Abstract
Background
Metastasis-directed therapy (MDT) significantly delays the initiation of palliative androgen deprivation therapy (pADT) in patients with oligorecurrent prostate cancer (PCa) with a positive impact on patient’s quality of life. However, it remains unclear whether the addition of ADT improves polymetastatic free survival (PMFS) and metastatic castration refractory PCa-free survival (mCRPC-FS) and how long concomitant hormone therapy should be given. A significant overall survival (OS) benefit was shown when an androgen receptor targeted agent (ARTA) was added to pADT in patients with metastatic hormone sensitive PCa (HSPC). However, whether the addition of and ARTA to MDT in the treatment of oligorecurrent PCa results in better PMFS and mCRPC-FS has not been proven yet.
Methods & design
Patients diagnosed with oligorecurrent HSPC (defined as a maximum of 5 extracranial metastases on PSMA PET-CT) will be randomized in a 1:1:1 allocation ratio between arm A: MDT alone, arm B: MDT with 1 month ADT, or arm C: MDT with 6 months ADT together with ARTA (enzalutamide 4 × 40 mg daily) for 6 months. Patients will be stratified by PSA doubling time (≤ 3 vs. > 3 months), number of metastases (1 vs. > 1) and initial localization of metastases (M1a vs. M1b and/or M1c). The primary endpoint is PMFS, and the secondary endpoints include mCRPC-FS, biochemical relapse-free survival (bRFS), clinical progression free survival (cPFS), cancer specific survival (CSS), overall survival (OS), quality of life (QOL) and toxicity.
Discussion
This is the first prospective multicentre randomized phase III trial that investigates whether the addition of short-term ADT during 1 month or short-term ADT during 6 months together with an ARTA to MDT significantly prolongs PMFS and/or mCRPC-FS.
Trial registration
ClinicalTrials.gov Identifier: NCT05352178, registered April 28, 2022.
Similar content being viewed by others
Background
Metastasis-directed therapy
Up to 50% of patients treated with curative intent for high-risk prostate cancer (PCa) will eventually develop biochemical recurrence (BCR) at long-term follow-up [1, 2]. BCR is a precursor for the development of distant metastases and a predictor of PCa-related death. With the introduction of more sensitive imaging modalities such as prostate-specific membrane antigen (PSMA) positron emission tomography/computed tomography (PET/CT) or positron emission tomography/magnetic resonance imaging (PET/MRI) at the time of BCR, more patients are currently diagnosed with a limited number of metastases, a disease state defined as oligometastatic and in general pragmatically defined as the development of maximally 5 metastatic spots at one point in time [3]. More specific, in this setting, this disease status has been termed oligorecurrent PCa and has a different prognosis in comparison to polymetastatic PCa. Indeed, it has been demonstrated that the number of metastases is an important prognostic factor for PCa-specific survival (PCSS) [4,5,6]. The optimal treatment strategy in patients presenting with oligorecurrent PCa is still a matter of debate [7, 8]. While historically, palliative androgen-deprivation (pADT) therapy has been considered a state-of-the-art treatment, the advent of metastasis-directed therapy (MDT), performed by either metastasectomy or stereotactic body radiation therapy (SBRT) has broadened the therapeutic window as it significantly delays the initiation of pADT and its substantial side-effects when compared to active surveillance [9]. Retrospective studies served as a solid back-up demonstrating that the initiation of pADT could be delayed for several years which positively impacts patient’s quality-of-life (QOL) [9, 10]. Moreover, in some patients, the early use of pADT might promote the development of the castrate-resistant state, in which metastatic progression is driven by androgen-independent pathways [11].
Importantly, all the above-referred studies demonstrated that MDT using SBRT in case of oligorecurrent prostate cancer has low toxicity [9, 12, 13].
The SABR-COMET study [14] demonstrated that (for different tumor types, 21% of them being PCa patients) adding SBRT on top of the palliative systemic treatment in patients with a low-volume metastatic recurrence after previous treatment of the primary tumour significantly improved overall survival (OS) when compared to palliative systemic treatment alone. The eight-year OS was 27.2% in the SABR arm vs. 13.6% in the control arm (HR 0.5, 95% CI 0.3–0.84, p = 0.008) [15].
Our own research team published long-term outcomes of one of the largest retrospective analyses on MDT for oligorecurrent PCa after radical prostatectomy. In total, 191 oligorecurrent PCa patients were analysed. Estimated median palliative-ADT free survival was 66 months and estimated median mCRPC-free survival was not reached, but 83% of patients were still free of mCRPC at 10 years. In total, 314 MDTs were performed, and 25 patients (13%) received ≥ 3 MDTs. Repeated MDT resulted in low toxicity and could be offered to well-informed and motivated patients [13].
Combining MDT with ADT
ADT has a radio-sensitizing effect by inhibiting the androgen receptor-mediated repair of radiotherapy (RT)-induced DNA damage in the PCa cells [16]. The addition of a non-timeless period of ADT to primary RT has shown to improve OS for intermediate- and high-risk PCa [17, 18]. Two recent trials also suggested a progression-free by adding temporary ADT to salvage RT, especially among young and fit patients [19, 20]. Vice-versa, the addition of RT to ADT improved OS in patients presenting with high-risk disease and patients presenting with pelvic nodal disease [21,22,23,24,25].
When SBRT for oligorecurrent disease is applied, it is not clear whether adding ADT for a certain period will extend the postponement of polymetastatic disease and the development of mCRPC. Scientific reports on MDT in PCa so far use SBRT as monotherapy or in combination with a certain period of ADT [12, 13, 26, 27].
Combining ADT with second-line hormonal therapy
In three large randomized controlled trials (ENZAMET [28], ARCHES [29] and TITAN [30]), the addition of an androgen receptor targeted agent (ARTA) to ADT in men with metastatic hormone-sensitive PCa (mHSPC) was tested [28, 29, 31]. In ARCHES, the primary endpoint was radiographic progression-free survival (rPFS). rPFS was significantly improved when enzalutamide was added to ADT with a HR of 0.39 (0.3–0.5; p < 0.001). Approximately 36% of patients included in this trial had low-volume metastatic disease [29]. Recently the analysis of the secondary endpoints was published and concluded that the combination of enzalutamide with ADT reduced risk of death by 34% with a HR of 0.66 (0.53–0.81; p < 0.001) [32]. In the ENZAMET trial, the primary endpoint was overall survival (OS). The addition of enzalutamide to ADT improved OS with a HR of 0.67 (0.52–0.86; p = 0.002). Approximately half of the patients had low volume metastatic disease [28]. In the TITAN trial, apalutamide was added to ADT. The endpoints were rPFS and OS. rPFS was significantly improved in the combination group with a HR of 0.48 (0.39–0.60; p < 0.001). OS at 24 months was improved for the combination with a HR of 0.67 (0.51–0.89; p < 0.005). In this trial, 37% of patients had low volume metastatic disease [31]. In summary, all these trials resulted in the same conclusion: the addition of ARTA to ADT significantly improves clinical outcomes.
In two other large randomized controlled trials (STAMPEDE [33] and LATITUDE [34]), the addition of abiraterone acetate plus prednisone to ADT in men with mHSPC at first presentation was studied. Both trials showed a significant improvement in OS with a HR of 0.61 (0.53–0.70; p < 0.001) in the subgroup analysis for mHSPC in the STAMPEDE trial and a HR of 0.62 (0.51–0.76; p < 0,001) in the LATITUDE trial [33, 34]. Finally, the androgen receptor inhibitor, darolutamide, was tested in the ARASENS trial [35] in combination with ADT, and docetaxel among patients with mHSPC with OS as primary endpoint. The OS was significantly improved in the combination group with darolutamide with a HR of 0.68 (0.57–0.80; p < 0,001) [35].
But, although a substantial number of patients in the above-mentioned studies had low-volume metastatic disease, none of them examined the combination treatment of SBRT along with ADT and ARTA.
Methods/design
Study design
SPARKLE (a new Spark in treating oligorecurrent Prostate cancer: Adding systemic treatment to stereotactic body Radiotherapy or metastasectomy: Key to Long-lasting Event-free survival?) is approved by the Ethics committee of the Leuven University Hospitals (LUH) (EC2022/S65935) and is registered at the EudraCT data base (2022–000,066-18) and at clinicaltrials.gov (NCT05352178). It is a prospective, multicenter, randomized, open-label, three-arm, phase III study. The aim is to investigate whether the addition of short-term ADT during 1 month or short-term ADT during 6 months together with an ARTA to MDT significantly prologs polymetastatic-free survival (PMFS). The following arms will be compared (1:1:1) (Fig. 1):
-
1. Arm A: MDT alone
-
2. Arm B: MDT + 1 month of ADT
-
3. Arm C: MDT + 6 months of ADT together with 6 months ARTA (enzalutamide)
Trial design
BcR: Biochemical recurrence; OligoM + : oligometastatic disease; PSMA PET-CT/MRI: prostate-specific membrane antigen (PSMA) positron emission tomography/computed tomography (PET/CT) or positron emission tomography/magnetic resonance imaging (PET/MRI); T: testosterone; PSA: prostate specific antigen; M1a: non-regional lymph node metastases, M1b: bone metastases, M1c: visceral metastases; SBRT: stereotactic body radiotherapy; ADT: androgen deprivation therapy
The primary endpoint is polymetastatic-free survival (PMFS).
Inclusion criteria
All patients must fulfil the following inclusion criteria:
-
• Histologically proven initial diagnosis of prostatic adenocarcinoma.
-
• Prior treated and controlled primary tumor. Patients with local recurrence can be included only when accompanied by M1a-c disease, provided that the total number of active lesions does not exceed 5.
-
• Biochemical recurrence defined by prostate-specific antigen (PSA) values > 0.2 ng/ml (i.e., two consecutive increases) following radical prostatectomy ± postoperative RT and a PSA value of 2 ng/ml above the nadir after high-dose RT and confirmed at least once [36].
-
• Presence of oligorecurrent disease defined as a maximum of 5 extracranial metastases in any organ, diagnosed on PSMA PET-CT (PSMA PET-MRI is allowed, but optional) reported according to the E-PSMA consensus guidelines for interpretation of PSMA-PET [37]. Nodal (N1) disease can be included only when accompanied by M1a-c disease, provided that the total number of active lesions does not exceed 5.
-
• Serum testosterone level within normal range.
-
• WHO performance 0–2.
-
• Age > = 18 years old.
-
• Willing to provide a signed informed consent.
-
• Absence of psychological, sociological, or geographical condition potentially hampering compliance with study protocol.
-
• Patients must be presented at the multidisciplinary board meeting and the inclusion in the trial needs approval by this board.
Exclusion criteria
-
• Serum testosterone level at castration level.
-
• PSA rise while on active treatment (LHRH-agonist, LHRH antagonist, anti-androgen, maximal androgen blockade, oestrogens).
-
• Presence of poly-metastatic disease, defined as more than 5 extracranial metastatic lesions visible on PSMA PET-CT.
-
• Pelvic nodal disease (N1) without the presence of metastatic disease (M1a-c).
-
• Active malignancy other than prostate cancer that could potentially interfere with the interpretation of this trial (decision left to the principal investigator).
-
• Previous treatments (RT, surgery) or comorbidities rendering new treatment with SBRT or metastasectomy impossible.
-
• Contraindications for intake of enzalutamide (seizure or any condition that may predispose to seizure; significant cardiovascular disease within the last three months including myocardial infarction, unstable angina, congestive heart failure, ongoing arrythmias of grade > 2 or a thromboembolic event).
-
• Not able to understand the treatment protocol or sign the informed consent.
Evaluation and randomization
Patients must be staged with PSMA PET-CT/MRI within 4 weeks prior to randomization. The study will employ a 1:1:1 randomization between arm A: arm B: arm C. Patients will be stratified according to PSA doubling time (≤ 3 vs. > 3 months), number of metastases (1 versus > 1) and initial localization of metastases (M1a vs. M1b and/or M1c) (Fig. 1). Randomization will be performed centrally at the University Hospitals Leuven.
Interventions
All patients eligible for the trial will be recruited after a mandatory discussion on the multidisciplinary urology tumour board, and after approval from the attending physician if a patients is referred from another external treatment centre. Leuven University Hospitals has started recruitment in April 2022. Participating treatment centres will be added subsequently following the legal ethical requirements i.e. starting at least 3 months after inclusion of the first patient in Leuven University Hospitals. After being considered eligible, the patient will follow the trial procedure. At first, a screen visit is scheduled, on which the patient will receive a standard clinical examination and laboratory analysis including peripheral blood cell count with formula, liver and kidney function, alkaline phosphatase, lactate dehydrogenase, PSA and testosterone. Three Quality-of-life questionnaire (QLQ-30, QLQ-PR25 and EQ-5D) [38, 39] as well as a toxicity score will be carried out [40] after signature of the informed consent. Post-treatment follow-up will be planned according to the trial protocol: there are 5 follow-up visits (month 1 and further on 3-monthly basis) scheduled in year 1 and 3-monthly follow-up visits thereafter unless clinical evolution requires more monitoring. The timeline of the participants is shown in Fig. 2. The summary of the study visits is displayers in Table 1.
Stereotactic body radiotherapy
For the treatment with SBRT, all patients will receive a CT simulation with 1 mm CT slice thickness through the oligorecurrence site(s) and neighbouring organs at risk. In case of non-bony oligorecurrence, intravenous contrast will be applied (standard procedure). For lung lesions we recommend motion management with a 4D-CT simulation scan. The isocenter will be placed in the center of the oligorecurrent lesion (standard procedure). In order to increase patient comfort and stability, different support devices can be used depending on the location of the metastases and following the standard procedure of the participating centres. Delineation of the oligorecurrent metastatic lesion(s) as gross target volume (GTV) will be based on CT and hybrid PSMA PET imaging (PET-CT/MRI). The additional use of magnetic resonance imaging is left at the discretion of the treating team, however, is highly recommended in case of bony metastases. The GTV will be expanded to create the Planning Target Volume (PTV) with a margin that accounts for setup error and organ motion with a maximum of 7 mm. Using intensity-modulated arc therapy (IMAT) or volumetric arc therapy (VMAT), the aim is to prescribe a biologically equivalent dose (BED) of at least 100 Gy using an alpha over beta of 3. Typically, a total dose of 36 Gy will be prescribed in 3 fractions of 12 Gy. Treatment will be prescribed to the periphery of the target and (80% of the dose should cover 90% of the PTV). Dose constraints for organ at risk (OAR) will be in accordance the AAPM task group 100 report [41]. Dose constraints for OAR take precedence over the prescribed dose to the PTV. Treatment will be delivered using photons from a linear accelerator. Image-guided RT is mandatory and will be performed using daily cone-beam CT. Fractions will be separated > / = 48 h and < 72 h.
Surgery
The surgical technique to be used is at the discretion and expertise of the surgeon but has to be in accordance with the best surgical practice available. When possible, minimally invasive techniques are preferred. A template-based lymph node dissection (LND) is preferred above removing only the suspicious node in the case of lymph node metastasis, but not mandatory. Pelvic LND is defined as the removal of lymph nodes distal to the aortic bifurcation (internal, external and obturator iliac, common iliac, perirectal and/or presacral). Retroperitoneal LND is defined as the removal of lymph nodes above the aortic bifurcation, with upper level at least 1 cm above the most cranial lesion. The surgical removal of bone metastasis or visceral metastasis will always be performed in consultation and according to the expertise of the surgeon specialized for the respective location of metastasis.
Hormonal therapy
Androgen deprivation therapy (goserelin, leuprorelin, triptorelin, degarelix) has to be started at least 2 weeks before the RT. SBRT must be completed within the timeframe of chemical castration i.e. within 4 weeks in Arm B and within 6 months in Arm C. To prevent flare-up, bicalutamide 50 mg will also be started once daily for 1 month in case of administration of goserelin, leuprorelin or triptorelin. From the second week of bicalutamide intake, ADT can be initiated.
Enzalutamide
Enzalutamide (Xtandi®, Astellas Pharma) has to be started together with the start of ADT.
Premature discontinuation of trial treatment
Participants may voluntary withdraw their consent to participate in the Trial for any reason at any time. The participant’s request to withdraw from the Trial must always be respected without prejudice or effect on further treatment. Withdrawal of consent will be documented in the participant’s medical record. Trial data and samples collected before withdrawal can be used in the trial. No new trial data or samples will be collected after withdrawal of the participant. The investigator may also decide at any time during the course of the study to temporarily suspend or permanently discontinue the Trial treatment if continuation of the study would be detrimental to, or not in the best interest of the participant. Similarly, the Sponsor, Ethics Committee or authorized regulatory authority may decide to discontinue or prematurely terminate the Trial when new information becomes available whereby the rights, safety and well-being of Trial participants can no longer be assured, when the integrity of the Trial has been compromised, or when the scientific value of the Trial is outdated and/or unjustifiable. In any case of premature termination of the study and/or interruption/discontinuation of treatment, the Investigator will continue to monitor the participant’s condition and provide adequate medical care and follow-up. In all situations where study participation is discontinued, as well as when the study is completed as planned, the investigator will assess the participants health and prescribe the best treatment available at that time.
Objectives
Primary endpoint
-
◦ Poly-Metastatic Free Survival (PMFS) will be determined from the last day of the first SBRT or from the day surgery was performed until the first day of poly-progression which is defined as the detection > 5 new lesions at PSMA PET-CT/MRI (± combined with MRI if needed to improve diagnostic accuracy). In case of poly-progression, pADT combined with chemotherapy [42,43,44], ARTA [28, 29, 31] or abiraterone-acetate [33, 34] will be considered the standard-of-care. The decision on which treatment will be offered will be taken on the multidisciplinary meeting in every case and will take into account former treatment. If recurrence occurs in ≤ 5 lesions, a new MDT is proposed if technically feasible and the patient will receive again the treatment he was allocated to at the time of initial randomisation. Patients free from poly-progression are censored at their last follow-up.
Secondary endpoints
-
◦ Metastatic Castration-Refractory Prostate Cancer Free Survival (mCRPC-FS) will be determined from the last day of the first SBRT or from the day surgery was performed until the first day of diagnosis of CRPC. CRPC is defined according to the contemporary EAU-guidelines as the time to biochemical and/or clinical progression at castrate testosterone levels (< 50 ng/dl). Biochemical progression is defined as three consecutive PSA rises (1 week interval), of which at least 2 rises with a PSA level of > 2 ng/ml and a rise of 50% above the nadir PSA level [45]. Patients free from CRPC are censored at their last follow-up.
-
◦ Biochemical relapse-free survival (bRFS) will be determined from the last day of the first SBRT or from the day surgery was performed until the first day of BCR. BCR is defined as three consecutive PSA rises (1 week interval), of which at least 2 rises with a PSA level of > 2 ng/ml and a rise of 50% above the nadir PSA level. Patients free from BCR are censored at their last follow-up.
-
◦ Clinical progression free survival (cPFS) will be determined from the last day of the first SBRT or from the day surgery was performed until the first day of clinical relapse. Patients free from clinical relapse are censored at their last follow-up. Clinical relapse is defined as the appearance of 1 new lesion with a high suspicion on PSMA PET-CT/MRI [46].
-
◦ Cancer Specific Survival (CSS) will be determined from last day of the first SBRT or from the day surgery was performed until PCa death. Death of other causes is considered a competing event, while patients alive are censored at last follow-up.
-
◦ Overall Survival (OS) will be determined from last day of the first SBRT or from the day metastasectomy was performed until death from any cause, with censoring of patients alive at last follow-up.
-
◦ Acute and late toxicity score as a result of RT will be scores using the Common Toxicity Criteria Version 5.0 [47]. Toxicity will be scored at every visit during follow-up (see Table 1).
-
◦ Quality of life scoring using the EORTC QLQ-C30 supplement with QLQ-PR25. We will assess the quality-of-life-years with the EuroQOL classification system (EQ-5D-5L). The questionnaires are administered at baseline, last day of treatment, and during follow-up consultation at month M1, M3, M6, M12 and M24 (see Table 1).
Statistical analysis
Sample size
The required sample size was based on the following considerations. We assume a delay of PMFS after MDT alone of approximately 21 months [9]. We consider an additional median delay of PMFS of 12 months in arm B and another additional 12 months of PMFS in Arm C as clinically meaningful. The sample size calculation was determined for a two-sided long-rank test for each of the three pairwise comparisons (Arm A vs. Arm B, Arm A vs. Arm C, Arm B vs. Arm C). We suppose a 5-years of accrual and a minimum of 5 years of follow-up to determine the primary endpoint with a 10% 5-year censoring (drop-out) rate. To account for multiple testing, a Bonferroni-correction was applied, implying a test-wise significance level of 0.0167, in order to keep a family-wise significance level of 5%. A sample size of 873 patients is required (291 patients in each arm) to obtain a power of at least 80% in each of the three tests.
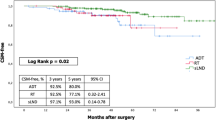
Data analysis
Patients will be analysed in the groups to which they are assigned (intention-to-treat). A stratified two-sided log-rank test will be used for the three pairwise comparisons of the primary analysis, to test for a difference between the three treatment arms with regards to poly-metastasis free survival (PMFS). A Bonferroni correction will be applied to guarantee a study-wise 5% significance level for the primary endpoint. Stratification factors are PSA doubling time (≤ 3 vs. > 3 months), number of metastases (1 versus > 1) and initial localization of metastases (M1a vs. M1b and/or M1c). Kaplan–Meier estimates will be obtained, and a KM curve will be constructed. The hazard ratio (HR) will be determined with 95% confidence interval by means of a Cox proportional hazards model. For the evaluation of mCRPC-FS, cPFS and OS the same method will be used as for the primary endpoint. CSS will be estimated using the cumulative incidence function rather than the Kaplan–Meier estimates to count for death of other causes as a competing event.
Group differences with regards to longitudinally measured ordinal outcomes such as toxicity will be analysed by means of proportional odds models with estimation based on generalized estimating equations (GEE). Multiple imputation will be applied in case of considerable drop-out, providing consistent estimates under a missing-at-random (MAR) drop-out pattern, hence when the probability of drop-out depends on treatment group or previous observations. Group differences with regards to longitudinally measured continuous outcomes such as quality of life scores will be analysed by means of linear mixed models. Likelihood methods will then be used for parameter estimation providing valid inference under MAR. For all longitudinal analyses, the explanatory model will contain both treatment group, time point of measurement and their interaction in order to test post-hoc group effects at specific time points. Statistical analysis will be performed using SAS software.
Interim analysis
An interim analysis is planned approximately after 60 months and after including 179 patients in each arm. A that time we have at least 80% power to analyse arm A vs. arm B and arm A vs. arm C. To control the type I error, both tests will be evaluated at a significance level of 0.0083. If both tests are significant, arm A can be stopped. Otherwise, all arms will be continued. In such case, the final analysis will compare arms B and C at a significance level of 0.0167. In case of significance of either arm B or C versus arm A at interim analysis, the final analysis of the remaining comparisons will also be performed at a significance level of 0.0167. In case both comparisons at the interim analysis are non-significant, both arm B and C will be compared with arm A at the final analysis at a significance level of 0.0083.
Recruitment
Patients will be recruited via the multidisciplinary urology-oncology team meetings at the participating centres. Patients will also be included if the referring urologist agrees that this study is presented to their patients.
Monitoring
All research physicians and research centres meet the qualification requirements of the responsible Ethics Committee in terms of professional training, experience in clinical trials and equipment. Because the trial medication is well characterized and of a low risk, no Data Monitoring Committee has been set up. Investigators will seek information on the occurrence of safety events at each participant contact. All events, whether reported by the participant or noted by Trial staff, will be recorded in a timely manner in the participant’s medical record and in the eCRF. The following minimum information will be recorded for each event: event description, start and stop date of the event, severity, seriousness, causality assessment to the IMP and/or Trial procedures, outcome. The Investigator will grant direct access to research data and documents for the purpose of monitoring, audits and/or inspections by authorized entities. As such eCRFs, source records and other study-related documentation (e.g. Investigator Site File, the Trial Master File, pharmacy records, etc.) will be kept current, complete and accurate at all times. All protocol modifications will be registered in the clinical trial protocol history. Protocol amendments will be submitted in writing to the responsible Ethics Committee and the national competent authority. All serious adverse events (SAEs) must be reported by reported within 24 h of the Investigator’s first awareness of the information. This is also the case for previously non-serious AEs which subsequently become SAEs. If the Investigator or research team becomes aware of an SAE with suspected causal relationship to the IMP or experiment, after the participant has completed the Trial, this SAE must be reported within the same timelines as for SAEs occurring during the Trial.
Conclusion
This protocol reports the design of a randomized phase III trial to evaluate the effectiveness of the addition of short-term ADT during 1 month or during 6 months together with an androgen receptor targeted therapy (ARTA) to MDT significantly prolongs PMFS, in patients with hormone sensitive oligorecurrent prostate cancer.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to limitations of national privacy policies (they contain information that could compromise the privacy of the study participants) but are available on reasonable request from the corresponding author.
Abbreviations
- AAPM:
-
American association of physicists in medicine
- AE:
-
Adverse event
- ADT:
-
Androgen deprivation therapy
- ARTA:
-
Androgen receptor targeted agents
- BED:
-
Biologically equivalent dose
- BCR:
-
Biochemical recurrence
- bRFS:
-
Biochemical relapse-free survival
- CI:
-
Coordinating investigator
- cPFS:
-
Clinical progression-free survival
- CSS:
-
Cancer specific survival
- CTCAE:
-
Common toxicity criteria of adverse effects
- eCRF:
-
Electronic case report form
- GEE:
-
Generalized estimating equations
- GTV:
-
Gross target volume
- LUH:
-
Leuven university hospitals
- IMAT:
-
Intensity-modulated arc therapy
- MAR:
-
Missing at random
- mCRPC-FS:
-
Metastatic castration-refractory prostate cancer free survival
- MDT:
-
Metastasis-directed therapy
- OAR:
-
Organ at risk
- OS:
-
Overall survival
- PET-MRI:
-
Positron emission tomography/magnetic resonance imaging
- PCa:
-
Prostate cancer
- PCSS:
-
Prostate cancer specific survival
- PMFS:
-
Polymetastatic-free survival
- PSA:
-
Prostate specific antigen
- PSMA PET-CT:
-
Prostate-specific membrane antigen positron emission tomography-computed tomography
- PTV:
-
Planning targeted therapy
- QOL:
-
Quality of life
- rPFS:
-
Radiographic progression-free survival
- RT:
-
Radiotherapy
- SAE:
-
Serious adverse event
- SBRT:
-
Stereotactic body radiation therapy
- VMAT:
-
Volumetric arc therapy
- WHO:
-
World health organization
References
Stephenson AJ, Scardino PT, Eastham JA, Bianco FJ Jr, Dotan ZA, Fearn PA, et al. Preoperative nomogram predicting the 10-year probability of prostate cancer recurrence after radical prostatectomy. J Natl Cancer Inst. 2006;98(10):715–7.
Würnschimmel C, Wenzel M, Wang N, Tian Z, Karakiewicz PI, Graefen M, et al. Radical prostatectomy for localized prostate cancer: 20-year oncological outcomes from a German high-volume center. Urol Oncol. 2021;39(12):830.e17-e26.
Weichselbaum RR, Hellman S. Oligometastases revisited. Nat Rev Clin Oncol. 2011;8(6):378–82.
Ost P, Decaestecker K, Lambert B, Fonteyne V, Delrue L, Lumen N, et al. Prognostic factors influencing prostate cancer-specific survival in non-castrate patients with metastatic prostate cancer. Prostate. 2014;74(3):297–305.
Soloway MS, Hardeman SW, Hickey D, Raymond J, Todd B, Soloway S, et al. Stratification of patients with metastatic prostate cancer based on extent of disease on initial bone scan. Cancer. 1988;61(1):195–202.
Schweizer MT, Zhou XC, Wang H, Yang T, Shaukat F, Partin AW, et al. Metastasis-free survival is associated with overall survival in men with PSA-recurrent prostate cancer treated with deferred androgen deprivation therapy. Ann Oncol. 2013;24(11):2881–6.
Battaglia A, De Meerleer G, Tosco L, Moris L, Van den Broeck T, Devos G, et al. Novel Insights into the Management of Oligometastatic Prostate Cancer: A Comprehensive Review. Eur Urol Oncol. 2019;2(2):174–88.
Ost P, Bossi A, Decaestecker K, De Meerleer G, Giannarini G, Karnes RJ, et al. Metastasis-directed therapy of regional and distant recurrences after curative treatment of prostate cancer: a systematic review of the literature. Eur Urol. 2015;67(5):852–63.
Ost P, Reynders D, Decaestecker K, Fonteyne V, Lumen N, De Bruycker A, et al. Surveillance or Metastasis-Directed Therapy for Oligometastatic Prostate Cancer Recurrence: A Prospective, Randomized, Multicenter Phase II Trial. J Clin Oncol. 2018;36(5):446–53.
Zilli T, Ost P. Metastasis-directed therapy: a new standard for oligorecurrent prostate cancer? Oncotarget. 2018;9(76):34196–7.
Karantanos T, Corn PG, Thompson TC. Prostate cancer progression after androgen deprivation therapy: mechanisms of castrate resistance and novel therapeutic approaches. Oncogene. 2013;32(49):5501–11.
Ost P, Reynders D, Decaestecker K, Fonteyne V, Lumen N, Bruycker AD, et al. Surveillance or metastasis-directed therapy for oligometastatic prostate cancer recurrence (STOMP): five-year results of a randomized phase II trial. J Clin Oncol. 2020;38(6_suppl):10–10.
Devos G, Berghen C, Van Eecke H, Stichele AV, Van Poppel H, Goffin K, et al. Oncological outcomes of metastasis-directed therapy in oligorecurrent prostate cancer patients following radical prostatectomy. Cancers (Basel). 2020;12(8):2271.
Palma DA, Olson R, Harrow S, Gaede S, Louie AV, Haasbeek C, et al. Stereotactic ablative radiotherapy versus standard of care palliative treatment in patients with oligometastatic cancers (SABR-COMET): a randomised, phase 2, open-label trial. Lancet. 2019;393(10185):2051–8.
Harrow S, Palma DA, Olson R, Gaede S, Louie AV, Haasbeek C, et al. Stereotactic radiation for the comprehensive treatment of oligometastases (SABR-COMET) - extended long-term outcomes. Int J Radiat Oncol Biol Phys. 2022;114(4):611–6.
Chua ML, Bristow RG. Testosterone in Androgen Receptor Signaling and DNA Repair: Enemy or Frenemy? Clin Cancer Res. 2016;22(13):3124–6.
Kishan AU, Tendulkar RD, Tran PT, Parker CC, Nguyen PL, Stephenson AJ, et al. Optimizing the Timing of Salvage Postprostatectomy Radiotherapy and the Use of Concurrent Hormonal Therapy for Prostate Cancer. Eur Urol Oncol. 2018;1(1):3–18.
Locke JA, Dal Pra A, Supiot S, Warde P, Bristow RG. Synergistic action of image-guided radiotherapy and androgen deprivation therapy. Nat Rev Urol. 2015;12(4):193–204.
Shipley WU, Seiferheld W, Lukka HR, Major PP, Heney NM, Grignon DJ, et al. Radiation with or without Antiandrogen Therapy in Recurrent Prostate Cancer. N Engl J Med. 2017;376(5):417–28.
Carrie C, Magné N, Burban-Provost P, Sargos P, Latorzeff I, Lagrange JL, et al. Short-term androgen deprivation therapy combined with radiotherapy as salvage treatment after radical prostatectomy for prostate cancer (GETUG-AFU 16): a 112-month follow-up of a phase 3, randomised trial. Lancet Oncol. 2019;20(12):1740–9.
Lin CC, Gray PJ, Jemal A, Efstathiou JA. Androgen deprivation with or without radiation therapy for clinically node-positive prostate cancer. J Natl Cancer Inst. 2015;107(7):djv119.
Bryant AK, Kader AK, McKay RR, Einck JP, Mell LK, Mundt AJ, et al. Definitive Radiation Therapy and Survival in Clinically Node-Positive Prostate Cancer. Int J Radiat Oncol Biol Phys. 2018;101(5):1188–93.
Seisen T, Vetterlein MW, Karabon P, Jindal T, Sood A, Nocera L, et al. Efficacy of Local Treatment in Prostate Cancer Patients with Clinically Pelvic Lymph Node-positive Disease at Initial Diagnosis. Eur Urol. 2018;73(3):452–61.
James ND, Spears MR, Clarke NW, Dearnaley DP, Mason MD, Parker CC, et al. Failure-Free Survival and Radiotherapy in Patients With Newly Diagnosed Nonmetastatic Prostate Cancer: Data From Patients in the Control Arm of the STAMPEDE Trial. JAMA Oncol. 2016;2(3):348–57.
Widmark A, Klepp O, Solberg A, Damber JE, Angelsen A, Fransson P, et al. Endocrine treatment, with or without radiotherapy, in locally advanced prostate cancer (SPCG-7/SFUO-3): an open randomised phase III trial. Lancet. 2009;373(9660):301–8.
Decaestecker K, De Meerleer G, Lambert B, Delrue L, Fonteyne V, Claeys T, et al. Repeated stereotactic body radiotherapy for oligometastatic prostate cancer recurrence. Radiat Oncol. 2014;9:135.
Berkovic P, De Meerleer G, Delrue L, Lambert B, Fonteyne V, Lumen N, et al. Salvage stereotactic body radiotherapy for patients with limited prostate cancer metastases: deferring androgen deprivation therapy. Clin Genitourin Cancer. 2013;11(1):27–32.
Davis ID, Martin AJ, Stockler MR, Begbie S, Chi KN, Chowdhury S, et al. Enzalutamide with Standard First-Line Therapy in Metastatic Prostate Cancer. N Engl J Med. 2019;381(2):121–31.
Armstrong AJ, Szmulewitz RZ, Petrylak DP, Holzbeierlein J, Villers A, Azad A, et al. ARCHES: A Randomized, Phase III Study of Androgen Deprivation Therapy With Enzalutamide or Placebo in Men With Metastatic Hormone-Sensitive Prostate Cancer. J Clin Oncol. 2019;37(32):2974–86.
Chi KN, Chowdhury S, Bjartell A, Chung BH, Gomes AJPdS, Given R, et al. Apalutamide in Patients With Metastatic Castration-Sensitive Prostate Cancer: Final Survival Analysis of the Randomized, Double-Blind, Phase III TITAN Study. J Clin Oncol. 2021;39(20):2294–303.
Chi KN, Agarwal N, Bjartell A, Chung BH, Pereira de Santana Gomes AJ, Given R, et al. Apalutamide for Metastatic, Castration-Sensitive Prostate Cancer. N Engl J Med. 2019;381(1):13–24.
Armstrong AJ, Azad AA, Iguchi T, Szmulewitz RZ, Petrylak DP, Holzbeierlein J, et al. Improved Survival With Enzalutamide in Patients With Metastatic Hormone-Sensitive Prostate Cancer. J Clin Oncol. 2022;40(15):1616–22.
James ND, de Bono JS, Spears MR, Clarke NW, Mason MD, Dearnaley DP, et al. Abiraterone for Prostate Cancer Not Previously Treated with Hormone Therapy. N Engl J Med. 2017;377(4):338–51.
Fizazi K, Tran N, Fein L, Matsubara N, Rodriguez-Antolin A, Alekseev BY, et al. Abiraterone plus Prednisone in Metastatic, Castration-Sensitive Prostate Cancer. N Engl J Med. 2017;377(4):352–60.
Smith MR, Hussain M, Saad F, Fizazi K, Sternberg CN, Crawford ED, et al. Darolutamide and Survival in Metastatic, Hormone-Sensitive Prostate Cancer. N Engl J Med. 2022;386(12):1132–42.
Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T, et al. EAU guidelines on prostate cancer. part 1: screening, diagnosis, and local treatment with curative intent-update 2013. Eur Urol. 2014;65(1):124–37.
Ceci F, Oprea-Lager DE, Emmett L, Adam JA, Bomanji J, Czernin J, et al. E-PSMA: the EANM standardized reporting guidelines v1.0 for PSMA-PET. Eur J Nucl Med Mol Imaging. 2021;48(5):1626–38.
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85(5):365–76.
van Andel G, Bottomley A, Fosså SD, Efficace F, Coens C, Guerif S, et al. An international field study of the EORTC QLQ-PR25: a questionnaire for assessing the health-related quality of life of patients with prostate cancer. Eur J Cancer. 2008;44(16):2418–24.
Mitropoulos D, Artibani W, Biyani CS, Bjerggaard Jensen J, Rouprêt M, Truss M. Validation of the Clavien-Dindo Grading System in Urology by the European Association of Urology Guidelines Ad Hoc Panel. Eur Urol Focus. 2018;4(4):608–13.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47.
James ND, Sydes MR, Clarke NW, Mason MD, Dearnaley DP, Spears MR, et al. Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. Lancet. 2016;387(10024):1163–77.
Sweeney CJ, Chen YH, Carducci M, Liu G, Jarrard DF, Eisenberger M, et al. Chemohormonal Therapy in Metastatic Hormone-Sensitive Prostate Cancer. N Engl J Med. 2015;373(8):737–46.
Gravis G, Fizazi K, Joly F, Oudard S, Priou F, Esterni B, et al. Androgen-deprivation therapy alone or with docetaxel in non-castrate metastatic prostate cancer (GETUG-AFU 15): a randomised, open-label, phase 3 trial. Lancet Oncol. 2013;14(2):149–58.
Cornford P, van den Bergh RCN, Briers Eea. EAU-EANM-ESTRO-ESUR-SIOG Guidelines on Prostate Cancer. Part II-2020 Update: Treatment of Relapsing and Metastatic Prostate Cancer. Eur Urol. 2021;79(2):263–82.
Fanti S, Goffin K, Hadaschik BA, Herrmann K, Maurer T, MacLennan S, et al. Consensus statements on PSMA PET/CT response assessment criteria in prostate cancer. Eur J Nucl Med Mol Imaging. 2021;48(2):469–76.
Ariyaratne H, Chesham H, Pettingell J, Alonzi R. Image-guided radiotherapy for prostate cancer with cone beam CT: dosimetric effects of imaging frequency and PTV margin. Radiother Oncol. 2016;121(1):103–8.
Acknowledgements
Not applicable.
Access to data
All study data collected and prepared during the execution of the trial protocol are the sole property of Sponsor, unless otherwise agreed in the clinical trial agreement.
Funding
All applied therapies are completely reimbursed thus no funding was required for the start of the study. Kato Rans is a PhD fellow funded by the “Stichting tegen Kanker (FAF-C/2018/1309)”.
Author information
Authors and Affiliations
Contributions
Conception and design: KR, CB, SJ, GDM. Revision of study design and protocol: KR, CB, HD, KG, AL, KP, SJ, GDM. Study coordination: KR, CB, SJ, GDM. Acquisition of data and patient recruitment: KR, CB, FA, OD, JDH, CD, BE, NL, CS, KS, HV, BV, SJ, GDM. Data management and statistical analysis: KR, CB, AL, GDM. Supervision: CB, GDM, SJ. Drafting the manuscript: KR, CB, GDM. Revision of, adaptation of and final approval of manuscript: All authors. Accountable of all aspects of the work: All authors. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was obtained by the Ethical Committee Research / KULeuven on March 24, 2022. A signed informed consent is required for all patients before inclusion in the study. The study is registered on Clinicaltrials.gov (NCT05352178). All personal data shall be treated as confidential at all times including during collection, handling and use or processing, and the personal data (including in any electronic format) shall be stored securely at all times and with all technical and organizational security measures necessary for compliance with EU and national data protection laws (whichever is more stringent). The Sponsor shall take appropriate steps to ensure the security of all personal data and guard against unauthorized access to or disclosure thereof or loss or destruction while in custody. The Sponsor is, even if there is no fault, liable for the damage suffered by the participant or in the event of death his/her beneficiaries and which is directly or indirectly related to his/her participation in the study. The participant does not have to demonstrate an error for this. The Sponsor has for this liability insurance. The Coordinating Investigator (CI) will fulfil his ethical obligation to disseminate and make the research results public. As such the CI is responsible for the timeliness, completeness and accuracy of the reports. Negative and inconclusive, as well as positive results will be published or otherwise made publicly available.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests for this trial.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rans, K., Charlien, B., Filip, A. et al. SPARKLE: a new spark in treating oligorecurrent prostate cancer: adding systemic treatment to stereotactic body radiotherapy or metastasectomy: key to long-lasting event-free survival?. BMC Cancer 22, 1294 (2022). https://doi.org/10.1186/s12885-022-10374-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-022-10374-0