Abstract
Background
Paclitaxel plus S-1(PTXS) has shown definite efficacy for advanced gastric cancer. However, the efficacy and safety of this regimen in neoadjuvant setting for locally advanced gastric cancer (LAGC) are unclear. This study aimed to compare the efficacy of neoadjuvant chemotherapy (NAC) PTXS and oxaliplatin plus S-1 (SOX) regime for patients with LAGC.
Methods
A total of 103 patients with LAGC (cT3/4NanyM0/x) who were treated with three cycles of neoadjuvant SOX regimen (n = 77) or PTXS regimen (n = 26) between 2011 and 2017 were enrolled in this study. NAC-related clinical response, pathological response, postoperative complication, and overall survival were analyzed between the groups.
Results
The baseline data did not differ significantly between both groups. After NAC, the disease control rate of the SOX group (94.8%) was comparable with that of the PTXS group (92.3%) (p = 0.641). Twenty-three cases (29.9%) in the SOX group and 10 cases (38.5%) in the PTX group got the descending stage with no statistical difference (p = 0.417). No significant differences were observed in the overall pathological response rate and the overall postoperative complication rate between the two groups (p > 0.05). There were also no differences between groups in terms of 5-year overall and disease-free survival (p > 0.05).
Conclusions
The validity of NAC PTXS was not inferior to that of SOX regimen for locally advanced gastric cancer in terms of treatment response and overall survival. PTXS regimen could be expected to be ideal neoadjuvant chemotherapy for patients with LAGC and should be adopted for the test arm of a large randomized controlled trial.
Similar content being viewed by others
Introduction
Compared with early gastric cancer, the current treatment of LAGC is still challenging worldwide. Although adjuvant chemotherapy can reduce the risk of recurrence and prolong survival in patients undergoing gastrectomy with D2 lymphadenectomy, the overall 5-year survival rate of patients remains low [1]. Therefore, since the MAGIC (Medical Research Council Adjuvant Gastric Infusional Chemotherapy) trial, numerous clinical studies on neoadjuvant chemotherapy for gastric cancer have been carried out [1,2,3,4,5]. The advantages of neoadjuvant chemotherapy, including tumor downstaging, improved R0 resection rate, validation of drug sensitivity, reduced recurrence, and improved survival, have been confirmed by more and more studies [1, 2, 4].
Neoadjuvant chemotherapy regimens for LAGC mainly refer to adjuvant chemotherapy regimens, including platinum-containing regimens and taxane-containing regimens. A series of large German multicenter clinical studies showed that the superiority of the neoadjuvant FLOT regimen (docetaxel plus oxaliplatin, fluorouracil, and leucovorin) over the ECF or ECX regimens (epirubicin plus cisplatin, and fluorouracil/capecitabine) in terms of overall survival and pathological response [6, 7]. Therefore, the FLOT regimen has become the standard regimen for perioperative chemotherapy for LAGC in European countries. However, the S-1-based doublet regimens (S-1 plus platinum, S-1 plus oxaliplatin, S-1 plus paclitaxel) are commonly used in perioperative chemotherapy regimens in Asian countries, and numerous studies have demonstrated the efficacy and safety of these doublet regimens [8,9,10,11]. The Chinese large-scale phase III clinical trial (RESOLVE) confirmed the significant efficacy of the neoadjuvant SOX (S-1 plus oxaliplatin) regimen, and thus established the SOX regimen as the first choice for neoadjuvant chemotherapy for LAGC in China [12]. In addition, a recent randomized clinical trial reported that there were no significant differences in complete or subtotal tumor regression grading, adverse effects, and postoperative morbidity between the neoadjuvant FLOT group and the SOX group [13].
The efficacy of the taxane-based triplet regimen in perioperative chemotherapy for LAGC was confirmed, but this regimen was considered more toxic [7, 13, 14]. Therefore, a taxane-based doublet regimen such as PTXS was also used as neoadjuvant chemotherapy for patients with LAGC. And several studies showed that the neoadjuvant PTXS regimen was effective and safe for patients with LAGC [11, 15]. Moreover, a high-quality review concluded that the PTXS chemotherapy was more effective and safer for advanced gastric cancer when compared with S-1 plus other drugs or S-1 alone [16]. Therefore, the neoadjuvant PTXS chemotherapy was also used for patients with LAGC in our center, with good effects and low side effects.
To date, there are no previous studies on neoadjuvant chemotherapy for patients with LAGC that compared the safety and efficacy of the SOX and PTXS regimens. So, we performed this retrospective study to explore the difference in clinical response, pathological response, postoperative complication, and overall survival between the two regimens.
Patients and methods
Patients
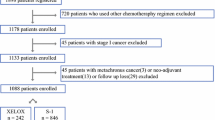
A total of 161 patients with locally advanced gastric adenocarcinoma (cT3/4NanyM0/x) received neoadjuvant chemotherapy between 2011 and 2017 in our center (Department of Gastrointestinal Surgery IV, Peking University Cancer Hospital & Institute). Among them, 103 patients who were treated with three cycles of neoadjuvant SOX regimen (n = 77) or PTXS regimen (n = 26) were included in the present study (Fig. 1). There was no uniform standard for neoadjuvant chemotherapy for LAGC, which mainly depended on the doctor's preference for medication or the potential side effects of chemotherapy drugs.
Clinicopathological data were collected in a prospectively generated database. Written informed consent was obtained from each patient enrolled in the study. All operations in this study were in accordance with the ethical standards of the Ethics Committee of Peking University Cancer Hospital & Institute.
Treatment
The neoadjuvant SOX chemotherapy was administered to patients with 3 cycles (3 weeks per cycle) of intravenous oxaliplatin (130 mg/m2 on day 1) plus oral S-1 (40-60 mg/m2 twice daily on days 1 to 14), if there were no intolerable side effects. Day 15 to day 21 was the rest week. Similarly, the neoadjuvant PTXS regimen was given to patients with 3 cycles (3 weeks per cycle) of intravenous paclitaxel (175 mg/m2 on day 1) plus oral S-1 (40-60 mg/m2 twice daily on days 1 to 14). The drug dose was adjusted according to patients with grade three and above adverse effects.
Lesions were evaluated according to the Response Evaluation Criteria in Solid Tumors (RECIST 1.1) criteria by enhanced CT, endoscopic ultrasonography (EUS), and MRI as needed after 3 cycles of neoadjuvant chemotherapy. Laparoscopic or open radical gastrectomy with standard D2 lymphadenectomy was performed 3–4 weeks after the last cycle of neoadjuvant chemotherapy. The extent of gastric resection and lymph node dissection was performed according to the gastric treatment guidelines [17].
All patients started to receive adjuvant chemotherapy about one month after surgery, and the regimen was usually continued with the preoperative regimen except for disease progression. The duration of perioperative chemotherapy was half a year. Dose reduction or chemotherapy discontinuation was carried out to help patients cope with serious side effects. Oral S-1 alone could be continued as monotherapy when patients could not tolerate the severe adverse events caused by the combined chemotherapy.
Follow-up
Patients received examinations every 3 months for the first two years after surgery, every 6 months for the next 3 years, and every year thereafter. Examinations included physical examinations, laboratory tests, X-ray/CT of the chest, and CT/ultrasonography of the abdomen and pelvis. PET/CT was conducted when appropriate.
The evaluation of the clinical response
The primary gastric lesion and perigastric lymph nodes examined by the contrast-enhanced CT were assessed by professional radiologists using Response Evaluation Criteria in Solid Tumors (RECIST; version 1.1) [18]. Complete response (CR) means that all target lesions have disappeared. Partial response (PR) is defined as at least a 30% decrease in the sum of diameters of all target lesions compared with the baseline sum diameters. Progressive disease (PD) refers to the appearance of one or more new lesions or at least a 20% increase in the sum of diameters of target lesions. Stable disease (SD) is defined as neither a sufficient decrease to qualify for PR nor a sufficient increase to qualify for PD. Disease control rate (DCR) represents the sum of CR, PR, and SD rates.
The evaluation of the pathological assessment
The degree of pathological response was classified according to TRG criteria. TRG 0 (complete response): no viable cancer cells, including lymph nodes; TRG 1 (near-complete response): single cells or rare small groups of cancer cells; TRG 2 (partial response): residual cancer cells with evident tumor regression but more than single cells or rare groups of cancer cells; TRG 3 (poor or no response): extensive residual cancer with no evident tumor regression.
Statistical analysis
Categorical variables were analyzed using the Chi-square test or Fisher’s exact test. Continuous variables were compared with t-tests or Mann–Whitney U tests. The overall survival (OS) was defined as the period from the time of operation to death or last follow-up. The disease-free survival (DFS) was defined as the period from the time of operation to recurrence. Survival curves were constructed by the Kaplan–Meier method, and differences were analyzed by the log-rank tests. Statistical analyses were calculated by SPSS version 23.0 (SPSS, Inc., Chicago, IL, USA). P-value < 0.05 was considered significant.
Results
Patient and clinical characteristics
During the study period, 161 patients with LAGC received neoadjuvant therapy. A total of 87 cases were excluded from the study for various reasons (Fig. 1). Finally, 103 eligible patients (77 in the SOX group and 26 in the PTXS group) received three cycles of neoadjuvant chemotherapy and underwent gastrectomy with D2 lymphadenectomy. No significant differences were observed in age, gender, body mass index, tumor location, cT stage, cN stage, and cTNM stage between the SOX and PTXS groups (Table 1, p > 0.05). All cases received D2 lymphadenectomy, 67.5% of patients in the SOX group and 65.4% of patients in the PTXS group underwent total gastrectomy. A total of 79.2% versus 80.8% of patients were diagnosed as stage III in the SOX and PTXS groups, respectively. Therefore, the baseline data of the two groups of patients were balanced.
Radiological response
No significant difference was observed in the pretreatment cTNM stage between the PTXS group and the SOX group. Among 77 patients in the SOX group, 0, 33, 40, and 4 cases, respectively, obtained CR (0%), PR (42.9%), SD (51.9%) and PD (5.2%). Among 26 patients in the PTX group, 0,9,15, and 2 cases, respectively, received CR (0%), PR (34.6%), SD (57.7%) and PD (7.7%) (Table 2). From Table 2, the disease control rate (CR + PR + SD) of the SOX group (94.8%) was comparable with that of the PTXS group (92.3%) (p = 0.641).
Descending stage rate
After neoadjuvant chemotherapy, a total of 33 patients (32%) got the descending stage. There were 23 cases (29.9%) in the SOX group and 10 cases (38.5%) in the PTX group with no statistical difference (p = 0.417) (Table 2).
Pathological response
There was no significant difference in the R0 resection rate between the SOX group (93.5%) and the PTXS group (92.3%). According to Lauren’s classification, 16.9% of tumors in the SOX group and 26.9% of tumors in the PTXS group were diffuse types. The proportion of the N0 stage was relatively higher in the SOX group (48%) than in the PTXS group (34.6%), but there was no significant difference between both groups. Compared with the pre-neoadjuvant chemotherapy (pre-NAC) T and N stage, the pathological T and N stages decreased significantly in both groups (Tables 2 and 3). The downstaging rate of the T stage in the SOX group was significantly better than that in the PTXS group (p = 0.015). The median number of harvested lymph nodes was 26 in the SOX group and 32 in the PTXS group with no significant difference (Table 3, p = 0.120).
The pCR rate was 5.2% in the SOX group and 0% in the PTXS group, but there was no significant difference between the two groups (p > 0.05). No significant difference was found in the overall pathological response rate (TRG grade 0 + 1 + 2) between the SOX group (49.4%) and the PTXS group (34.6%) (Table 3, p > 0.05).
Postoperative complications
No significant difference was observed in the overall postoperative complication rate between the SOX group (13.0%) and the PTXS group (7.7%). There was no anastomotic leakage in the SOX group and one in the PTXS group. There were no perioperative deaths in either group. The specific types of postoperative complications in the two groups are shown in Table 4.
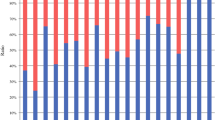
Survival analysis
During follow-up, there were nine patients with recurrence in the PTXS group, and 19 in the SOX group with no significant difference (p > 0.05). The median OS was 62 months (95% CI, 47- 76) in the PTXS group versus 92 months (95% CI, 79–105) in the SOX group. The 5-year OS rate was 55.6% in the PTXS group and 61.4% in the SOX group, with no significant difference (p = 0.651, Fig. 2).
There was also no difference in median DFS between the PTXS group (65 months, 95% CI, 48–81) and the SOX group (105 months, 95% CI, 91–117). The 5-year DFS rate was 66.7% in the PTXS group and 63.6% in the SOX group, with no significant difference (p = 0.304, Fig. 3).
Discussion
The application value of neoadjuvant chemotherapy for locally advanced gastric cancer has reached a consensus. However, the standard neoadjuvant chemotherapy regimen is still not unified worldwide. In China, although the SOX regimen has become the first-line neoadjuvant chemotherapy regimen, some patients cannot tolerate it due to serious side effects such as neurotoxicity or myelosuppression. Chemotherapy regimens containing paclitaxel showed satisfactory efficacy and safety in the treatment of advanced gastric cancer [19, 20]. Therefore, paclitaxel has been also used in the perioperative chemotherapy regimen for LAGC [13, 21, 22]. If the PTXS regimen is not inferior to the SOX regimen in the context of neoadjuvant therapy, then the regimen can be used as an alternative to the SOX regimen.
The present study demonstrated that the proportion of downstaging rate was higher in the PTXS group (38.5%) than that in the SOX group (29.9%), although there was no statistically significant difference. Consistent with previous reports [1, 3, 4], neoadjuvant chemotherapy could achieve downstaging. Therefore, for patients with severely locally advanced gastric cancer, especially those who cannot tolerate the SOX regimen, the neoadjuvant PTXS is a desirable option.
The determination of clinical staging by CT evaluation was not very accurate. In this study, stage 0 and stage I were absent in TNM staging after neoadjuvant chemotherapy (Table 2). However, there were four patients with pathological stage 0 and 9 patients with pathological stage I in the SOX group, and one patient with pathological stage I in the PTXS group (Table 3). It was reported that the accuracy of CT in diagnosing T staging was about 77–89%, and the accuracy of diagnosing N staging was about 59- 78% [23, 24]. A prospective study (JCOG1302A) reported that there were 141 (15.2%) and 71 (7.7%) patients with pathological T1 and T2 tumors respectively among 928 patients with cT3/T4 [25]. The overdiagnosis was mainly due to the intratumoral edema or fibrosis that made the lesion look thicker on CT or endoscopic ultrasonography [25, 26]. Therefore, the efficacy of neoadjuvant chemotherapy for gastric cancer should not be evaluated solely by CT, but also combined with other tools, such as MRI or PET/CT when necessary.
This study did not reveal a statistically significant difference between neoadjuvant SOX and PTXS regimens in terms of DCR and TRG. These results indicated that the effect of PTXS as a neoadjuvant chemotherapy regimen in the treatment of LAGC was not inferior to that of the SOX regimen. Due to the synergistic cytotoxic effect of paclitaxel and fluorouracil, the significant efficacy of this regimen in advanced gastric cancer was confirmed in many clinical studies [20, 27].
The effect of different neoadjuvant chemotherapy regimens on surgical complications is also a matter of concern. This study showed that the postoperative complication rate was low and not significantly different between the two groups. Many studies showed that neoadjuvant chemotherapy did not increase the complications and postoperative mortality [1]. However, some other studies found that neoadjuvant chemotherapy increased the complication rate after gastrectomy with D2 lymphadenectomy, and reported the complication rate of patients receiving neoadjuvant chemotherapy regimen containing paclitaxel or docetaxel ranged from 17–31.3% [28,29,30]. Actually, gastrectomy is usually performed three to four weeks after neoadjuvant chemotherapy, at which time the effect of chemotherapy on tissue healing is negligible.
The present study also found that the 5-year OS of the PTXS group was not significantly different from that of the SOX group. Paclitaxel as monotherapy or in combination with other drugs could improve survival without compromising the quality of life (QoL) for patients with advanced gastric cancers [31]. A phage III trial comparing the efficacy and safety of paclitaxel/capecitabine (PACX) and cisplatin/capecitabine (XP) in advanced gastric cancer showed that QoL was significantly improved in PACX versus XP [19]. Baoyu Yang et al. reported that paclitaxel combined with a leucovorin and 5-fluorouracil regimen as neoadjuvant chemotherapy for gastric cancer could improve the R0 resection rate (85.2%) and 5-year survival rate (56.9%), and showed good tolerability [27].
Conclusions
There were no significant differences between the NAC PTXS group and the SOX group in terms of clinical response, pathological response, postoperative complication rate, and 5-year survival rate. Therefore, for patients with LAGC who cannot tolerate neoadjuvant SOX, the PTXS regimen would be an ideal alternative, especially for patients with renal insufficiency. This study was a single-center retrospective trial and had its limitations. The above conclusions are insufficient and need to be verified by further multi-center randomized controlled trials in the future.
Availability of data and materials
All data generated or analysed during this study are included in the Supplementary file 1.
Abbreviations
- PTXS:
-
Paclitaxel plus S-1
- LAGC:
-
Locally advanced gastric cancer
- SOX:
-
Oxaliplatin plus S-1
- NAC:
-
Neoadjuvant chemotherapy
- MAGIC:
-
Medical Research Council Adjuvant Gastric Infusional Chemotherapy
- EUS:
-
Endoscopic ultrasonography
- MRI:
-
Magnetic Resonance Imaging
- RECIST:
-
Response evaluation criteria in solid tumors
- CR:
-
Complete response
- PR:
-
Partial response
- PD:
-
Progressive disease
- SD:
-
Stable disease
- DCR:
-
Disease control rate
- TRG:
-
Tumor regression grade
- OS:
-
Overall survival
- DFS:
-
Disease-free survival
- DCR:
-
Disease control rate
References
Coccolini F, Nardi M, Montori G, Ceresoli M, Celotti A, Cascinu S, Fugazzola P, Tomasoni M, Glehen O, Catena F, et al. Neoadjuvant chemotherapy in advanced gastric and esophago-gastric cancer. Meta-analysis of randomized trials. Int J Surg. 2018;51:120–7.
Cunningham D, Allum WH, Stenning SP, Thompson JN, Van de Velde CJ, Nicolson M, Scarffe JH, Lofts FJ, Falk SJ, Iveson TJ, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355(1):11–20.
Li Z, Shan F, Ying X, Zhang Y, E JY, Wang Y, Ren H, Su X, Ji J. Assessment of laparoscopic distal gastrectomy after neoadjuvant chemotherapy for locally advanced gastric cancer: a randomized clinical trial. JAMA Surg. 2019;154(12):1093–101.
Zhao JH, Gao P, Song YX, Sun JX, Chen XW, Ma B, Yang YC, Wang ZN. Which is better for gastric cancer patients, perioperative or adjuvant chemotherapy: a meta-analysis. BMC Cancer. 2016;16:631.
Eto K, Hiki N, Kumagai K, Shoji Y, Tsuda Y, Kano Y, Yasufuku I, Okumura Y, Tsujiura M, Ida S, et al. Prophylactic effect of neoadjuvant chemotherapy in gastric cancer patients with postoperative complications. Gastric Cancer. 2018;21(4):703–9.
Al-Batran SE, Hofheinz RD, Pauligk C, Kopp HG, Haag GM, Luley KB, Meiler J, Homann N, Lorenzen S, Schmalenberg H, et al. Histopathological regression after neoadjuvant docetaxel, oxaliplatin, fluorouracil, and leucovorin versus epirubicin, cisplatin, and fluorouracil or capecitabine in patients with resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4-AIO): results from the phase 2 part of a multicentre, open-label, randomised phase 2/3 trial. Lancet Oncol. 2016;17(12):1697–708.
Al-Batran SE, Homann N, Pauligk C, Goetze TO, Meiler J, Kasper S, Kopp HG, Mayer F, Haag GM, Luley K, et al. Perioperative chemotherapy with fluorouracil plus leucovorin, oxaliplatin, and docetaxel versus fluorouracil or capecitabine plus cisplatin and epirubicin for locally advanced, resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4): a randomised, phase 2/3 trial. Lancet. 2019;393(10184):1948–57.
Kim GM, Jeung HC, Rha SY, Kim HS, Jung I, Nam BH, Lee KH, Chung HC. A randomized phase II trial of S-1-oxaliplatin versus capecitabine-oxaliplatin in advanced gastric cancer. Eur J Cancer. 2012;48(4):518–26.
Yamada Y, Higuchi K, Nishikawa K, Gotoh M, Fuse N, Sugimoto N, Nishina T, Amagai K, Chin K, Niwa Y, et al. Phase III study comparing oxaliplatin plus S-1 with cisplatin plus S-1 in chemotherapy-naive patients with advanced gastric cancer. Ann Oncol. 2015;26(1):141–8.
Satake H, Miki A, Kondo M, Kotake T, Okita Y, Hatachi Y, Yasui H, Imai Y, Ichikawa C, Murotani K, et al. Phase I study of neoadjuvant chemotherapy with S-1 and oxaliplatin for locally advanced gastric cancer (Neo G-SOX PI). ESMO Open. 2017;2(1): e000130.
Peng YF, Imano M, Itoh T, Satoh T, Chiba Y, Imamoto H, Tsubaki M, Nishida S, Yasuda T, Furukawa H. A phase II trial of perioperative chemotherapy involving a single intraperitoneal administration of paclitaxel followed by sequential S-1 plus intravenous paclitaxel for serosa-positive gastric cancer. J Surg Oncol. 2015;111(8):1041–6.
Zhang X, Liang H, Li Z, Xue Y, Wang Y, Zhou Z, Yu J, Bu Z, Chen L, Du Y, et al. Perioperative or postoperative adjuvant oxaliplatin with S-1 versus adjuvant oxaliplatin with capecitabine in patients with locally advanced gastric or gastro-oesophageal junction adenocarcinoma undergoing D2 gastrectomy (RESOLVE): an open-label, superiority and non-inferiority, phase 3 randomised controlled trial. Lancet Oncol. 2021;22(8):1081–92.
Sah BK, Zhang B, Zhang H, Li J, Yuan F, Ma T, Shi M, Xu W, Zhu Z, Liu W, et al. Neoadjuvant FLOT versus SOX phase II randomized clinical trial for patients with locally advanced gastric cancer. Nat Commun. 2020;11(1):6093.
Hirakawa M, Sato Y, Ohnuma H, Takayama T, Sagawa T, Nobuoka T, Harada K, Miyamoto H, Sato Y, Takahashi Y, et al. A phase II study of neoadjuvant combination chemotherapy with docetaxel, cisplatin, and S-1 for locally advanced resectable gastric cancer: nucleotide excision repair (NER) as potential chemoresistance marker. Cancer Chemother Pharmacol. 2013;71(3):789–97.
Yoshikawa T, Tanabe K, Nishikawa K, Ito Y, Matsui T, Kimura Y, Hirabayashi N, Mikata S, Iwahashi M, Fukushima R, et al. Induction of a pathological complete response by four courses of neoadjuvant chemotherapy for gastric cancer: early results of the randomized phase II COMPASS trial. Ann Surg Oncol. 2014;21(1):213–9.
Bian NN, Wang YH, Min GT. S-1 combined with paclitaxel may benefit advanced gastric cancer: evidence from a systematic review and meta-analysis. Int J Surg. 2019;62:34–43.
Japanese Gastric Cancer A. Japanese gastric cancer treatment guidelines 2018 (5th edition). Gastric Cancer. 2021;24(1):1–21.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47.
Lu Z, Zhang X, Liu W, Liu T, Hu B, Li W, Fan Q, Xu J, Xu N, Bai Y, et al. A multicenter, randomized trial comparing efficacy and safety of paclitaxel/capecitabine and cisplatin/capecitabine in advanced gastric cancer. Gastric Cancer. 2018;21(5):782–91.
Yeh KH, Lu YS, Hsu CH, Lin JF, Hsu C, Kuo SH, Li SJ, Cheng AL. Phase II study of weekly paclitaxel and 24-hour infusion of high-dose 5-fluorouracil and leucovorin in the treatment of recurrent or metastatic gastric cancer. Oncology. 2005;69(1):88–95.
Yoshida K, Kodera Y, Kochi M, Ichikawa W, Kakeji Y, Sano T, Nagao N, Takahashi M, Takagane A, Watanabe T, et al. Addition of docetaxel to oral fluoropyrimidine improves efficacy in patients with stage iii gastric cancer: interim analysis of JACCRO GC-07, a randomized controlled trial. J Clin Oncol. 2019;37(15):1296–304.
Ito S, Sano T, Mizusawa J, Takahari D, Katayama H, Katai H, Kawashima Y, Kinoshita T, Terashima M, Nashimoto A, et al. A phase II study of preoperative chemotherapy with docetaxel, cisplatin, and S-1 followed by gastrectomy with D2 plus para-aortic lymph node dissection for gastric cancer with extensive lymph node metastasis: JCOG1002. Gastric Cancer. 2017;20(2):322–31.
Shimizu K, Ito K, Matsunaga N, Shimizu A, Kawakami Y. Diagnosis of gastric cancer with MDCT using the water-filling method and multiplanar reconstruction: CT-histologic correlation. AJR Am J Roentgenol. 2005;185(5):1152–8.
Chen CY, Hsu JS, Wu DC, Kang WY, Hsieh JS, Jaw TS, Wu MT, Liu GC. Gastric cancer: preoperative local staging with 3D multi-detector row CT–correlation with surgical and histopathologic results. Radiology. 2007;242(2):472–82.
Fukagawa T, Katai H, Mizusawa J, Nakamura K, Sano T, Terashima M, Ito S, Yoshikawa T, Fukushima N, Kawachi Y, et al. A prospective multi-institutional validity study to evaluate the accuracy of clinical diagnosis of pathological stage III gastric cancer (JCOG1302A). Gastric Cancer. 2018;21(1):68–73.
Ott K, Weber WA, Lordick F, Becker K, Busch R, Herrmann K, Wieder H, Fink U, Schwaiger M, Siewert JR. Metabolic imaging predicts response, survival, and recurrence in adenocarcinomas of the esophagogastric junction. J Clin Oncol. 2006;24(29):4692–8.
Yang B, Shi C, Lin X, Wang X, Chen Q. Retrospective study on efficacy of a paclitaxel combined with a leucovorin and fluorouracil regimen for advanced gastric cancer. Tumori. 2019;105(6):509–15.
Oyama K, Fushida S, Kinoshita J, Makino I, Nakamura K, Hayashi H, Nakagawara H, Tajima H, Fujita H, Takamura H, et al. Efficacy of pre-operative chemotherapy with docetaxel, cisplatin, and S-1 (DCS therapy) and curative resection for gastric cancer with pathologically positive para-aortic lymph nodes. J Surg Oncol. 2012;105(6):535–41.
Migita K, Nashimoto A, Yabusaki H, Matsuki A, Aizawa M. Efficacy of neoadjuvant chemotherapy with docetaxel, cisplatin and S-1 for resectable locally advanced gastric cancer. Int J Clin Oncol. 2016;21(1):102–9.
Sasaki K, Onodera S, Otsuka K, Satomura H, Kurayama E, Kubo T, Takahashi M, Ito J, Nakajima M, Yamaguchi S, et al. Validity of neoadjuvant chemotherapy with docetaxel, cisplatin, and S-1 for resectable locally advanced gastric cancer. Med Oncol. 2017;34(8):139.
Sakamoto J, Matsui T, Kodera Y. Paclitaxel chemotherapy for the treatment of gastric cancer. Gastric Cancer. 2009;12(2):69–78.
Acknowledgements
We thank all patients who participated in this study.
Funding
This study was supported by the National Natural Science Foundation of China (No. 82171720, 81872022, 81672439), Beijing Natural Science Foundation (No.7162039), Capital’s Funds for Health Improvement and Research (CFH 2018–2-2153), Beijing Hospitals Authority Clinical Medicine Development of Special Funding Support (No. ZYLX202116).
Author information
Authors and Affiliations
Contributions
Conception and design: C.H.Z, B.H.W, X.Q.S; Data collection: B.H.W, M.X.L, L.C, K.X, F.T; Analysis and interpretation of data: C.H.Z, M.C, H.Y; Writing-original draft: C.H.Z; Data curation and review of the manuscript: B.H.W, J.D.X, Z.D.Y; Study supervision: M.C, N.Z, Z.D.Y. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was obtained from the Ethics Committee of Peking University Cancer Hospital & Institute (Ethical code: 2022–5-12). The study was in accordance with the 1964 Helsinki declaration. All participants gave written informed consent to participate in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest related to this research project.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, C., Wu, B., Yang, H. et al. The validity of neoadjuvant chemotherapy with paclitaxel plus S-1 is not inferior to that of SOX regimen for locally advanced gastric cancer: an observational study. BMC Cancer 22, 1223 (2022). https://doi.org/10.1186/s12885-022-10230-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-022-10230-1