Abstract
Objective
The International Federation of Gynecology and Obstetrics (FIGO) 2023 staging system for endometrial cancer (EC) was released with incorporating histology, lympho-vascular space invasion, and molecular classification together. Our objective is to further explore the clinical utility and prognostic significance of the 2023 FIGO staging system in China.
Methods
A retrospective analysis was conducted for patients who received standard surgeries and underwent genetic testing using multigene next-generation sequencing (NGS) panels between December 2018 and December 2023 at Fudan University Shanghai Cancer Center, Shanghai, China. The genomic and clinical data of all patients were analyzed, and stages were determined by both the 2009 and 2023 FIGO staging systems. Kaplan–Meier estimators and Cox proportional hazards models were used for survival analysis.
Results
A total of 547 patients were enrolled in the study. After the restaged by the FIGO 2023 staging system, stage shifts occurred in 147/547 (26.9%) patients. In patients with early stages in FIGO 2009 (stage I-II), 63 cases were rearranged to IAmPOLEmut and 53 cases to IICmp53abn due to the molecular classification of POLEmut and p53abn. Altogether 345 cases were in stage I, 107 cases in stage II, 69 cases in stage III, and 26 cases in stage IV according to the FIGO 2023 staging criteria. For stage I diseases, the 3-year PFS rate was 92.7% and 95.3% in 2009 and 2023 FIGO staging systems, respectively. The 3-year PFS of stage II in 2023 FIGO was lower than that of FIGO 2009 (3-year PFS: 85.0% versus 90.9%), especially in substage IIC and IICmp53abn. Three cases (12%) of stage IIIA in FIGO 2009 were shifted to stage IA3 FIGO 2023, with 3-year PFS rates of 90.9% versus 100%, respectively. In NGS analysis, the most prevalent gene alterations were observed in PTEN and PIK3CA.
Conclusion
The FIGO 2023 staging system was proved to be a good predictor of survival for EC patients with enhanced precision compared to FIGO 2009. Predominant stage shifts were observed in early-stage diseases. Distinct gene alterations of different subtypes may help to explore more accurate target therapies.
Similar content being viewed by others
Introduction
Endometrial cancer (EC) is one of the most common gynecological cancers for women with an increasing incidence worldwide [1, 2]. It has been fifteen years since the International Federation of Gynecology and Obstetrics released the FIGO 2009 staging system for EC. In 2013, The Cancer Genome Atlas (TCGA) published a molecular classification with distinct molecular characteristics and prognostic predictions. Simplified classifications of the ProMisE and Trans-PORTEC had markedly enhanced the clinical utility of molecular classification, which include POLE ultramutation (POLEmut), mismatch repair deficiency (MMRd), p53- abnormality (p53abn), and no specific molecular profile (NSMP) [3, 4].
With the accumulated data on the prognostic significance of molecular classification and clinical characteristics, the new 2023 FIGO staging system has been released, incorporating molecular classification, lympho-vascular space invasion (LVSI), and invasive pathological type as significant prognostic indicators [5,6,7,8,9]. The 2023 update improves the existing staging system by providing more precise indications for prognoses and treatment of EC.
After the 2023 FIGO staging system was released, it has not been widely applied yet, especially in China. Although several retrospective studies had reported the improved prediction of prognosis with the 2023 FIGO staging system [10,11,12], some scholars still wondered if it was too early to incorporate evolving premature and complicated variables that lack robust supporting evidence, such as LVSI and aggressive histology [13, 14]. Thus, we conducted this retrospective study to further evaluate the clinical applicability of the FIGO2023 staging system and explore its prognostic significance of endometrial cancer.
Materials and methods
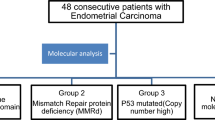
We collected data from patients who received standard surgeries and genetic testing at Fudan University Shanghai Cancer Center (FUSCC) between December 2018 and December 2023, approved by the Institutional Review Board (IRB), which included surgical details, pathological reports, immunohistochemistry (IHC) results, postoperative therapies, and follow-up details. The inclusion and exclusion criteria are in Supplementary Fig. 1. The stage was determined by both the 2009 and 2023 FIGO staging systems. All pathological results were reviewed by at least two senior pathologists. The multi-gene next-generation sequencing (NGS) panel was utilized, including APC, AKT1, ATM, BRAF, BRCA1, BRCA2, CDH1, CHEK2, EGFR, EPCAM, ERBB2, HRAS, KIT, KRAS, MET, MLH1, MSH2, MSH6, MUTYH, NRAS, PDGFRA, PIK3CA, PMS2, POLD1, POLE, PTCH1, PTEN, SDHB, SDHC, SDHD, SMAD4, STK11, TP53, and 66 microsatellite loci, etc. (Supplementary Table 1). The NGS panel detected insertions, deletions, base substitutions, and copy number alterations of the assessed genes, as well as microsatellite instability (MSI) status. Patients were classified into POLE mutated (POLEmut), mismatch repair deficient (MMRd), no specific molecular profile (NSMP), or p53 abnormal (p53abn) subtypes, according to the results of NGS and MSI status as previous studies suggested [15, 16]. The molecular classification was determined by at least two senior pathologists. Sub-stratification of stages IIIC1 and IIIC2 was not evaluated due to flawed information on lymph node micro- and macro-metastasis assessments.
Statistical analyses were performed using R Studio (version 4.2.1; R Studio, http://www.R-project.org) and IBM SPSS Statistics (Version 26.0). A significance level of p < 0.05 was considered statistically significant. Patients’ clinicopathologic characteristics were presented, and staging shifts were depicted using both table and Sankey diagram generated with RAWGraphs (https://app.rawgraphs.io). Progression-free survival (PFS) and overall survival (OS) were assessed via Kaplan–Meier analysis, and corresponding 95% confidence intervals (CIs) were calculated using the Brookmeyer-Crowley method.
Results
Clinicopathologic characteristics
A total of 547 patients were enrolled in the study. According to the results of NGS, 69 POLEmut patients, 118 MMRd patients, 280 NSMP patients, and 80 p53abn patients were observed, respectively. PFS and OS rates of different molecular subtypes were shown in Fig. 1, in which 3-year PFS and OS of POLEmut patients were 98.5% [95%-confidence interval (CI) 95.6–100] and 100%, respectively. 3-year survival rates of p53abn were the lowest [3-year PFS: 73.8% (95%-CI 61.6–88.5), 3-year OS: 94.0% (95%-CI 87.4–100)]. For MMRd and NSMP subtypes, the 3-year PFS rate was 85.7% (95%-CI 76.9–95.5) versus 90.7% (95%-CI 85.6–96.2), with the 3-year OS rate of 97.2% (95%-CI 93.2–100) versus 97.6% (95%-CI 94.8–100), respectively.
The median follow-up time was 19.0 months [interquartile range (IQR): 9.0–32.0]. During the process of follow-up, 38 patients had recurrences, and 9 deaths were observed. More detailed characteristics are listed in Table 1.
Stage shifts of patients
Among 547 patients, altogether 147 cases (26.9%) were observed with stage shifts (Table 2). Figure 2 provides the Sankey diagram of all stage shifts.
In patients with early stages in 2009 FIGO (stage I-II), 63 cases (14.0%) of 2009 FIGO early-stage disease were rearranged to IAmPOLEmut and 53 cases (11.8%) to IICmp53abn due to the molecular classification of POLEmut and p53abn. Stage shifts were also observed in the early stages with the incorporation of substantial lympho-vascular space invasion (LVSI) and aggressive pathological types. Four cases of 2009 FIGO stage IA converted to 2023 FIGO IIB due to substantial LVSI. Furthermore, 16 cases of stage IA (4.7%), and 7 cases of stage IB (9.5%) were reclassified as stage IIC due to aggressive histology, plus 1 case of stage IA (0.3%) converted to stage IC with aggressive histology without myometrial invasion.
In advanced-stage disease (stages III-IV), a total of 3 stage shifts were observed, which with concurrent endometrial and ovarian low-grade endometrioid cancer were restaged from IIIA under FIGO2009 to IA3 under FIGO 2023.
Survival analysis
For stage I disease, substage IAmPOLEmut exhibited an excellent prognosis with 3-year PFS and OS of 98.4% (95%-CI 95.3–100) and 100%, respectively. For stage II disease, the 3-year PFS in the 2023 FIGO staging system was lower than that of 2009, with 3-year PFS: 85.0% (95%-CI 75.2–96.0) versus 90.9% (95%-CI 79.5–100). The 3-year PFS for substage IIC and IICmp53abn patients was lower compared to other early-stage diseases, with 3-year PFS 72.6% (95%-CI 45.9–100) and 88.3% (95%-CI 76.6–100), respectively. For patients with stage shift of FIGO2009 stage IIIA, the 3-year PFS rates of FIGO2009 stage IIIA1 and IA3 in the 2023 FIGO staging were 87.5% (95%-CI 67.3–100) versus 100%, respectively. The prognoses of stage I-IV of FIGO 2009 and 2023 staging were detailed in Table 3.
For all patients, univariate analyses showed that those with aggressive histological types (p < 0.0001), lymph node metastases (LNM) (p = 0.0054), and LVSI (p = 0.0015) had worse prognoses (Supplementary Fig. 2). In multivariate analyses, Grade III, LNM, non-aggressive histological subtypes, and absence of LVSI were significant prognostic factors (p < 0.0001), with an odds ratio (OR): 4.29, 3.09, 0.25, and 0.34, respectively. The prognoses of stage I-IV of FIGO 2023 staging were detailed in Table 3
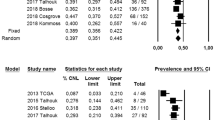
IHC versus NGS concordance
Immunohistochemistry (IHC) of p53 protein and MMR protein was detected, which includes p53, MLH1, PMS2, MSH2, and MSH6 protein expression. Forty-eight cases were excluded due to the lack of IHC information. Detailed results of NGS and IHC detection for MSI/MMR and TP53/p53 status are shown in Fig. 3. While taking MMR IHC as a substitution for MSI assay, 38 cases exhibited different results between MMR IHC and MSI assay, with a concordance rate of 92.4%. As for TP53/p53 status, 79 discordant NGS versus IHC cases were observed, representing a discordance rate of 15.8%.
The overall concordance rate was 88.3% when taking the p53 IHC and MMR IHC together into consideration. These discordant situations mentioned above within IHC and NGS result in altered molecular subtypes, especially in the NSMP and p53abn subtypes, as shown in Table 4.
Targetable gene alterations
A comprehensive statistical analysis of the NGS panel results was performed (Table 5). PIK3CA and PTEN, pivotal components of the PI3K/AKT pathway, exhibited a high mutation rate of 59% and 81% in all cases, respectively. Especially in the POLEmut subgroup, the alteration rates of PIK3CA and PTEN were 88% and 96%, respectively. Genes associated with the homologous recombination repair (HRR) pathway, such as BRCA1/2 and ATM, demonstrated mutation rates of 14%, 26%, and 34% in the MMRd subtype. Additionally, estrogen receptor (ER) and progesterone receptor (PR) exhibited high positivity rates in the NSMP subgroup (by IHC), with positivity percentages of 90% and 88%, respectively. Moreover, in the prognostic analyses, NRAS mutation found as a significant prognostic factor (p = 0.039). (Supplementary Fig. 3).
Discussion
In this study, significant shift was observed by restaging with the 2023 FIGO staging system to provide more precise prognostic indications.
The majority of staging alterations occurred in clinically earlier-stage patients (Stages I-II) due to the introduction of molecular subtypes, LVSI status, and aggressive histological types [5]. Patients in the early stages have improved prognostic precision compared with the 2009 system, especially in substages IAmPOLEmut and IICmp53abn (Supplementary Fig. 2). Multiple studies have confirmed good prognoses of the POLEmut subgroup, regardless of postoperative adjuvant therapy [8, 17,18,19,20]. In this study, we also verified the excellent prognosis of the IAmPOLEmut cases, with a 3-year PFS rate of 98.4%. Therefore, de-escalating therapy was suggested by ESGO/ESTRO/ESP guidelines for early-stage POLEmut patients [21, 22]. As IICmp53abn patients exhibiting poorer prognoses (3-year PFS rate of 88.3%), regardless of histological type, stage, or grade [23, 24], more advanced therapies were suggested for p53abn EC patients[21]. Moreover, the aggressive histological types were involved in the FIGO 2023 staging system [5]. Previous studies demonstrated the worse prognoses of EC patients with aggressive histology [6, 25]. Our results also figured out that substage IIC patients have significantly worse 3-year PFS rates compared to other stage II diseases with non-aggressive histology type, with 3-year PFS of 72.6% versus 85.6% (IIA) and 100% (IIB), respectively.
Stage shift in stage III diseases was mainly because of the inclusion of the new IA3 category. The introduction of synchronous early-stage uterine and ovarian cancers (SEOs) provides additional refinement in prognosis compared to the 2009 FIGO system. Of note, there were discernible prognostic disparities between IA3 and IIIA1 patients, with a 3-year PFS rate of 100% and 87.5%, respectively. Similarly, Gravbrot et al. also noted significant prognostic distinctions between Stage IIIA and IA3 in their cohort of The National Cancer Database (NCDB) [12]. In the etiology of SEOs, most researchers suggest a complex interplay involving clonality, epigenetics, and the tumor microenvironment, indicating a shared origin associated with a favorable prognosis [26, 27]. Therefore, the postoperative treatment was not necessary for patients with stage IA3.
Besides, in our study, LVSI, aggressive histological subtypes, and lymph node metastases were also identified as significant prognostic factors, which is consistent with previous literature [6,7,8,9]. Sentinel lymph node biopsy (SLNB) has been widely used in low-risk EC, and the 37 patients in our study who underwent SLNB demonstrated excellent prognoses. However, there remains controversy regarding the use of SLNB in intermediate-high-risk EC. To address this, a clinical trial (NCT04276532) is currently underway in this patient population. Beyond SLNB, radiomics analysis has emerged as a promising method for predicting nodal metastasis in EC in recent years [28].
ProMisE and TransPORTEC studies have suggested that p53, MLH1, MSH2, MSH6, and PMS2 protein immunostaining status as a substitute for TP53 NGS and microsatellite instability status [3, 29], with an approximate accuracy range of 81.3%-95.6% and 93.3%-98.8% [30,31,32,33], respectively. We also employed the IHC as an alternative to molecular testing for economic practicality and clinical accessibility. According to our results, IHC was an acceptable alternative to next-generation NGS in the molecular subtype of EC, especially for mismatch repair protein immunostaining with a concordance rate of 92.4%. However, the concordance rate (84.2%) between IHC and NGS indicated a more cautious decision of interchange of TP53/p53. Discordant results of two techniques testing TP53 status could be explained by tumor heterogeneity, alterations in non-coding regulatory regions, flawed detection of stop-gained mutation, and large-scale deletions or insertions [31, 34]. Some conflicting cases within MMR IHC and MSI assay could be potentially explained by MLH1 promoter methylation, solely MLH1 or MSH6 mutation resulting in protein dysfunction without structural changes, and other undefined situations [33, 35]. In some confusing cases, NGS might be recommended to provide more precise information and avoid misdiagnoses in these patients.
The elevated somatic mutation frequency observed in our study of PIK3CA and PTEN suggests a potential therapeutic strategy targeting the PI3K/AKT/mTOR pathway, and the clinical trials in advanced or recurrent EC showed modest antitumor activity with these targeted therapies. Combined targeted therapy might be an option for these patients [36,37,38,39]. In MMRd patients of our study, the highly mutated genes associated with homologous recombination repair pathways suggest potential responsiveness to immune checkpoint inhibition therapy, as previous studies reported [40, 41]. High expression of estrogen and progesterone receptors of NSMP in our study implied the high hormone sensitivity of this subtype. Thereby emerging research has revealed the potential efficacy of anti-estrogen therapy for NSMP patients, such as Letrozole and Anastrozole, particularly among those at elevated risk of disease recurrence and metastasis [42,43,44]. As for NRAS mutation, few studies revealed effective therapeutic methods targeting NRAS alone, but targeting MAPK or PI3K pathways may be an indirect but effective therapy (NCT01763164 and NCT01781429) [45,46,47].
Several limitations should be considered when interpreting the results of our study. Firstly, although our study involved a large sample size, our cohort is confined to a single center which may compromise the power of our findings. Secondly, with the flawed information on lymph node micro-metastasis assessments, the sub-stratification of stages IIIC1 and IIIC2 was unavailable in our study. Thirdly, our results may suffer from a retrospective nature, which may lead to bias inevitably.
In conclusion, in this study, we further explored the clinical applicability and prognostic significance of the 2023 FIGO staging system, and tried to find the potential targeted therapies for different molecular subtypes. Large population-based study is still necessary to validate the accuracy of our findings.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer Statistics, 2021. CA Cancer J Clin. 2021;71:7–33. https://doi.org/10.3322/caac.21654.
Crosbie EJ, Kitson SJ, McAlpine JN, Mukhopadhyay A, Powell ME, Singh N. Endometrial cancer. Lancet. 2022;399:1412–28. https://doi.org/10.1016/s0140-6736(22)00323-3.
Talhouk A, McConechy MK, Leung S, Yang W, Lum A, Senz J, Boyd N, Pike J, Anglesio M, Kwon JS, et al. Confirmation of ProMisE: A simple, genomics-based clinical classifier for endometrial cancer. Cancer. 2017;123:802–13. https://doi.org/10.1002/cncr.30496.
Stelloo E, Bosse T, Nout RA, MacKay HJ, Church DN, Nijman HW, Leary A, Edmondson RJ, Powell ME, Crosbie EJ, et al. Refining prognosis and identifying targetable pathways for high-risk endometrial cancer; a TransPORTEC initiative. Mod Pathol. 2015;28:836–44. https://doi.org/10.1038/modpathol.2015.43.
Berek JS, Matias-Guiu X, Creutzberg C, Fotopoulou C, Gaffney D, Kehoe S, Lindemann K, Mutch D, Concin N. FIGO staging of endometrial cancer: 2023. Int J Gynaecol Obstet. 2023;162:383–94. https://doi.org/10.1002/ijgo.14923.
Barlin JN, Soslow RA, Lutz M, Zhou QC, St Clair CM, Leitao MM Jr, Iasonos A, Hensley ML, Barakat RR, Matias-Guiu X, Abu-Rustum NR. Redefining stage I endometrial cancer: incorporating histology, a binary grading system, myometrial invasion, and lymph node assessment. Int J Gynecol Cancer. 2013;23:1620–8. https://doi.org/10.1097/IGC.0b013e3182a5055e.
Barnes EA, Martell K, Parra-Herran C, Taggar AS, Donovan E, Leung E. Substantial lymphovascular space invasion predicts worse outcomes in early-stage endometrioid endometrial cancer. Brachytherapy. 2021;20:527–35. https://doi.org/10.1016/j.brachy.2020.12.006.
León-Castillo A, de Boer SM, Powell ME, Mileshkin LR, Mackay HJ, Leary A, Nijman HW, Singh N, Pollock PM, Bessette P, et al. Molecular Classification of the PORTEC-3 Trial for High-Risk Endometrial Cancer: Impact on Prognosis and Benefit From Adjuvant Therapy. J Clin Oncol. 2020;38:3388–97. https://doi.org/10.1200/jco.20.00549.
Bosse T, Peters EE, Creutzberg CL, Jürgenliemk-Schulz IM, Jobsen JJ, Mens JW, Lutgens LC, van der Steen-Banasik EM, Smit VT, Nout RA. Substantial lymph-vascular space invasion (LVSI) is a significant risk factor for recurrence in endometrial cancer–A pooled analysis of PORTEC 1 and 2 trials. Eur J Cancer. 2015;51:1742–50. https://doi.org/10.1016/j.ejca.2015.05.015.
Han KH, Park N, Lee M, Lee C, Kim H. The new 2023 FIGO staging system for endometrial cancer: what is different from the previous 2009 FIGO staging system? J Gynecol Oncol. 2024. https://doi.org/10.3802/jgo.2024.35.e59.
Schwameis R, Fanfani F, Ebner C, Zimmermann N, Peters I, Nero C, Marth C, Ristl R, Leitner K, Grimm C, et al. Verification of the prognostic precision of the new 2023 FIGO staging system in endometrial cancer patients - An international pooled analysis of three ESGO accredited centres. Eur J Cancer. 2023;193:113317. https://doi.org/10.1016/j.ejca.2023.113317.
Gravbrot N, Weil CR, DeCesaris CM, Gaffney DK, Suneja G, Burt LM. Differentiation of survival outcomes by anatomic involvement and histology with the revised 2023 International Federation of Gynecology and Obstetrics staging system for endometrial cancer. Eur J Cancer. 2024;201:113913. https://doi.org/10.1016/j.ejca.2024.113913.
Leitao MM Jr. 2023 changes to FIGO endometrial cancer staging: Counterpoint. Gynecol Oncol. 2024;184:146–9. https://doi.org/10.1016/j.ygyno.2024.01.040.
McCluggage WG, Bosse T, Gilks CB, Howitt BE, McAlpine JN, Nucci MR, Rabban JT, Singh N, Talia KL, Parra-Herran C. FIGO 2023 endometrial cancer staging: too much, too soon? Int J Gynecol Cancer. 2023. https://doi.org/10.1136/ijgc-2023-004981.
Mendiola M, Heredia-Soto V, Ruz-Caracuel I, Baillo A, Ramon-Patino JL, Escudero FJ, Miguel M, Pelaez-Garcia A, Hernandez A, Feliu J, et al. Comparison of Methods for Testing Mismatch Repair Status in Endometrial Cancer. Int J Mol Sci. 2023;24. https://doi.org/10.3390/ijms241914468.
Rios-Doria E, Momeni-Boroujeni A, Friedman CF, Selenica P, Zhou Q, Wu M, Marra A, Leitao MM Jr, Iasonos A, Alektiar KM, et al. Integration of clinical sequencing and immunohistochemistry for the molecular classification of endometrial carcinoma. Gynecol Oncol. 2023;174:262–72. https://doi.org/10.1016/j.ygyno.2023.05.059.
Creutzberg CL, Nout RA, Lybeert ML, Wárlám-Rodenhuis CC, Jobsen JJ, Mens JW, Lutgens LC, Pras E, van de Poll-Franse LV, van Putten WL. Fifteen-year radiotherapy outcomes of the randomized PORTEC-1 trial for endometrial carcinoma. Int J Radiat Oncol Biol Phys. 2011;81:e631-638. https://doi.org/10.1016/j.ijrobp.2011.04.013.
Wortman BG, Creutzberg CL, Putter H, Jürgenliemk-Schulz IM, Jobsen JJ, Lutgens L, van der Steen-Banasik EM, Mens JWM, Slot A, Kroese MCS, et al. Ten-year results of the PORTEC-2 trial for high-intermediate risk endometrial carcinoma: improving patient selection for adjuvant therapy. Br J Cancer. 2018;119:1067–74. https://doi.org/10.1038/s41416-018-0310-8.
Di Donato V, Kontopantelis E, Cuccu I, Sgamba L, Golia D’Augè T, Pernazza A, Della Rocca C, Manganaro L, Catalano C, Perniola G, et al. Magnetic resonance imaging-radiomics in endometrial cancer: a systematic review and meta-analysis. Int J Gynecol Cancer. 2023;33:1070–6. https://doi.org/10.1136/ijgc-2023-004313.
Bogani G, Chiappa V, Lopez S, Salvatore C, Interlenghi M, D'Oria O, Giannini A, Leone Roberti Maggiore U, Chiarello G, Palladino S, et al. Radiomics and Molecular Classification in Endometrial Cancer (The ROME Study): A Step Forward to a Simplified Precision Medicine. Healthcare (Basel). 2022;10. https://doi.org/10.3390/healthcare10122464.
Concin N, Matias-Guiu X, Vergote I, Cibula D, Mirza MR, Marnitz S, Ledermann J, Bosse T, Chargari C, Fagotti A, et al. ESGO/ESTRO/ESP guidelines for the management of patients with endometrial carcinoma. Int J Gynecol Cancer. 2021;31:12–39. https://doi.org/10.1136/ijgc-2020-002230.
Stasenko M, Tunnage I, Ashley CW, Rubinstein MM, Latham AJ, Da Cruz Paula A, Mueller JJ, Leitao MM Jr, Friedman CF, Makker V, et al. Clinical outcomes of patients with POLE mutated endometrioid endometrial cancer. Gynecol Oncol. 2020;156:194–202. https://doi.org/10.1016/j.ygyno.2019.10.028.
Kandoth C, Schultz N, Cherniack AD, Akbani R, Liu Y, Shen H, Robertson AG, Pashtan I, Shen R, Benz CC, et al. Integrated genomic characterization of endometrial carcinoma. Nature. 2013;497:67–73. https://doi.org/10.1038/nature12113.
Laliscia C, Gadducci A, Coccia N, Mattioni R, Fuentes T, Caretto M, Pistolesi S, Puccini P, Perrone F, Morganti R, Paiar F. Lymph-vascular Space Involvement and/or p53 Overexpression Correlated With the Clinical Outcome of Early-stage Endometrial Cancer Patients Treated With Adjuvant Vaginal Brachytherapy. Anticancer Res. 2023;43:149–56. https://doi.org/10.21873/anticanres.16144.
Ayeni TA, Bakkum-Gamez JN, Mariani A, McGree ME, Weaver AL, Haddock MG, Keeney GL, Long HJ 3rd, Dowdy SC, Podratz KC. Comparative outcomes assessment of uterine grade 3 endometrioid, serous, and clear cell carcinomas. Gynecol Oncol. 2013;129:478–85. https://doi.org/10.1016/j.ygyno.2013.03.011.
Sakamoto I, Hirotsu Y, Amemiya K, Nozaki T, Mochizuki H, Omata M. Elucidation of genomic origin of synchronous endometrial and ovarian cancer (SEO) by genomic and microsatellite analysis. J Gynecol Oncol. 2023;34:e6. https://doi.org/10.3802/jgo.2023.34.e6.
Schultheis AM, Ng CK, De Filippo MR, Piscuoglio S, Macedo GS, Gatius S, Perez Mies B, Soslow RA, Lim RS, Viale A, et al. Massively Parallel Sequencing-Based Clonality Analysis of Synchronous Endometrioid Endometrial and Ovarian Carcinomas. J Natl Cancer Inst. 2016;108:djv427. https://doi.org/10.1093/jnci/djv427.
Cuccu I, Raspagliesi F, Malzoni M, Vizza E, Papadia A, Di Donato V, Giannini A, De Iaco P, Perrone AM, Plotti F, et al. Sentinel node mapping in high-intermediate and high-risk endometrial cancer: Analysis of 5-year oncologic outcomes. Eur J Surg Oncol. 2024;50:108018. https://doi.org/10.1016/j.ejso.2024.108018.
McConechy MK, Talhouk A, Li-Chang HH, Leung S, Huntsman DG, Gilks CB, McAlpine JN. Detection of DNA mismatch repair (MMR) deficiencies by immunohistochemistry can effectively diagnose the microsatellite instability (MSI) phenotype in endometrial carcinomas. Gynecol Oncol. 2015;137:306–10. https://doi.org/10.1016/j.ygyno.2015.01.541.
Streel S, Salmon A, Dheur A, Bours V, Leroi N, Habran L, Delbecque K, Goffin F, Pleyers C, Kakkos A, et al. Diagnostic Performance of Immunohistochemistry Compared to Molecular Techniques for Microsatellite Instability and p53 Mutation Detection in Endometrial Cancer. Int J Mol Sci. 2023;24. https://doi.org/10.3390/ijms24054866.
Kang N, Zhang X, Wang Z, Dai Y, Lu S, Su W, Gai F, Zhu C, Shen D, Wang J. Validation of a one-step genomics-based molecular classifier for endometrial carcinoma in a large Chinese population. Pathol Res Pract. 2024;254:155152. https://doi.org/10.1016/j.prp.2024.155152.
Rao Q, Liao J, Li Y, Zhang X, Xu G, Zhu C, Tian S, Chen Q, Zhou H, Zhang B. Application of NGS molecular classification in the diagnosis of endometrial carcinoma: A supplement to traditional pathological diagnosis. Cancer Med. 2023;12:5409–19. https://doi.org/10.1002/cam4.5363.
Wang C, Kuang W, Zeng J, Ren Y, Liu Q, Sun H, Feng M, Liang D. A retrospective study of consistency between immunohistochemistry and polymerase chain reaction of microsatellite instability in endometrial cancer. PeerJ. 2023;11:e15920. https://doi.org/10.7717/peerj.15920.
Riedinger CJ, Esnakula A, Haight PJ, Suarez AA, Chen W, Gillespie J, Villacres A, Chassen A, Cohn DE, Goodfellow PJ, Cosgrove CM. Characterization of mismatch-repair/microsatellite instability-discordant endometrial cancers. Cancer. 2024;130:385–99. https://doi.org/10.1002/cncr.35030.
Smithgall MC, Remotti H, Hsiao SJ, Mansukhani M, Liu-Jarin X, Fernandes H. Investigation of discrepant mismatch repair immunohistochemistry and microsatellite instability polymerase chain reaction test results for gynecologic cancers using next-generation sequencing. Hum Pathol. 2022;119:41–50. https://doi.org/10.1016/j.humpath.2021.10.004.
Juric D, Rodon J, Tabernero J, Janku F, Burris HA, Schellens JHM, Middleton MR, Berlin J, Schuler M, Gil-Martin M, et al. Phosphatidylinositol 3-Kinase α-Selective Inhibition With Alpelisib (BYL719) in PIK3CA-Altered Solid Tumors: Results From the First-in-Human Study. J Clin Oncol. 2018;36:1291–9. https://doi.org/10.1200/jco.2017.72.7107.
Myers AP, Konstantinopoulos PA, Barry WT, Luo W, Broaddus RR, Makker V, Drapkin R, Liu J, Doyle A, Horowitz NS, et al. Phase II, 2-stage, 2-arm, PIK3CA mutation stratified trial of MK-2206 in recurrent endometrial cancer. Int J Cancer. 2020;147:413–22. https://doi.org/10.1002/ijc.32783.
Shoji K, Oda K, Kashiyama T, Ikeda Y, Nakagawa S, Sone K, Miyamoto Y, Hiraike H, Tanikawa M, Miyasaka A, et al. Genotype-dependent efficacy of a dual PI3K/mTOR inhibitor, NVP-BEZ235, and an mTOR inhibitor, RAD001, in endometrial carcinomas. PLoS ONE. 2012;7:e37431. https://doi.org/10.1371/journal.pone.0037431.
Heudel P, Frenel JS, Dalban C, Bazan F, Joly F, Arnaud A, Abdeddaim C, Chevalier-Place A, Augereau P, Pautier P, et al. Safety and Efficacy of the mTOR Inhibitor, Vistusertib, Combined With Anastrozole in Patients With Hormone Receptor-Positive Recurrent or Metastatic Endometrial Cancer: The VICTORIA Multicenter, Open-label, Phase 1/2 Randomized Clinical Trial. JAMA Oncol. 2022;8:1001–9. https://doi.org/10.1001/jamaoncol.2022.1047.
Piha-Paul SA, Oh DY, Ueno M, Malka D, Chung HC, Nagrial A, Kelley RK, Ros W, Italiano A, Nakagawa K, et al. Efficacy and safety of pembrolizumab for the treatment of advanced biliary cancer: Results from the KEYNOTE-158 and KEYNOTE-028 studies. Int J Cancer. 2020;147:2190–8. https://doi.org/10.1002/ijc.33013.
Frenel JS, Le Tourneau C, O’Neil B, Ott PA, Piha-Paul SA, Gomez-Roca C, van Brummelen EMJ, Rugo HS, Thomas S, Saraf S, et al. Safety and Efficacy of Pembrolizumab in Advanced, Programmed Death Ligand 1-Positive Cervical Cancer: Results From the Phase Ib KEYNOTE-028 Trial. J Clin Oncol. 2017;35:4035–41. https://doi.org/10.1200/jco.2017.74.5471.
Bhatnagar AS, Brodie AM, Long BJ, Evans DB, Miller WR. Intracellular aromatase and its relevance to the pharmacological efficacy of aromatase inhibitors. J Steroid Biochem Mol Biol. 2001;76:199–202. https://doi.org/10.1016/s0960-0760(01)00050-4.
Chung YS, Woo HY, Lee JY, Park E, Nam EJ, Kim S, Kim SW, Kim YT. Mismatch repair status influences response to fertility-sparing treatment of endometrial cancer. Am J Obstet Gynecol. 2021;224:370.e371-370.e313. https://doi.org/10.1016/j.ajog.2020.10.003.
Covens AL, Filiaci V, Gersell D, Lutman CV, Bonebrake A, Lee YC. Phase II study of fulvestrant in recurrent/metastatic endometrial carcinoma: a Gynecologic Oncology Group study. Gynecol Oncol. 2011;120:185–8. https://doi.org/10.1016/j.ygyno.2010.10.015.
Moore AR, Rosenberg SC, McCormick F, Malek S. RAS-targeted therapies: is the undruggable drugged? Nat Rev Drug Discov. 2020;19:533–52. https://doi.org/10.1038/s41573-020-0068-6.
Dummer R, Schadendorf D, Ascierto PA, Arance A, Dutriaux C, Di Giacomo AM, Rutkowski P, Del Vecchio M, Gutzmer R, Mandala M, et al. Binimetinib versus dacarbazine in patients with advanced NRAS-mutant melanoma (NEMO): a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2017;18:435–45. https://doi.org/10.1016/s1470-2045(17)30180-8.
Sullivan RJ, Infante JR, Janku F, Wong DJL, Sosman JA, Keedy V, Patel MR, Shapiro GI, Mier JW, Tolcher AW, et al. First-in-Class ERK1/2 Inhibitor Ulixertinib (BVD-523) in Patients with MAPK Mutant Advanced Solid Tumors: Results of a Phase I Dose-Escalation and Expansion Study. Cancer Discov. 2018;8:184–95. https://doi.org/10.1158/2159-8290.Cd-17-1119.
Acknowledgements
Not applicable.
Funding
This study was supported by Shanghai Science and Technology Innovation Action Plan (No. 20Z11900703), and the Climb Grant of National Cancer Center (grant No. NCC201909B02).
Author information
Authors and Affiliations
Contributions
C.Y., X.Y., Q.Y., and Y.X. contributed to data collection, data analysis, and bioinformatics analysis, X.Z. and X.H. contributed to experimental technical support and data management, H.Y. and H.W. contributed to project administration, X.Z. and Y.R. contributed to conceptualization, manuscript revision. Y.R. contributed to funding acquisition. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the clinical ethics committee of Fudan University Shanghai Cancer Center, Fudan University. All patients had signed informed consent. This study was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration.
Consent for publication
Not appliable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yu, C., Yuan, X., Yao, Q. et al. Clinical application of FIGO 2023 staging system of endometrial cancer in a Chinese cohort. BMC Cancer 24, 862 (2024). https://doi.org/10.1186/s12885-024-12633-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12633-8