Abstract
Background
Multiple myeloma (MM) is an incurable plasma cell malignancy. Red cell distribution width (RDW) is a prognostic marker in various diseases, solid tumors, and hematologic neoplasms, but its prognostic significance in MM is controversial. In this study, we aimed to assess the relationship between RDW and the clinical prognosis of MM patients through a meta-analysis.
Methods
Relevant literature were retrieved from PubMed, Embase, and Web of Science databases according to PRISMA guideline. All relevant parameters were extracted and combined for statistical analysis. The effect size was presented as hazard ratio (HR)/odds ratio (OR) and 95% confidence interval (CI). HR/OR > 1 in MM patients with high RDW suggested a worse prognosis. Heterogeneity test evaluation was performed using Cochran's Q test and I2 statistics. A Pheterogeneity < 0.10 or I2 > 50% suggested significant heterogeneity. P < 0.05 was considered statistically significant. Statistical analysis was performed using Stata 12.0 software.
Results
8 articles involving 9 studies with 1165 patients were included in our meta-analysis. Our results suggested that elevated RDW is significantly associated with poor prognosis in MM (OS: HR = 1.91, 95%CI: 1.48–2.46; PFS: HR = 2.87, 95% CI: 2.02–4.07). A significant correlation was not found between RDW and International Staging System (ISS) staging (ISS III VS ISS I-II: OR:1.53; 95%CI:0.97–2.42).
Conclusion
Our results suggested that RDW is a robust predictor of newly diagnosed MM outcomes.
Similar content being viewed by others
Introduction
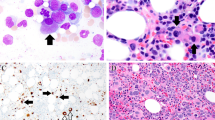
Multiple myeloma (MM), the second most common hematologic malignancy after non-Hodgkin's lymphoma in adults worldwide [1], is characterized by abnormal accumulation of malignant plasma cells in the bone marrow and excessive production of monoclonal immunoglobulins [2]. Proteasome inhibitors and immunomodulatory drugs, the primary agents currently used in the treatment of multiple myeloma [2], have significantly improved the survival of patients [3]. With the introduction of therapies such as autologous stem cell transplantation (ASCT) and CD38 monoclonal antibodies (e.g., Daratumumab), the overall treatment of MM has gradually achieved good results, with patients achieving deeper depth of remission and longer overall survival [4,5,6]. However, it remains an incurable disease due to genetic heterogeneity and other reasons [7]. Therefore, there is a pressing need to identify the high-risk patients with poor prognoses so that novel and intensive protocols can be initiated earlier to improve survival.
Currently, The Revised International Staging System (R-ISS) is a powerful prognostic staging system commonly used for MM and an authoritative reference for treatment strategies [8], which is proposed by the International Myeloma Working Group (IMWG) based on International Staging System (ISS), high-risk cytogenetics [t(4;14), t(14;16) and del17p by interphase fluorescent in situ hybridization (iFISH)] and elevated serum lactate dehydrogenase (LDH) [9]. However, patients with the same stage who received similar treatment regimens still had dramatically different clinical outcomes. It suggests that the current staging system is not comprehensive enough in predicting survival outcomes and reflecting the biological heterogeneity of MM patients. In addition, fluorescence in situ hybridization (FISH) assays are very expensive. Therefore, there is significant interest in investigating readily accessible biomarkers to estimate survival outcomes in MM.
Increasing evidence suggests that the systemic inflammatory response may play an essential role in the development of tumors [10]. The prognostic value of inflammatory factors such as C-reactive protein, neutrophil to lymphocyte ratio (NLR), and red blood cell distribution width (RDW) has been assessed in various types of cancer. RDW, which reflects the variability of red blood cell size, has been reported to be associated with a worse prognosis in a variety of cancers, including pancreatic [11], colorectal [12], and breast cancers [13].
Recent studies have shown that RDW is a potential prognostic marker in MM. However, based on their findings, the opinion about the prognostic value of RDW in MM remains inconclusive. It is generally acknowledged that meta-analysis is a powerful statistic tool to overcome the limitation of different sample sizes from individual studies and generate the best estimation. In this study, we aimed to draw the prognostic value of elevated RDW in MM.
Methods
Search strategy
We have conducted a comprehensive literature search of articles through the PubMed, Embase, and Web of Science databases with no date or language restrictions. The last search was conducted on March 25, 2022. The main search terms included: (“RDW” OR “red blood cell distribution width” OR “red cell distribution width”) AND (“multiple myeloma” OR “Myeloma”) AND (“prognosis” OR “prognostic” OR “outcome” OR “survival” OR “predict” OR “prediction”). Furthermore, we also checked the relevant articles in the reference list.
Inclusion and exclusion criteria
The inclusion criteria for this meta-analysis to select study are as follows: (1) studied patients with MM were diagnosed according to the criteria of the International Myeloma Working Group in 2014. The following inclusion criteria were used to select studies for this meta-analysis:(1) The MM patients of studies were identified according to the International Myeloma Working Group 2014 diagnostic criteria. [14]. (2) Association between RDW and overall survival (OS) and progression-free survival (PFS) was reported. (3) RDW was measured by blood-based methods without any formal treatment. The exclusion criteria are as follows: (1) abstracts, letters, meta-analysis, case reports, or reviews. (2) basic studies or animal trials. (3) studies with insufficient data for estimating hazard ratio (HR) and 95% confidence interval (CI). (4) patients suffered from other primary tumors, severe infections, or relapsed MM.
Data extraction and quality assessment
Two independent authors evaluated and extracted all candidate articles (Xiaomin Chen and Jiayue Liu). Articles that could not be categorized based on title and abstract were retrieved for full-text review. If disagreement occurred, two authors discussed and arrived at a consensus with a third author (Jialin Duan). For each study, the following items were recorded: first author, year of publication, country, sample size and gender, age, follow-ups, cut-off value, treatment strategy, ISS stage, and HRs with 95%Cis. The Newcastle–Ottawa Scale (NOS) was used to assess each of the included studies’ quality by two independent authors (Xiaomin Chen and Jialin Duan) [15]. The NOS consists of three parts: selection (0–4 points), comparability (0–2 points), and outcome assessment (0–3 points). NOS scores of ≥ 7 were assigned as high-quality studies.
Statistical analysis
HRs and 95%CIs were obtained directly from each of the publications. HR > 1 in MM patients with high RDW suggested a worse prognosis. The relationship between RDW and clinicopathological parameters was evaluated by the combined odds ratio (OR) and its 95%CIs. Cochran’s Q test and Higgins I-squared statistical methods were used to evaluate the heterogeneity of the included studies. A Pheterogeneity < 0.10 or I2 > 50% suggested significant heterogeneity [16]. Both the fixed-effects (Mantel–Haenszel method) model and the random effects (DerSimonian–Laird method) model were used to calculate the combined HRs and 95%CIs [17]. The sources of heterogeneity were explored using subgroup analysis. Sensitivity analysis was used to evaluate the stability of the combined results. Publication bias was assessed by Begg’s funnel plot and Egger’s linear regression test [18, 19]. All p-values were bilateral, and p < 0.05 was considered statistically significant. All the data were analyzed by STATA12.0 software (STATA, Colleges Station, TX).
Results
Study characteristics
The initial search strategies retrieved a total of 82 articles. After meticulous inspection of the articles, 8 articles published between 2014 and 2020 were finally enrolled in our meta-analysis [20,21,22,23,24,25,26,27]. The processes of study selection were summarized in the flow diagram (Fig. 1). One of the articles was divided into two independent samples for retrospective analysis based on whether patients were treated with bortezomib or not. Therefore, we included 8 articles involving 9 studies and 1165 patients. One study used RDW-SD for RDW, and others used RDW-CV. Among them, participants in seven studies were Chinese, and one was Korean. 8 articles directly reported HRs and 95% CIs calculated by multifactorial analysis. All included studies involved all disease stages. The characteristics of the included studies were shown in Table 1.
The prognostic value of RDW
8 studies reported the correlations between RDW and OS. As shown in Fig. 2a, the combined results of the eight studies suggested that elevated RDW was associated with worse OS (HR = 1.91, 95%CI: 1.48–2.46) in MM with no heterogeneity (I2 = 2.4%, Ph = 0.411) 0.5 studies reported the correlations of RDW and PFS. A fixed-effects model (I2 = 0.0%, Ph = 0.857) was also used for studies evaluating PFS. Our results revealed that elevated RDW predicted a poor PFS with a combined HR of 2.87 (95% CI: 2.02–4.07; Fig. 2b).
Then the relationship between RDW and clinicopathological parameters was analyzed using a random utility model. 7 out of 8 studies provided data on RDW and ISS staging. The results showed that RDW levels were unrelated to ISS staging (ISS III VS ISS I-II: OR:1.53; 95%CI:0.97–2.42). However, there was significant heterogeneity between studies (I2 = 63.3%, Ph = 0.012; Fig. 2c).
To analyze the source of heterogeneity, we performed a subgroup analysis of these seven studies, including sample size (< 100 vs. ≥ 100), cut-off values (< 15 vs. ≥ 15), and detection parameters (RDW-CV vs. RDW-SD). The results suggest that the sample size may be a source of heterogeneity (P = 0.002, Table 2). A combination of five studies with sample sizes greater than 100 suggested that elevated RDW was associated with advanced ISS staging (HR = 2.00, 95%CI: 1.37–2.92) with a small heterogeneity (I2 = 35.9%, Ph = 0.182).
Sensitivity analysis and publication bias
Sensitivity analyses on RDW were performed, removing one study at a time to reveal the effect of individual datasets on combined HRs. The results showed that our findings were stable, and no study significantly affected the results (Fig. 3).
In order to evaluate publication bias, we performed Begg’s funnel plot and Egger’s linear regression test. There was no publication bias in the included studies from these tests (Begg’s Test: Pr >|z|= 0.260; Egger’s test: P >|t|= 0.116). Begg’s funnel plot was shown in Fig. 4.
Discussion
MM is an incurable malignancy of the hematopoietic system. It is characterized by the intense proliferation of malignant plasma cells, leading to bone destruction, suppression of bone marrow function, and renal failure [28]. Increasing evidence demonstrates that chronic inflammation plays an important role in MM tumor growth and disease progression [10, 29, 30]. RDW is a parameter automatically measured in the complete blood count (CBC). RDW is an indicator of heterogeneity in the volume of peripheral blood erythrocytes [31]. RDW has recently also been the marker associated with inflammation [32]. It is considered a powerful prognostic marker in various diseases and tumors [33,34,35]. There remains a controversy, however, about the prognostic value of RDW in MM.
Our meta-analysis of 8 articles showed that elevated RDW predicted poor OS/PFS in MM patients (OS: HR = 1.91, 95%CI: 1.48–2.46; PFS: HR = 2.87, 95% CI: 2.02–4.07). There was no significant correlation between RDW and ISS staging. Due to the significant heterogeneity of the results, we performed a subgroup analysis. It is suggested that the heterogeneity of the included studies may derive from the sample size. Studies with sample sizes greater than 100 suggested that elevated RDW was strongly associated with advanced ISS staging. Therefore, it is reasonable to speculate that our overall study on the relationship between RDW and ISS may have a false-negative result.
The possible mechanisms underlying the correlation between elevated RDW and poor prognosis in MM are oxidative stress, chronic inflammation, cellular senescence, and poor nutritional status [36,37,38,39]. All these factors can reduce erythrocyte survival, leading to a higher mixing of circulating erythrocyte volumes [40]. RDW is an indicator of heterogeneity in the volume of peripheral blood erythrocytes [31]. Consequently, RDW is also evaluated.
Multiple myeloma cells have higher levels of intracellular reactive oxygen species (ROS) and lower levels of antioxidant molecules than normal cells due to increased oncogene activation and/or metabolic activity (e.g., high immunoglobulin synthesis rate) [41]. High levels of ROS have been shown to promote proliferation and enhance motility and invasion [42]. Decreased activity of the antioxidant molecules ARE and PON1 are considered to be biomarkers of poor prognosis in multiple myeloma patients as markers of poor prognosis [43]. Chronic persistent inflammation and inflammatory factors (e.g., IL-6) play an important role in MM [44]. Increasing evidence showed that cellular senescence and senescence-associated secretory phenotypes (SASP) establish a tumor environment that supports tumor cell proliferation and survival and promotes the development of multiple myeloma [45]. It has been established that poor nutritional status is a strong indicator of poor prognosis in MM [46, 47]. In conclusion, high RDW is a strong indicator reflecting poor prognosis in MM patients.
There are several limitations in this study that need to be clarified. The main limitation of our study was the small number of eligible studies in terms of establishing prognostic value. Second, these studies were retrospective and more susceptible to some bias. Furthermore, the power of both Egger's test and Begg's test was relatively lower when the number of studies included in the meta-analysis was less than 10. Therefore, publication bias may not be detected by Egger's test and Begg's test. It is hoped that more rationally designed, high-quality, multi-center studies will be conducted in the future to enrich our results further.
Conclusion
In summary, this meta-analysis demonstrated that elevated RDW might be a negative prognostic factor for patients with MM.
Availability of data and materials
All data analyzed during this study are included in this published article.
Abbreviations
- MM:
-
Multiple myeloma
- RDW:
-
Red cell distribution width
- NOS:
-
The Newcastle–Ottawa Scale
- 95%CI:
-
95% Confidence interval
- HR:
-
Hazard ratio
- OR:
-
Odds ratio
- OS:
-
Overall survival
- PFS:
-
Progress free survival
- ISS:
-
International Staging System
References
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7–33.
Hallek M, Haller H. Multiple myeloma. Internist (Berl). 2019;60(1):1–2.
Kumar SK, Dispenzieri A, Lacy MQ, Gertz MA, Buadi FK, Pandey S, et al. Continued improvement in survival in multiple myeloma: changes in early mortality and outcomes in older patients. Leukemia. 2014;28(5):1122–8.
Cavo M, Gay F, Beksac M, Pantani L, Petrucci MT, Dimopoulos MA, et al. Autologous haematopoietic stem-cell transplantation versus bortezomib-melphalan-prednisone, with or without bortezomib-lenalidomide-dexamethasone consolidation therapy, and lenalidomide maintenance for newly diagnosed multiple myeloma (EMN02/HO95): a multicentre, randomised, open-label, phase 3 study. The Lancet Haematology. 2020;7(6):e456–68.
Varga C, Maglio M, Ghobrial IM, Richardson PG. Current use of monoclonal antibodies in the treatment of multiple myeloma. Br J Haematol. 2018;181(4):447–59.
Libby E, Garcia D, Quintana D, Fekrazad MH, Bauman J, Ebaid A, et al. Disease-specific survival for patients with multiple myeloma: significant improvements over time in all age groups. Leuk Lymphoma. 2014;55(12):2850–7.
Mikkilineni L, Kochenderfer JN. CAR T cell therapies for patients with multiple myeloma. Nat Rev Clin Oncol. 2021;18(2):71–84.
Palumbo A, Avet-Loiseau H, Oliva S, Lokhorst HM, Goldschmidt H, Rosinol L, et al. Revised International Staging System for Multiple Myeloma: A Report From International Myeloma Working Group. J Clin Oncol. 2015;33(26):2863–9.
Kastritis E, Terpos E, Roussou M, Gavriatopoulou M, Migkou M, Eleutherakis-Papaiakovou E, et al. Evaluation of the Revised International Staging System in an independent cohort of unselected patients with multiple myeloma. Haematologica. 2017;102(3):593–9.
Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420(6917):860–7.
Dang C, Wang M, Qin T, Qin R. Clinical importance of preoperative red-cell volume distribution width as a prognostic marker in patients undergoing radical surgery for pancreatic cancer. Surg Today. 2022;52(3):465–74.
Cheng KC, Lin YM, Liu CC, Wu KL, Lee KC. High Red Cell Distribution Width Is Associated with Worse Prognosis in Early Colorectal Cancer after Curative Resection: A Propensity-Matched Analysis. Cancers. 2022;14(4):945.
Yao D, Wang Z, Cai H, Li Y, Li B. Relationship between red cell distribution width and prognosis in patients with breast cancer after operation: a retrospective cohort study. Biosci Rep. 2019;39(7):BSR20190740.
Rajkumar SV, Dimopoulos MA, Palumbo A, Blade J, Merlini G, Mateos MV, et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 2014;15(12):e538–48.
Lo CK, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 2014;14:45.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
DerSimonian R, Laird N. Meta-analysis in clinical trials revisited. Contemp Clin Trials. 2015;45(Pt A):139–45.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Lee H, Kong S-Y, Sohn JY, Shim H, Youn HS, Lee S, et al. Elevated Red Blood Cell Distribution Width as a Simple Prognostic Factor in Patients with Symptomatic Multiple Myeloma. Biomed Res Int. 2014;2014:145619.
Meng S, Ma Z, Lu C, Liu H, Tu H, Zhang W, et al. Prognostic Value of Elevated Red Blood Cell Distribution Width in Chinese Patients with Multiple Myeloma. Ann Clin Lab Sci. 2017;47(3):282–90.
Wang J, Xie X, Cheng F, Zhou X, Xia J, Qian X, et al. Evaluation of pretreatment red cell distribution width in patients with multiple myeloma. Cancer Biomark. 2017;20(3):267–72.
Ma Y, Jin Z, Zhou S, Ye H, Jiang S, Yu K. Prognostic significance of the red blood cell distribution width that maintain at high level following completion of first line therapy in mutiple myeloma patients. Oncotarget. 2018;9(11):10118–27.
Zhou D, Xu P, Peng M, Shao X, Wang M, Ouyang J, et al. Pre-treatment red blood cell distribution width provides prognostic information in multiple myeloma. Clin Chim Acta. 2018;481:34–41.
Liu S, Shi J, Guo H, Xu F, Wei M, Sun K, et al. Prognostic Significance Of The Inflammatory Index-Based Scoring System In Patients Preliminarily Diagnosed With Multiple Myeloma In The Bortezomib-Based Chemotherapy Era. Cancer Manag Res. 2019;11:9409–20.
Sun C, Ye JN, Wang H, Zhu JW, Zhou X, Li JY. Prognostic Value of Red Blood Cell Distribution Width in Senile Potients with Non-trans planted Multiple Myeloma. Zhongguo Shi Yan Xue Ye Xue Za Zhi. 2019;27(1):115–22.
Li DY, Yue YF, Chen L, Zhao ZG, Wang XF, Xu W, et al. Standard deviation of red blood cell distribution width in predicting the prognosis of 143 patients with newly treated multiple myeloma. Chin J Cancer Prevent Treatment. 2020;27(6):475–9 and 498.
Goldschmidt H. Clinical update-multiple myeloma. Radiologe. 2022;62(1):3–11.
de Jong MME, Kellermayer Z, Papazian N, Tahri S, Hofste Op Bruinink D, Hoogenboezem R, et al. The multiple myeloma microenvironment is defined by an inflammatory stromal cell landscape. Nature immunol. 2021;22(6):769–80.
Rasche L, Weinhold N. Pathogenesis of multiple myeloma. Internist (Berl). 2019;60(1):3–9.
Montagnana M, Danese E. Red cell distribution width and cancer. Ann Transl Med. 2016;4(20):399.
Salvagno GL, Sanchis-Gomar F, Picanza A, Lippi G. Red blood cell distribution width: A simple parameter with multiple clinical applications. Crit Rev Clin Lab Sci. 2015;52(2):86–105.
Arbel Y, Shacham Y, Finkelstein A, Halkin A, Milwidsky A, Berliner S, et al. Red blood cell distribution width (RDW) and long-term survival in patients with ST elevation myocardial infarction. Thromb Res. 2014;134(5):976–9.
Hu L, Li M, Ding Y, Pu L, Liu J, Xie J, et al. Prognostic value of RDW in cancers: a systematic review and meta-analysis. Oncotarget. 2017;8(9):16027–35.
Wang C, Zhang H, Cao X, Deng R, Ye Y, Fu Z, et al. Red cell distribution width (RDW): a prognostic indicator of severe COVID-19. Ann Transl Med. 2020;8(19):1230.
Ferrucci L, Guralnik JM, Woodman RC, Bandinelli S, Lauretani F, Corsi AM, et al. Proinflammatory state and circulating erythropoietin in persons with and without anemia. Am J Med. 2005;118(11):1288.
Kiefer CR, Snyder LM. Oxidation and erythrocyte senescence. Curr Opin Hematol. 2000;7(2):113–6.
Wang PF, Song SY, Guo H, Wang TJ, Liu N, Yan CX. Prognostic role of pretreatment red blood cell distribution width in patients with cancer: A meta-analysis of 49 studies. J Cancer. 2019;10(18):4305–17.
Weiss G, Goodnough LT. Anemia of chronic disease. N Engl J Med. 2005;352(10):1011–23.
Patel KV, Semba RD, Ferrucci L, Newman AB, Fried LP, Wallace RB, et al. Red cell distribution width and mortality in older adults: a meta-analysis. J Gerontol A Biol Sci Med Sci. 2010;65(3):258–65.
Lipchick BC, Fink EE, Nikiforov MA. Oxidative stress and proteasome inhibitors in multiple myeloma. Pharmacol Res. 2016;105:210–5.
Burdon RH. Superoxide and hydrogen peroxide in relation to mammalian cell proliferation. Free Radic Biol Med. 1995;18(4):775–94.
Ellidag HY, Eren E, Aydin O, Yildirim M, Sezer C, Yilmaz N. Multiple myeloma: relationship to antioxidant esterases. Med Princ Pract. 2014;23(1):18–23.
Musolino C, Allegra A, Innao V, Allegra AG, Pioggia G, Gangemi S. Inflammatory and Anti-Inflammatory Equilibrium, Proliferative and Antiproliferative Balance: The Role of Cytokines in Multiple Myeloma. Mediators Inflamm. 2017;2017:1852517.
Hu D, Yuan S, Zhong J, Liu Z, Wang Y, Liu L, et al. Cellular senescence and hematological malignancies: From pathogenesis to therapeutics. Pharmacol Ther. 2021;223:107817.
Liang F, Dong XY, Tang GF, Qi KM, Chen W, Sang W, et al. Influence of prognostic nutritional index and controlling nutritional status on the prognosis of patients with multiple myeloma. Zhonghua Xue Ye Xue Za Zhi. 2021;42(4):332–7.
Zhou X, Lu Y, Xia J, Mao J, Wang J, Guo H. Association between baseline Controlling Nutritional Status score and clinical outcomes of patients with multiple myeloma. Cancer Biomark. 2021;32(1):65–71.
Acknowledgements
We are grateful to all researchers of enrolled studies.
Funding
This study was supported by Sichuan department of science and technology (grant no.20YYJC0940).
Author information
Authors and Affiliations
Contributions
Xiaomin Chen and Jiayue Liu designed the project. Xiaomin Chen, Jiayue Liu and Jialin Duan performed data extraction and analysis. Quality assessment was conducted by Hao Xiong, Yang Liu and Xinwen Zhang. Xiaomin Chen and Chunlan Huang made critical changes to the manuscript and oversaw the project. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, X., Liu, J., Duan, J. et al. Is RDW a clinically relevant prognostic factor for newly diagnosed multiple myeloma? A systematic review and meta-analysis. BMC Cancer 22, 796 (2022). https://doi.org/10.1186/s12885-022-09902-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-022-09902-9