplasms, accounting for 10–20% of diagnosed brain tumors [1]. According to secreting biologically active hormones, PAs can be classified as functioning PAs (FPAs) and nonfunctioning PAs (NPFAs). For most NFPAs and FPAs (except prolactinomas), surgical resection is still the first-line treatment option [2]. However, about 20% of patients developed tumor recurrent after gross-total resection for NFPAs [3,4,5,6,7]. For subtotal resection without adjuvant radiotherapy, the rate of tumor progression could range from 50 to 60% [4,5,6,7]. Thus, postsurgical radiotherapy is indicated for postsurgical residual or recurrent NFPAs. Furthermore, initial gamma knife radiosurgery (GKRS) can be an alternative treatment for selected NFPA patients with comorbidities, documented growth small tumors, cavernous sinus invasion, or advanced age [8,9,10]. Medical therapy with dopamine agonists (DAs) is currently the preferred first-line treatment option for prolactinomas [11]. For DA-resistant or intolerant prolactinomas, GKRS is one of the effective treatment options, with hormonal remission rate of 4.5–83% [12,13,14].
GKRS, which has advantages of providing highly precise, better conformity, and focused delivery of radiation, is the most commonly used radiation technique in the treatment of PAs. Hypopituitarism is one of the most common complications of GKRS [15]. Its incidence ranged from 12.3 to 39.0% [9, 16,17,18]. Potential risk factors included tumor volume, prior radiation therapy, mean dose to the pituitary gland, margin dose, and suprasellar extension [9, 16, 19,20,21]. However, the incidence and risk factors of hypopituitarism after GKRS are still uncertain.
We have more than 26 years of experiences in using Gamma Knife (Elekta, Stockholm, Sweden) for PAs at the Second Affiliated Hospital of Guangzhou Medical University since 1993. Thus, in this large single-center retrospective study, we aimed to investigate the incidence and risk factors of hypopituitarism after GKRS for PAs.
Patients and methods
Patients
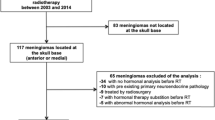
Between December 1993 and December 2016, 241 patients with complete clinical and endocrine evaluation before and after GKRS for PAs at the Department of Radiotherapy, Second Affiliated Hospital of Guangzhou Medical University, were enrolled in our study. Study inclusion criteria: (1) magnetic resonance imaging (MRI) or surgical findings suggested the diagnosis of pituitary adenomas; (2) complete clinical and endocrinological evaluations before and after GKRS; (3) follow-up ≥ 12 months; (4) at least one pituitary axis intact.
Informed consent was obtained from each participant. All procedures were approved by the institutional committee of the Second Affiliated Hospital of Guangzhou Medical University.
Endocrine and imaging evaluations
To assess endocrine function in patients both pre- and post-GKRS, various serum hormone levels were measured, including free triiodothyronine (FT3), free thyroxine (FT4), thyrotropin (also known as thyroid-stimulating hormone, TSH), cortisol, adrenocorticotropic hormone, prolactin, growth hormone (GH), insulin-like growth factor-1 (IGF-1), follicle-stimulating hormone (FSH), luteinizing hormone (LH), testosterone, and estradiol. Hypothyroidism criteria included a low FT4 in combination with low, normal, or slightly elevated TSH levels. Hypocortisolism was identified by a morning (08:00) cortisol level under 4 µg/dL or an insufficient cortisol increase (below 20 µg/dL) during a stimulation or insulin tolerance test. For men, hypogonadism was indicated by low serum testosterone levels without concurrent elevated levels of LH and FSH. In women, hypogonadism was characterized by amenorrhea with low serum estradiol and low gonadotropin levels in premenopausal females, while menopausal women exhibited no high gonadotropin (LH and FSH) levels [22, 23]. Growth hormone (GH) deficiency was judged based on a subnormal response to the insulin tolerance test (less than 5 µg/L) or a low IGF-1 adjusted for age and sex. New-onset hypopituitarism post-GKRS was defined by a newly detected deficiency in any hormonal axis or the necessity for hormone replacement therapy.
Imaging assessments were conducted for the entire cohort of 241 patients using established MRI protocols for the pituitary gland before and after Gamma Knife radiosurgery (GKRS). Measurements of the tumor dimensions were recorded in three perpendicular planes: transverse (TR), anteroposterior (AP), and craniocaudal (CC). Tumor volumes were calculated employing the formula: V = (π × [TR × AP × CC]) / 6 [24]. Tumor progression was defined as tumor volume increased at least 20% or any tumor regrowth. In contrast, tumor shrinkage was defined as tumor volume reduction at least 20% without any tumor regrowth. Tumors were considered stable if the volume change was within 20%. Parasellar invasion corresponded to a Knosp grade of 3 or 4, while suprasellar extension was described as a tumor presence within 2 mm of the optic nerve and chiasm.
GKRS technique
The Model B Leksell Gamma Knife Unit was utilized prior to April 2014 and then exchanged with the Perfexion Unit (Elekta Instrument, Inc., Stockholm, Sweden). Anesthesia was administered locally for placement of the stereotactic Leksell frame. Subsequent to the installation of the frame, a thin-slice MRI with contrast material was conducted targeting the sella. The GKRS treatment planning was collaboratively conducted by a medical physicist, radiation oncologist, and neurosurgeon. All patients underwent single-fraction GKRS in the study. The dose selection for GKRS primarily relied on the tumor type, tumor size, distance from the optic nerve and chiasm, and past radiotherapy. In order to achieve superior conformality, small collimators of sizes 4 mm and 8 mm were predominantly utilized.
Statistical analysis
All statistical analyses were performed by SPSS software version 21.0 (IBM Corp., Armonk, NY, USA). Univariate and multivariate analyses of the potential risk factors (age, sex, parasellar invasion, suprasellar extension, previous surgery, tumor margin dose, tumor type, tumor volume, pre-existing hypopituitarism before GKRS, tumor progression after GKRS, and frequency of GKRS) associated with new-onset hypopituitarism were performed by log-rank test statistics and a step-forward likelihood ratio method of Cox proportional hazard models, respectively. Kaplan–Meier curve was plotted for new-onset hypopituitarism. A p-value of < 0.05 was considered statistically significant.
Results
Population and characteristics
Overall, 241 patients were enrolled in this study. The patient population consisted of 108 men (44.8%) and 133 women (55.2%) with a median age of 42.7 (range, 7.2–75.5) years. The median follow-up was 56.0 (range, 12.7–297.6) months. The median tumor volume at GKRS was 2.14 (range, 0.02–74.49) cm3. There were 154 (63.9%), 47 (19.5%), 38 (15.8%), and 2 (0.8%) cases of NFPAs, prolactinomas, acromegaly, and Cushing diseases, respectively. Prior to GKRS, 73 (30.3%) patients had undergone one surgical resection, 16 (6.6%) had two resections, and 3 (1.2%) had three. Two hundred and eight patients had undergone a single GKRS. Thirty (12.4%) and 3 (1.2%) patients had undergone 2 or more times of GKRS for residual or regrowth tumor respectively. Moreover, 65 patients (27.0%) had parasellar invasion and 155 (64.3%) had suprasellar extension. Seventeen patients (7.1%) occurred tumor progression. Tumors shrank or remained stable in 224 patients (92.9%). In this study, all patients undergone single-session GRKS, the median tumor margin radiation dose was 14.0 (range, 8.0–23.6) Gy. The median maximum radiation dose was 33.3 (range, 20.0–66.6) Gy. The median prescription isodose was 40% (range, 25–60%). The baseline characteristics of these patients are summarized in Table 1.
Endocrine outcomes after GKRS
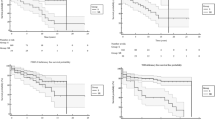
In this study, 119 patients presented with hypopituitarism prior to GKRS, including hypogonadism (n = 104), hypothyroidism (n = 30), hypocortisolism (n = 19) and GH deficiency (n = 5). One hundred and twenty-two patients presented with normal endocrine function before GKRS. Finally, 50 patients (20.7%) developed new-onset hypopituitarism after GKRS in the entire series, including hypogonadism (n = 22), hypothyroidism (n = 29) and hypocortisolism (n = 20) (Table 2). Of the 50 patients, 14 patients exhibited multi-axis hormone deficits. The median time to the occurrence of new-onset hypopituitarism was 44.1 (range, 13.5–141.4) months. The rates of new-onset hypopituitarism were 7%, 16%, 20%, 39%, and 45% at 1, 3, 5, 10, and 15 years, respectively (Fig. 1). For those patients who had undergone a single GKRS, 42 patients (20.2%) developed new-onset hypopituitarism, the rates of new-onset hypopituitarism were 8%, 17%, 20%, 40%, and 44% at 1, 3, 5, 10, and 15 years, respectively. For those treated with 2 or more times GKRS, 8 patients (24.2%) developed new-onset hypopituitarism, the rates of new-onset hypopituitarism were 3%, 11%, 15%, 36%, and 49% at 1, 3, 5, 10, and 15 years, respectively.
For those treated with a single GKRS, in the univariable analysis, sex (p = 0.012), suprasellar extension (p = 0.048), tumor volume (≥ 5 cm3) (p < 0.001), tumor progression (p = 0.001), pre-existing hypopituitarism (p = 0.011), and previous surgery (p = 0.009) were significantly associated with new-onset hypopituitarism. In the multivariate analysis, tumor volume (≥ 5 cm3) and tumor progression were independent risk factors associated with new-onset hypopituitarism (hazard ratio [HR] = 3.401, 95% confidence interval [CI] = 1.708–6.773 and HR = 3.594, 95% CI = 1.032–12.516, respectively) (Table 3; Figs. 2 and 3). For patients who received 2 or more times GKRS, no risk factors associated with new-onset hypopituitarism were found (Table 4). Besides, the incidence of new-onset hypopituitarism did not differ between a single GKRS and 2 or more times GKRS (p = 0.857).
Discussion
The overall prevalence of hypopituitarism was 29 per 100,000 cases based on a previous survey [25]. The mechanism of hypopituitarism included dysfunction of the pituitary gland or hypothalamic damage. Various diseases may cause hypopituitarism. The most common causes of primary hypopituitarism are PAs and complications of surgery or radiation therapy for PAs [15]. PAs can cause hypopituitarism because of tumor growth and compression of pituitary gland and stalk. The pituitary gland and hypothalamus can be damaged by pituitary surgery or radiotherapy. One or more factors can result in hypopituitarism. Patients who develop hypopituitarism have a poor quality of life, high risk of morbidity and even mortality [26, 27].
Table 5 summarizes recent literatures describing GKRS for PAs. Previous studies reported a highly heterogeneous incidence rate of hypopituitarism after GKRS for PAs, which ranged from 12.3 to 39% [9, 16,17,18,19,20,21, 28, 29]. Sex, tumor volume, suprasellar extension, prior radiation, mean dose to the pituitary gland, isodose line, margin dose, and maximum dose were reported to be significantly associated with hypopituitarism after GKRS for PAs [9, 16,17,18,19,20,21, 28]. According to Pollock et al. [28], the incidence of new-onset hypopituitarism was 27% based on 62 PAs treated with GKRS. In this study, hypopituitarism was relatively higher for patients with a tumor volume > 4.0 cm3. Sheehan et al. [20] investigated 512 PA patients undergoing GKRS and reported that new-onset hypopituitarism following GKRS was noted in 21% of the patients and prior radiation therapy and greater tumor margin doses were predictive of new-onset hypopituitarism. Xu et al. [21] examined a total of 262 PA patients treated with stereotactic radiosurgery (SRS) and reported a new-onset hypopituitarism rate of 30%. This study investigated that suprasellar extension and higher margin dose (> 16 Gy) increased the risk of hypopituitarism after GKRS. Sicignano et al. [16] enrolled 130 PA patients and reported a new-onset hypopituitarism rate of 12.3%. In this study, they identified that dosimetric (the mean dose and amount of healthy tissue within the high-dose region) parameters were correlated with the risk of new-onset hypopituitarism. In another study, Lee et al. [9] reported that 24% of PAs caused new-onset hypopituitarism, and patients who had received a tumor margin dose of > 18 Gy as well as a maximum dose of > 36 Gy had a higher risk for hypopituitarism. Graffeo et al. [30] found that higher mean pituitary gland dose (> 11 Gy) was associated with new-onset hypopituitarism after SRS. From a multicenter and international study, Cordeiro et al. [17] revealed that 248 of 1023 (24.2%) patients developed new-onset hypopituitarism and they found that a lower isodose line (< 50%) was an independent predictor of new-onset hypopituitarism (p = 0.001, HR = 1.38).
In the present study, we described 241 patients with PA treated with GKRS, in which new-onset hypopituitarism occurred in 50 patients (20.7%). This incidence was comparable with previous published data of hypopituitarism following GKRS (Table 5). In our series, the median time for the occurrence of hypopituitarism after GKRS was 44.1 (range, 13.5–141.4) months, which was apparently similar with that in a previous study. Since 33 cases (13.7%) received two or more times GKRS in the study, we conducted subgroup analyses for a single GKRS and multiple GKRS treatments. In a single GKRS group, our multivariate analysis demonstrated that tumor volume (≥ 5 cm3) and tumor progression were significantly associated with new-onset hypopituitarism after GKRS. New-onset hypopituitarism occurs in 15.9% of patients with tumors < 5 cm3 relative to 43.8% of patients with tumors > 5 cm3. These data suggested that large tumors were associated with high risk for new-onset hypopituitarism after GKRS for PAs. In large tumors, the pituitary gland is compressed more seriously than those in small tumors. Besides, large tumor volumes may make it difficult to deliver an ideal radiation dose to the target volume. The radiation dose and volume of surrounding structures including the pituitary gland, pituitary stalk, and hypothalamus were increased, which might be at risk for new-onset hypopituitarism after GKRS. Tumor progression after GKRS was also a risk factor for new-onset hypopituitarism in a single GKRS group in this study. This may be related to the aggravation of compression on the normal pituitary gland after tumor progression. Among the 4 patients with tumor progression, 3 (75%) developed new-onset hypopituitarism. In the 3 cases of tumor progression and new-onset hypopituitarism, one patient’s tumor progression and new-onset hypopituitarism were detected simultaneously, while the new-onset hypopituitarism in the other 2 cases occurred after the tumor progression. In contrast, only 19.1% of patients with shrinking or stable tumors experienced new-onset hypopituitarism. Although the number of cases in the tumor progression group is small, with only 4 cases, this could limit statistical analysis, but the issue of new-onset hypopituitarism due to tumor progression after GKRS treatment cannot be overlooked. Insufficient GKRS dosage can lead to tumor progression and subsequent pituitary dysfunction, while excessive GKRS dosage may also result in hypopituitarism. How to balance GKRS dosage, local tumor control, and new-onset hypopituitarism warrants careful consideration. For patients (n = 33) who received 2 or more times GKRS, no risk factors associated with new-onset hypopituitarism were found. Besides, the incidence of new-onset hypopituitarism did not differ between a single GKRS and 2 or more times GKRS. This may be related to the small number of cases in the multiple GKRS group.
Three-dimensional conformal radiotherapy, intensity-modulated radiotherapy, and fractionated stereotactic radiotherapy are common radiation techniques. However, no clinical trials have compared the efficacy and safety of conventional radiotherapy with SRS. Previous studies reported that new-onset hypopituitarism after conventional radiotherapy can occur in up to 80% of the cases in 10 years [31]. In most studies, the incidence of hypopituitarism after GKRS for PAs ranged from 12.3 to 39% [9, 16,17,18,19,20,21, 28, 29]. Conventional radiotherapy is less precise than SRS, which increases the radiation volume to the pituitary gland, pituitary stalk, and hypothalamus. Therefore, it may convey more risk of adverse effects. Furthermore, SRS has a better dose conformity with only single fraction and is more convenient than conventional radiotherapy. Thus, SRS has been the most commonly used radiation technique in many centers and is an essential part in the treatment of PAs.
In our experience, 20.7% of patients with PAs developed new hypopituitarism after GKRS. Hypopituitarism is not an uncommon complication of GKRS. New hypopituitarism may occur several years after GKRS. Large tumor volume (≥ 5 cm3) and tumor progression after GKRS are risk factors for new-onset hypopituitarism after a single GKRS. Thus, regular endocrine follow-up is necessary. Since tumor progression can also lead to pituitary dysfunction, clinicians must carefully weigh the issues of local tumor control and pituitary dysfunction when determining the appropriate prescription dose, in order to make better clinical decisions. Although uncorrected hypopituitarism is related with early mortality and morbidity, with the help of endocrinologist, it can be treated with hormone replacement.
Study limitations
This study has several limitations. First, this was a single-center retrospective study that was stopped in 2016, and thereby reflected treatment and selection biases. Second, because many patients came from a long distance from nationwide, endocrine tests and MRI evaluations were missing, thus, only 241 patients were included according the inclusion criteria in this study, which might lead to a selection bias. Third, the number of patients is relatively small, and this may limit the statistical power. Four, for some patients located far from the center, endocrine evaluations were mainly taken in the local hospital; thus, there might be slight variation in the definition of hypopituitarism. Finaly, dosimetric parameters on the pituitary stalk or gland were associated with the risk of hypopituitarism after GKRS, however, these dosimetric parameters were not available in this study.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to part of the data in the study related to other studies, but are available from the corresponding author on reasonable request.
Abbreviations
- AP:
-
Anteroposterior
- CC:
-
Craniocaudal
- Das:
-
Dopamine agonists
- FPAs:
-
Functioning pituitary adenomas
- FSH:
-
Follicle-stimulating hormone
- FT3:
-
Free triiodothyronine
- FT4:
-
Free thyroxine
- GH:
-
Growth hormone
- GKRS:
-
Gamma knife radiosurgery
- IGF-1:
-
Insulin-like growth factor-1
- LH:
-
Luteinizing hormone
- NPFAs:
-
Nonfunctioning pituitary adenomas
- Pas:
-
Pituitary adenomas
- SRS:
-
Stereotactic radiosurgery
- TSH:
-
Thyroid-stimulating hormone
- TR:
-
Transverse
References
Ostrom QT, Gittleman H, Xu J, Kromer C, Wolinsky Y, Kruchko C, Barnholtz-Sloan JS. CBTRUS Statistical Report: primary brain and other Central Nervous System tumors diagnosed in the United States in 2009–2013. Neurooncology. 2016;18(suppl5):v1–75.
Esposito D, Olsson DS, Ragnarsson O, Buchfelder M, Skoglund T, Johannsson G. Non-functioning pituitary adenomas: indications for pituitary surgery and post-surgical management. Pituitary. 2019;22(4):422–34.
Chang EF, Zada G, Kim S, Lamborn KR, Quinones-Hinojosa A, Tyrrell JB, Wilson CB, Kunwar S. Long-term recurrence and mortality after surgery and adjuvant radiotherapy for nonfunctional pituitary adenomas. J Neurosurg. 2008;108(4):736–45.
Dallapiazza RF, Grober Y, Starke RM, Laws ER Jr., Jane JA Jr. Long-term results of endonasal endoscopic transsphenoidal resection of nonfunctioning pituitary macroadenomas. Neurosurgery. 2015;76(1):42–52. discussion 52 – 43.
Ferrante E, Ferraroni M, Castrignano T, Menicatti L, Anagni M, Reimondo G, Del Monte P, Bernasconi D, Loli P, Faustini-Fustini M, et al. Non-functioning pituitary adenoma database: a useful resource to improve the clinical management of pituitary tumors. Eur J Endocrinol. 2006;155(6):823–9.
Picozzi P, Losa M, Mortini P, Valle MA, Franzin A, Attuati L, Ferrari da Passano C, Giovanelli M. Radiosurgery and the prevention of regrowth of incompletely removed nonfunctioning pituitary adenomas. J Neurosurg. 2005;102:71–4.
Park P, Chandler WF, Barkan AL, Orrego JJ, Cowan JA, Griffith KA, Tsien C. The role of radiation therapy after surgical resection of nonfunctional pituitary macroadenomas. Neurosurgery. 2004;55(1):100–6. discussion 106–107.
Lucas JW, Bodach ME, Tumialan LM, Oyesiku NM, Patil CG, Litvack Z, Aghi MK, Zada G. Congress of Neurological Surgeons Systematic Review and evidence-based Guideline on Primary Management of patients with nonfunctioning pituitary adenomas. Neurosurgery. 2016;79(4):E533–535.
Lee CC, Kano H, Yang HC, Xu Z, Yen CP, Chung WY, Pan DH, Lunsford LD, Sheehan JP. Initial Gamma Knife radiosurgery for nonfunctioning pituitary adenomas. J Neurosurg. 2014;120(3):647–54.
Yu J, Li Y, Quan T, Li X, Peng C, Zeng J, Liang S, Huang M, He Y, Deng Y. Initial Gamma Knife radiosurgery for nonfunctioning pituitary adenomas: results from a 26-year experience. Endocrine. 2020;68(2):399–410.
Molitch ME. Diagnosis and treatment of Pituitary adenomas: a review. JAMA. 2017;317(5):516–24.
Liu X, Kano H, Kondziolka D, Park KJ, Iyer A, Shin S, Niranjan A, Flickinger JC, Lunsford LD. Gamma knife stereotactic radiosurgery for drug resistant or intolerant invasive prolactinomas. Pituitary. 2013;16(1):68–75.
Petrovich Z, Yu C, Giannotta SL, Zee CS, Apuzzo ML. Gamma knife radiosurgery for pituitary adenoma: early results. Neurosurgery. 2003;53(1):51–9. discussion 59–61.
Jezkova J, Hana V, Kosak M, Krsek M, Liscak R, Vymazal J, Pecen L, Marek J. Role of gamma knife radiosurgery in the treatment of prolactinomas. Pituitary. 2019;22(4):411–21.
Higham CE, Johannsson G, Shalet SM, Hypopituitarism. Lancet (London England). 2016;388(10058):2403–15.
Sicignano G, Losa M, del Vecchio A, Cattaneo GM, Picozzi P, Bolognesi A, Mortini P, Calandrino R. Dosimetric factors associated with pituitary function after Gamma Knife surgery (GKS) of pituitary adenomas. Radiotherapy Oncology: J Eur Soc Therapeutic Radiol Oncol. 2012;104(1):119–24.
Cordeiro D, Xu Z, Mehta GU, Ding D, Vance ML, Kano H, Sisterson N, Yang HC, Kondziolka D, Lunsford LD et al. Hypopituitarism after Gamma Knife radiosurgery for pituitary adenomas: a multicenter, international study. Journal of neurosurgery 2018.
Sun S, Liu A, Zhang Y. Long-term Follow-Up studies of Gamma Knife Radiosurgery for Postsurgical Nonfunctioning Pituitary Adenomas. World neurosurgery; 2019.
Park KJ, Kano H, Parry PV, Niranjan A, Flickinger JC, Lunsford LD, Kondziolka D. Long-term outcomes after gamma knife stereotactic radiosurgery for nonfunctional pituitary adenomas. Neurosurgery. 2011;69(6):1188–99.
Sheehan JP, Starke RM, Mathieu D, Young B, Sneed PK, Chiang VL, Lee JY, Kano H, Park KJ, Niranjan A, et al. Gamma Knife radiosurgery for the management of nonfunctioning pituitary adenomas: a multicenter study. J Neurosurg. 2013;119(2):446–56.
Xu Z, Lee Vance M, Schlesinger D, Sheehan JP. Hypopituitarism after stereotactic radiosurgery for pituitary adenomas. Neurosurgery. 2013;72(4):630–7.
Fleseriu M, Hashim IA, Karavitaki N, Melmed S, Murad MH, Salvatori R, Samuels MH. Hormonal replacement in hypopituitarism in adults: an endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101(11):3888–921.
Tanaka S, Link MJ, Brown PD, Stafford SL, Young WF Jr., Pollock BE. Gamma knife radiosurgery for patients with prolactin-secreting pituitary adenomas. World Neurosurg. 2010;74(1):147–52.
Snell JW, Sheehan J, Stroila M, Steiner L. Assessment of imaging studies used with radiosurgery: a volumetric algorithm and an estimation of its error. Technical note. J Neurosurg. 2006;104(1):157–62.
Regal M, Paramo C, Sierra SM, Garcia-Mayor RV. Prevalence and incidence of hypopituitarism in an adult caucasian population in northwestern Spain. Clin Endocrinol. 2001;55(6):735–40.
Johnson MD, Woodburn CJ, Vance ML. Quality of life in patients with a pituitary adenoma. Pituitary. 2003;6(2):81–7.
Webb SM, Crespo I, Santos A, Resmini E, Aulinas A, Valassi E. MANAGEMENT OF ENDOCRINE DISEASE: quality of life tools for the management of pituitary disease. Eur J Endocrinol. 2017;177(1):R13–26.
Pollock BE, Cochran J, Natt N, Brown PD, Erickson D, Link MJ, Garces YI, Foote RL, Stafford SL, Schomberg PJ. Gamma knife radiosurgery for patients with nonfunctioning pituitary adenomas: results from a 15-year experience. Int J Radiat Oncol Biol Phys. 2008;70(5):1325–9.
Gopalan R, Schlesinger D, Vance ML, Laws E, Sheehan J. Long-term outcomes after Gamma Knife radiosurgery for patients with a nonfunctioning pituitary adenoma. Neurosurgery. 2011;69(2):284–93.
Graffeo CS, Link MJ, Brown PD, Young WF Jr., Pollock BE. Hypopituitarism after single-fraction pituitary adenoma radiosurgery: dosimetric analysis based on patients treated using contemporary techniques. Int J Radiat Oncol Biol Phys. 2018;101(3):618–23.
Loeffler JS, Shih HA. Radiation therapy in the management of pituitary adenomas. J Clin Endocrinol Metab. 2011;96(7):1992–2003.
Acknowledgements
Not applicable.
Funding
This work was supported by plan on enhancing scientific research in GMU; the Basic and Applied Basic Research Fund of Guangdong Province (2021A1515110596)(2022A1515220024); the Basic and Applied Basic Research Fund of Guangzhou science project (2024A04J3630).
Author information
Authors and Affiliations
Contributions
Research idea and study design: Jinxiu Yu, Jiaming Fu, Yanli Li. Data acquisition: Jinxiu Yu, Junyi Fu, Guangxin Hu, Guanye Hu, Wentao Hu.Statistical analysis: Yanli Li, Jiaming Fu. Manuscript drafting: Jinxiu Yu, Jiaming Fu, Yanli Li. Supervision and mentorship: Detian Liu, Junyi Fu. Each author contributed important content during manuscript drafting or revision and accepts accountability for the overall work, and all the authors agreed on the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval
The studies involving human participants were reviewed and approved by the institutional committee of the Second Affiliated Hospital of Guangzhou Medical University. The patients/ participants provided their written informed consent to participate in this study. All procedures performed were in accordance with the ethical standards of these committees and with the 1964 Declaration of Helsinki and its later amendments.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yu, J., Fu, J., Li, Y. et al. Hypopituitarism after gamma knife radiosurgery for pituitary adenomas: long-term results from a single-center experience. BMC Cancer 24, 963 (2024). https://doi.org/10.1186/s12885-024-12735-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12735-3