Abstract
Background
Pancreatic cancer poses a serious medical problem worldwide. Countries in the Western Pacific Region are facing public health challenges from cancer. This study assesses the time trends of pancreatic cancer mortality in the Western Pacific Region from 1990 to 2019 and predicts its trend to 2044.
Methods
Mortality data were obtained from the Global Health Data Exchange. We used an age-period-cohort model to estimate age, period and birth cohort effects on pancreatic cancer mortality from 1990 to 2019 by calculating net drift, local drift, age-specific rate, period rate ratio, and cohort rate ratio. We also predict pancreatic cancer mortality to 2044 in Western Pacific countries.
Results
Overall, there were 178,276 (95% uncertain interval: 157,771 to 198,636) pancreatic cancer deaths in the Western Pacific Region in 2019, accounting for 33.6% of all deaths due to pancreatic cancer worldwide. There were significant increases in pancreatic cancer disability-adjusted life years between 1990 and 2019 in the Western Pacific Region, mainly due to population growth and aging. Pancreatic cancer mortality increased with age. The period effect showed an increasing trend of mortality for both sexes over the study period. Compared to the reference period (2000 to 2004), the rate ratio was elevated in both males and females in the period of 2015 to 2019. There was an overall increasing rate ratio from early birth cohorts to recent cohorts. Deaths may continue to increase in the next 25 years in the ten countries, while most countries have seen their age-standardized rate forecasts fall.
Conclusion
The mortality of pancreatic cancer is still high in the Western Pacific Region. Countries/territories should focus on pancreatic cancer prevention and early cancer screening in high-risk populations. Specific public health methods and policies aimed at reducing risk factors for pancreatic cancer are also needed.
Similar content being viewed by others
Introduction
Pancreatic cancer is characterized by poor prognosis, with an overall 5-year survival rate of approximately 10% [1]. The global burden of pancreatic cancer has more than doubled over the past 25 years and now poses a serious medical problem worldwide [2]. The Western Pacific Region is one of the six World Health Organization (WHO) regions and is home to more than a quarter of the world’s population [3]. During the past few decades, the societies and economies of Western Pacific countries/territories have developed, leading to longer life expectancies [4]. The Western Pacific Regional Action Plan for the Prevention and Control of Noncommunicable Diseases 2014–2020 was endorsed by member states in 2013 to avoidable mortality due to noncommunicable diseases in the Western Pacific region [5]. However, the proportion of elderly individuals is growing faster than any other age group in the Western Pacific Region, which will lead to a high cancer burden.
Population aging is one of the important social characteristics in the Western Pacific Region [4]. Pancreatic cancer is typically a disease of older people, and age has been identified as an independent risk factor for pancreatic cancer patients [6]. Although there is ongoing research into pancreatic cancer burden, few studies have analyzed the time trends of pancreatic cancer mortality in Western Pacific countries/territories. Advances in the diagnosis and treatment of pancreatic cancer have been made over the past few years, but we still confront various health challenges. Under these circumstances, assessing, monitoring and comparing progress among pancreatic cancer patients in Western Pacific countries/territories are critical for cancer prevention and adjustment of strategies of treatment. Published studies have explored the trends in the disease burden of pancreatic cancer in some regions and countries [7,8,9]. However, studies focused on the age, period and birth cohort effects on pancreatic cancer mortality and predicting future trends remain lacking.
In this article, we conducted a systematic analysis based on the Global Burden of Disease Study (GBD) 2019 to explore the time trends of pancreatic cancer mortality in Western Pacific Region from 1990 to 2019, analyze the age, period, and cohort effects on mortality, and predict mortality to 2044, aiming to provide new insight into regional health.
Methods
Data source
The data were obtained from the Global Health Data Exchange available from https://ghdx.healthdata.org (accessed on January 15, 2023), including annual number, age-standardized rate (ASR) and their 95% uncertainty intervals (UIs). GBD 2019 provided 369 diseases and injuries and 87 risk factors for six WHO regions, 21 GBD regions and all countries/territories from 1990 to 2019 [10, 11]. In GBD 2019, pancreatic cancer was identified according to the International Classification of Diseases, version 10 as the following codes: C25-C25.9, Z85.07, contained primary malignancy of the pancreas (common and less common tumor types). More information about the methods and processing for quantifying data can be found in published studies [12, 13].
Sociodemographic index (SDI)
The SDI is a comprehensive index that reflects the development of a country or region. It ranges from 0 to 1 and can be calculated by the overall fertility rate among females younger than 25 years old, the average education level of people aged 15 and older, and the per capita income [14]. The SDI values of countries/territories can be downloaded at https://ghdx.healthdata.org/record/ihme-data/gbd-2019-socio-demographic-index-sdi-1950-2019.
Age-period-cohort model
The age-period-cohort model reflects the effects of age groups, periods of observation and birth cohorts on disease morbidity and mortality [15]. This approach aims to reveal the contribution of age-related social factors, technological factors and biological factors to disease trends [16]. The age effect refers to the impact of changes, including population aging, on pancreatic cancer mortality. The period effect refers to the change in risk of pancreatic cancer mortality of each age group caused by objective factors. The birth cohort effect refers to the effect of different levels of exposure to disease risk factors exposure on the mortality of different birth cohorts.
In a typical age-period-cohort model, the age and period intervals should be equal. Because GBD 2019 estimates are produced in 5-year age groups with data (15 to 19, 20 to 24, 25 to 29, ……, 90 to 94, 95 to 99), we arranged the pancreatic cancer deaths and global population data into successive 5-year periods (1990 to 1994, 1995 to 1999, 2000 to 2004, 2005 to 2009, 2010 to 2014, 2015 to 2019), with 2000 to 2004 (medium: 2002) as the reference period. Based on the equation (linear relationship between the three variables: birth cohort = period – age), twenty-two consecutive birth cohorts were also created (1895 to 1900, 1900 to 1905, 1905 to 1910, ……, 2000 to 2004) [16].
The estimated indexes were calculated and obtained from the age-period-cohort web tool (https://analysistools.cancer.gov/apc), including net drift, local drifts (estimated annual percentage change in each age group), longitudinal age curves (age-specific rate), period rate ratio (ratio of age-specific rates in a specific period relative to reference period) and cohort rate ratio (ratio of age-specific rates in a specific cohort relative to reference cohort). The methodological details of the age-period-cohort web tool are described in previous literature [17].
Decomposition analysis
Decomposition analysis is used to identify the additive contribution of different effects in two populations to the difference in their overall value [18]. It will allow for a better understanding of the factors associated with the changes in the absolute number of age-related disease burdens during a period [19]. In this study, we constructed a decomposition analysis to evaluate changes in disability-adjusted life years (DALYs) by three factors: (1) population size, (2) aging population, and (3) epidemiologic changes.
Data analysis
Data processing was performed in RStudio software (Version 4.2.2). The estimated annual percentage changes (EAPCs) and their 95% confidence intervals (CIs) were calculated to assess the mortality trend using linear regression analysis. The ASR showed an upward trend when the EAPC and its lower 95% CI were positive. In contrast, the ASR showed a downward trend when the EAPCs and their upper 95% CI were negative [20]. We performed classification analysis using the EAPCs of the ASR (1990 to 2019) and the ASR (in 2019). The 33rd and 66th percentiles (lower and upper terciles) were used to classify countries/territories into nine categories. The “Nordpred” package is used for predicting future deaths, which takes into account the data on global population projections and changing population structure. All rates are reported per 100,000 population. Visualizations were performed by the “ggplot2” package.
Results
An overview of burden
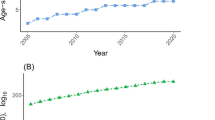
Table 1 shows the mortality for pancreatic cancer globally and in the Western Pacific Region in 2019 and its change trend from 1990 to 2019. Overall, there were 178,276 (95% UI: 157,771 to 198,636) deaths due to pancreatic cancer in the Western Pacific Region in 2019, accounting for 33.6% of all pancreatic cancer deaths worldwide. The age-standardized death rate (ASDR) was 6.71 (95% UI: 5.92 to 7.45) per 100,000 population in 2019, which was nearly 1.4-fold higher than that in 1990 (4.54, 95% UI: 4.19 to 4.87). During the past 30 years, males always had higher number of deaths and ASDRs than females (Fig. 1A). The ASDR in the Western Pacific Region increased from 1990 to 2019 at an EAPC of 1.5 (95% CI: 1.39 to 1.62) and at a percent change of 47.8% (30.3% to 67.2%), which is higher than the level observed globally. The number of pancreatic cancer deaths in the Western Pacific Region peaked at the ages of 70 to 74 years for both sexes in 2019. The number of deaths is lower in females younger than 85 years than in males in the same age group, whereas the number is higher in females than in males in age groups of 85 years and older. Age-specific death rates increased with increasing age for both sexes; death rates for males were always higher than those for females in all age groups (Fig. 2).
Time trends of pancreatic cancer mortality in the Western Pacific Region, 1990 to 2019. A Counts and age-standardized rates of pancreatic cancer mortality by sex, 1990 to 2019. B Age-standardized death rate for pancreatic cancer attributable to smoking, high fasting plasma glucose and high body mass index by sex, 1990 to 2019
GBD 2019 estimated that smoking, high fasting plasma glucose and high body mass index (BMI) are the three main risk factors for pancreatic cancer. The age-standardized proportions of all pancreatic cancer deaths that were attributable to these three risks in the Western Pacific Region in 2019 were 21.5%, 7.1% and 3.5%, respectively. From 1990 to 2019, the ASDRs of the three risk factors all showed upward trends in both sexes, and the ASDRs for all three risk factors were higher for males than for females (Fig. 1B). The fractions of pancreatic cancer age-specific deaths attributable to different risk factors by age group for males and females in 2019 are shown in Fig. S1.
Among the countries/territories in this study, China (117,374) had the highest number of deaths in 2019, followed by Japan (37,462) and the Republic of Korea (7,303) (Table 2). The highest and lowest ASDRs were observed in Palau (11.95) and Papua New Guinea (1.81), respectively (Tables S1-S3). From 1990 to 2019, only Samoa (EAPC = -0.38, 95% CI: -0.61 to -0.15) and Republic of Korea (EAPC = -0.33, 95% CI: -0.57 to -0.09) showed downward trends in the ASDR. Vietnam had seen the fastest growth in the ASDR of pancreatic cancer (EAPC = 3.76, 95% CI: 3.54 to 3.98). The deaths and ASDRs of pancreatic cancer attributable to smoking, high fasting plasma glucose, and high BMI in 1990 and 2019 are shown in Tables S4-S6. The fractions of pancreatic cancer age-standardized deaths attributable to three risk factors among countries/territories for males and females in 2019 are shown in Fig. S2.
Classification and decomposition analysis
To understand the burden differences between countries, we performed a quadrant analysis using the EAPCs of the ASDR (1990 to 2019, only contained countries with EAPC > 0) and the ASDR (in 2019) (Fig. 3). Ten countries/territories were in the upper tercile of the distribution, which represents that they had the highest disease burden in 2019. Among them, the Northern Mariana Islands, Mongolia, Niue and China are in the upper tercile of the distribution of the EAPC, indicating that these countries have the greatest increase in the mortality of pancreatic cancer. Although the ASDRs in Japan, Australia and New Zealand increased slightly, these countries still had the highest burden in 2019. Kiribati is the only country located in the lower tercile of the distribution in the ASDR and EAPC combined.
We developed a decomposition analysis of pancreatic cancer DALYs by population size, age structure, and epidemiologic changes. As shown in Fig. 4A, there were significant increases in pancreatic cancer DALYs in the Western Pacific Region for both sexes. Population growth, aging and epidemiologic changes contributed 40.3%, 30.5% and 29.2% in both sexes, respectively, to the increased DALYs between 1990 and 2019. In the five countries with the highest deaths, the contribution of aging to the overall DALY increase was most pronounced in Japan (82.1%). Population growth in Australia accounted for the highest proportion (55.1%) of the increase in the five countries (Fig. 4B). Decomposition analysis of DALYs attributable to three risk factors is shown in Figs. S3-S5.
Time trends in pancreatic cancer mortality in different age groups
Figure 5A-C show temporal changes in the age distribution of pancreatic cancer deaths. From 1990 to 2019, people who were over 50 years accounted for the largest proportion of pancreatic cancer deaths in the Western Pacific Region. Additionally, the proportion of people over 70 years old is rising year by year in both sexes. The age distribution of deaths for each country/territory is shown in Fig. S6.
Age distribution of pancreatic cancer deaths and local drifts of pancreatic cancer mortality by SDI and sex, 1990 to 2019. Temporal change in the relative proportion of pancreatic cancer deaths across age groups (15 to 49 years, 50 to 69 years, 70 + years) in (A) both sexes, B males and (C) females, 1990 to 2019. Local drifts of pancreatic cancer mortality (from age-period-cohort models) for 16 age groups in (D) both sexes, E males and (F) females, 1990 to 2019
Figure 5D-F show the overall annual percentage change (net drift) and annual percentage change in different age groups (local drifts) of pancreatic cancer mortality. Overall, pancreatic cancer mortality had increasing trends in almost all age groups. The increasing trend was enhanced with increasing age, and death rates increased the most in the oldest group (local drift = 2.79, 95% CI: 1.83 to 3.76). During the study period, net drift for males was higher than that for females. Males over 25 years old had increasing trends for pancreatic cancer death, while females older than 50 years had increasing trends. Additionally, among people over the age of 90, mortality rates increased slower for males than for females. Local drifts and net drifts by sex are shown in Tables S7-S10.
Age-period-cohort analysis
Generally, we found similar patterns in age effects in both sexes, with the lowest mortality in young people and with risk increasing with age. The age effect was more pronounced among older men than in older women (aged > 55 years) in the same age group. The period effect showed an increasing risk of mortality for both sexes over the study period. After the 2000 to 2004 period (median: 2002), the mortality risk increased faster in males than in females. Compared to the reference period (2000 to 2004), the pancreatic cancer mortality risk was 1.22 (95% CI: 1.19 to 1.26) in males and 1.09 (95% CI: 1.06 to 1.12) in females in the period of 2015 to 2019. There was an overall increasing rate ratio from early birth cohorts to recent cohorts. Similar to the period effects, the increase in the group effect was more pronounced in males (Fig. 6). The age-period-cohort model on pancreatic cancer mortality in Western Pacific countries/territories is shown in Fig. S7.
Prediction of mortality to 2044
We selected ten countries/territories with the highest pancreatic cancer deaths in 2019 to predict the number and ASR of deaths to 2044, including China, Japan, Republic of Korea, Viet Nam, Australia, Philippines, Malaysia, New Zealand, Singapore and Cambodia (Fig. 7). Most countries have seen their ASDR forecasts fall. ASDRs in 2044 may be 1.27 times higher in 2019 in the Philippines and may slightly increase in Vietnam and Australia. We also predict the number of deaths in these countries from 2020 to 2044 (Fig. S8). The results showed that deaths may continue to increase in the next 25 years in the ten countries.
Discussion
Cancer is a serious medical and public health problem worldwide, and cancer mortality is becoming an important indicator of progress toward sustainable development goals. In this study, we used an age-period-cohort model to assess the time trends of pancreatic cancer mortality in the Western Pacific Region and predicted the future situation. In 2019, the Western Pacific Region accounted for a high proportion of global pancreatic cancer deaths and may increase in the future, emphasizing the impact of pancreatic cancer burden in this region of the globe. Based on regional situations and global experiences, countries/territories in the Western Pacific Region should develop targeted strategies aimed at high-risk pancreatic cancer populations.
During the past 30 years, the burden of pancreatic cancer was higher in high SDI countries and lower in low SDI countries [12]. Higher pancreatic cancer incidence and mortality in high SDI countries may be due to population aging and lifestyle choices that increase exposure to risk factors, such as obesity and diabetes [12]. For countries with large populations, there were significant increases in DALYs of pancreatic cancer mainly due to population growth and aging. Moreover, high-income countries have great accuracy of cancer-related deaths in databases due to a well-established cancer registry, while low-income and middle-income countries have inadequate access to high-quality cancer data [21,22,23]. Thus, the differences in the accuracy of data registries influenced the reliability of some analyses in such low- and middle-income countries. The differences in epidemiological accuracy across countries should be given more attention in the future.
Death cases and ASDR of pancreatic cancer were higher in men than in women in the Western Pacific Region over the past 30 years, which was similar to the global level [24]. Females have a lower incidence of pancreatic cancer and may be less likely to be exposed to some risk factors for pancreatic cancer, such as smoking or factors related to hormonal effects [12]. The global age-standardized prevalence of tobacco use in males (32.7%) is nearly five times that in females (6.62%) [25]. Since 1990, some countries in the Western Pacific Region have not had significant reductions in the prevalence of daily smoking among males [26]. The incidence and death of pancreatic cancer in women may be more attributable to metabolic factors. The worldwide prevalence of overweight and obesity was found to be higher in older females than in older males [27, 28]. However, most countries/territories in the Western Pacific Region have a lower prevalence of obesity.
Smoking is a recognized risk factor for various cancers [1, 29, 30]. Despite a significant decline in the prevalence of smoking since 1990, population growth has led to a significant increase in the total number of smokers worldwide [25]. Cigarettes produce a variety of carcinogens, including tobacco-specific nitrosamines, polycyclic aromatic hydrocarbons, and volatile organic compounds [31]. We found that the age-standardized deaths attributable to smoking increased slightly during the past 30 years, and it was still higher than the age-standardized deaths attributable to the two metabolic factors. The Western Pacific Region is home to one-third of the global smoking population, and some countries have a large number of smokers [25, 32]. Despite tobacco control campaigns in many member states, the current rate of tobacco reduction in the Western Pacific is not fast enough to meet the 2025 target [32]. The Framework Convention on Tobacco Control entered into force in 2005, and it redefined approaches to tobacco control and use [33]. Although there has been some regional and national progress in tobacco use and control in recent years, social factors may contribute to the increased disease burden attributable to smoking. We found that population growth and aging are important factors in the increase in pancreatic cancer DALYs, which was similar to the finding from GBD 2015 Tobacco Collaborators: unless progress in reducing tobacco use can be substantially accelerated, population growth is poised to heighten the disease burden associated with smoking [26].
The age effect increased from the youngest to the oldest age group. Several characteristics of aging are very similar to specific cancer hallmarks [34]. Pancreatic cancer has been considered an age-related disease because the cancer appears to share many features with aging, including genomic instability, telomere wear, epigenetic changes, and metabolic alterations [35]. As time goes on, increased exposure to environmental and behavioral factors (such as smoking) may contribute to the chronic accumulation of DNA damage that increases the probability of cancer. Senescent cells in human bodies can manifest as a senescence-associated secretory phenotype, which can secrete various cytokines and growth factors to drive tumorigenesis, including pancreatic cancer [35, 36].
The period effect showed that the mortality risk of pancreatic cancer markedly increased in the Western Pacific Region during the study period. During the past few decades, risk factors for pancreatic cancer have continued to increase among populations. First, the prevalence of smoking has increased; in 2019, male smoking rates were above 20% in more than 150 countries [25, 26]. Among populations over 15 years old, countries with the highest prevalence of tobacco use were mostly in Asia and Oceania [25]. At present, Western Pacific countries are in a critical period of social progress and economic development. People may smoke to relieve pressure and obtain a soothing mood beacuse nicotine causes an acute mood “boost”, including an increased positive effect and a decreased negative effect [37]. Moreover, the westernization of diet and lifestyle in Western Pacific countries may contribute to an increased risk of pancreatic cancer. Dietary patterns changed from a predominantly plant-based diet to a high-energy diet and animal-based foods in some Western Pacific countries [38,39,40]. The consumption of energy-dense foods such as meat, snacks, and beverages increased, resulting in high BMI and hyperglycemia.
Similar to the period effect, more exposure to risk factors from the early birth cohort to the latest cohort can contribute to pancreatic cancer burden. We noticed that the cohort rate ratio slightly decreased since the cohort was born in 1985 (from 1.47 in 1985 to 1.37 in 2000). In the latest birth cohort, people can receive better science and health education, and access to medical knowledge is also more abundant. Health awareness has improved among younger people, and they may devote more attention to healthy lifestyles and cancer prevention.
We also predict that the number of future deaths from pancreatic cancer in ten Western Pacific countries will continue to increase. This may be related to the increase in population size and change in population structure in the future. The trends of pancreatic cancer mortality across the Western Pacific Region suggested that these countries should implement stronger measures to reduce the disease burden of pancreatic cancer. Countries that had relatively good performance in cancer prevention and reducing mortality can serve as a reference for others, emphasizing primary health care, scientific education and early cancer screening. In some countries where the population continues to grow and the population is aging, more attention will be needed in the health of high-risk populations and early cancer screening. At present, the main treatments for pancreatic cancer include surgery, chemotherapy and immunotherapy [41]. Some new therapeutic strategies, such as chemotherapy combined with immunotherapy, may improve clinical outcomes for pancreatic cancer patients in the future [42].
This study has many limitations. First, the accuracy of the GBD estimates was limited by the quality and availability of each country’s registration system. For some countries/territories without detailed cancer data sources, GBD estimates were mainly generated from modeling processes, neighboring locations and predictive covariates, which may result in potential substantial uncertainty [43]. The reported high mortality in high-income countries might be partly due to robust systems for determining the cause of cancer death and accurate diagnostic data in registration databases. Some low-income countries cannot provide accurate and adequate data on pancreatic cancer mortality due to incomplete health care systems. Thus, the estimates are very likely to substantially underestimate cancer mortality in low-income countries. This hinders the estimates of the actual disease burden in some places. Next, the age-period-cohort model was conducted in a period of five years due to the 5-year intervals in the GBD 2019, which might smoothen some variations in age, period and birth cohort effects. Future work should focus on more primary data on pancreatic cancer mortality, which might include data from registration databases, cancer centers and longer-term cohort studies. This means that more attention should be given to establishing integrative disease surveillance systems to capture pancreatic cancer-related incidence and mortality, especially in developing countries. Considering that the burden of pancreatic cancer varies by age, sex, country and region, the mortality data should also be classified according to more dimensions in the future. The economic burden caused by pancreatic cancer should also be given more attention.
Conclusion
Pancreatic cancer is an important cause of mortality, and pancreatic cancer deaths continue to increase in the Western Pacific Region. Much of this increase was due to increases in population growth, aging and exposure to risk factors. Our data analysis of pancreatic cancer mortality in Western Pacific Region is limited by the accuracy of data collection in several countries/territories, which needs to be further improved in the future. Modifiable pancreatic cancer risk factors, including behavioral factors and metabolic factors, need to be changed in the Western Pacific region by joint efforts of all countries/territories. Effective cancer prevention approaches and novel anticancer therapy strategies will be essential to achieve the aims of reducing the mortality of pancreatic cancer.
Availability of data and materials
The datasets generated and/or analysed during the current study are available in the Global Health Data Exchange query (https://vizhub.healthdata.org/gbd-results/).
Abbreviations
- ASDR:
-
Age-standardized death rate
- ASR:
-
Age-standardized rate
- CI:
-
Confidence interval
- DALY:
-
Disability-adjusted life year
- EAPC:
-
Estimated annual percentage change
- GBD:
-
Global Burden of Disease
- SDI:
-
Sociodemographic index
- UI:
-
Uncertainty interval
References
Cai J, Chen H, Lu M, Zhang Y, Lu B, You L, et al. Advances in the epidemiology of pancreatic cancer: Trends, risk factors, screening, and prognosis. Cancer Lett. 2021;520:1–11.
Klein AP. Pancreatic cancer epidemiology: understanding the role of lifestyle and inherited risk factors. Nat Rev Gastroenterol Hepatol. 2021;18:493–502.
A new voice for the Western Pacific region. Lancet Reg Health West Pac. 2020;1:100015.
Kasai DT. Preparing for population ageing in the Western Pacific Region. Lancet Reg Health West Pac. 2021;6:100069.
Shin HR, Varghese C. WHO Western Pacific regional action plan for the prevention and control of NCDs (2014–2020). Epidemiol Health. 2014;36:e2014007.
Shi H, Chen Z, Dong S, He R, Du Y, Qin Z, et al. A nomogram for predicting survival in patients with advanced (stage III/IV) pancreatic body tail cancer: a SEER-based study. BMC Gastroenterol. 2022;22:279.
Xu XH, Zeng XY, Wang LJ, Liu YN, Liu JM, Qi JL, et al. The disease burden of pancreatic cancer in China in 1990 and 2017. Zhonghua Liu Xing Bing Xue Za Zhi. 2019;40:1084–8.
Yu J, Yang X, He W, Ye W. Burden of pancreatic cancer along with attributable risk factors in Europe between 1990 and 2019, and projections until 2039. Int J Cancer. 2021;149:993–1001.
Chaves DO, Bastos AC, Almeida AM, Guerra MR, Teixeira MTB, Melo APS, et al. The increasing burden of pancreatic cancer in Brazil from 2000 to 2019: estimates from the Global Burden of Disease Study 2019. Rev Soc Bras Med Trop. 2022;55:e0271.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–22.
GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223–49.
GBD 2017 Pancreatic Cancer Collaborators. The global, regional, and national burden of pancreatic cancer and its attributable risk factors in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2019;4:934–47.
Kocarnik JM, Compton K, Dean FE, Fu W, Gaw BL, Harvey JD, et al. Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life Years for 29 Cancer Groups From 2010 to 2019: A Systematic Analysis for the Global Burden of Disease Study 2019. JAMA Oncol. 2022;8:420–44.
GBD 2019 Demographics Collaborators. Global age-sex-specific fertility. mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1160–203.
Robertson C, Boyle P. Age-period-cohort analysis of chronic disease rates. I: Modelling approach. Stat Med. 1998;17:1305–23.
Bell A. Age period cohort analysis: a review of what we should and shouldn’t do. Ann Hum Biol. 2020;47:208–17.
Rosenberg PS, Check DP, Anderson WF. A web tool for age-period-cohort analysis of cancer incidence and mortality rates. Cancer Epidemiol Biomarkers Prev. 2014;23:2296–302.
Xie Y, Bowe B, Mokdad AH, Xian H, Yan Y, Li T, et al. Analysis of the Global Burden of Disease study highlights the global, regional, and national trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney Int. 2018;94:567–81.
Chang AY, Skirbekk VF, Tyrovolas S, Kassebaum NJ, Dieleman JL. Measuring population ageing: an analysis of the Global Burden of Disease Study 2017. Lancet Public Health. 2019;4:e159–67.
Zheng Y, Yu Q, Lin Y, Zhou Y, Lan L, Yang S, et al. Global burden and trends of sexually transmitted infections from 1990 to 2019: an observational trend study. Lancet Infect Dis. 2022;22:541–51.
Anazawa T, Miyata H, Gotoh M. Cancer registries in Japan: National Clinical Database and site-specific cancer registries. Int J Clin Oncol. 2015;20:5–10.
Egawa S, Toma H, Ohigashi H, Okusaka T, Nakao A, Hatori T, et al. Japan Pancreatic Cancer Registry; 30th year anniversary: Japan Pancreas Society. Pancreas. 2012;41:985–92.
Znaor A, Eser S, Anton-Culver H, Fadhil I, Ryzhov A, Silverman BG, et al. Cancer surveillance in northern Africa, and central and western Asia: challenges and strategies in support of developing cancer registries. Lancet Oncol. 2018;19:e85–92.
Ilic I, Ilic M. International patterns in incidence and mortality trends of pancreatic cancer in the last three decades: A joinpoint regression analysis. World J Gastroenterol. 2022;28:4698–715.
GBD 2019 Tobacco Collaborators. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990–2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet. 2021;397:2337–60.
GBD 2015 Tobacco Collaborators. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990–2015: a systematic analysis from the Global Burden of Disease Study 2015. Lancet. 2017;389:1885–1906.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–81.
Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N Engl J Med. 2017;377:13–27.
GBD 2019 Colorectal Cancer Collaborators. Global, regional, and national burden of colorectal cancer and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Gastroenterol Hepatol. 2022;7:627–47.
Deng Y, Zhao P, Zhou L, Xiang D, Hu J, Liu Y, et al. Epidemiological trends of tracheal, bronchus, and lung cancer at the global, regional, and national levels: a population-based study. J Hematol Oncol. 2020;13:98.
Hecht SS, Hatsukami DK. Smokeless tobacco and cigarette smoking: chemical mechanisms and cancer prevention. Nat Rev Cancer. 2022;22:143–55.
Tobacco control in the Western Pacific region. Lancet Reg Health West Pac. 2021;10:100179.
Devita VT Jr. The Framework Convention on Tobacco Control. Nat Clin Pract Oncol. 2005;2:171.
López-Otín C, Pietrocola F, Roiz-Valle D, Galluzzi L, Kroemer G. Meta-hallmarks of aging and cancer. Cell Metab. 2023;35:12–35.
Chen Z, Wang Z, Du Y, Shi H, Zhou W. The microbiota and aging microenvironment in pancreatic cancer: Cell origin and fate. Biochim Biophys Acta Rev Cancer. 2022;1877:188826.
Coppé JP, Desprez PY, Krtolica A, Campisi J. The senescence-associated secretory phenotype: the dark side of tumor suppression. Annu Rev Pathol. 2010;5:99–118.
Kendall AD, Hedeker D, Diviak KR, Mermelstein RJ. The Mood Boost from Tobacco Cigarettes is More Erratic with the Additions of Cannabis and Alcohol. Nicotine Tob Res. 2022;24:1169–76.
Bu T, Tang D, Liu Y, Chen D. Trends in Dietary Patterns and Diet-related Behaviors in China. Am J Health Behav. 2021;45:371–83.
Lee EJ, Lee KR, Lee SJ. Study on the change and acculturation of dietary pattern of Southeast Asian workers living in South Korea. Appetite. 2017;117:203–13.
Noor MI. The nutrition and health transition in Malaysia. Public Health Nutr. 2002;5:191–5.
Mizrahi JD, Surana R, Valle JW, Shroff RT. Pancreatic cancer. Lancet. 2020;395:2008–20.
Ostios-Garcia L, Villamayor J, Garcia-Lorenzo E, Vinal D, Feliu J. Understanding the immune response and the current landscape of immunotherapy in pancreatic cancer. World J Gastroenterol. 2021;27:6775–93.
Golabi P, Paik JM, Alqahtani S, Younossi Y, Tuncer G, Younossi ZM. Burden of non-alcoholic fatty liver disease in Asia, the Middle East and North Africa: Data from Global Burden of Disease 2009–2019. J Hepatol. 2021;75:795–809.
Acknowledgements
We thank the Global Burden of Disease Study 2019 for providing the data and AJE (www.aje.com) for the expert linguistic services provided.
Funding
This research was funded by the Medical Innovation and Development Project of Lanzhou University (lzuyxcx-2022–177).
Author information
Authors and Affiliations
Contributions
WJ, CX and WZ designed the work. WJ and CX drafted the initial manuscript. WJ analyzed the data and performed the statistical analyses. YD and XL1 (Xiao Li) performed the visualization. XL2 (Xin Li) and WZ provided language help. All authors reviewed the drafted manuscript for critical content and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent to publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1
The fractions of pancreatic cancer age-specific deaths attributable to smoking, high fasting plasma glucose, and high body mass index by age group by sex, 2019. Figure S2 The fractions of pancreatic cancer age-standardized deaths attributable to smoking, high fasting plasma glucose, and high body mass index among countries/territories by sex, 2019. Figure S3 Decomposition analysis of DALYs attributable to smoking in Western Pacific region, 1990 to 2019. Figure S4 Decomposition analysis of DALYs attributable to high fasting plasma glucose in Western Pacific region, 1990 to 2019. Figure S5 Decomposition analysis of DALYs attributable to high body mass index in the Western Pacific region, 1990 to 2019. Figure S6 Temporal change in the relative proportion of pancreatic cancer deaths across age groups (15 to 49 years, 50 to 69 years, 70+ years) in Western Pacific countries/territories, 1990 to 2019. Figure S7 Age, period and cohort effects on pancreatic cancer mortality. Figure S8 Predicting pancreatic cancer deaths to 2044 in ten Western Pacific countries.
Additional file 2: Table S1
Rank of pancreatic cancer ASDR in Western Pacific countries for both sexes, 1990 and 2019. Table S2 Rank of pancreatic cancer ASDR in Western Pacific countries in males, 1990 and 2019. Table S3 Rank of pancreatic cancer ASDR in Western Pacific countries in females, 1990 and 2019. Table S4 The deaths and ASDR of pancreatic cancer attributable to smoking in Western Pacific countries/territories in 1990 and 2019. Table S5 The deaths and ASDR of pancreatic cancer attributable to high fasting plasma glucose in Western Pacific countries/territories in 1990 and 2019. Table S6 The deaths and ASDR of pancreatic cancer attributable to high body-mass index in Western Pacific countries/territories in 1990 and 2019. Table S7 Local drifts of pancreatic cancer in the Western Pacific region for both sexes combined, 1990 to 2019. Table S8 Local drifts of pancreatic cancer in the Western Pacific region for males, 1990 to 2019. Table S9 Local drifts of pancreatic cancer in the Western Pacific region for females, 1990 to 2019. Table S10 Net drift of pancreatic cancer in the Western Pacific region, 1990 to 2019.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jiang, W., Xiang, C., Du, Y. et al. Time trend of pancreatic cancer mortality in the Western Pacific Region: age-period-cohort analysis from 1990 to 2019 and forecasting for 2044. BMC Cancer 23, 876 (2023). https://doi.org/10.1186/s12885-023-11369-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-023-11369-1