Abstract
Background
Definitive concurrent chemoradiotherapy (dCCRT) is the gold standard for the treatment of locally advanced esophageal squamous cell carcinoma (ESCC). However, the potential benefits of consolidation chemotherapy after dCCRT in patients with esophageal cancer remain debatable. Prospective randomized controlled trials comparing the outcomes of dCCRT with or without consolidation chemotherapy in patients with ESCC are lacking. In this study, we aim to generate evidence regarding consolidation chemotherapy efficacy in patients with locally advanced, inoperable ESCC.
Methods
This is a multicenter, prospective, open-label, phase-III randomized controlled trial comparing non-inferiority of dCCRT alone to consolidation chemotherapy following dCCRT. In total, 600 patients will be enrolled and randomly assigned in a 1:1 ratio to receive either consolidation chemotherapy after dCCRT (Arm A) or dCCRT alone (Arm B). Overall survival will be the primary endpoint, whereas progression-free survival, locoregional progression-free survival, distant metastasis-free survival, and treatment-related toxicity will be the secondary endpoints.
Discussion
This study aid in further understanding the effects of consolidation chemotherapy after dCCRT in patients with locally advanced, inoperable ESCC.
Trial registration
ChiCTR1800017646.
Similar content being viewed by others
Background
Esophageal cancer is the eighth most prevalent cancer and the sixth leading cause of cancer-related deaths globally [1]. In China, among all cancers, esophageal cancer has the highest morbidity and mortality rates, respectively [2]. More than 90% of patients with esophageal cancer in China demonstrate squamous cell carcinoma accounts; in contrast, esophageal adenocarcinoma is frequently observed in Western countries [3]. For nearly two decades, definitive concurrent chemoradiotherapy (dCCRT) has been the gold-standard treatment for locally advanced, inoperable ESCC [4].
The RTOG 85-01 trial established the standard pattern of dCCRT for esophageal cancer [5]. In this trial, dCCRT group patients received radiotherapy in combination with two cycles of concurrent chemoradiotherapy (CCRT; cisplatin and 5-fluorouracil), followed by two cycles of consolidation chemotherapy (cisplatin and 5-fluorouracil). These results confirmed the efficacy of dCCRT in treating locally advanced esophageal carcinoma [5]. When using combined chemoradiotherapy, subsequent studies have widely adopted the treatment regimen of two cycles of CCRT followed by another two cycles of consolidation chemotherapy. Despite significant advancements in combined treatment modalities, locoregional recurrence remains the prevailing pattern of post-dCCRT recurrence in patients with esophageal cancer, with 2-year local recurrence rates ranging from 43% to 58% [4, 6,7,8,9]. The rationale for consolidation chemotherapy in dCCRT is also based on the hypothesis that the earlier the non–cross-resistant agents are used, the higher is the likelihood of increased cancer cell death [10]. Nevertheless, the efficacy of consolidation chemotherapy after dCCRT in ESCC management has not been assessed through randomized trials. Only a few retrospective studies have compared the effectiveness of dCCRT with or without subsequent consolidation chemotherapy [11,12,13]. Chen et al. reported that the consolidation chemotherapy following dCCRT did not yield significant progression-free survival (PFS; 25.4 vs. 23.0 months, P = 0.49) and OS (35 vs. 34.6 months, P = 0.9) improvements in patients with ESCC [11]. However, Adenis et al. asserted that patients who receive consolidation chemotherapy after dCCRT tend to have improved median overall survival (OS; 20.1 vs. 9.9 months) and 3-year OS rate (26.4% vs. 15.5%) [13]. Nonetheless, the bias and the sample size variance in these retrospective studies have led to this issue remaining debatable. Furthermore, Wu et al. also showed that patients with ESCC did not benefit from the consolidation chemotherapy after dCCRT on both PFS and OS [12]. In the context of relevant data scarcity, a prospective non-inferiority randomized trial investigating the impact of consolidation chemotherapy after dCCRT in patients with ESCC is urgently needed.
Rationale
To the best of our knowledge, the use of consolidation chemotherapy following dCCRT for locally advanced, inoperable ESCC was first reported over two decades previously. Furthermore, despite advancements in intensity-modulated radiotherapy technology (IMRT), dependable evidence substantiating the efficacy of consolidation chemotherapy is lacking. According to the limited evidence reported thus far, compared with dCCRT alone, consolidation chemotherapy after dCCRT does not provide a significant survival benefit in patients with locally advanced, inoperable ESCC. As such, this will be the first multicenter, prospective, phase III randomized controlled trial to provide strong evidence regarding the efficacy of consolidation chemotherapy following dCCRT in patients with inoperable ESCC.
Methods
Study design
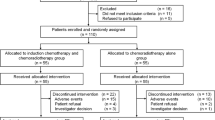
This will be a prospective, two-arm, phase III randomized controlled trial aimed at assessing non-inferiority of dCCRT alone to consolidation chemotherapy following dCCRT in patients with locally advanced, inoperable ESCC. Each patient will be randomly assigned at a 1:1 ratio to receive either consolidation chemotherapy after dCCRT (Arm A) or dCCRT alone (Arm B; Fig. 1).
Randomization was stratified by tumor location (cervical V thoracic) and tumor stage (II V III V IV). Written informed consent will be obtained from all patients before participation in this trial. All participating medical centers are well-experienced in radiotherapy and chemotherapy delivery.
Target population
Male and female patients with histologically proven ESCC who provide their written informed consent are eligible for this trial. The principal investigator will thoroughly evaluate and confirm that patients fulfill all the inclusion criteria.
Sample size considerations
The sample size is based on data from a retrospective study [11] and a phase III randomized controlled trial [14]—which suggested that dCCRT yields 2-year OS rates of ≥60% and 56%, respectively. Therefore, we hypothesized that consolidation chemotherapy after dCCRT (Arm A) and dCCRT alone (Arm B) will yield 2-year OS rates of approximately 60% and 48%–65%, respectively. According to Power Analysis and Sample Size (version 15.0), these rates will be obtained with a two-sided type I error of 5% with 90% power, a type II error (β) of 20% with 15% noninferiority margin, and a dropout rate related to dCCRT or loss to follow-up of 5%. Therefore, the final sample size will be 600, with a 1:1 allocation in each arm.
Inclusion criteria
-
1.
Being aged 18–75 years
-
2.
Having an Eastern Cooperative Oncology Group performance status of 0-2
-
3.
Having histologically proven ESCC
-
4.
Having a pretreatment stage of cT2N0M0-cTxNxM1a-1b (according to the 6th edition of AJCC/UICC TNM staging system, excluding metastasis beyond the supraclavicular or celiac lymph node and distant organ metastasis)
-
5.
Surgically unresectable.
-
6.
Not having prior chemotherapy or radiotherapy history and not being enrolled in other clinical trials
-
7.
Having adequate organ function (white blood cell count ≥ 3 × 109/L; neutrophil count ≥ 1.5 × 109/L; hemoglobin level ≥ 90g/L; platelet count ≥ 100 × 109/L; total bilirubin level ≤ 1.5 × upper limit of normal (ULN); aspartate transaminase level ≤ 2.5 × ULN; alanine transaminase level ≤ 2.5 × ULN; serum creatinine level ≤ 1.5 × ULN)
-
8.
Having a life expectancy of ≥3 months
-
9.
Providing written informed consent.
Exclusion criteria
-
1.
Having a past or current history of another malignant disease, except completely treatable nonmelanoma skin cancer and cervical carcinoma in situ (with PFS ≥ 3 years).
-
2.
Having an uncontrolled cardiac disease (e.g., myocardial infarction within the previous 6 months and coronary artery disease), diabetes, or hypertension.
-
3.
Having a severe mental disorder
-
4.
Being pregnant or lactating
-
5.
Having a tumor invading the airway or aorta
-
6.
Having complete obstruction due to esophageal cancer, signs of esophageal perforation or bleeding, or already developing perforation and bleeding
-
7.
Receiving oral or intravenous corticosteroids
-
8.
Having dysfunction in major organs, such as the liver, kidneys, heart, and lungs, immune deficiency, or active infection
-
9.
Having other possibly ineligible conditions based on the researchers’ judgment
Exit criteria
-
1.
Cancer progression
-
2.
Request to withdraw from the trial
-
3.
Development of grade 4 or higher nonhematologic toxicity (according to Common Terminology Criteria for Adverse Events (CTCAE; version 4.0), which could not reduce grade 2 or after treatment) or development of serious adverse events.
-
4.
Interruption in radiotherapy for >2 weeks for any reasons
-
5.
No treatment initiation for 4 weeks after enrollment
-
6.
Development of possibly ineligible conditions based on the researchers’ judgment
Study interventions
Chemotherapy
CCRT (Both arms)
All patients will receive two cycles of chemotherapy (cisplatin: 75 mg/m2/day, IVGTT, day 1; capecitabine: 800 mg/m2/day, bid, PO, d1–14) every 3 weeks during radiotherapy.
Consolidation chemotherapy (Arm A)
After CCRT, patients in arm A will receive two cycles of consolidation chemotherapy (cisplatin: 75 mg/m2/day, IVGTT, day 1; capecitabine: 1000 mg/m2/day, bid, PO, d1–14) every 3 weeks.
Observation group (Arm B)
Patients in arm B will receive no interventions.
Radiotherapy
The treatment plan is shown in Fig. 1. Radiation will be delivered with ≥6-MV photons 5 days per week to administer a total dose of 59.4 Gy in 33 fractions. All patients will be placed in the treatment position in an individualized immobilization device, and IMRT will be used.
The definition of volumes will be in accordance with the Report 50 (1993) and Report 62 (1999) of the International Commission on Radiation Units & Measurements (ICRU). The gross target volume (GTV) is defined as the gross demonstrable location and extent of the tumor, detected through endoscopic ultrasound, barium swallow x-ray, or computed tomography (CT) (whichever is larger). A regional lymph node with a diameter of ≥1 cm (for cervical, mediastinal, or celiac lymph nodes) or 0.5 cm (for tracheoesophageal groove lymph nodes) or that proven to be metastatic through positron emission tomography (PET)–CT will be defined as a GTVnd. Involved-field irradiation will be adopted when defining the clinical target volume (CTV). The CTV encompasses the GTV and the region draining the lymphatics, which will be defined as follows: a 3-cm craniocaudal margin, a 0.5–0.8-cm lateral margin beyond the GTV, and a GTVnd with a 1–1.5cm margin, including the metastatic lymph nodes. The PGTV is at 1 cm craniocaudally beyond the GTV and 0.5cm radially and the GTVnd. The planning target volume (PTV) will be defined as the CTV plus a 0.5–0.7cm expansion. Patients will be treated typically with daily fractions of 1.8 Gy to a total initial dose of 50.4 Gy to the PTV, followed by a cone down of 9 Gy to a total dose of 59.4 Gy to the PGTV.
The treatment plan will consider normal organ dose constraints as follows: The volume of lung tissue receiving ≥20 Gy should be <28% of the total lung volume, and the mean dose has to be <18 Gy. For the spinal cord, the maximal point dose should be <45 Gy. The volume of the heart receiving ≥30 Gy radiation must be <40% of the total heart volume, and the mean dose should be <26 Gy. The PTV and the organ at risk will be assessed using a dose–volume histogram.
Dose modifications
Radiotherapy interruption
In patients who develop grade 3 or higher hematological or nonhematological toxicity, radiotherapy will be delayed until the toxicity grade decreases to ≤2. At most, a 2-week delay will be permitted. Patients with a longer delay will be excluded from the trial.
Chemotherapy interruption
Chemotherapy dose modifications will be based on the most severe toxicity in the patients' last cycle. In patients who develop grade 2 or higher hematological toxicity, chemotherapy will be delayed until the toxicity grade decreases to ≤1. At most, a 2-week delay will be permitted. Patients with a longer delay will be excluded from the trial and asked to discontinue chemotherapy.
Chemotherapy dose modifications may be required in the following situation: a patient develops grade 4 hematological toxicity or grade 3 or higher nonhematological toxicity, but the toxicity grade decreases to ≤1 within 2 weeks before the next cycle. Patients who remain ineligible after this period will be asked to discontinue chemotherapy.
If modification is necessary, cisplatin and capecitabine doses will be reduced to 75% of the planned dose. Dose modifications may be made at most twice; if more than two modifications are required, chemotherapy will be terminated.
Study objectives
The main objective of this trial is to compare OS in ESCC patients treated with or without consolidation chemotherapy after dCCRT. Our secondary objectives are to compare PFS, locoregional PFS (LPFS), distant metastasis-free survival (DMFS), and treatment-related toxicity.
OS is defined as the time from the date of dCCRT initiation until the date of death. PFS is defined as the time from the date of dCCRT until the date of first progression or death. LPFS is defined as the time from the date of dCCRT until the date of first locoregional progression (a primary tumor or locoregional lymph nodes) or death. DMFS is defined as the time from the date of dCCRT until the date of first distant metastasis (nonregional lymph nodes or a distant organ) or death.
Pretherapeutic assessments
Before administering any treatment, we will perform routine examination and record its results for every potential patient. The routine examination will include the following:
-
1.
A physical examination, as well as vital sign and medical history taking
-
2.
Karnofsky performance status and Eastern Cooperative Oncology Group performance status
-
3.
Standard laboratory tests (routine complete blood count and blood biochemistry), pulmonary function test, and electrocardiography
-
4.
Upper digestive tract endoscopy with biopsy
-
5.
CT of the thorax or PET–CT; magnetic resonance imaging (MRI) of the esophagus, endoscopic ultrasound of the esophagus, or both; brain MRI (if needed); whole-body bone emission CT (if required); or CT or ultrasound of the neck and abdomen
-
6.
European Organisation for Research and Treatment of Cancer quality of life
Assessments during the treatment phase
The outcomes of physical examinations, vital signs, routine complete blood count, blood biochemistry, and radiotherapy-related pulmonary and esophageal toxicity will be recorded weekly during the dCCRT period, according to CTCAE (version 4.0). Changes in esophageal wall thickness and lymph node size (if needed) will be evaluated through contrast-enhanced CT of the neck, thorax, and abdomen. Changes in the esophageal tract will be assessed through contrast-enhanced CT of the upper gastrointestinal tract. The residual primary tumor will be evaluated through upper endoscopy followed by biopsy. Local tumors, locoregional lymph nodes, and distant metastases will be assessed through PET–CT. After 2–6 weeks of dCCRT, patients without disease progression will be randomized at a 1:1 ratio to arm A or B by a central randomization center; moreover, patients demonstrating disease progression will be excluded from the study.
Assessments during the follow-up phase
After completion of the study treatment, patients will be followed up every 3 months for the first 2 years and then every 6 months from the third year onward. All patients will be followed up until death or at least 3 years after treatment.
Statistical analysis
Data analyses will be performed according to the intention-to-treat principle in all randomized patients. Between-group comparisons will be performed using chi-squared and Fisher’s exact test for categorical parameters and Student’s t test for normally distributed continuous variables or the Mann–Whitney U test or analysis of variance for nonnormally distributed continuous variables. Survival rates will be calculated using the Kaplan-Meier method, and comparisons between the groups will be performed using the log-rank test. The difference will be considered statistically significant at a P value of <0.05.
Funding and current status
Our study has been approved by the Medical Ethics Committee of Henan Cancer Hospital (2018087) and supported by the Health Commission of Henan Province (182106000062). Moreover, the funding body has peer-reviewed the study protocol.
Our study commenced on July 27, 2018. Currently, it remains in the patient recruitment stage. Since August 1, 2018. 200 patients have been recruited.
Discussion
Numerous trials have reported that compared with radiotherapy alone, dCCRT can significantly reduce treatment failure and prolong survival in patients with esophageal cancer [4,5,6, 14,15,16]. However, a majority of these trials have primarily included populations from Western countries, where esophageal adenocarcinoma is more prevalent than ESCC. In contrast, ESCC is the predominant histological type of esophageal cancer in China [2]. Therefore, exploring alternative treatment approaches specifically targeting ESCC is warranted.
Consolidation chemotherapy is defined as the prolongation of chemotherapy duration by the administration of additional drugs at the end of a defined number of initial chemotherapy cycles, after the achievement of maximum tumor response, in individual patients [17]. According to the RTOG 85-01 trial, the most adopted dCCRT scheme includes two cycles of consolidation chemotherapy after dCCRT [5]. However, the specific role and rationale for incorporating consolidation chemotherapy remain undefined; nevertheless, incorporating consolidation chemotherapy may reduce the likelihood of distant metastases and ultimately improve OS. Thus far, only a few retrospective studies have focused on consolidation chemotherapy. For instance, Chen et al. and Wu et al. have demonstrated that consolidation chemotherapy does not yield significant improvements in disease control or PFS in patients with ESCC. In contrast, Adenis et al. suggested that patients who undergo consolidation chemotherapy tend to have prolonged OS [11,12,13]. Furthermore, Wang et al. compared the potential survival advantages of consolidation chemotherapy and dCCRT alone in patients diagnosed as having unresectable esophageal cancer; the authors revealed a short-term survival benefit and a reduced likelihood of distant metastasis [18]. Similarly, Lin et al. and Xia et al. observed that consolidation chemotherapy is strongly associated with prolonged OS in ESCC patients undergoing dCCRT [19, 20]. However, the results observed across the aforementioned studies have been heterogeneous; therefore, additional prospective randomized controlled trials validating the benefits of consolidation chemotherapy in patients with ESCC are needed urgently.
The incidence rate of local recurrence among esophageal cancer patients who undergo dCCRT can be 43%–58%, and this recurrence can significantly reduce the patients' long-term survival rates [7,8,9]. Recent studies have suggested that LPFS of ESCC patients receiving dCCRT with a higher radiation dose (≥59.4Gy) and those receiving dCCRT with a standard radiation dose (50 Gy/2 Gy or 50.4 Gy/1.8 Gy) is comparable [21, 22]. The standard radiation dose for dCCRT is 50 Gy, as indicated in the RTOG 85-01 trial [5]. However, Chang et al. noted that a higher dose of radiation (≥60 Gy) may prolong survival [23]. This finding was further supported by another study [24]—which also indicated that a higher dose may enhance local control. Nevertheless, recent randomized studies have demonstrated that in dCCRT for ESCC, the standard radiation dose (50 Gy/2 Gy or 50.4 Gy/1.8 Gy) has an effect similar to that of a higher radiation dose (≥59.4 Gy/1.8 Gy) but with relatively less treatment-related toxicity [21, 22, 25, 26]. Consequently, in future clinical practice, the standard radiation dose should be recommended for dCCRT in patients with ESCC.
Although several studies have analyzed the effects of different CCRT regimens, none have demonstrated considerably improved treatment efficacy or substantially decreased toxicity [15, 16, 27,28,29,30]. 5-Fluorouracil plus cisplatin has been used as a standard regimen in many dCCRT studies after the RTOG 85-01 trial [5, 6, 31,32,33]. This chemotherapy regimen achieves a curative effect but with serious treatment toxicity, such as severe myelosuppression and mucositis [5]. In three trials (including the SCOPE1 trial), capecitabine, an oral prodrug of 5-fluorouracil, demonstrated a high complete remission rate with acceptable toxicity [28, 29]. Therefore, capecitabine plus cisplatin may be a more acceptable candidate for subsequent dCCRT trials [14, 34, 35]. Some trials have also explored the efficacy of other chemotherapy regimens in dCCRT, such as paclitaxel plus carboplatin and the FOLFOX regimen [15, 17, 36] and 5-fluorouracil plus paclitaxel [30]. However, none of the aforementioned regimens demonstrates relatively high efficacy or relatively less toxicity.
Even though dCCRT remains the predominant treatment modality for esophageal cancer patients, high-level evidence regarding the use of consolidation chemotherapy for patients with ESCC is highly insufficient. To date, no prospective study has compared the outcomes of dCCRT with or without consolidation chemotherapy in patients with ESCC. Nevertheless, the current prospective randomized controlled trial will aid in understanding whether consolidation chemotherapy after dCCRT yields relatively superior benefits in patients with locally advanced, inoperable ESCC.
In conclusion, our study will be a multicenter, prospective, open-label, phase III randomized controlled trial to investigate the efficacy and safety of consolidation chemotherapy following dCCRT in patients with inoperable ESCC. The study will make valuable contributions to the evidence regarding the effects of consolidation chemotherapy for esophageal cancer in China.
Availability of data and materials
This article has used no dataset. Therefore, no additional data files are available.
Abbreviations
- dCCRT:
-
Definitive concurrent chemoradiotherapy
- ESCC:
-
Esophageal squamous cell carcinoma
- PFS:
-
Progression-free survival
- LPFS:
-
Locoregional PFS
- DMFS:
-
Distant metastasis-free survival
- OS:
-
Overall survival
- IMRT:
-
Intensity-modulated radiotherapy technology
- AJCC:
-
American joint committee on cancer
- UICC:
-
International union against cancer
- ULN:
-
Upper limit of normal
- CTCAE:
-
Common Terminology Criteria for Adverse Events
- PO:
-
Peros
- IVGGT:
-
Intravenously guttae
- ICRU:
-
International Commission on Radiation Units & Measurements
- GTV:
-
Gross target volume
- CTV:
-
Clinical target volume
- PTV:
-
Planning target volume
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
References
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359-86.
Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–32.
Liang H, Fan JH, Qiao YL. Epidemiology, etiology, and prevention of esophageal squamous cell carcinoma in China. Cancer Biol Med. 2017;14(1):33–41.
Herskovic A, Martz K, al-Sarraf M, Leichman L, Brindle J, Vaitkevicius V, et al. Combined chemotherapy and radiotherapy compared with radiotherapy alone in patients with cancer of the esophagus. N Engl J Med. 1992;326(24):1593–8.
Cooper JS, Guo MD, Herskovic A, Macdonald JS, Martenson JA Jr, Al-Sarraf M, et al. Chemoradiotherapy of locally advanced esophageal cancer: long-term follow-up of a prospective randomized trial (RTOG 85–01). Radiation Therapy Oncology Group. JAMA. 1999;281(17):1623–7.
Minsky BD, Pajak TF, Ginsberg RJ, Pisansky TM, Martenson J, Komaki R, et al. INT 0123 (Radiation Therapy Oncology Group 94–05) phase III trial of combined-modality therapy for esophageal cancer: high-dose versus standard-dose radiation therapy. J Clin Oncol. 2002;20(5):1167–74.
Chiu PW, Chan AC, Leung SF, Leong HT, Kwong KH, Li MK, et al. Multicenter prospective randomized trial comparing standard esophagectomy with chemoradiotherapy for treatment of squamous esophageal cancer: early results from the Chinese University Research Group for Esophageal Cancer (CURE). J Gastrointest Surg. 2005;9(6):794–802.
Bedenne L, Michel P, Bouche O, Milan C, Mariette C, Conroy T, et al. Chemoradiation followed by surgery compared with chemoradiation alone in squamous cancer of the esophagus: FFCD 9102. J Clin Oncol. 2007;25(10):827–34.
Stahl M, Stuschke M, Lehmann N, Meyer HJ, Walz MK, Seeber S, et al. Chemoradiation with and without surgery in patients with locally advanced squamous cell carcinoma of the esophagus. J Clin Oncol. 2005;23(10):2310–7.
Grossi F, Aita M, Follador A, Defferrari C, Brianti A, Sinaccio G, et al. Sequential, alternating, and maintenance/consolidation chemotherapy in advanced non-small cell lung cancer: a review of the literature. Oncologist. 2007;12(4):451–64.
Chen Y, Guo L, Cheng X, Wang J, Zhang Y, Wang Y, et al. With or without consolidation chemotherapy using cisplatin/5-FU after concurrent chemoradiotherapy in stage II-III squamous cell carcinoma of the esophagus: a propensity score-matched analysis. Radiother Oncol. 2018;129(1):154–60.
Wu SX, Li XY, Xu HY, Xu QN, Luo HS, Du ZS, et al. Effect of consolidation chemotherapy following definitive chemoradiotherapy in patients with esophageal squamous cell cancer. Sci Rep. 2017;7(1):16870.
Adenis A, Castan F, Conroy T. Consolidation chemotherapy after definite concurrent chemoradiation in patients with non-operable esophageal cancer: Is it useful? Radiother Oncol. 2018;129(1):180–1.
Crosby T, Hurt CN, Falk S, Gollins S, Mukherjee S, Staffurth J, et al. Chemoradiotherapy with or without cetuximab in patients with oesophageal cancer (SCOPE1): a multicentre, phase 2/3 randomised trial. Lancet Oncol. 2013;14(7):627–37.
Conroy T, Galais MP, Raoul JL, Bouche O, Gourgou-Bourgade S, Douillard JY, et al. Definitive chemoradiotherapy with FOLFOX versus fluorouracil and cisplatin in patients with oesophageal cancer (PRODIGE5/ACCORD17): final results of a randomised, phase 2/3 trial. Lancet Oncol. 2014;15(3):305–14.
Chen Y, Zhu Z, Zhao W, Li L, Ye J, Wu C, et al. A randomized phase 3 trial comparing paclitaxel plus 5-fluorouracil versus cisplatin plus 5-fluorouracil in Chemoradiotherapy for locally advanced esophageal carcinoma-the ESO-shanghai 1 trial protocol. Radiat Oncol. 2018;13(1):33.
Ajani JA, Ilson DH, Daugherty K, Pazdur R, Lynch PM, Kelsen DP. Activity of taxol in patients with squamous cell carcinoma and adenocarcinoma of the esophagus. J Natl Cancer Inst. 1994;86(14):1086–91.
Wang J, Xiao L, Wang S, Pang Q, Wang J. Addition of induction or consolidation chemotherapy in definitive concurrent chemoradiotherapy versus concurrent chemoradiotherapy alone for patients with unresectable esophageal cancer: a systematic review and meta-analysis. Front Oncol. 2021;11:8839–51.
Lin CY, Lien MY, Chen CC, Fang HY, Lin YS, Chen CK, et al. Consolidative chemotherapy after definitive concurrent chemoradiotherapy for esophageal squamous cell carcinoma patients: a population based cohort study. BMC Gastroenterol. 2022;22(1):381.
Xia X, Liu Z, Qin Q, Di X, Zhang Z, Sun X, et al. Long-term survival in nonsurgical esophageal cancer patients who received consolidation chemotherapy compared with patients who received concurrent chemoradiotherapy alone: a systematic review and meta-analysis. Front Oncol. 2020;10:604657.
Wang X, Bai H, Li R, Wang L, Zhang W, Liang J, et al. High versus standard radiation dose of definitive concurrent chemoradiotherapy for esophageal cancer: a systematic review and meta-analysis of randomized clinical trials. Radiother Oncol. 2023;180:109463.
Xu Y, Dong B, Zhu W, Li J, Huang R, Sun Z, et al. A phase iii multicenter randomized clinical trial of 60 Gy versus 50 Gy radiation dose in concurrent chemoradiotherapy for inoperable esophageal squamous cell carcinoma. Clin Cancer Res. 2022;28(9):1792–9.
Chang CL, Tsai HC, Lin WC, Chang JH, Hsu HL, Chow JM, et al. Dose escalation intensity-modulated radiotherapy-based concurrent chemoradiotherapy is effective for advanced-stage thoracic esophageal squamous cell carcinoma. Radiother Oncol. 2017;125(1):73–9.
Song T, Liang X, Fang M, Wu S. High-dose versus conventional-dose irradiation in cisplatin-based definitive concurrent chemoradiotherapy for esophageal cancer: a systematic review and pooled analysis. Expert Rev Anticancer Ther. 2015;15(10):1157–69.
Hulshof M, Geijsen ED, Rozema T, Oppedijk V, Buijsen J, Neelis KJ, et al. Randomized study on dose escalation in definitive chemoradiation for patients with locally advanced esophageal cancer (ARTDECO Study). J Clin Oncol. 2021;39(25):2816–24.
You J, Zhu S, Li J, Li J, Shen J, Zhao Y, et al. High-dose versus standard-dose intensity-modulated radiotherapy with concurrent paclitaxel plus carboplatin for patients with thoracic esophageal squamous cell carcinoma: a randomized, multicenter, open-label, phase 3 superiority trial. Int J Radiat Oncol Biol Phys. 2023;115(5):1129–37.
Okines AFC, Norman AR, McCloud P, Kang YK, Cunningham D. Meta-analysis of the REAL-2 and ML17032 trials: evaluating capecitabine-based combination chemotherapy and infused 5-fluorouracil-based combination chemotherapy for the treatment of advanced oesophago-gastric cancer. Ann Oncol. 2009;20(9):1529–34.
Lee SJ, Ahn BM, Kim JG, Sohn SK, Chae YS, Moon JH, et al. Definitive chemoradiotherapy with capecitabine and cisplatin in patients with esophageal cancer: a pilot study. J Korean Med Sci. 2009;24(1):120–5.
Lee SS, Kim SB, Park SI, Kim YH, Ryu JS, Song HY, et al. Capecitabine and cisplatin chemotherapy (XP) alone or sequentially combined chemoradiotherapy containing XP regimen in patients with three different settings of stage IV esophageal cancer. Jpn J Clin Oncol. 2007;37(11):829–35.
Chen Y, Ye J, Zhu Z, Zhao W, Zhou J, Wu C, et al. Comparing paclitaxel plus fluorouracil versus cisplatin plus fluorouracil in chemoradiotherapy for locally advanced esophageal squamous cell cancer: a randomized, multicenter, phase III clinical trial. J Clin Oncol. 2019;37(20):1695–703.
al-Sarraf M, Martz K, Herskovic A, Leichman L, Brindle JS, Vaitkevicius VK, et al. Progress report of combined chemoradiotherapy versus radiotherapy alone in patients with esophageal cancer: an intergroup study. J Clin Oncol. 1997;15(1):277–84.
Zhao KL, Shi XH, Jiang GL, Yao WQ, Guo XM, Wu GD, et al. Late course accelerated hyperfractionated radiotherapy plus concurrent chemotherapy for squamous cell carcinoma of the esophagus: a phase III randomized study. Int J Radiat Oncol Biol Phys. 2005;62(4):1014–20.
Mirinezhad SK, Somi MH, Seyednezhad F, Jangjoo AG, Ghojazadeh M, Mohammadzadeh M, et al. Survival in patients treated with definitive chemo- radiotherapy for non-metastatic esophageal cancer in north- west iran. Asian Pac J Cancer Prev. 2013;14(3):1677–80.
Xing L, Liang Y, Zhang J, Wu P, Xu D, Liu F, et al. Definitive chemoradiotherapy with capecitabine and cisplatin for elder patients with locally advanced squamous cell esophageal cancer. J Cancer Res Clin Oncol. 2014;140(5):867–72.
Chen F, Luo H, Xing L, Liang N, Xie J, Zhang J. Feasibility and efficiency of concurrent chemoradiotherapy with capecitabine and cisplatin versus radiotherapy alone for elderly patients with locally advanced esophageal squamous cell carcinoma: Experience of two centers. Thorac Cancer. 2018;9(1):59–65.
Ilson DH, Wadleigh RG, Leichman LP, Kelsen DP. Paclitaxel given by a weekly 1-h infusion in advanced esophageal cancer. Ann Oncol. 2007;18(5):898–902.
Acknowledgements
We would like to thank the patients who choose to participate in clinical trials. We also thank the Health Commission of Henan Province and Zhengzhou University for providing financial support.
Funding
This work was supported by a grant from the Health Commission of Henan Province (grant number 182106000062).
Author information
Authors and Affiliations
Contributions
CF was responsible for the data collection and drafting the manuscript. HG was responsible for the design of the study, and revised the manuscript critically. XW, XZ, YS, KY, YJ, XL, WX, YL, YY, JL, QJ, CH, XW, XN, JZ, BT, WW, YZ, ZF, CY, YL, HL, XC, JX, FL, XZ, JW, SW, GC, YZ, LJ, HG participated in the design of the study. All authors read and approved the final manuscript to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Our study was approved by the medical ethic committee of the Henan cancer hospital (2018087). The other two medical ethics committees of the participating centers also gave positive advice on the local feasibility of the trial. During the study, all modifications, extensions and updates of trial procedures should be reviewed and approved by the medical ethics committee in every participating center. Our study has been registered in the Chinese Clinical Trial registry (ChiCTR1800017646). Written informed consent will be obtained from all participants before randomization.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fan, C., Wang, X., Zheng, X. et al. Consolidation chemotherapy after definitive concurrent chemoradiotherapy in patients with inoperable esophageal squamous cell carcinoma: a multicenter non-inferiority phase III randomized clinical trial. BMC Cancer 24, 321 (2024). https://doi.org/10.1186/s12885-024-12002-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12002-5