Abstract
Objective
To evaluate the safety of first-line systemic therapy for metastatic colorectal cancer through network meta-analysis.
Methods
The literature from PubMed, Embase, Web of Science, and Cochrane Library databases was searched from the inception of the databases to August 15, 2023, and strict inclusion and exclusion criteria were applied to screen studies. The Cochrane Bias Risk Assessment Tool (RoB 2.0) was used to evaluate the quality of the included literature. Network meta-analysis was conducted using Stata 15.0 and R4.3.1 software to compare the incidence of adverse events (AEs) among different treatment regimens.
Results
A total of 53 randomized controlled trials, involving 17,351 patients with metastatic colorectal cancer (mCRC), were ultimately included, encompassing 29 different therapeutic approaches. According to SUCRA rankings, the CAPOX regimen is most likely to rank first in terms of safety, while the FOLFOXIRI + panitumumab regimen is most likely to rank last. In terms of specific AEs, the CAPOX regimen, whether used alone or in combination with targeted drugs (bevacizumab and cetuximab), is associated with a reduced risk of neutropenia and febrile neutropenia, as well as an increased risk of thrombocytopenia and diarrhea. The FOLFOX regimen, with or without bevacizumab, is linked to an increased risk of neutropenia and peripheral sensory neuropathy. The FOLFIRI/CAPIRI + bevacizumab regimen is associated with a reduced risk of peripheral sensory neuropathy. S-1 and S-1 + oxaliplatin are well-tolerated in terms of gastrointestinal reactions. The FOLFOXIRI regimen, whether used alone or in combination with targeted drugs, is associated with various AEs.
Conclusion
In summary, the CAPOX regimen may be the safest option among the first-line systemic treatment regimens for mCRC patients, while the FOLFOXIRI + panitumumab regimen may be associated with a higher incidence of grade 3 or higher AEs.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) ranks as the fourth most common cause of cancer-related deaths worldwide, resulting in nearly 900,000 fatalities annually [1]. Metastasis is observed in approximately 20–30% of patients upon colorectal cancer diagnosis [2], and about 10–25% of patients develop metachronous metastasis following treatment-oriented surgery [3]. Metastatic colorectal cancer (mCRC) carries a grim prognosis, with a 5-year survival rate of less than 20% [4]. While surgery and local ablation can address some isolated metastases, there is no cure for the majority of CRC patients with multiple systemic metastases, necessitating palliative systemic treatment to extend overall survival. Presently, the National Comprehensive Cancer Network (NCCN) recommends various first-line systemic treatment regimens for mCRC patients [5]. These regimens primarily consist of dual and triple chemotherapy protocols based on 5-fluorouracil (5-FU) or capecitabine in combination with other cytotoxic agents (oxaliplatin or irinotecan), often with the addition of targeted drugs. However, many of these treatments lack direct comparative clinical trials, and some remain controversial in terms of safety. One meta-analysis indicates that FOLFOXIRI (5-fluorouracil plus leucovorin plus oxaliplatin plus irinotecan) + bevacizumab may increase the incidence of neutropenia and diarrhea compared to dual chemotherapy regimens with or without targeted drugs [6], while two other meta-analyses suggest that this regimen does not elevate treatment toxicity [7, 8]. The presence of toxic side effects restricts the clinical application of chemotherapy regimens and targeted drugs, such as hypertension and proteinuria induced by bevacizumab [9, 10], skin toxicity induced by Panitumumab and Cetuximab [11, 12], and hypomagnesemia related to panitumumab [13]. The safety of treatment protocols significantly impacts patients’ prognosis and quality of life. Reducing drug toxicity, mitigating the risk of adverse reactions, and enhancing patients’ quality of life necessitate ongoing exploration and practice by medical professionals.
Network meta-analysis (NMA) is frequently employed to compare differences among multiple treatment regimens, combining direct and indirect comparisons to offer crucial references for clinical drug usage guidance [14]. In prior NMA studies, more emphasis has been placed on evaluating the effectiveness of systemic therapy for colorectal cancer, with less attention directed toward assessing safety. One meta-analysis assessed the safety of 16 first-line systemic treatment regimens for mCRC patients but was limited to an overall analysis of grade 3 or higher adverse events (AEs) and did not specifically analyze the characteristics of individual AEs [8]. If clinicians have early knowledge of potential AEs and corresponding treatment measures associated with each treatment plan, they can choose the most suitable treatment method based on the specific conditions of patients. This approach is beneficial in enhancing the quality of life for patients. Therefore, by utilizing a network meta-analysis method to evaluate the safety of first-line systemic treatment for metastatic colorectal cancer, this study compares and ranks various adverse reactions to provide guidance for clinical decision-making.
Materials and methods
Design and registration
This systematic review study process followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2020) statement [15], and the protocol was registered with the International Prospective Registry of Systematic Reviews (PROSPERO: CRD42023462360).
Literature search
Two researchers (YR.Z, PP.M) independently searched for studies published in PubMed, Embase, Web of Science, and the Cochrane Library from the establishment of the database to August 15, 2023. The search terms were designed by combining subject words and free words. The search keywords encompassed colorectal neoplasm, colorectal cancer, metastasis, first-line chemotherapy, FOLFOX (5-fluorouracil plus leucovorin plus oxaliplatin), FOLFIRI (5-fluorouracil plus leucovorin plus irinotecan), CAPOX (capecitabine plus oxaliplatin), FOLFOXIRI, 5-fluorouracil, capecitabine, bevacizumab, cetuximab, panitumumab, and randomization. Specific search strategies are presented in supplementary materials (Appendix 1).
Inclusion and exclusion criteria
The inclusion criteria were as follows:
-
(a)
Population: Patients with pathologically confirmed colorectal cancer and distant metastases who have not received any treatment after diagnosis;
-
(b)
Interventions: Systemic therapy as first-line treatment for patients with mCRC;
-
(c)
Outcomes: Grade ≥ 3 AEs or toxic reactions (according to the Common Toxicity Criteria of the American National Cancer Institute) ;
-
(d)
Study type: Randomized controlled trial (RCT) with sample size ≥ 30;
-
(e)
Language: English.
Exclusion criteria:
-
(a)
Participants: Colorectal cancer patients without metastasis;
-
(b)
Interventions: Non-first line systemic treatment regimens (maintenance therapy, radiation therapy, second- or third-line therapy, etc.) ;
-
(c)
Outcomes: No relevant outcome indicators or data could not be extracted;
-
(d)
Non-RCT trials;
-
(e)
Duplicate studies or secondary analyses, in vitro experiments, animal experiments, reviews, letters, guidelines, case reports, pathological mechanisms, conference abstracts, reviews, or systematic reviews.
Literature screening and data extraction
Two researchers (YR.Z, PP.M) independently screened all articles identified by the database search. First, EndNote X 9.0 software was used to remove duplicate literature and exclude case reports, conference abstracts, letters, and review articles. Then, the titles and abstracts of the remaining literature were screened to exclude studies that were not relevant to the topic, and the full texts and supplementary information of the remaining studies were reviewed to identify eligible studies. Finally, data were extracted according to a unified extraction table, which included information such as the author, publication year, study design, study country, study period, number of study sites, follow-up time, total number of samples, and the number of AEs. The two researchers (YR.Z, PP.M) independently cross-checked all included papers and extracted data. Any disputed articles were referred to a third researcher (HMF) for consensus resolution.
Quality assessment
Two independent reviewers (YR.Z and PP.M) assessed the risk of bias using Version 2 of the Cochrane Risk-of-Bias Tool for randomized trials (RoB 2.0) (https://doi.org/10.1136/bmj.l4898). Each study was categorized as “low risk of bias,” “some concerns,” or “high risk of bias” across the following domains: bias arising from the randomization process; bias due to deviations from the intended intervention; bias from missing outcome data; bias in the measurement of outcomes; and bias in the selection of the reported results, including deviations from the registered protocol. We rated trials as having an overall high risk of bias if one or more domains were rated “high risk of bias” and as having an overall low risk of bias if all domains were rated “low risk of bias.”
Statistical analysis
Bayesian random-effects (BRE) models were employed to analyze the effects of interventions and compare their safety. Risk ratio (RR) and its 95% confidence interval (CrI) were used to combine the incidence of AEs, with a 95% CrI excluding 1 representing a statistically significant difference. The Markov chain Monte Carlo method was adopted for modeling, with four Markov chains running simultaneously. The annealing times were set to 20,000, and the modeling was completed after 50,000 simulation iterations [16]. The deviance information criterion (DIC) was used to compare model fit and global consistency. With there was a closed loop in the network, local consistency was analyzed using the node-splitting method [17]. Additionally, interventions were ranked based on the surface under the cumulative rank curve (SUCRA), and league tables were generated to compare differences in effects among interventions [18]. A funnel plot was used to intuitively reflect the heterogeneity among the studies. Analyses were conducted using Stata 15.0 (Stata Corporation, College Station, TX) and R 4.3.1 (R Development Core Team, Vienna, http://www.R-project.org). A difference with a p-value of less than 0.05 was considered statistically significant.
Results
Literature search results
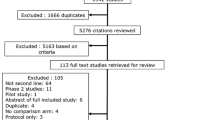
In the initial literature search, 36,127 articles were retrieved, and 11,616 duplicate studies were excluded. Following the inclusion and exclusion criteria, the article titles and abstracts were carefully examined, leading to the exclusion of 24,283 studies, while 228 potential related studies were initially included. After analyzing the full texts and supplementary materials, 53 RCT studies [19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71] were ultimately included for data extraction and statistical analysis. The flowchart of the literature retrieval and screening is presented in Fig. 1.
Basic characteristics of the included literature
In 53 Phase II/III randomized controlled trials, which included 17,351 mCRC patients, 29 different treatment schemes were used. Among these schemes, more patients received FOLFOX/FOLFIRI + Bevacizumab and CAPOX (Table 1 and Supplementary Table S1). These studies were published between 2000 and 2023. Only two were single-center studies [23, 24], while the rest were multicenter studies.
Quality evaluation
42 studies mentioned correct randomization methods, while 11 studies had unclear randomization methods. Among them, 20 studies reported well-established allocation concealment schemes and were rated as low risk; 31 studies had unclear allocation schemes and were categorized as an unknown risk, and 2 studies did not use allocation concealment schemes, resulting in a high risk. In addition, 25 studies did not mention blinding, and 18 studies did not employ a method to establish blinding for practitioners and patients. Lastly, 50 studies did not deviate from established interventions, and 3 studies had an unknown bias. All study outcomes were measured appropriately, and the outcome data were complete. Furthermore, all outcome measures mentioned in the study design were reported (Supplementary Figures S1 and S2).
Network meta-analysis of all AEs
Grade ≥ 3 AEs
Seventeen studies compared the incidence of grade 3 or higher AEs across 15 treatment regimens (Fig. 2A). The RR was 0.38 (95% CrI, 0.16–0.85) for the FULV (5-fluorouracil plus leucovorin) vs. FULV + bevacizumab regimen and 0.27 (95% CrI, 0.01–0.85) for CAPOX vs. FOLFOXIRI + bevacizumab regimen, indicating that the FULV and CAPOX regimens had a lower risk of grade 3 or higher AEs, as shown in Fig. 2B. The top three safety regimens based on SUCRA values were FULV (89.76%), CAPOX (85.29%), and FOLFIRI (76.34%), while the least safe regimen was FOLFOX + panitumumab (19.91%), as illustrated in Supplementary Table S2.
Death related to AEs
Eighteen studies compared the risk of death associated with AEs among 14 treatment regimens (Fig. 3A). Based on the safety ranking determined by the SUCRA value (where a higher SUCRA value indicates a lower incidence of AEs and a safer treatment regimen), the top three treatment plans were FOLFIRI + cetuximab (81.72%), FULV + bevacizumab (72.52%), and FOLFOX (68.53%). These results are presented in Supplementary Table S2. However, the league table results indicated that there was no statistically significant difference between these regimens (Fig. 3B).
Network meta-analysis on specific AEs
Hematological AEs
Neutropenia
Forty-four studies compared the incidence of neutropenia among 27 treatment regimens (Fig. 4A). The RR was 0.01 (95% CrI, 0–0.26) for CAPOX + cetuximab vs. FOLFOXIRI + cetuximab, 0.09 (95% CrI, 0.01–0.79) for capecitabine vs. CAPIRI (capecitabine plus irinotecan), and 0.1 (95% CrI, 0.05, 0.17) for CAPOX vs. FOLFOX. These results indicate that CAPOX + cetuximab, capecitabine, and CAPOX regimens had a lower risk of neutropenia, as depicted in Supplementary Figure S3. The top three regimens for safety based on SUCRA values were CAPOX + cetuximab (94.08%), capecitabine (89.93%), and CAPOX (83.63%). The least safe regimen was FOLFOXIRI + bevacizumab (6.55%), as shown in Table 2.
Network plot of hematological adverse events. (A) Neutropenia; (B) Leukopenia; (C) Anemia; (D)Thrombocytopenia. Bmab, bevacizumab; Cap, capecitabine; Cet, cetuximab; Oxa, oxaliplatin; Pmab, panitumumab; FU,5-fluorouracil; LV, leucovorin; Iri, irinotecan; CAPOX, capecitabine plus oxaliplatin; CAPIRI, capecitabine plus irinotecan; FOLFOX, 5-fluorouracil plus leucovorin plus oxaliplatin; FOLFOXIRI, 5-fluorouracil plus leucovorin plus oxaliplatin plus irinotecan; FOLFIRI, 5-fluorouracil plus leucovorin plus irinotecan; FUIRI, 5-fluorouracil plus irinotecan; IROX, irinotecan plus oxaliplatin. Each node represented a different treatment and its size depended on the number of patients that is directly examined. The nodes were joined by lines with different thickness which shows whether there was a direct relationship between treatments and the thickness was weighted according to the available direct evidence between them
Febrile neutropenia
Twenty-seven studies compared the incidence of febrile neutropenia among 19 treatment regimens (Supplementary Figure S4A). The RR was 0.15 (95% CrI, 0.05–0.36) for CAPOX vs. FOLFOXIRI, 28.45 (95% CrI, 1.85–437.2) for FOLFIRI vs. S-1 + oxaliplatin, and 0.11 (95% CrI, 0.02–0.41) for CAPOX + bevacizumab vs. FOLFOXIRI + bevacizumab, indicating a lower risk of febrile neutropenia for CAPOX, S-1 + oxaliplatin, and CAPOX + bevacizumab regimens, as shown in Supplementary Figure S5. The top three regimens for safety, based on SUCRA values, were CAPOX (91%), S-1 + oxaliplatin (87.86%), and CAPOX + bevacizumab (84.48%). The least safe regimen was FOLFIRI + cetuximab (13.54%), as indicated in Table 2.
Leukopenia
Eighteen studies compared the incidence of leukopenia among 19 treatment regimens (Fig. 4B). The RR was 0.01 (95% CrI, 0–0.68) for CAPOX + cetuximab vs. FOLFOXIRI + cetuximab, and 0.05 (95% CrI, 0–0.85) for CAPOX + bevacizumab vs. FOLFIRI + bevacizumab, indicating that CAPOX + cetuximab and CAPOX + bevacizumab had a lower risk of leukopenia, as depicted in Supplementary Figure S6. The top three regimens for safety, based on SUCRA values, were CAPOX + cetuximab (90.41%), CAPIRI + cetuximab (81.34%), and CAPOX + bevacizumab (80.12%). The least safe regimen was IROX (14.49%, irinotecan plus oxaliplatin), as shown in Table 2.
Anemia
Thirty studies compared the incidence of anemia among 22 treatment regimens (Fig. 4C). The top three regimens for safety, based on SUCRA values, were CAPOX + cetuximab (84.12%), CAPOX + bevacizumab (77.94%), and 5-FU + oxaliplatin (72.45%). The least safe regimen was FOLFOXIRI (16.05%), as indicated in Table 2. However, the league table results indicated that there was no statistical difference between the protocols (Supplementary Figure S7).
Thrombocytopenia
Thirty-four studies compared the incidence of thrombocytopenia among 25 treatment regimens (Fig. 4D). The RR was 0.04 (95% CrI, 0–0.39) for CAPIRI + bevacizumab vs. CAPOX + bevacizumab, and 0.05 (95% CrI, 0–0.84) for FOLFIRI + bevacizumab vs. FOLFOXIRI + bevacizumab, indicating that CAPIRI + bevacizumab and FOLFIRI + bevacizumab had a lower risk of thrombocytopenia, as shown in Supplementary Figure S8. The top three regimens for safety, based on SUCRA values, were CAPIRI + bevacizumab (84.43%), FOLFIRI + bevacizumab (79.98%), and CAPIRI + cetuximab (78.26%). The least safe regimen was S-1 + oxaliplatin (15.73%), as indicated in Table 2.
Gastrointestinal AEs
Diarrhea
Fifty-one studies compared the incidence of diarrhea among 29 treatment regimens (Fig. 5A). The RR was 0.15 (95% CrI, 0.02–0.95) for FOLFOX + bevacizumab vs. FOLFOXIRI regimen, 20.1 (95% CrI, 1.42–279.88) for CAPIRI vs. FULV + bevacizumab regimen, and 5.19 (95% CrI, 1.01–27.99) for CAPOX vs. FULV regimen. These results indicate that FOLFOX + bevacizumab, FULV + bevacizumab, and FULV regimens had a lower risk of diarrhea, as shown in Supplementary Figure S9. The top three safety regimens, based on SUCRA values, were FOLFOX + bevacizumab (83.63%), FULV + bevacizumab (82.64%), and FULV (82.28%). The least safe regimen was CAPIRI (16.85%), as illustrated in Table 2.
Network plot of Digestive adverse events. (A) Diarrhea; (B) Nausea; (C) Vomiting; (D) Mucositis/stomatitis. Bmab, bevacizumab. Cap, capecitabine; Cet, cetuximab; Oxa, oxaliplatin; Pmab, panitumumab; FU,5-fluorouracil; LV, leucovorin; Iri, irinotecan; CAPOX, capecitabine plus oxaliplatin; CAPIRI, capecitabine plus irinotecan; FOLFOX, 5-fluorouracil plus leucovorin plus oxaliplatin; FOLFOXIRI, 5-fluorouracil plus leucovorin plus oxaliplatin plus irinotecan; FOLFIRI, 5-fluorouracil plus leucovorin plus irinotecan; FUIRI, 5-fluorouracil plus irinotecan; IROX, irinotecan plus oxaliplatin. Each node represented a different treatment and its size depended on the number of patients that is directly examined. The nodes were joined by lines with different thickness which shows whether there was a direct relationship between treatments and the thickness was weighted according to the available direct evidence between them
Nausea
Thirty-one studies compared the incidence of nausea among 24 treatment regimens (Fig. 5B). The RR was 0.02 (95% CrI, 0–0.47) for FOLFIRI + cetuximab vs. FOLFOXIRI + cetuximab regimen, 0.03 (95% CrI, 0–0.48) for CAPOX vs. FOLFOXIRI regimen, and 39.22 (95% CrI, 1.54–2529.6) for FOLFOXIRI vs. S-1 + oxaliplatin. These results indicated that FOLFIRI + cetuximab, CAPOX, and S-1 + oxaliplatin regimens had a lower risk of nausea, as shown in Supplementary Figure S10. The top three safety regimens, based on SUCRA values, were FOLFIRI + cetuximab (85.81%), CAPOX (79.95%), and S-1 + oxaliplatin (78.5%). The least safe regimen was S-1 + oxaliplatin + LV (2.59%), as illustrated in Table 2.
Vomiting
Thirty-one studies compared the incidence of vomiting among 25 treatment regimens (Fig. 5C). The RR was 42.05 (95% CrI, 3.95–566.39) for IROX vs. S-1 + oxaliplatin, 0 (95% CrI, 0–0.51) for CAPIRI + cetuximab vs. FOLFOXIRI + cetuximab, and 0.06 (95% CrI, 0–0.85) for CAPOX vs. CAPOX + bevacizumab regimens. These results indicate that S-1 + oxaliplatin, CAPIRI + cetuximab, and CAPOX regimens had a lower risk of vomiting, as shown in Supplementary Figure S11. The top three regimens for safety, based on SUCRA values, were S-1 + oxaliplatin (90.57%), CAPIRI + cetuximab (85.73%), and CAPOX (81.54%). The least safe regimen was FOLFOXIRI + cetuximab (8.98%), as illustrated in Table 2.
Mucositis/stomatitis
Forty studies compared the incidence of mucositis or stomatitis among 28 treatment regimens (Fig. 5D). The RR was 0.06 (95% CrI, 0–0.62) for CAPOX vs. FOLFOX + cetuximab regimen and 0.14 (95% CrI, 0.03–0.55) for FOLFOX vs. FOLFOX + panitumumab. These results indicate a lower risk of mucositis or stomatitis for CAPOX and FOLFOX regimens, as shown in Supplementary Figure S12. The top three treatment regimens for safety, based on SUCRA values, were CAPOX (76.72%), Cap + bevacizumab (73.45%), and FOLFIRI + cetuximab (71.48%). The least safe regimen was FOLFOX + Cetuximab (16.71%), as illustrated in Table 2.
Anorexia
Ten studies compared the incidence of anorexia among 8 treatment regimens (Supplementary Figure S4B). The top three treatment regimens for safety, based on SUCRA values, were FOLFOX + bevacizumab (73.69%), CAPOX + bevacizumab (66.91%), and FOLFIRI + panitumumab (66.26%). The least safe regimen was S-1 + Iri + bevacizumab (15.18%), as illustrated in Table 2. However, the league table results showed that there was no statistical difference between the protocols (Supplementary Figure S13).
Neurological AEs
Peripheral sensory neuropathy
Twelve studies compared the risk of peripheral sensory neuropathy among 10 treatment regimens (Fig. 6A). The RR was 0.02 (95% CrI, 0–0.32) for CAPIRI + bevacizumab vs. CAPOX + bevacizumab, 0.02 (95% CrI, 0–0.16) for FOLFIRI + bevacizumab vs. FOLFOX + bevacizumab, and 0.04 (95% CrI, 0–0.38) for FOLFOXIRI + bevacizumab. These results indicate a lower risk of peripheral sensory neuropathy for CAPIRI + bevacizumab and FOLFIRI + bevacizumab regimens, as shown in Supplementary Figure S14. The top three treatment regimens for safety, based on SUCRA values, were CAPIRI + bevacizumab (88.87%), FOLFIRI + bevacizumab (86.12%), and FOLFIRI + cetuximab (82.62%). The lowest-ranked regimen was S-1 + oxaliplatin + LV (2.98%), as illustrated in Table 2.
Network plot of Neurological adverse events. (A) Peripheral sensory neuropathy; (B) Fatigue; (C) Hypertension; (D) Thromboembolic events. Bmab, bevacizumab. Cap, capecitabine; Cet, cetuximab; Oxa, oxaliplatin; Pmab, panitumumab; FU,5-fluorouracil; LV, leucovorin; Iri, irinotecan; CAPOX, capecitabine plus oxaliplatin; CAPIRI, capecitabine plus irinotecan; FOLFOX, 5-fluorouracil plus leucovorin plus oxaliplatin; FOLFOXIRI, 5-fluorouracil plus leucovorin plus oxaliplatin plus irinotecan; FOLFIRI, 5-fluorouracil plus leucovorin plus irinotecan; FUIRI, 5-fluorouracil plus irinotecan; IROX, irinotecan plus oxaliplatin. Each node represented a different treatment and its size depended on the number of patients that is directly examined. The nodes were joined by lines with different thickness which shows whether there was a direct relationship between treatments and the thickness was weighted according to the available direct evidence between them
Fatigue
Twenty-two studies compared the incidence of fatigue among 20 treatment regimens (Fig. 6B). CAPOX was associated with a lower risk of fatigue compared to CAPOX + Cetuximab (RR = 0.13, 95% CI: 0.02–0.83), as shown in Supplementary Figure S15. The top three regimens for safety, based on SUCRA values, were FOLFOXIRI + cetuximab (72.03%), CAPOX + bevacizumab (71.17%), and CAPOX (68.53%). The last-ranked regimen was CAPOX + Cetuximab (15.49%), as illustrated in Table 2.
Circulatory AEs
Hypertension
Nineteen studies compared the incidence of hypertension among 13 treatment regimens (Fig. 6C). Compared with FOLFOX + cetuximab (RR = 15.8, 95% CI: 2.05-436.84) and FOLFOX + panitumumab (RR = 9.65, 95% CI: 1.14, 323.19), FOLFOX + bevacizumab had a higher risk of hypertension. Compared with FOLFIRI + Bevacizumab (RR = 0.17, 95% CI: 0.06, 0.41) and FOLFIRI + cetuximab (RR = 0.16, 95% CI: 0.04, 0.66), FOLFIRI had a lower risk of hypertension. The results are shown in Supplementary Figure S16. The top three treatment regimens for safety, based on SUCRA values, were FOLFOX + cetuximab (88.06%), FOLFOX + panitumumab (80.96%), and FOLFIRI (80.54%). The last-ranked regimen was FOLFOXIRI + Bevacizumab (13.64%), as illustrated in Table 2.
Thromboembolic events
Eight studies compared the incidence of thromboembolic events among 7 treatment regimens (Fig. 6D). The top three treatment regimens for safety, based on SUCRA values, were FOLFOX (89.2%), FULV (74.78%), and FOLFOX + bevacizumab (61.62%), with the last regimen being FULV + bevacizumab (22.23%), as illustrated in Table 2. However, the league table results indicated no statistical difference between the protocols (Supplementary Figure S17).
Consistency and publication bias assessment
DIC was employed to compare the consistency model with the inconsistency model. All closed-loop models exhibited variation values of less than 5, indicating good consistency, as indicated by DIC. The local inconsistency test between direct evidence and indirect evidence revealed local inconsistency between CAPIRI + Bevacizumab and CAPOX + Bevacizumab (P = 0.01) and FOLFIRI + Bevacizumab (P = 0.01) in terms of thrombocytopenia, as shown in Supplementary Table S3. Regarding the assessment of publication bias, no evidence of publication bias was observed in the comparison-adjusted funnel plots (Supplementary Figures S18 and S19).
Discussion
In this study, we utilized the NMA method to compare and rank first-line systemic treatment regimens for mCRC patients, analyzing the specific AEs associated with each regimen. This approach aims to identify treatment regimens with high safety profiles and clarify the toxicity characteristics of each treatment regimen. Such findings are essential for offering guidance in clinical decision-making and hold significant practical values in enhancing the treatment outcomes and quality of life for mCRC patients.
Based on the NMA results, the CAPOX regimen ranked first in the SUCRA comprehensive rankings of AEs. It may currently be the safest regimen for first-line systemic treatment of mCRC patients. However, the analysis of specific AEs revealed that the CAPOX regimen was associated with thrombocytopenia and diarrhea. Degirmencioglu et al. [72] also showed that the CAPOX regimen was inferior to the FOLFOX regimen in terms of disease progression, metastasis, and mortality in patients with colorectal cancer. There was no significant difference between the two regimens in overall survival. An observational study from India indicated that the CAPOX regimen was more effective but was prone to grade 3/4 blood and gastrointestinal toxicities such as thrombocytopenia (11.7%) and diarrhea (5.5%), consistent with our findings [73]. Additionally, CAPOX regimens were well-tolerated in febrile neutropenia, neutropenia, and leukopenia. A meta-analysis concluded that oxaliplatin-based regimens were better tolerated regarding leukopenia and febrile neutropenia compared to irinotecan-based regimens [74]. Two RCTs [50, 58] also demonstrated that neutropenia and leukopenia were less likely to occur with CAPOX than FOLFOX. S-1 is an oral fluoropyrimidine chemotherapy agent designed to enhance the antitumor activity of 5-fluorouracil while reducing its severe gastrointestinal toxicity, including nausea, vomiting, stomatitis, and diarrhea [75]. Our study also found that S-1 or S-1 + Oxaliplatin regimens were well-tolerated in terms of gastrointestinal response.
FULV secured the second position in the SUCRA comprehensive rankings for AEs, indicating good safety. When comparing single-drug chemotherapy with combined chemotherapy or chemotherapy combined with targeted drugs, it becomes apparent that while they significantly enhance the anti-tumor effect, they also increase the occurrence of side effects. In a detailed analysis of specific AEs, both the FOLFOX and FOLFOX + bevacizumab regimens were associated with neutropenia and peripheral sensory neuropathy. Furthermore, the FOLFOX + bevacizumab regimens were linked to hypertension. FOLFOX exhibited a lower risk of hypertension compared to FOLFOX + bevacizumab (RR = 0.22 (95% CrI: 0.05–0.73). This finding was consistent with results from two RCTs [23, 60], which demonstrated that FOLFOX + bevacizumab was more likely to result in hypertension when directly compared with FOLFOX. This aligns with previous studies, which identified hypertension as the most common side effect of bevacizumab [76,77,78]. The FOLFOX + panitumumab and FOLFOX + cetuximab regimens were associated with multiple AEs. A meta-analysis assessing the safety of panitumumab in CRC patients revealed a higher frequency of grade 3/4 AEs in the panitumumab group when compared to the control group (RR = 1.17, 95% CI: 1.08–1.27, P = 0.0001) [79]. Concerning the toxic side effects of cetuximab, a separate meta-analysis suggested that cetuximab was linked to an increased risk of leukopenia, neutropenia, and anemia events in patients with colorectal cancer [80]. Another meta-analysis reported that cetuximab carried a greater risk of skin diseases compared to bevacizumab [81]. One study demonstrated a significantly higher incidence of hand and foot skin reactions (P = 0.02) in patients treated with CAPIRI + bevacizumab compared with patients treated with FOLFIRI + bevacizumab [47] .In addition, two RCTs also demonstrated that FOLFOX + cetuximab was associated with a higher incidence of grade 3 or higher AEs when compared to FOLFOX with or without bevacizumab [28, 58].
Irinotecan-based regimens, specifically FOLFIRI + bevacizumab and CAPIRI + bevacizumab, were well tolerated with regards to thrombocytopenia and peripheral sensory neuropathy. A meta-analysis indicated that irinotecan-based regimens were associated with a lower risk of peripheral sensory neuropathy and thrombocytopenia compared to oxaliplatin-based regimens [74]. Additionally, two RCTs provided evidence that CAPIRI + bevacizumab was less likely to cause peripheral sensory neuropathy and thrombocytopenia compared to CAPOX + bevacizumab [32, 42]. An RCT study demonstrated that FOLFIRI + bevacizumab was directly linked to a reduction in peripheral sensory neuropathy when compared with FOLFOX + bevacizumab [36]. According to the SUCRA ranking, the FOLFOXIRI scheme was more likely to result in grade 3 or higher AEs compared to FOLFIRI. Consistently, a meta-analysis showed that the incidence of neutropenia, anemia, diarrhea, stomatitis, and neuropathy in the FOLFOXIRI group was significantly higher than that in the FOLFIRI group [81], which aligns with the results of this study. Furthermore, three RCTs [26, 30, 40] also indicated that FOLFOXIRI + bevacizumab might increase the risk of grade 3 or higher AEs when directly compared with FOLFOX/FOLFIRI + bevacizumab.
As far as we know, this study possesses several notable advantages. Firstly, it employed network meta-analysis to directly and indirectly compare multiple interventions, addressing the limitation of traditional meta-analysis that only allows the analysis of two directly compared interventions. Secondly, this study evaluated the risk of AEs across different treatment regimens, providing a clearer understanding of the toxicity profile associated with each regimen. Thirdly, in comparison to other NMAs assessing the safety of first-line systemic treatment for mCRC [8], this study included and analyzed a more extensive range of treatment regimens and outcome indicators. It also incorporated and assessed the latest relevant studies, offering a robust reference for clinical treatment regimen selection. However, this study has acknowledged limitations. Firstly, due to the absence of head-to-head trials, some treatment options were excluded from the network for different outcomes. Secondly, our study did not analyze results according to the RAS and BRAF status or left/right status. This was primarily because among the 53 studies included, only two RCT studies [19, 22] compared treatment outcomes for left and right colon cancer, and 13 RCT studies mentioned the RAS and BRAF status. Consequently, we cannot fully evaluate all treatment options for mCRC based on RAS and BRAF status or left/right status. Thirdly, the different dosage forms of treatment regimens may affect the final assessment. Fourthly, for four outcome measures (i.e., death related to AEs, anemia, anorexia, and thromboembolic event), ranking guidance may be limited due to the absence of statistical differences between treatment regimens. Fifthly, there was local inconsistency in the indicator of thrombocytopenia. After a thorough examination and analysis of the original text, it was discovered that the number of responders in the CAPIRI + Bevacizumab regimen was frequently recorded as 0 for this indicator, potentially contributing to outcome inconsistency. Sixth, during literature screening, we only included studies where the language was English, which may have increased the bias of the results.
Conclusion
Based on SUCRA rankings, the CAPOX regimen is most likely to secure the top position in terms of safety, while the FOLFOXIRI + panitumumab regimen is most likely to rank last. In the analysis of specific AEs, The CAPOX regimen, whether combined with or without targeted drugs (bevacizumab and cetuximab), is associated with a reduced risk of neutropenia and febrile neutropenia, as well as an increased risk of thrombocytopenia and diarrhea. The FOLFOX regimen, with or without bevacizumab, is linked to an increased incidence of neutropenia and peripheral sensory neuropathy. The FOLFIRI/CAPIRI + bevacizumab regimen is connected to a decrease in the risk of peripheral sensory neuropathy. S-1 and S-1 + oxaliplatin are well tolerated with respect to gastrointestinal reactions. The FOLFOXIRI regimen, whether combined with or without targeted drugs, is associated with various AEs.
In summary, the CAPOX regimen appears to be the safest option among the first-line systemic treatment regimens for mCRC patients, while the FOLFOXIRI + panitumumab regimen may be associated with a higher incidence of grade 3 or higher AEs. More pharmacological and clinical trials are required to optimize first-line systemic regimens, enhancing efficacy and minimizing toxicity. Additionally, further well-designed, high-quality RCTs are anticipated to validate our findings.
Data availability
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
References
Dekker E, Tanis PJ, Vleugels JLA, Kasi PM, Wallace MB. Colorectal cancer. Lancet. 2019;394(10207):1467–80.
Biller LH, Schrag D. Diagnosis and treatment of metastatic colorectal Cancer: a review. JAMA. 2021;325(7):669–85.
Malakorn S, Ouchi A, Hu CY, Sandhu L, Dasari A, You YN, Kopetz ES, Ellis LM, Chang GJ. Tumor sidedness, recurrence, and Survival after curative resection of localized Colon cancer. Clin Colorectal Cancer. 2021;20(1):e53–60.
Carlomagno C, De Stefano A, Rosanova M, De Falco S, Attademo L, Fiore G, De Placido S. Multiple treatment lines and prognosis in metastatic colorectal cancer patients. Cancer Metastasis Rev. 2019;38(1–2):307–13.
Benson AB, Venook AP, Al-Hawary MM, Arain MA, Chen YJ, Ciombor KK, Cohen S, Cooper HS, Deming D, Farkas L, et al. Colon cancer, Version 2.2021, NCCN Clinical Practice guidelines in Oncology. J Natl Compr Canc Netw. 2021;19(3):329–59.
Shui L, Wu YS, Lin H, Shui P, Sun Q, Chen X. Triplet Chemotherapy (FOLFOXIRI) plus Bevacizumab Versus Doublet Chemotherapy (FOLFOX/FOLFIRI) plus Bevacizumab in Conversion Therapy for metastatic colorectal Cancer: a Meta-analysis. Cell Physiol Biochem. 2018;48(5):1870–81.
Zhou M, Yu P, Hernick Davin DB, Li Y, Wang Y, Fu L, Zhang J. Is FOLFOXIRI alone or combined with targeted therapy administered as first-line treatment a reasonable choice for most patients with mCRC? Systematic review and network meta-analysis. Oncotarget. 2017;8(37):62339–48.
Xu S, Sak A, Erol YB. Network Meta-analysis of first-line systemic treatment for patients with metastatic colorectal Cancer. Cancer Control. 2021;28:10732748211033497.
Quintanilha JCF, Wang J, Sibley AB, Jiang C, Etheridge AS, Shen F, Jiang G, Mulkey F, Patel JN, Hertz DL, et al. Bevacizumab-induced hypertension and proteinuria: a genome-wide study of more than 1000 patients. Br J Cancer. 2022;126(2):265–74.
Lacouture ME, Mitchell EP, Piperdi B, Pillai MV, Shearer H, Iannotti N, Xu F, Yassine M. Skin toxicity evaluation protocol with panitumumab (STEPP), a phase II, open-label, randomized trial evaluating the impact of a pre-emptive skin treatment regimen on skin toxicities and quality of life in patients with metastatic colorectal cancer. J Clin Oncol. 2010;28(8):1351–7.
Petrelli F, Ardito R, Ghidini A, Zaniboni A, Ghidini M, Barni S, Tomasello G. Different toxicity of Cetuximab and Panitumumab in Metastatic Colorectal Cancer treatment: a systematic review and Meta-analysis. Oncology. 2018;94(4):191–9.
Bond MJG, Bolhuis K, Loosveld OJL, de Groot JWB, Droogendijk H, Helgason HH, Hendriks MP, Klaase JM, Kazemier G, Liem MSL, et al. First-line systemic treatment strategies in patients with initially unresectable colorectal cancer liver metastases (CAIRO5): an open-label, multicentre, randomised, controlled, phase 3 study from the Dutch Colorectal Cancer Group. Lancet Oncol. 2023;24(7):757–71.
Leowattana W, Leowattana P, Leowattana T. Systemic treatment for metastatic colorectal cancer. World J Gastroenterol. 2023;29(10):1569–88.
Rouse B, Chaimani A, Li T. Network meta-analysis: an introduction for clinicians. Intern Emerg Med. 2017;12(1):103–11.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Brooks SP, Gelman A. General Methods for Monitoring Convergence of Iterative Simulations. J Comput Graphical Stat. 1998;7(4):434–55.
Dempster AP. The direct use of likelihood for significance testing. Stat Comput. 1997;7(4):247–52.
Veroniki AA, Straus SE, Fyraridis A, Tricco AC. The rank-heat plot is a novel way to present the results from a network meta-analysis including multiple outcomes. J Clin Epidemiol. 2016;76:193–9.
Watanabe J, Muro K, Shitara K, Yamazaki K, Shiozawa M, Ohori H, Takashima A, Yokota M, Makiyama A, Akazawa N, et al. Panitumumab vs Bevacizumab added to Standard First-Line Chemotherapy and overall survival among patients with RAS Wild-type, left-sided metastatic colorectal Cancer: a Randomized Clinical Trial. JAMA. 2023;329(15):1271–82.
Stintzing S, Heinrich K, Tougeron D, Modest DP, Schwaner I, Eucker J, Pihusch R, Stauch M, Kaiser F, Kahl C, et al. FOLFOXIRI Plus Cetuximab or Bevacizumab as First-Line treatment of BRAF(V600E)-Mutant metastatic colorectal Cancer: the Randomized Phase II FIRE-4.5 (AIO KRK0116) study. J Clin Oncol. 2023;41(25):4143–53.
Sastre J, García-Alfonso P, Viéitez JM, Cano MT, Rivera F, Reina-Zoilo JJ, Salud-Salvia A, Quintero G, Robles-Díaz L, Safont MJ, et al. Influence of BRAF and PIK3CA mutations on the efficacy of FOLFIRI plus bevacizumab or cetuximab as first-line therapy in patients with RAS wild-type metastatic colorectal carcinoma and < 3 baseline circulating tumour cells: the randomised phase II VISNÚ-2 study. ESMO Open. 2021;6(2):100062.
Heinemann V, von Weikersthal LF, Decker T, Kiani A, Kaiser F, Al-Batran SE, Heintges T, Lerchenmüller C, Kahl C, Seipelt G, et al. FOLFIRI plus cetuximab or bevacizumab for advanced colorectal cancer: final survival and per-protocol analysis of FIRE-3, a randomised clinical trial. Br J Cancer. 2021;124(3):587–94.
Tang W, Ren L, Liu T, Ye Q, Wei Y, He G, Lin Q, Wang X, Wang M, Liang F, et al. Bevacizumab Plus mFOLFOX6 Versus mFOLFOX6 alone as first-line treatment for RAS Mutant Unresectable Colorectal Liver-Limited metastases: the BECOME randomized controlled trial. J Clin Oncol. 2020;38(27):3175–84.
Sadahiro S, Suzuki T, Okada K, Saito G, Miyakita H, Ogimi T, Chan LF, Kamei Y. Oral S-1 with 24-h infusion of Irinotecan plus Bevacizumab versus FOLFIRI plus Bevacizumab as First-Line chemotherapy for metastatic colorectal Cancer: an open-label Randomized Phase II Trial. Oncology. 2020;98(9):637–42.
Maiello E, Di Maggio G, Cordio S, Cinieri S, Giuliani F, Pisconti S, Rinaldi A, Febbraro A, Latiano TP, Aieta M, et al. Bevacizumab in Combination with either FOLFOX-4 or XELOX-2 in first-line treatment of patients with metastatic colorectal Cancer: a Multicenter Randomized Phase II Trial of the Gruppo Oncologico Dell’Italia Meridionale (GOIM 2802). Clin Colorectal Cancer. 2020;19(2):109–15.
Aranda E, Viéitez JM, Gómez-España A, Gil Calle S, Salud-Salvia A, Graña B, Garcia-Alfonso P, Rivera F, Quintero-Aldana GA, Reina-Zoilo JJ, et al. FOLFOXIRI plus bevacizumab versus FOLFOX plus bevacizumab for patients with metastatic colorectal cancer and ≥ 3 circulating tumour cells: the randomised phase III VISNÚ-1 trial. ESMO Open. 2020;5(6):e000944.
Parikh AR, Lee FC, Yau L, Koh H, Knost J, Mitchell EP, Bosanac I, Choong N, Scappaticci F, Mancao C, et al. MAVERICC, a Randomized, Biomarker-stratified, phase II study of mFOLFOX6-Bevacizumab versus FOLFIRI-Bevacizumab as First-line chemotherapy in metastatic colorectal Cancer. Clin Cancer Res. 2019;25(10):2988–95.
Oki E, Emi Y, Yamanaka T, Uetake H, Muro K, Takahashi T, Nagasaka T, Hatano E, Ojima H, Manaka D, et al. Randomised phase II trial of mFOLFOX6 plus bevacizumab versus mFOLFOX6 plus cetuximab as first-line treatment for colorectal liver metastasis (ATOM trial). Br J Cancer. 2019;121(3):222–9.
Modest DP, Martens UM, Riera-Knorrenschild J, Greeve J, Florschütz A, Wessendorf S, Ettrich T, Kanzler S, Nörenberg D, Ricke J, et al. FOLFOXIRI Plus Panitumumab as First-Line treatment of RAS Wild-Type metastatic colorectal Cancer: the randomized, Open-Label, phase II VOLFI study (AIO KRK0109). J Clin Oncol. 2019;37(35):3401–11.
Hurwitz HI, Tan BR, Reeves JA, Xiong H, Somer B, Lenz HJ, Hochster HS, Scappaticci F, Palma JF, Price R, et al. Phase II randomized trial of sequential or concurrent FOLFOXIRI-Bevacizumab Versus FOLFOX-Bevacizumab for metastatic colorectal Cancer (STEAM). Oncologist. 2019;24(7):921–32.
Qin S, Li J, Wang L, Xu J, Cheng Y, Bai Y, Li W, Xu N, Lin LZ, Wu Q, et al. Efficacy and tolerability of First-Line Cetuximab Plus Leucovorin, Fluorouracil, and oxaliplatin (FOLFOX-4) Versus FOLFOX-4 in patients with RAS Wild-Type metastatic colorectal Cancer: the Open-Label, Randomized, Phase III TAILOR Trial. J Clin Oncol. 2018;36(30):3031–9.
Nakayama G, Mitsuma A, Sunagawa Y, Ishigure K, Yokoyama H, Matsui T, Nakayama H, Nakata K, Ishiyama A, Asada T, et al. Randomized Phase II Trial of CapOX plus Bevacizumab and CapIRI plus Bevacizumab as First-Line treatment for Japanese patients with metastatic colorectal Cancer (CCOG-1201 study). Oncologist. 2018;23(8):919–27.
Rivera F, Karthaus M, Hecht JR, Sevilla I, Forget F, Fasola G, Canon JL, Guan X, Demonty G, Schwartzberg LS. Final analysis of the randomised PEAK trial: overall survival and tumour responses during first-line treatment with mFOLFOX6 plus either panitumumab or bevacizumab in patients with metastatic colorectal carcinoma. Int J Colorectal Dis. 2017;32(8):1179–90.
Kwakman JJM, Simkens LHJ, van Rooijen JM, van de Wouw AJ, Ten Tije AJ, Creemers GJM, Hendriks MP, Los M, van Alphen RJ, Polée MB, et al. Randomized phase III trial of S-1 versus capecitabine in the first-line treatment of metastatic colorectal cancer: SALTO study by the Dutch Colorectal Cancer Group. Ann Oncol. 2017;28(6):1288–93.
Carrato A, Abad A, Massuti B, Grávalos C, Escudero P, Longo-Muñoz F, Manzano JL, Gómez A, Safont MJ, Gallego J, et al. First-line panitumumab plus FOLFOX4 or FOLFIRI in colorectal cancer with multiple or unresectable liver metastases: a randomised, phase II trial (PLANET-TTD). Eur J Cancer. 2017;81:191–202.
Yamazaki K, Nagase M, Tamagawa H, Ueda S, Tamura T, Murata K, Eguchi Nakajima T, Baba E, Tsuda M, Moriwaki T, et al. Randomized phase III study of bevacizumab plus FOLFIRI and bevacizumab plus mFOLFOX6 as first-line treatment for patients with metastatic colorectal cancer (WJOG4407G). Ann Oncol. 2016;27(8):1539–46.
Aparicio T, Lavau-Denes S, Phelip JM, Maillard E, Jouve JL, Gargot D, Gasmi M, Locher C, Adhoute X, Michel P, et al. Randomized phase III trial in elderly patients comparing LV5FU2 with or without irinotecan for first-line treatment of metastatic colorectal cancer (FFCD 2001-02). Ann Oncol. 2016;27(1):121–7.
Yamazaki K, Kuwano H, Ojima H, Otsuji T, Kato T, Shimada K, Hyodo I, Nishina T, Shirao K, Esaki T, et al. A randomized phase II study of combination therapy with S-1, oral leucovorin, and oxaliplatin (SOL) and mFOLFOX6 in patients with previously untreated metastatic colorectal cancer. Cancer Chemother Pharmacol. 2015;75(3):569–77.
Kim JH, Zang DY, Chung IJ, Cho SH, Park KU, Oh HS, Lee KH, Lee BH, Kim MJ, Park CK, et al. A Muti-center, Randomized Phase II study of oxaliplatin and S-1 versus Capecitabine and Oxaliplatin in patients with metastatic colorectal Cancer. J Cancer. 2015;6(10):1041–8.
Loupakis F, Cremolini C, Masi G, Lonardi S, Zagonel V, Salvatore L, Cortesi E, Tomasello G, Ronzoni M, Spadi R, et al. Initial therapy with FOLFOXIRI and bevacizumab for metastatic colorectal cancer. N Engl J Med. 2014;371(17):1609–18.
Douillard JY, Siena S, Cassidy J, Tabernero J, Burkes R, Barugel M, Humblet Y, Bodoky G, Cunningham D, Jassem J, et al. Final results from PRIME: randomized phase III study of panitumumab with FOLFOX4 for first-line treatment of metastatic colorectal cancer. Ann Oncol. 2014;25(7):1346–55.
Schmiegel W, Reinacher-Schick A, Arnold D, Kubicka S, Freier W, Dietrich G, Geißler M, Hegewisch-Becker S, Tannapfel A, Pohl M, et al. Capecitabine/irinotecan or capecitabine/oxaliplatin in combination with bevacizumab is effective and safe as first-line therapy for metastatic colorectal cancer: a randomized phase II study of the AIO colorectal study group. Ann Oncol. 2013;24(6):1580–7.
Hong YS, Jung KH, Kim HJ, Kim KP, Kim SY, Lee JL, Shim BY, Zang DY, Kim JH, Ahn JB, et al. Randomized phase II study of capecitabine with or without oxaliplatin as first-line treatment for elderly or fragile patients with metastatic colorectal cancer: a prospective, multicenter trial of the Korean Cancer Study Group CO06-01. Am J Clin Oncol. 2013;36(6):565–71.
Ducreux M, Adenis A, Pignon JP, François E, Chauffert B, Ichanté JL, Boucher E, Ychou M, Pierga JY, Montoto-Grillot C, et al. Efficacy and safety of bevacizumab-based combination regimens in patients with previously untreated metastatic colorectal cancer: final results from a randomised phase II study of bevacizumab plus 5-fluorouracil, leucovorin plus irinotecan versus bevacizumab plus capecitabine plus irinotecan (FNCLCC ACCORD 13/0503 study). Eur J Cancer. 2013;49(6):1236–45.
Cunningham D, Lang I, Marcuello E, Lorusso V, Ocvirk J, Shin DB, Jonker D, Osborne S, Andre N, Waterkamp D, et al. Bevacizumab plus capecitabine versus capecitabine alone in elderly patients with previously untreated metastatic colorectal cancer (AVEX): an open-label, randomised phase 3 trial. Lancet Oncol. 2013;14(11):1077–85.
Ychou M, Rivoire M, Thezenas S, Quenet F, Delpero JR, Rebischung C, Letoublon C, Guimbaud R, Francois E, Ducreux M, et al. A randomized phase II trial of three intensified chemotherapy regimens in first-line treatment of colorectal cancer patients with initially unresectable or not optimally resectable liver metastases. The METHEP trial. Ann Surg Oncol. 2013;20(13):4289–97.
Souglakos J, Ziras N, Kakolyris S, Boukovinas I, Kentepozidis N, Makrantonakis P, Xynogalos S, Christophyllakis C, Kouroussis C, Vamvakas L, et al. Randomised phase-II trial of CAPIRI (capecitabine, irinotecan) plus bevacizumab vs FOLFIRI (folinic acid, 5-fluorouracil, irinotecan) plus bevacizumab as first-line treatment of patients with unresectable/metastatic colorectal cancer (mCRC). Br J Cancer. 2012;106(3):453–9.
Pectasides D, Papaxoinis G, Kalogeras KT, Eleftheraki AG, Xanthakis I, Makatsoris T, Samantas E, Varthalitis I, Papakostas P, Nikitas N, et al. XELIRI-bevacizumab versus FOLFIRI-bevacizumab as first-line treatment in patients with metastatic colorectal cancer: a Hellenic Cooperative Oncology Group phase III trial with collateral biomarker analysis. BMC Cancer. 2012;12:271.
Hong YS, Park YS, Lim HY, Lee J, Kim TW, Kim KP, Kim SY, Baek JY, Kim JH, Lee KW, et al. S-1 plus oxaliplatin versus capecitabine plus oxaliplatin for first-line treatment of patients with metastatic colorectal cancer: a randomised, non-inferiority phase 3 trial. Lancet Oncol. 2012;13(11):1125–32.
Moosmann N, von Weikersthal LF, Vehling-Kaiser U, Stauch M, Hass HG, Dietzfelbinger H, Oruzio D, Klein S, Zellmann K, Decker T, et al. Cetuximab plus capecitabine and irinotecan compared with cetuximab plus capecitabine and oxaliplatin as first-line treatment for patients with metastatic colorectal cancer: AIO KRK-0104–a randomized trial of the German AIO CRC study group. J Clin Oncol. 2011;29(8):1050–8.
Guan ZZ, Xu JM, Luo RC, Feng FY, Wang LW, Shen L, Yu SY, Ba Y, Liang J, Wang D, et al. Efficacy and safety of bevacizumab plus chemotherapy in Chinese patients with metastatic colorectal cancer: a randomized phase III ARTIST trial. Chin J Cancer. 2011;30(10):682–9.
von Fischer L, Schalhorn A, Stauch M, Quietzsch D, Maubach PA, Lambertz H, Oruzio D, Schlag R, Weigang-Köhler K, Vehling-Kaiser U, et al. Phase III trial of irinotecan plus infusional 5-fluorouracil/folinic acid versus irinotecan plus oxaliplatin as first-line treatment of advanced colorectal cancer. Eur J Cancer. 2011;47(2):206–14.
Ducreux M, Bennouna J, Hebbar M, Ychou M, Lledo G, Conroy T, Adenis A, Faroux R, Rebischung C, Bergougnoux L, et al. Capecitabine plus oxaliplatin (XELOX) versus 5-fluorouracil/leucovorin plus oxaliplatin (FOLFOX-6) as first-line treatment for metastatic colorectal cancer. Int J Cancer. 2011;128(3):682–90.
Cassidy J, Clarke S, Díaz-Rubio E, Scheithauer W, Figer A, Wong R, Koski S, Rittweger K, Gilberg F, Saltz L. XELOX vs FOLFOX-4 as first-line therapy for metastatic colorectal cancer: NO16966 updated results. Br J Cancer. 2011;105(1):58–64.
Tebbutt NC, Wilson K, Gebski VJ, Cummins MM, Zannino D, van Hazel GA, Robinson B, Broad A, Ganju V, Ackland SP, et al. Capecitabine, bevacizumab, and mitomycin in first-line treatment of metastatic colorectal cancer: results of the Australasian gastrointestinal trials Group Randomized Phase III MAX Study. J Clin Oncol. 2010;28(19):3191–8.
Rosati G, Cordio S, Bordonaro R, Caputo G, Novello G, Reggiardo G, Manzione L. Capecitabine in combination with oxaliplatin or irinotecan in elderly patients with advanced colorectal cancer: results of a randomized phase II study. Ann Oncol. 2010;21(4):781–6.
Cunningham D, Sirohi B, Pluzanska A, Utracka-Hutka B, Zaluski J, Glynne-Jones R, Koralewski P, Bridgewater J, Mainwaring P, Wasan H, et al. Two different first-line 5-fluorouracil regimens with or without oxaliplatin in patients with metastatic colorectal cancer. Ann Oncol. 2009;20(2):244–50.
Bokemeyer C, Bondarenko I, Makhson A, Hartmann JT, Aparicio J, de Braud F, Donea S, Ludwig H, Schuch G, Stroh C, et al. Fluorouracil, leucovorin, and oxaliplatin with and without cetuximab in the first-line treatment of metastatic colorectal cancer. J Clin Oncol. 2009;27(5):663–71.
Aranda E, Valladares M, Martinez-Villacampa M, Benavides M, Gomez A, Massutti B, Marcuello E, Constenla M, Cámara JC, Carrato A, et al. Randomized study of weekly irinotecan plus high-dose 5-fluorouracil (FUIRI) versus biweekly irinotecan plus 5-fluorouracil/leucovorin (FOLFIRI) as first-line chemotherapy for patients with metastatic colorectal cancer: a Spanish Cooperative Group for the Treatment of Digestive Tumors Study. Ann Oncol. 2009;20(2):251–7.
Hochster HS, Hart LL, Ramanathan RK, Childs BH, Hainsworth JD, Cohn AL, Wong L, Fehrenbacher L, Abubakr Y, Saif MW, et al. Safety and efficacy of oxaliplatin and fluoropyrimidine regimens with or without bevacizumab as first-line treatment of metastatic colorectal cancer: results of the TREE study. J Clin Oncol. 2008;26(21):3523–9.
Borner M, Koeberle D, Von Moos R, Saletti P, Rauch D, Hess V, Trojan A, Helbling D, Pestalozzi B, Caspar C, et al. Adding cetuximab to capecitabine plus oxaliplatin (XELOX) in first-line treatment of metastatic colorectal cancer: a randomized phase II trial of the Swiss Group for Clinical Cancer Research SAKK. Ann Oncol. 2008;19(7):1288–92.
Fuchs CS, Marshall J, Mitchell E, Wierzbicki R, Ganju V, Jeffery M, Schulz J, Richards D, Soufi-Mahjoubi R, Wang B, et al. Randomized, controlled trial of irinotecan plus infusional, bolus, or oral fluoropyrimidines in first-line treatment of metastatic colorectal cancer: results from the BICC-C study. J Clin Oncol. 2007;25(30):4779–86.
Falcone A, Ricci S, Brunetti I, Pfanner E, Allegrini G, Barbara C, Crinò L, Benedetti G, Evangelista W, Fanchini L, et al. Phase III trial of infusional fluorouracil, leucovorin, oxaliplatin, and irinotecan (FOLFOXIRI) compared with infusional fluorouracil, leucovorin, and irinotecan (FOLFIRI) as first-line treatment for metastatic colorectal cancer: the Gruppo Oncologico Nord Ovest. J Clin Oncol. 2007;25(13):1670–6.
Díaz-Rubio E, Tabernero J, Gómez-España A, Massutí B, Sastre J, Chaves M, Abad A, Carrato A, Queralt B, Reina JJ, et al. Phase III study of capecitabine plus oxaliplatin compared with continuous-infusion fluorouracil plus oxaliplatin as first-line therapy in metastatic colorectal cancer: final report of the Spanish Cooperative Group for the Treatment of Digestive Tumors Trial. J Clin Oncol. 2007;25(27):4224–30.
Souglakos J, Androulakis N, Syrigos K, Polyzos A, Ziras N, Athanasiadis A, Kakolyris S, Tsousis S, Kouroussis C, Vamvakas L, et al. FOLFOXIRI (folinic acid, 5-fluorouracil, oxaliplatin and irinotecan) vs FOLFIRI (folinic acid, 5-fluorouracil and irinotecan) as first-line treatment in metastatic colorectal cancer (MCC): a multicentre randomised phase III trial from the Hellenic Oncology Research Group (HORG). Br J Cancer. 2006;94(6):798–805.
Hospers GA, Schaapveld M, Nortier JW, Wils J, van Bochove A, de Jong RS, Creemers GJ, Erjavec Z, de Gooyer DJ, Slee PH, et al. Randomised Phase III study of biweekly 24-h infusion of high-dose 5FU with folinic acid and oxaliplatin versus monthly plus 5-FU/folinic acid in first-line treatment of advanced colorectal cancer. Ann Oncol. 2006;17(3):443–9.
Kabbinavar FF, Schulz J, McCleod M, Patel T, Hamm JT, Hecht JR, Mass R, Perrou B, Nelson B, Novotny WF. Addition of bevacizumab to bolus fluorouracil and leucovorin in first-line metastatic colorectal cancer: results of a randomized phase II trial. J Clin Oncol. 2005;23(16):3697–705.
Hurwitz H, Fehrenbacher L, Novotny W, Cartwright T, Hainsworth J, Heim W, Berlin J, Baron A, Griffing S, Holmgren E, et al. Bevacizumab plus Irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med. 2004;350(23):2335–42.
Goldberg RM, Sargent DJ, Morton RF, Fuchs CS, Ramanathan RK, Williamson SK, Findlay BP, Pitot HC, Alberts SR. A randomized controlled trial of fluorouracil plus leucovorin, irinotecan, and oxaliplatin combinations in patients with previously untreated metastatic colorectal cancer. J Clin Oncol. 2004;22(1):23–30.
Kabbinavar F, Hurwitz HI, Fehrenbacher L, Meropol NJ, Novotny WF, Lieberman G, Griffing S, Bergsland E. Phase II, randomized trial comparing bevacizumab plus fluorouracil (FU)/leucovorin (LV) with FU/LV alone in patients with metastatic colorectal cancer. J Clin Oncol. 2003;21(1):60–5.
Giacchetti S, Perpoint B, Zidani R, Le Bail N, Faggiuolo R, Focan C, Chollet P, Llory JF, Letourneau Y, Coudert B, et al. Phase III multicenter randomized trial of oxaliplatin added to chronomodulated fluorouracil-leucovorin as first-line treatment of metastatic colorectal cancer. J Clin Oncol. 2000;18(1):136–47.
Degirmencioglu S, Tanrıverdi O, Demiray AG, Senol H, Dogu GG, Yaren A. Retrospective comparison of efficacy and safety of CAPOX and FOLFOX regimens as adjuvant treatment in patients with stage III colon cancer. J Int Med Res. 2019;47(6):2507–15.
Kalidindi AV, Dubashi B, Jayanthi M, Shewade DG. Efficacy and safety of capecitabine and oxaliplatin (CAPOX) treatment in colorectal cancer: an observational study from a tertiary cancer center in South India. Indian J Cancer. 2022;59(1):73–9.
Kawai S, Takeshima N, Hayasaka Y, Notsu A, Yamazaki M, Kawabata T, Yamazaki K, Mori K, Yasui H. Comparison of irinotecan and oxaliplatin as the first-line therapies for metastatic colorectal cancer: a meta-analysis. BMC Cancer. 2021;21(1):116.
Saif MW, Syrigos KN, Katirtzoglou NA. S-1: a promising new oral fluoropyrimidine derivative. Expert Opin Investig Drugs. 2009;18(3):335–48.
Berger MD, Yamauchi S, Cao S, Hanna DL, Sunakawa Y, Schirripa M, Matsusaka S, Yang D, Groshen S, Zhang W, et al. Autophagy-related polymorphisms predict hypertension in patients with metastatic colorectal cancer treated with FOLFIRI and bevacizumab: results from TRIBE and FIRE-3 trials. Eur J Cancer. 2017;77:13–20.
Ranpura V, Pulipati B, Chu D, Zhu X, Wu S. Increased risk of high-grade hypertension with bevacizumab in cancer patients: a meta-analysis. Am J Hypertens. 2010;23(5):460–8.
Wang C, Tan C, Chen X, Chen S. The efficacy and safety of panitumumab supplementation for colorectal cancer: a meta-analysis of randomized controlled studies. Med (Baltim). 2020;99(11):e19210.
Cui R, Chu L, Liu ZQ, Xiao YY, Zhu XL, Chen YJ, Xu Q. Hematologic toxicity assessment in solid tumor patients treated with cetuximab: a pooled analysis of 18 randomized controlled trials. Int J Cancer. 2015;136(4):936–44.
Cui Y, Guo Y. The effectiveness and safety of bevacizumab versus cetuximab in the treatment of colorectal cancer: a systematic review and meta-analysis. Int J Clin Pharm. 2022;44(4):843–51.
Xu W, Kuang M, Gong Y, Cao C, Chen J, Tang C. Survival benefit and safety of the combinations of FOLFOXIRI ± bevacizumab versus the combinations of FOLFIRI ± bevacizumab as first-line treatment for unresectable metastatic colorectal cancer: a meta-analysis. Onco Targets Ther. 2016;9:4833–42.
Acknowledgements
Not applicable.
Funding
This study was funded by the project of Science and Technology Department of Shaanxi Province (2021SF-233).
Author information
Authors and Affiliations
Contributions
All authors contributed to the conceptualization and design of the study. Yanrong Zhan and Wenzhe Feng were involved in conceptualization, methodology, software, original manuscript writing, data organization, and visualization, among other aspects. Shufa Tan and Pingping Mei contributed to the investigation, initial draft writing, review, and editing. Wenzhe Feng and Hua Jiang played a role in methodology, software, and initial draft writing. Xianwen Cheng was responsible for conceptualization, supervision, project management, and funding acquisition. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All analyses were based on previous published studies, thus no ethical approval and patient consent are required.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhan, Y., Cheng, X., Mei, P. et al. Safety of first-line systemic therapy in patients with metastatic colorectal cancer: a network meta-analysis of randomized controlled trials. BMC Cancer 24, 893 (2024). https://doi.org/10.1186/s12885-024-12662-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12662-3