Abstract
Background
Cancer chemotherapy indications for patients with poor performance status and advanced lung cancer are limited. Molecular targeted drugs, including epidermal growth factor receptor (EGFR)-tyrosine kinase inhibitors, can be used in patients with poor performance status owing to their high efficacy and safety. The third-generation EGFR-tyrosine kinase inhibitor osimertinib has demonstrated effectiveness in the initial treatment of advanced EGFR mutation-positive non-small cell lung cancer in patients with good performance status; however, no evidence exists of the drug’s effectiveness in patients with poor performance status in a prospective study. We designed a study that aims to investigate the efficacy and safety of first-line osimertinib treatment in patients with advanced non-small cell lung cancer harboring sensitive EGFR mutations and with poor performance status.
Methods
The OPEN/TORG2040 study is a multicenter, single-arm, phase II trial for patients with unresectable, advanced EGFR mutation-positive non-small cell lung cancer with a poor performance status (≥ 2). Eligible patients will receive osimertinib until disease progression or unacceptable toxicity. The primary endpoint is the objective response rate of the first-line osimertinib treatment. Considering a threshold value of 45%, expected value of 70% for objective response rate, one-sided significance level of 5%, statistical power of 80%, and ineligible patients, the sample size was set to 30. The secondary endpoints are disease control rate, performance status improvement rate, and safety and patient-reported outcomes using the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-Core Quality of Life Questionnaire and Lung Cancer 13. Time to treatment failure, progression-free survival, and overall survival will also be assessed.
Discussion
Our study can determine the clinical benefits of osimertinib treatment in patients with poor performance status, since the clinical outcomes of patients with EGFR mutation-positive non-small cell lung cancer with poor performance status treated with this drug as a first-line treatment have not been sufficiently evaluated.
Trial registration
Japan Registry of Clinical Trials: jRCTs041200100 (registration date: February 12, 2021).
Similar content being viewed by others
Background
Epidermal growth factor receptor (EGFR) gene mutations have been identified as predictors of the effect of EGFR-tyrosine kinase inhibitors (TKIs) on EGFR mutation-positive non-small cell lung cancer (NSCLC) [1,2,3]. Among the EGFR gene mutations, exon 19 deletions (DEL) and exon 21 L858R point mutations, which account for approximately 90% of the total mutations, and uncommon mutations, such as exon 18 G719X and exon 21 L861Q, are known to be EGFR-TKI-sensitizing mutations [4, 5]. In addition, a T790M mutation has been identified in approximately half of the patients as a resistance factor to first- and second-generation EGFR-TKIs, such as gefitinib, erlotinib, afatinib and dacomitinib.
Osimertinib is a third-generation, irreversible EGFR-TKI that selectively inhibits both EGFR-TKI-sensitizing and EGFR-T790M-resistant mutations [6, 7]. In a double-blind, phase III trial (FLAURA), osimertinib showed efficacy superior to that of first-generation gefitinib or erlotinib in the first-line treatment of EGFR mutation (DEL or L858R)-positive advanced NSCLC, with a similar safety profile and lower rates of serious adverse events [8, 9]. Osimertinib is currently being used as the first-line treatment for patients with advanced EGFR mutation-positive NSCLC in clinical practice. However, in the FLAURA trial, patients with a performance status (PS) of 0 to 1 were eligible, and the efficacy and safety of osimertinib treatment in patients with EGFR mutation-positive NSCLC with a poor PS (2 or more) have not been fully verified.
Poor PS is a known adverse prognostic factor in advanced NSCLC [10, 11] and a risk factor for serious adverse events, including drug-induced interstitial lung disease [12]. The median survival of patients with advanced NSCLC who are not eligible for cytotoxic chemotherapy due to poor PS was reported about 3–4 months [13, 14]. A previous prospective study of first-line gefitinib treatment for patients with advanced EGFR mutation (DEL, L858R, G719X or L861Q)-positive NSCLC without indication for cytotoxic chemotherapy as a result of poor PS has supported the use of EGFR-TKIs for these patients [15]. Several studies have indicated that osimertinib could be beneficial in patients with poor PS and EGFR T790M mutation-positive NSCLC following the progression of first- and second-generation EGFR-TKI treatments [16,17,18,19]. However, the existing data are insufficient to determine the efficacy and safety of osimertinib in chemo-naïve patients with EGFR mutation-positive NSCLC and poor PS.
First-line osimertinib treatment for patients with poor PS could be beneficial and clinically meaningful, considering the limited benefits of cytotoxic chemotherapy. Thus, this study aims to assess the efficacy and safety of first-line osimertinib treatment in patients with poor PS and advanced NSCLC harboring sensitizing EGFR mutations.
Design
Study design and treatment
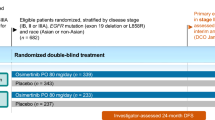
This study, whose objective is to assess the efficacy and safety of first-line osimertinib treatment in patients with advanced NSCLC harboring sensitive EGFR mutations and with poor PS, was designed as a multicenter, single-arm, phase II trial conducted by the Thoracic Oncology Research Group (TORG) in accordance with the Declaration of Helsinki. The study schema is illustrated in Fig. 1. The protocol was approved by the National Hospital Organization Nagoya Medical Center Certified Review Board of Clinical Research (approval date: December 21, 2020; approval number: C2020-010). This clinical trial was registered in the Japan Registry of Clinical Trials (registration date: February 12, 2021; registry number: jRCTs041200100). Registration for this study begin in February 2021 and will end in August 2022. Eligible patients with EGFR mutation-positive NSCLC and with a PS of 2 to 4 will receive osimertinib (80 mg orally, once daily) until disease progression or unacceptable toxicity. However, if the patients continue to show clinical benefit with the treatment as judged by the investigator, they may continue to receive osimertinib beyond the progression defined by the Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1.
Eligibility criteria
Each patient’s general condition will be assessed using the Eastern Cooperative Oncology Group PS, and patients with PS ≥ 2 will be eligible for this study. The key patient inclusion and exclusion criteria are listed in Table 1. After their eligibility is confirmed, the patients will be asked to provide informed consent. Patient registration began in February 2021 and should continue for 1.5 years.
Evaluation of treatment efficacy
Computed tomography scans of the chest and abdomen, a computed tomography or magnetic resonance imaging scan of the brain, a bone scan or positron emission tomography scan, blood test, urine test, electrocardiography, and echocardiography are required before initiation of study treatment. Patients will undergo a tumor assessment, Eastern Cooperative Oncology Group PS evaluation, and patient-reported outcome assessments using the European Organization for Research and Treatment of Cancer (EORTC) Quality of Life Questionnaire (QLQ)-Core Quality of Life Questionnaire (C30) and Lung Cancer 13 (LC13) at baseline, every 6 weeks (± 2) during the first 24 weeks, and every 8 weeks (± 2) thereafter. The tumor response will be evaluated in accordance with RECIST version 1.1. Adverse events will be recorded using the National Cancer Institute’s Common Terminology Criteria for Adverse Events version 5.0.
Endpoints
The primary endpoint is the objective response rate (ORR) of first-line osimertinib treatment. ORR is defined as the proportion of patients whose best response is complete response or partial response. However, response evaluation following the initiation of other anticancer treatments is not employed.
The secondary endpoints are disease control rate, proportion of PS improvement, safety, and patient-reported outcomes. In addition, the time to treatment failure, progression-free survival, and overall survival will also be assessed. Disease control rate is the proportion of patients whose best response is complete response, partial response, or stable disease. Proportion of PS improvement is defined as the proportion of patients who have improved by one or more steps from baseline after the start of study treatment. The time to treatment failure is defined as the duration from registration to the first date of disease progression, death, or stop of the trial treatment. Progression without diagnostic imaging is also included in disease progression. Survivors who have not progressed and continue treatment on their last visit will be censored at the last date of observation. Progression-free survival is defined as duration from registration to the confirmation of disease progression or the date of death. A survivor without disease progression is censored at the date of evaluation based on RECIST. Overall survival is the duration from registration to all causes of death. A survivor is censored at the last date of observation.
Statistical analysis
A previous Japanese study for patients with EGFR mutation-positive NSCLC without indication for cytotoxic chemotherapy as a result of poor PS, which included 26 of 30 patients with PS 2 to 4, reported that first-line gefitinib had an ORR of 66% (90% confidence interval [CI], 51 to 80%) [15]. Retrospective studies of first-line or second-line EGFR-TKI treatment for patients with EGFR mutation-positive NSCLC with PS 2 to 4 showed an ORR of 16.4 to 70.0% [13, 16, 17, 20]. Although there was insufficient evidence for first-line osimertinib in EGFR mutation-positive patients with poor PS, our prospective observational study reported an ORR of 56.3% (95% CI: 47.1 to 78.0%) [21]. This study is to confirm similar efficacy of gefitinib monotherapy and safety; therefore, the threshold of ORR was set to 45%. In the Japanese PS 0 to 1 population of the FLAURA trial, the ORRs of osimertinib and gefitinib were 75.4 and 76.4%, respectively [9]. Since the patients in this study should have PS 2 to 4, the expected ORR was set to 70%. With a threshold value of 45% and expected value of 70% for ORR, one-sided significance level of 5%, and statistical power of 80%, and by taking ineligible patients into account, the sample size was set to 30 patients.
The patients who meet the key eligible criteria and receive at least one trial treatment will comprise the full-analysis set (FAS). Within the FAS, an analysis set that does not have a serious protocol violation is defined as the per-protocol set. FAS will be used for the primary efficacy analysis. All patients who receive at least one trial treatment will be analyzed for safety.
The exact 90% CI of ORR will be estimated using the Clopper–Pearson method. A binomial test with a one-sided significance level of 0.05 will be performed based on the null hypothesis that the ORR is below the 45% threshold. The 95% CI for disease control rate and proportion of PS improvement will be estimated. The percent of change from baseline for EORTC QLQ-C30 and LC13 will be calculated. The worst grade of adverse event will be summarized. The survival curves for time to treatment failure, progression-free survival, and overall survival will be estimated using the Kaplan–Meier method.
Discussion
This is the first prospective trial to assess the clinical benefits of osimertinib as a first-line treatment in EGFR mutation-positive NSCLC patients with a poor PS (≥ 2). Patients with poor PS have been excluded from most clinical trials because of their poor prognosis and concerns about management. There is little evidence for first-line osimertinib in EGFR mutation-positive patients with poor PS. Therefore, regarding the setting of the statistical analysis in this study, the threshold of ORR was estimated by referring to the lower limit of the CI for the ORR in the previous retrospective study for patients with EGFR T790M mutation-positive NSCLC and a poor P S[16] and our prospective observational study of first-line osimertinib for patients with poor PS[21]. Molecular targeted therapies, such as EGFR-TKIs, can be expected to promote improvement from the lung cancer-induced deterioration of the physical condition of patients due to their high response rate. Whereas an accumulation of real-world data is important, it is reasonable that a prospective investigation of the efficacy and safety of the treatment, even in patients with poor PS, can be considered useful for clinical practice. The clinical influence of this study will be significant in identifying more effective treatments for bedridden patients with NSCLC to return to their daily lives. The results of the OPEN/TORG2040 study will unveil the clinical benefits of first-line osimertinib treatment in sensitizing patients with EGFR mutation-positive NSCLC and poor PS.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- EGFR:
-
Epidermal growth factor receptor
- TKI:
-
Tyrosine kinase inhibitor
- NSCLC:
-
Non-small cell lung cancer
- PS:
-
Performance status
- RECIST:
-
Response Evaluation Criteria in Solid Tumors
- EORTC:
-
European Organization for Research and Treatment of Cancer
- QLQ:
-
Quality of Life Questionnaire
- C30:
-
Core Quality of Life Questionnaire
- LC13:
-
Lung Cancer 13
- ORR:
-
Objective response rate
- FAS:
-
Full-analysis set
References
Lynch TJ, Bell DW, Sordella R, Gurubhagavatula S, Okimoto RA, Brannigan BW, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med. 2004;350:2129–39.
Paez JG, Jänne PA, Lee JC, Tracy S, Greulich H, Gabriel S, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science. 2004;304:1497–500.
Mok TS, Wu Y-L, Thongprasert S, Yang C-H, Chu D-T, Saijo N, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361:947–57.
Kobayashi Y, Mitsudomi T. Not all epidermal growth factor receptor mutations in lung cancer are created equal: perspectives for individualized treatment strategy. Cancer Sci. 2016;107:1179–86.
Lee B, Lee T, Lee S-H, Choi YL, Han J. Clinicopathologic characteristics of EGFR, KRAS, and ALK alterations in 6,595 lung cancers. Oncotarget. 2016;7:23874–84.
Jänne PA, Yang JC-H, Kim D-W, Planchard D, Ohe Y, Ramalingam SS, et al. AZD9291 in EGFR inhibitor-resistant non-small-cell lung cancer. N Engl J Med. 2015;372:1689–99.
Cross DAE, Ashton SE, Ghiorghiu S, Eberlein C, Nebhan CA, Spitzler PJ, et al. AZD9291, an irreversible EGFR TKI, overcomes T790M-mediated resistance to EGFR inhibitors in lung cancer. Cancer Discov. 2014;4:1046–61.
Soria J-C, Ohe Y, Vansteenkiste J, Reungwetwattana T, Chewaskulyong B, Lee KH, et al. Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N Engl J Med. 2018;378:113–25.
Ohe Y, Imamura F, Nogami N, Okamoto I, Kurata T, Kato T, et al. Osimertinib versus standard-of-care EGFR-TKI as first-line treatment for EGFRm advanced NSCLC: FLAURA Japanese subset. Jpn J Clin Oncol. 2019;49:29–36.
Albain KS, Crowley JJ, LeBlanc M, Livingston RB. Survival determinants in extensive-stage non-small-cell lung cancer: the southwest oncology group experience. J Clin Oncol. 1991;9:1618–26.
Paesmans M, Sculier JP, Libert P, Bureau G, Dabouis G, Thiriaux J, et al. Prognostic factors for survival in advanced non-small-cell lung cancer: univariate and multivariate analyses including recursive partitioning and amalgamation algorithms in 1,052 patients. The European lung Cancer working party. J Clin Oncol. 1995;13:1221–30.
Kudoh S, Kato H, Nishiwaki Y, Fukuoka M, Nakata K, Ichinose Y, et al. Interstitial lung disease in Japanese patients with lung cancer: a cohort and nested case-control study. Am J Respir Crit Care Med. 2008;177:1348–57.
Lee SM, Khan I, Upadhyay S, Lewanski C, Falk S, Skailes G, et al. First-line erlotinib in patients with advanced non-small-cell lung cancer unsuitable for chemotherapy (TOPICAL): a double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2012;13:1161–70.
Inoue A, Kobayashi K, Usui K, Maemondo M, Okinaga S, Mikami I, et al. First-line gefitinib for patients with advanced non-small-cell lung cancer harboring epidermal growth factor receptor mutations without indication for chemotherapy. J Clin Oncol. 2009;27:1394–400.
Nakashima K, Kimura M, Akamatsu H, Daga H, Imai H, Taira T, et al. Osimertinib for patients with EGFR T790M mutation-positive non-small-cell lung cancer and a poor performance status. Jpn J Clin Oncol. 2019;49:671–5.
Kato Y, Hosomi Y, Watanabe K, Yomota M, Kawai S, Okuma Y, et al. Impact of clinical features on the efficacy of osimertinib therapy in patients with T790M-positive non-small cell lung cancer and acquired resistance to epidermal growth factor receptor tyrosine kinase inhibitors. J Thorac Dis. 2019;11:2350–60.
Nakashima K, Ozawa Y, Daga H, Imai H, Tamiya M, Tokito T, et al. Osimertinib for patients with poor performance status and EGFR T790M mutation-positive advanced non-small cell lung cancer: a phase II clinical trial. Investig New Drugs. 2020;38:1854–61.
Tsubata Y, Watanabe K, Saito R, Nakamura A, Yoshioka H, Morita M, et al. Osimertinib in poor performance status patients with T790M-positive advanced non-small-cell lung cancer after progression of first- and second-generation EGFR-TKI treatments (NEJ032B). Int J Clin Oncol. 2022;27:112–20.
Satouchi M, Negoro S, Funada Y, Urata Y, Shimada T, Yoshimura S, et al. Predictive factors associated with prolonged survival in patients with advanced non-small-cell lung cancer (NSCLC) treated with gefitinib. Br J Cancer. 2007;96:1191–6.
Okuma Y, Hosomi Y, Nagamata M, Yamada Y, Sekihara K, Kato K, et al. Clinical outcomes after first-line EGFR inhibitor treatment for patients with NSCLC, EGFR mutation, and poor performance status. Anticancer Res. 2013;33:5057–64.
Igawa S, Fukui T, Kasajima M, Ono T, Ozawa T, Kakegawa M, et al. First-line osimertinib for poor performance status patients with EGFR mutation-positive non-small cell lung cancer: A prospective observational study. Investig. 2021;40:430–7.
Acknowledgements
The authors would like to thank the patients, their families, the TORG data center staff, and all the investigators who participated in the design of this study, as well as Editage (www.editage.jp) for the English language review.
Funding
This study is financially supported by AstraZeneca K.K., with no direct involvement in the data management, source data verification, or statistical analysis.
Author information
Authors and Affiliations
Contributions
TF, JS, SI, AK, TS, YK, HO, and KN were involved in the study conception and design. TF, AK, and KN will be involved in the analysis and interpretation of the data; TF and KN were involved in drafting the manuscript; and JS, SI, AK, TS, YK and HO were involved in revising the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The National Hospital Organization Nagoya Medical Center Certified Review Board of Clinical Research approved this protocol on December 21, 2020 (approval number: C2020-010). This clinical trial was registered in the Japan Registry of Clinical Trials (registered date: 12 February 2021, registry number: jRCTs041200100). Written informed consent was obtained from all the patients.
Consent for publication
Not applicable.
Competing interests
This study is conducted with financial support from AstraZeneca K.K.
TF received lecture fees from AstraZeneca K.K., Boehringer-Ingelheim Japan Inc., Chugai Pharmaceutical Co. Ltd., Eli Lilly Japan K.K., Novartis Pharma K.K., and Ono Pharmaceutical Co. Ltd., and honoraria from Nippon Kayaku Co. Ltd. and Pfizer Japan Inc. JS received lecture fees from AstraZeneca K.K., Chugai Pharmaceutical Co. Ltd., Daiichi Sankyo Co. Ltd., Bayer Yakuhin Co. Ltd., Kyowa Hakko Kirin Co. Ltd., MSD Co. Ltd., Nippon Kayaku Co. Ltd., Ono Pharmaceutical Co. Ltd., Pfizer Japan Inc., and Taiho Pharmaceutical Co. Ltd.; research funding from Chugai Pharmaceutical Co. Ltd., Ono Pharmaceutical Co. Ltd., Taiho Pharmaceutical Co. Ltd., and Yakult Honsha Co. Ltd.; and consulting or advisory fees from A2 Healthcare Corp. SI received lecture fees from AstraZeneca K.K., Boehringer-Ingelheim Japan Inc., Chugai Pharmaceutical Co. Ltd., Eli Lilly Japan K.K., MSD K.K., Ono Pharmaceutical Co. Ltd., and Taiho Pharmaceutical Co. Ltd., and research funding from Boehringer-Ingelheim Japan Inc., Chugai Pharmaceutical Co. Ltd., and Nippon Kayaku Co. Ltd. YK received lecture fees from AstraZeneca K.K., Boehringer-Ingelheim Japan Inc., Chugai Pharmaceutical Co. Ltd., Eli Lilly Japan K.K., MSD K.K., Ono Pharmaceutical Co. Ltd., and Taiho Pharmaceutical Co. Ltd., and research funding from MSD K.K. HO received lecture fees from Astellas Pharma Inc., Boehringer-Ingelheim Japan Inc., Bristol-Myers Squibb Co. Ltd., Chugai Pharmaceutical Co. Ltd., Kyorin Pharmaceutical Co. Ltd., Novartis Pharma K.K., and MSD K.K., and research funding from AstraZeneca K.K., Bristol-Myers Squibb Co. Ltd., Chugai Pharmaceutical Co. Ltd., Eli Lilly Japan K.K., Merck BioPharma Co. Ltd., and Taiho Pharmaceutical Co. Ltd. KN received lecture fees from AstraZeneca K.K., Boehringer-Ingelheim Japan Inc., Bristol-Myers Squibb Co. Ltd., Chugai Pharmaceutical Co. Ltd., Daiichi Sankyo Co. Ltd., Eli Lilly Japan K.K., Kyowa Hakko Kirin Co. Ltd., Mochida Pharmaceutical Co. Ltd., MSD K.K., Novartis Pharma K.K., Ono Pharmaceutical Co. Ltd., Pfizer Japan Inc., Shionogi & Co. Ltd., and Taiho Pharmaceutical Co. Ltd. AK and TIS declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fukui, T., Sasaki, J., Igawa, S. et al. Rationale and protocol design of a phase II study of first-line osimertinib treatment for patients with poor performance status and EGFR mutation-positive non-small cell lung cancer (OPEN/TORG2040). BMC Cancer 22, 1314 (2022). https://doi.org/10.1186/s12885-022-10409-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-022-10409-6