Abstract
Colorectal cancer is the leading cause of cancer death worldwide. The first and second lines of treatment for metastatic colorectal cancer (mCRC) include chemotherapy based on 5-fluorouracil. However, treatment following progression on the first and second line is still unclear. We searched PubMed, Scopus, Cochrane, and Web of Science databases for studies investigating the use of trifluridine-tipiracil with bevacizumab versus trifluridine-tipiracil alone for mCRC. We used RStudio version 4.2.3; and we considered p < 0.05 significant. Seven studies and 1,182 patients were included − 602 (51%) received trifluridine-tipiracil plus bevacizumab. Compared with control, the progression-free survival (PFS) (HR 0.52; 95% CI 0.42–0.63; p < 0.001) and overall survival (OS) (HR 0.61; 95% CI 0.52–0.70; p < 0.001) were significantly higher with bevacizumab. The objective response rate (ORR) (RR 3.14; 95% CI 1.51–6.51; p = 0.002) and disease control rate (DCR) (RR 1.66; 95% CI 1.28–2.16; p = 0.0001) favored the intervention. Regarding adverse events, the intervention had a higher rate of neutropenia (RR 1.38; 95% CI 1.19–1.59; p = 0.00001), whereas the monotherapy group had a higher risk of anemia (RR 0.60; 95% CI 0.44–0.82; p = 0.001). Our results support that the addition of bevacizumab is associated with a significant benefit in PFS, OS, ORR and DCR.
Graphical Abstract

Similar content being viewed by others
Introduction
Colorectal cancer (CRC) is one of the leading causes of cancer death, accounting for one in 10 cases, with an estimated 1,9 million new cases per year worldwide [1, 2]. Generally, first- and second-line treatment consists of fluorouracil-based chemotherapy with oxaliplatin and irinotecan, therapy targeting the vascular endothelial growth factor (VEGF) (mainly with Bevacizumab) or the epidermal growth factor receptor (EGFR) (the latter mainly in RAS wild-type tumors) [3,4,5,6]. When disease progression occurs after these therapies, patients are considered chemorefractory; however, as many of these patients perform well for treatment, they may be eligible for additional therapies, as progression-free survival is less than 2 months without additional therapy [7,8,9,10].
Trifluridine/tipiracil is an orally administered combination of trifluridine, a nucleic acid analog, and tipiracil, a thymidine phosphorylase inhibitor [11, 12]. Trifluridine is an active cytotoxic component that, inside neoplastic cells, is phosphorylated by thymidine kinase to form trifluridine triphosphate, which acts by incorporating itself into the cell DNA in place of thymine [13]. Thymidine phosphorylase is the enzyme responsible for the metabolism of trifluridine in the liver and gastrointestinal tract, transforming it into inactive forms; however, the addition of tipiracil to the combination is responsible for the total inhibition of this degradation, thus increasing the bioavailability of trifluridine [14, 15].
Continuous inhibition of angiogenesis, particularly with anti-VEGF antibodies, is an effective strategy for treating metastatic CRC [16, 17]. Bevacizumab, an anti-VEGF antibody, improved progression-free survival and overall survival in patients with metastatic CRC when added to first- or second-line chemotherapy [18]. More interestingly, the phase I/II C-TASK FORCE [19] study showed promising anti-tumor activity of TAS-102 (trifluridine/tipiracil) with bevacizumab in 25 colorectal cancer patients refractory to standard therapy. In this study, the median progression-free survival (PFS) was 5.6 months (95% CI; 3.4–7.6) and the median overall survival was 5.6 months (95% CI; 7.6–13.9). In contrast, these data are promising compared with those of large randomized trials that evaluated TAS-102 in monotherapy [20,21,22,23].
Thus, this meta-analysis clarified the real benefit of adding bevacizumab to trifluridine/tipiracil when compared directly with trifluridine/tipiracil in patients with chemorefractory metastatic CRC.
Methods
Protocol and registration
This systematic review adhered rigorously to the guidelines established by the Cochrane Collaboration and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Supplementary Tables 1 and 2) [24, 25]. To ensure transparency and reduce the risk of bias, the protocol was prospectively registered in the International Prospective Register of Systematic Reviews (PROSPERO) under the registration number CRD42024498571.
The studies were selected on the basis of the PICOT question, including studies in patients with chemorefractory metastatic colorectal cancer (P-population) taking bevacizumab plus trifluridine/tipiracil (I-intervention) or trifluridine/tipiracil monotherapy (C-control) to evaluate efficacy and safety (O-outcome). Thus, we sought to answer the following question: the addition of bevacizumab to trifluridine/tipiracil is effective and safe?
Eligibility criteria
Studies that met the following eligibility criteria were included: (1) clinical case-control and cohort studies; (2) trifluridine/tipiracil (35 mg/m² of body surface area) orally twice a day on days 1–5 and 8–12 in a 28-day cycle with or without bevacizumab (5 mg/kg of body weight) administered by intravenous infusion every 2 weeks; (3) patients ≥ 18 years of age with metastatic colorectal cancer; (4) refractory to fluoropyrimidine, irinotecan, and oxaliplatin; and (5) patients who have progressed to at least 1 line of treatment. We excluded studies with overlapping populations, case reports, reviews, editorials, conference abstracts, and studies with no outcomes of interest. Inclusion and exclusion criteria for the studies included in the systematic review and meta-analysis are detailed in Table S3.
Search strategy
PubMed, Cochrane Library, Scopus, and Web of Science were systematically searched on December 17, 2023. The detailed search strategy, utilizing MeSH terms, is provided in Table S4 of the Supplementary Material. To maximize capture of relevant studies, we went beyond the initial database search. Two reviewers (F.C.A.M. and F.D.D.L.P.) independently assessed the references of included articles and past systematic reviews. Additionally, we set up alerts in each database to automatically notify us of any newly published studies relevant to our inquiry. All identified articles, both from databases and reference lists, were imported into EndNote® X7 (Thomson Reuters, Philadelphia, USA) for reference management. We employed a combined approach of automated and manual methods to meticulously remove duplicate entries. Subsequently, both reviewers independently screened the titles and abstracts of retrieved articles. Should any discrepancies arise, consensus was achieved through discussions involving the two reviewers and the senior author (N.P.C.S.).
Data extraction
The following baseline characteristics were extracted: (1) ClinicalTrials.gov Identifier; (1) study design; (3) regimen details in the intervention and control arm (Supplementary Table S5); (4) number of patients allocated for each arm; and (5) main patient characteristics. The ensuing outcomes of interest were extracted: (1) PFS, defined as the time from patient randomization to disease progression or death from any cause; (2) OS, defined as the time from the start of treatment that patients are still alive; (3) Disease control rate (DCR), defined as the sum of complete response (CR), partial response (PR) and stable disease (SD); (4) Objective response rate (ORR), defined as the sum of CR and PR [26]; and (5) adverse events, defined as an unwanted effect of a treatment, which were evaluated by the Common Terminology Criteria for Adverse Events, version 5.0 [27]. Two authors (C.H.D.C.R. and F.D.D.L.P.) collected pre-specified baseline characteristics and outcome data. Where available, the full protocol of each study was consulted to verify study objectives, population, and other relevant information regarding study design and conduction. For publications reporting results from the same study, the most recent or complete publication reporting the information of interest was considered.
Endpoints and subgroup analysis
Outcomes of interest included: (1) PFS; (2) OS; (3) ORR; (4) DCR and patients with grade ≥ 3 of (5) neutropenia; (6) anemia; (7) thrombocytopenia; (8) nausea; (9) diarrhea; (10) vomiting; (11) fatigue and (12) febrile neutropenia.
Risk of bias assessment
To ensure objectivity and minimize individual bias, three independent reviewers (F.D.D.L.P., C.H.D.C.R., and F.C.A.M.) evaluated the risk of bias within each included randomized controlled trial. Any discrepancies were resolved through consensus discussions to achieve a unified judgment. The Cochrane Collaboration tool for assessing risk of bias in randomized trials (RoB 2) was utilized for quality assessment of individual randomized studies [28]. Each trial was assigned a score of high, low, or unclear risk of bias across five domains: randomization process, deviations from intended interventions, missing outcomes, measurement of outcomes, and selection of reported results. Non-randomized interventional studies were assessed through the Risk Of Bias In Non-randomized Studies of Interventions (ROBINS-I) tool [29], which contains seven domains and categorizes studies as having low, moderate, serious, critical, or unclear risk of bias. Funnel-plot analyses were employed to examine publication bias [30].
Statistical analysis
For time-to-event outcomes like progression-free survival (PFS) and overall survival (OS), we utilized the hazard ratio (HR) as the primary measure of effect. Higher HRs (> 1) favored the control group, indicating a greater risk of the event occurring in that group compared to the intervention group. Conversely, HRs less than 1 indicated a benefit associated with the intervention. For outcomes with binary endpoints, we employed risk ratios (RRs) alongside their corresponding 95% confidence intervals (CIs). These provided the relative risk of experiencing the event in one group compared to the other [31]. The Sidik-Jonkman estimator was used to calculate the tau2 variance between studies [32]. We used DerSimonian and Laird random-effect models for all endpoints [27]. Publication bias was explored using Egger’s linear regression test [33]. The packages used were “meta” and “metagen”. Statistical analyses were performed using R statistical software, version 4.2.3 (R Foundation for Statistical Computing).
Results
Search results and characteristics of included studies
The selection process is shown in detail in a PRISMA flow diagram (Fig. 1). Our systematic search identified a total of 790 references. After removing 249 duplicates and screening titles and abstracts for eligibility, we excluded 477 references and assessed 64 full-text manuscripts for inclusion and exclusion criteria. Of these, seven studies [34,35,36,37,38,39,40] met the criteria and were included in the analysis: two clinical trials and five retrospective cohort studies. These seven studies comprised a total of 1,182 patients.
A total of 602 patients with colorectal cancer were randomized to trifluridine-tipiracil plus bevacizumab and 580 patients to trifluridine-tipiracil monotherapy. The baseline characteristics of the included studies are summarized in Table 1. The median age ranged from 20 to 90 years. 663 (56.1%) patients were male and 519 (43.9%) were female. 1094 (92.5%) had an ECOG performance status of 0 or 1 and 31 (2,62%) had an ECOG ≥ 2. The primary tumor site of 683 (57.7%) patients was the left side and for 433 (36.6%) patients was the right side. 715 (60.5%) had one or two metastatic sites. The liver was affected in 305 (25.8%) patients, lung in 283 (23.9%), peritoneum in 100 (8.4%), lymph nodes in 71 (6.0%), and other sites in 38 (3.2%). RAS mutant-type was present in 720 (61%) patients and wild-type in 327 (27.6%). BRAF mutant-type was present in 39 (3.3%) patients and wild-type in 542 (45.8%). At least 1,063 (89.9%) patients received prior therapy with fluoropyrimidines, 1,054 (89.2%) received oxaliplatin; 1055 (89.3%) received irinotecan; 873 (73,9%) received at least one anti-VEGF agent, and 344 (29,1%) received at least one anti-EGFR agent in their previous treatment. The characteristics of the patients are summarized in Table 1 and Supplementary Table S6.
Results based on outcome
Progression-free survival
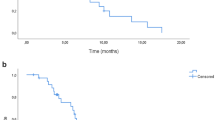
Among the 1,003 patients with metastatic colorectal cancer included in four studies, the estimated PFS significantly favored the trifluridine-tipiracil plus bevacizumab group (HR 0.52; 95% CI 0.42–0.63; p < 0.001; I²=49%; Fig. 2A).
Overall survival
Among 1,060 patients with chemorefractory metastatic colorectal cancer included from five studies, there was a significant difference from baseline in favor of the intervention with trifluridine/tipiracil plus bevacizumab group (HR 0.61; 95% CI 0.52–0.70; p < 0.001; I²=52%; Fig. 2B).
A Progression-free survival of patients with colorectal cancer treated with trifluridine-tipiracil plus bevacizumab versus trifluridine-tipiracil monotherapy. B Overall survival of patients with chemorefractory metastatic colorectal cancer treated with trifluridine-tipiracil plus bevacizumab versus trifluridine-tipiracil monotherapy
Objective response rate
Six studies were incorporated with a total of 1,125 patients. The intervention group with trifluridine-tipiracil plus bevacizumab exhibited a statistically significant advantage (RR 3.14; 95% CI 1.51–6.51; p = 0.002; I²=0%; Fig. 3A).
Disease control rate
Seven studies were incorporated with a total of 1,182 patients. A statistically significant superiority was observed for the bevacizumab intervention group (RR 1.66; 95% CI 1.28–2.16; p < 0.001; I²=55%; Fig. 3B).
A Objective response rate (ORR) of patients with chemorefractory metastatic colorectal cancer treated with trifluridine-tipiracil plus bevacizumab versus trifluridine-tipiracil monotherapy. B Disease control rate (DCR) of patients with colorectal cancer treated with trifluridine-tipiracil plus bevacizumab versus trifluridine-tipiracil monotherapy
Safety
Bevacizumab plus trifluridine-tipiracil significantly increased grade ≥ 3 of neutropenia (RR 1.38; 95% CI 1.19–1.59; p = 0.00001; I²=0%; Fig. S1A). In addition, trifluridine-tipiracil in monotherapy significantly increased grade ≥ 3 of anemia (RR 0.60; 95% CI 0.44–0.82; p = 0.001; I²=0%; Fig. S1H). There was no significant difference between the groups for grade ≥ 3 of diarrhea (RR 0.56; 95% CI 0.15–2.04; p = 0.37; I²=21%; Fig. S1D), fatigue (RR 0.50; 95% CI 0.20–1.23; p = 0.13; I²=10%; Fig. S1F), febrile neutropenia (RR 0.53; 95% CI 0.21–1.37; p = 0.19; I²=9%; Fig. S1G), nausea (RR 0.62; 95% CI 0.24–1.56; p = 0.30; I²=0%; Fig. S1C), thrombocytopenia (RR 1.48; 95% CI 0.72–3.04; p = 0.29; I²=0%; Fig. S1B), and vomiting (RR 0.75; 95% CI 0.25–2.21; p = 0.59; I²=0%; Fig. S1E). The hematological and non-hematological grade 3/4 adverse events are summarized in Table 2.
Sensitivity analyses
A leave-one-out sensitivity analysis was conducted focusing on progression-free survival (PFS), overall survival (OS), objective response rate (ORR), and disease control rate (DCR). The majority of outcomes exhibited low heterogeneity: ORR, anaemia, neutropenia, thrombocytopenia, nausea, and vomiting all demonstrated an I² of 0%; diarrhea exhibited an I² of 21%, fatigue an I² of 10%, and febrile neutropenia an I² of 9%. However, significant heterogeneity was observed in OS (I²=52%), PFS (I²=49%), and DCR (I²=55%). For OS, a notable reduction in heterogeneity was achieved by omitting the study by Fujii (2019) (HR 0.64; 95% CI 0.55–0.74; I²=0%; Fig. S2B). For PFS, a significant reduction in heterogeneity was observed upon the exclusion of Prager (2023) (HR 0.57; 95% CI 0.48–0.69; I²=8%; Fig. S2A). Nonetheless, no significant reduction in heterogeneity was noted when any of the analyzed studies were omitted for DCR (Fig. S2D).
Quality assessment
The individual assessment of each studies included in the meta-analysis is depicted in Figure S4. The analysis of the RCTs showed a low risk of bias. In the analysis of ROBINS-I for the non-randomized studies, only Kotani et al. (2019) and Fujii et al. (2020) showed moderate reliability, specifically in domains D1 and D6, respectively (Fig. S4C). The DCR funnel plot shows a low risk of bias for most of the included studies (Fig. 4).
Discussion
In this systematic review and meta-analysis involving 7 studies and 1,182 patients, we compared Trifluridine-Tipiracil plus Bevacizumab versus Trifluridine-Tipiracil Monotherapy in patients with metastatic colorectal cancer. The main results of the pooled analyses were as follows: (1) PFS was better in patients receiving trifluridine-tipiracil plus bevacizumab; (2) OS showed a significant difference in favor of the trifluridine-tipiracil plus bevacizumab group; (3) Clinical responses to treatment, such as ORR and DCR, were significantly beneficial in the bevacizumab group; and (3) adverse effects such as neutropenia and anemia were observed in both treatment groups.
Our results showed that combining bevacizumab with trifluridine-tipiracil significantly improved PFS compared with trifluridine-tipiracil monotherapy (HR 0.52; 95% CI 0.42–0.63; p < 0.001). These results are encouraging, particularly when compared with other gastrointestinal cancers treated with anti-angiogenic agents. The study conducted by Okunaka et al. [41] showed that the addition of ramucirumab (VEGF inhibitor) to trifluridine-tipiracil versus trifluridine-tipiracil monotherapy does not show a benefit for the PFS of patients with advanced gastric cancer (HR 0.66; 95% CI 0.43–1.03; p = 0.059).
Overall survival was significantly higher among patients who used bevacizumab instead of monotherapy (HR 0.61; 95% CI 0.52–0.70; p < 0.001). Similar to this, the addition of panitumumab, an anti-epidermal growth factor receptor (EGFR) monoclonal antibody (mAb), to chemotherapy with leucovorin, 5-fluorouracil, and oxaliplatin (FOLFOX) can significantly benefit patients with RAS-wild left-sided metastatic colorectal cancer compared with FOLFOX alone. The PRIME study reported a higher OS rate for this group (HR 0. 73; 95% CI 0.57–0.93; p = 0.011) [42, 43].
Patients in the bevacizumab group had a higher absolute ORR, with 5.14% (31) versus 1.37% (8); (RR 3.14; 95% CI 1.51–6.51; p = 0.002). These results suggest that the use of anti-VEGF antibody can generate substantial clinical responses to treatment. Similarly, a meta-analysis conducted by Tian et al. [44] showed that the use of anti-EGFR antibody in chemotherapy treatment with FOLFOXIRI (fluoracil, oxaliplatin and irinotecan) results in a higher ORR rate (RR 1.33; 95% CI; 1.13–1.58; P = 0.0009) compared with FOLFOXIRI alone.
In addition, bevacizumab therapy had a higher absolute DCR (RR 1.66; 95% CI 1.28–2.16; p = 0.0001). This association signals promising prospects for metastatic colorectal cancer, where the addition of new emerging therapies does not always result in an additive benefit. Thus, contrary to our results, the meta-analysis conducted by Zeng et al. [45] showed that the use of immunotherapy, particularly immune checkpoint inhibitors, in colorectal cancer does not seem to be associated with any benefit for DCR (OR 0.97; 95% CI 0.36–2.61; p = 0.95).
Adverse events associated with cancer treatment affect the physical and emotional well-being and quality of life and can compromise the activities of daily living of patients with colorectal cancer [46]. Although the incidence of adverse events is higher for most combination chemotherapies, only neutropenia was associated with the addition of bevacizumab (p = 0.00001); more interestingly, trifluridine–tipiracil monotherapy seems to have increased anemia in severe grades (p = 0.001), suggesting that bevacizumab could be protective for this adverse event.
This study has some limitations. First, the analysis was mainly based on observational and non-randomized studies, which may have influenced the effect size found in our results. However, the absence of heterogeneity in the pooled analysis of most of the results suggests that our meta-analysis conveys the best available evidence. Second, the studies had different patient follow-up times, which may have affected our results. However, despite the limitations presented, this did not prevent robust conclusions on efficacy and safety outcomes showing the potential benefit of bevacizumab combined with trifluridine-tipiracil.
Conclusion
This is the first meta-analysis to evaluate trifluridine–tipiracil plus bevacizumab versus trifluridine–tipiracil monotherapy for chemorefractory metastatic colorectal cancer. Our results support the notion that the addition of bevacizumab to trifluridine-tipiracil is associated with a significant improvement in PFS, OS, ORR, and DCR, suggesting the antitumor potential of this combination therapy.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
- BEV:
-
Bevacizumab
- BRAF:
-
BRAF gene
- CI:
-
Confidence Interval
- CR:
-
Complete Response
- CRC:
-
Colorectal Cancer
- DCR:
-
Disease Control Rate
- ECOG:
-
Eastern Cooperative Oncology Group
- EGFR:
-
Epidermal Growth Factor Receptor
- FOLFOX:
-
Leucovorin, 5-Fluorouracil, Oxaliplatin chemotherapy regimen
- GI:
-
Gastrointestinal. HR: Hazard Ratio
- I2 :
-
I squared statistic (measure of heterogeneity)
- MeSH:
-
Medical Subject Headings
- MAb:
-
Monoclonal Antibody
- ORR:
-
Objective Response Rate
- OS:
-
Overall Survival
- PFS:
-
Progression-Free Survival
- PR:
-
Partial Response
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
- PROSPERO:
-
International Prospective Register of Systematic Reviews
- RAS:
-
RAS gene
- RCT:
-
Randomized Controlled Trial
- RR:
-
Risk Ratio
- RECIST:
-
Response Evaluation Criteria for Solid Tumors
- ROBINS-I:
-
Risk of Bias in Non-randomized Studies - 1 tool
- RoB 2:
-
Risk of Bias tool 2
- USA:
-
United States of America
- VEGF:
-
Vascular Endothelial Growth Factor
References
Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics, 2023. CA Cancer J Clin. 2023;73:17–48.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72:7–33.
Cervantes A, Adam R, Roselló S, Arnold D, Normanno N, Taïeb J, et al. Metastatic colorectal cancer: ESMO clinical practice guideline for diagnosis, treatment and follow-up. Ann Oncol. 2023;34:10–32.
Benson AB, Venook AP, Al-Hawary MM, Arain MA, Chen Y-J, Ciombor KK, et al. Colon cancer, Version 2.2021, NCCN Clinical Practice guidelines in Oncology. J Natl Compr Canc Netw. 2021;19:329–59.
Sartore-Bianchi A, Trusolino L, Martino C, Bencardino K, Lonardi S, Bergamo F, et al. Dual-targeted therapy with trastuzumab and lapatinib in treatment-refractory, KRAS codon 12/13 wild-type, HER2-positive metastatic colorectal cancer (HERACLES): a proof-of-concept, multicentre, open-label, phase 2 trial. Lancet Oncol. 2016;17:738–46.
Tabernero J, Grothey A, Van Cutsem E, Yaeger R, Wasan H, Yoshino T, et al. Encorafenib Plus Cetuximab as a New Standard of Care for previously treated BRAF V600E-Mutant metastatic colorectal Cancer: updated survival results and subgroup analyses from the BEACON Study. J Clin Oncol. 2021;39:273–84.
Arnold D, Prager GW, Quintela A, Stein A, Moreno Vera S, Mounedji N, et al. Beyond second-line therapy in patients with metastatic colorectal cancer: a systematic review. Ann Oncol. 2018;29:835–56.
Mauri G, Gori V, Bonazzina E, Amatu A, Tosi F, Bencardino K, et al. Oxaliplatin retreatment in metastatic colorectal cancer: systematic review and future research opportunities. Cancer Treat Rev. 2020;91:102112.
Amatu A, Mauri G, Tosi F, Bencardino K, Bonazzina E, Gori V, et al. Efficacy of retreatment with oxaliplatin-based regimens in metastatic colorectal Cancer patients: the RETROX-CRC retrospective study. Cancers (Basel). 2022;14:1197.
Cremolini C, Rossini D, Dell’Aquila E, Lonardi S, Conca E, Del Re M, et al. Rechallenge for patients with RAS and BRAF wild-type metastatic colorectal cancer with acquired resistance to first-line cetuximab and irinotecan: a phase 2 single-arm clinical trial. JAMA Oncol. 2019;5:343–50.
Chan BM, Hochster HS, Lenz H-J. The safety and efficacy of trifluridine-tipiracil for metastatic colorectal cancer: a pharmacy perspective. Am J Health Syst Pharm. 2019;76:339–48.
Martinez-Perez J, Riesco-Martinez MC, Garcia-Carbonero R. The safety of trifluridine and tipiracil for the treatment of metastatic colorectal cancer. Expert Opin Drug Saf. 2018;17:643–50.
Falcone A, Ohtsu A, Van Cutsem E, Mayer RJ, Buscaglia M, Bendell JC, et al. Integrated safety summary for trifluridine/tipiracil (TAS-102). Anticancer Drugs. 2018;29:89–96.
Lee JJ, Chu E. Adherence, dosing, and managing toxicities with Trifluridine/Tipiracil (TAS-102). Clin Colorectal Cancer. 2017;16:85–92.
Voutsadakis IA. Biomarkers of trifluridine-tipiracil efficacy. J Clin Med. 2021;10:5568.
Otsu S, Hironaka S. Current status of angiogenesis inhibitors as second-line treatment for unresectable colorectal Cancer. Cancers (Basel). 2023;15:4564.
Lim SH, Cho HJ, Kim K-M, Lim HY, Kang WK, Lee J, et al. Comprehensive molecular analysis to predict the efficacy of chemotherapy containing bevacizumab in patients with metastatic colorectal cancer. Oncol Res. 2023;31:855–66.
Bennouna J, Sastre J, Arnold D, Österlund P, Greil R, Van Cutsem E, et al. Continuation of bevacizumab after first progression in metastatic colorectal cancer (ML18147): a randomised phase 3 trial. Lancet Oncol. 2013;14:29–37.
Kuboki Y, Nishina T, Shinozaki E, Yamazaki K, Shitara K, Okamoto W, et al. TAS-102 plus bevacizumab for patients with metastatic colorectal cancer refractory to standard therapies (C-TASK FORCE): an investigator-initiated, open-label, single-arm, multicentre, phase 1/2 study. Lancet Oncol. 2017;18:1172–81.
Mayer RJ, Van Cutsem E, Falcone A, Yoshino T, Garcia-Carbonero R, Mizunuma N, et al. Randomized trial of TAS-102 for refractory metastatic colorectal cancer. N Engl J Med. 2015;372:1909–19.
Yoshino T, Mizunuma N, Yamazaki K, Nishina T, Komatsu Y, Baba H, et al. TAS-102 monotherapy for pretreated metastatic colorectal cancer: a double-blind, randomised, placebo-controlled phase 2 trial. Lancet Oncol. 2012;13:993–1001.
Xu J, Kim TW, Shen L, Sriuranpong V, Pan H, Xu R, et al. Results of a Randomized, Double-Blind, Placebo-Controlled, phase III trial of Trifluridine/Tipiracil (TAS-102) monotherapy in Asian patients with previously treated metastatic colorectal Cancer: the TERRA Study. J Clin Oncol. 2018;36:350–8.
Van Cutsem E, Mayer RJ, Laurent S, Winkler R, Grávalos C, Benavides M, et al. The subgroups of the phase III RECOURSE trial of trifluridine/tipiracil (TAS-102) versus placebo with best supportive care in patients with metastatic colorectal cancer. Eur J Cancer. 2018;90:63–72.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Cochrane Handbook for Systematic Reviews of Interventions. https://training.cochrane.org/handbook. Accessed 14 Jan 2024.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
Common Terminology Criteria for Adverse Events (CTCAE). 2017.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
Chapter 13: Assessing risk of bias due to missing results in a synthesis. https://training.cochrane.org/handbook/current/chapter-13. Accessed 15 Sept 2023.
Chapter 13: Assessing risk of bias due to missing results in a synthesis | Cochrane Training. https://training.cochrane.org/handbook/current/chapter-13. Accessed 4 Nov 2023.
IntHout J, Ioannidis JPA, Borm GF. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Med Res Methodol. 2014;14:25.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Pfeiffer P, Yilmaz M, Möller S, Zitnjak D, Krogh M, Petersen LN, et al. TAS-102 with or without bevacizumab in patients with chemorefractory metastatic colorectal cancer: an investigator-initiated, open-label, randomised, phase 2 trial. Lancet Oncol. 2020;21:412–20.
Fujii H, Matsuhashi N, Kitahora M, Takahashi T, Hirose C, Iihara H, et al. Bevacizumab in Combination with TAS-102 improves clinical outcomes in patients with refractory metastatic colorectal Cancer: a retrospective study. Oncologist. 2020;25:e469–76.
Kotani D, Kuboki Y, Horasawa S, Kaneko A, Nakamura Y, Kawazoe A, et al. Retrospective cohort study of trifluridine/tipiracil (TAS-102) plus bevacizumab versus trifluridine/tipiracil monotherapy for metastatic colorectal cancer. BMC Cancer. 2019;19:1253.
Nie C, Xu W, Chen B, Lv H, Wang J, Liu Y, et al. An exploration of Trifluridine/Tipiracil Monotherapy and in Combination with Bevacizumab or Immune Checkpoint inhibitors for patients with metastatic colorectal Cancer: a real-world study. Clin Colorectal Cancer. 2023;22:76–84.
Prager GW, Taieb J, Fakih M, Ciardiello F, Van Cutsem E, Elez E, et al. Trifluridine-tipiracil and Bevacizumab in Refractory Metastatic Colorectal Cancer. N Engl J Med. 2023;388:1657–67.
Chida K, Kotani D, Nakamura Y, Kawazoe A, Kuboki Y, Shitara K, et al. Efficacy and safety of trifluridine/tipiracil plus bevacizumab and trifluridine/tipiracil or regorafenib monotherapy for chemorefractory metastatic colorectal cancer: a retrospective study. Ther Adv Med Oncol. 2021;13:17588359211009143.
Shibutani M, Nagahara H, Fukuoka T, Iseki Y, Wang EN, Okazaki Y, et al. Combining Bevacizumab with Trifluridine/Thymidine phosphorylase inhibitor improves the survival outcomes regardless of the usage history of Bevacizumab in Front-line treatment of patients with metastatic colorectal Cancer. Anticancer Res. 2020;40:4157–63.
Okunaka M, Kawazoe A, Nakamura H, Kotani D, Mishima S, Kuboki Y, et al. Efficacy and safety of trifluridine/tipiracil plus ramucirumab in comparison with trifluridine/tipiracil monotherapy for patients with advanced gastric cancer-single institutional experience. Gastric Cancer. 2023;26:1030–9.
Douillard J-Y, Oliner KS, Siena S, Tabernero J, Burkes R, Barugel M, et al. Panitumumab-FOLFOX4 treatment and RAS mutations in colorectal cancer. N Engl J Med. 2013;369:1023–34.
Boeckx N, Koukakis R, Op de Beeck K, Rolfo C, Van Camp G, Siena S, et al. Primary tumor sidedness has an impact on prognosis and treatment outcome in metastatic colorectal cancer: results from two randomized first-line panitumumab studies. Ann Oncol. 2017;28:1862–8.
Tian M, Li H, Dong W, Li Y, Jiang T, Lv Y, et al. Triplet-drug chemotherapy combined with anti-EGFR antibody as an effective therapy for patients with initially unresectable metastatic colorectal cancer: a meta-analysis. World J Surg Oncol. 2023;21:355.
Zeng T, Fang X, Lu J, Zhong Y, Lin X, Lin Z, et al. Efficacy and safety of immune checkpoint inhibitors in colorectal cancer: a systematic review and meta-analysis. Int J Colorectal Dis. 2022;37:251–8.
Bakkerus L, Buffart LM, Buffart TE, Meyer YM, Zonderhuis BM, Haasbeek CJA, et al. Health-related quality of life in patients with metastatic colorectal Cancer undergoing systemic therapy with or without maximal tumor debulking. J Natl Compr Canc Netw. 2023;21:1059-e10665.
Acknowledgements
We thank the Federal University of Pará (UFPA); the Center for Research Oncology (NPO/UFPA). The design of the study, sample collection, data analysis, interpretation, and manuscript writing were conducted independently of any influence or involvement from the funding agencies.
Funding
This research was funded by the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq). Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), the Pró-Reitoria de Pesquisa e Graduação da UFPA (PROPESP).
Author information
Authors and Affiliations
Contributions
Theoretical conceptualization, F.C.A.M.; idealization, F.C.A.M.; literature searching, F.D.D.L.P., F.C.A.M. and C.H.D.C.R. ; investigation, F.C.A.M. and F.D.D.L.P.; data curation, C.H.D.C.R., F.D.D.L.P. and F.C.A.M.; statistical analysis, F.C.A.M. and C.H.D.C.R.; contextualization, F.C.A.M.; methodology, F.C.A.M.; elaboration of draft, F.C.A.M., C.H.D.C.R., and F.D.D.L.P.; preparation of the original writing, F.C.A.M., C.H.D.C.R., and F.D.D.L.P.; adjustments rules and preparation of the original script, F.C.A.M., M.R.F., N.P.C.S., C.H.D.C.R., and F.D.D.L.P.; review, M.R.F., R.M.R.B. and N.P.C.S. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Aquino de Moraes, F.C., Dantas Leite Pessôa, F.D., Duarte de Castro Ribeiro, C.H. et al. Trifluridine–tipiracil plus bevacizumab versus trifluridine–tipiracil monotherapy for chemorefractory metastatic colorectal cancer: a systematic review and meta-analysis. BMC Cancer 24, 674 (2024). https://doi.org/10.1186/s12885-024-12447-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12447-8