Abstract
Background
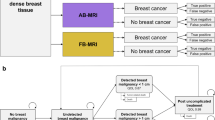
Abbreviated breast MRI (A-MRI) substantially reduces the image acquisition and reading times and has been reported to have similar diagnostic accuracy as a full diagnostic protocol but has not been evaluated prospectively with respect to impact on psychological distress in women with a prior history of breast cancer (PHBC). This study aimed to determine if surveillance mammography (MG) plus A-MRI reduced psychological distress and if A-MRI improved cancer detection rates (CDR) as compared to MG alone.
Methods
This prospective controlled trial of parallel design was performed at a tertiary cancer center on asymptomatic women with PHBC who were randomized into two groups: routine surveillance with MG or intervention of MG plus A-MRI in a 1:1 ratio. Primary outcome was anxiety measured by four validated questionnaires at three different time-points during the study. Other parameters including CDR and positive predictive value for biopsy (PPV3) were compared between imaging modalities of MG and A-MRI. Tissue diagnoses or 1 year of follow-up were used to establish the reference standard. Linear mixed models were used to analyze anxiety measures and Fisher’s exact test to compare imaging outcomes.
Results
One hundred ninety-eight patients were allocated to either MG alone (94) or MG plus A-MRI (104). No significant group difference emerged for improvement in trait anxiety, worry and perceived health status (all Time-by-surveillance group interaction ps > .05). There was some advantage of A-MRI in reducing state anxiety at Time 2 (p < .05). Anxiety scores in all questionnaires were similarly elevated in both groups (50.99 ± 4.6 with MG alone vs 51.73 ± 2.56 with MG plus A-MRI, p > 0.05) and did not change over time. A-MRI detected 5 invasive cancers and 1 ductal carcinoma in situ (DCIS), and MG detected 1 DCIS. A-MRI had higher incremental CDR (48/1000(5/104) vs MG 5/1000(1/198, p = 0.01)) and higher biopsy rates (19.2% (20/104) vs MG 2.1% (2/94), p < 0.00001) with no difference in PPV3 (A-MRI 28.6% (6/21) vs MG 16.7% (1/6, p > .05).
Conclusion
There was no significant impact of A-MRI to patient anxiety or perceived health status. Compared to MG alone, A-MRI had significantly higher incremental cancer detection in PHBC. Despite a higher rate of biopsies, A-MRI had no demonstrable impact on anxiety, worry, and perceived health status.
Trial registration
ClinicalTrials.gov (NCT02244593). Prospectively registered on Sept. 14, 2014.
Similar content being viewed by others
Background
Women with a prior personal history of breast cancer (PHBC) often have a high level of anxiety related to breast cancer surveillance [1]. Their actual recurrence rates are estimated in the order of 1% per year [2, 3], and depend on tumor size, histology and nodal status at diagnosis, with 5-year risks of recurrence of 7% for stage I, 11% for Stage II and 13% for stage III, and distant recurrences of 10- 41% at 20 years after completion of adjuvant chemotherapy [4, 5]. Early detection decreases mortality for women with breast cancer [6,7,8]. In women with PHBC, the survival benefit is improved if new or recurrent breast cancer is found on surveillance mammography (MG) instead of physical examination [9]. However, MG has been shown to be less sensitive in women with PHBC, with sensitivity of 65.4% compared with 76.5% in women with no PHBC [10]. Breast MRI is the most sensitive test for detecting breast cancer [11]. Breast MRI is currently recommended for women with PHBC and dense tissue or those diagnosed by age 50, as per American College of Radiology (ACR) guidelines [12]. Several other national guidelines do not recommend surveillance imaging with breast MRI after a personal history of breast cancer unless someone has a hereditary mutation or mammographically occult malignancy and of itself, breast tissue density is not an indication for surveillance breast MRI. Compliance with MRI screening has been shown to be low, on the order of 25%, due both to lack of availability and high costs associated with lengthy acquisition times [13, 14]. Abbreviated breast MRI (A-MRI), which substantially reduces the image acquisition and reading times, has been reported to have similar diagnostic accuracy as a full diagnostic protocol [13, 15,16,17,18,19]. Currently, A-MRI has not been adopted as the standard for screening for breast cancer and more studies are required to evaluate outcomes.
Prior studies demonstrated that supplementary MRI surveillance in women at high risk of breast cancer does not impact anxiety, cancer-specific distress or health-related quality of life [1, 20]. This is the first study to our knowledge to evaluate the psychological effect of adding abbreviated MRI to MG surveillance in women with PHBC.
The primary purpose of the current study was to determine if the intervention of adding A-MRI to MG surveillance was more effective than MG alone in reducing patient anxiety and, secondarily, if A-MRI improved cancer detection in women with PHBC. Our hypothesis was that the MRI group would be superior to mammography alone group to reduce patient anxiety.
Methods
Study subjects
This prospective randomized controlled trial of parallel design was performed at a large tertiary care academic medical center and was approved by the hospital’s institutional review board. Our study adheres to the CONSORT guidelines. Patients at a single tertiary care cancer center were approached by their treating oncologists or surgeons during routine clinical appointments if they met the eligibility criteria and their scheduled appointment time allowed. The patients’ oncologists or surgeons obtained written informed consent. Eight oncologists and three breast surgeons recruited patients between 2/1/2015 and 4/30/2019. Patients were followed for a minimum of 12 months.
The eligibility criteria included: (a) female patients 18 years or older; (b) PHBC (including DCIS and invasive ductal or lobular carcinoma); (c) prior unilateral mastectomy or breast conservation surgery; (d) treatment for breast cancer completed; and (e) no symptoms of breast cancer. Patients were excluded if they were considered high-risk (lifetime risk ≥ 25%) [21], were unable to undergo an MRI due to either physical or mental issues (i.e.: severe claustrophobia, allergy to gadolinium, severe renal failure), had bilateral mastectomies, were pregnant or breastfeeding, or had undergone a breast MRI within the last 6 months. Regular surveillance imaging consisted of annual surveillance MG, irrespective of breast tissue density. All patients had undergone prior mammographic imaging, and some (< 50%) had undergone prior breast MRI imaging.
Eligible patients were randomized in a 1:1 allocation ratio to one of the two arms of the study: 1) surveillance with MG or 2) MG plus A-MRI, with use of permuted blocks of variable length (2, 4, and 6) to ensure that recruiting physicians remained unaware of the randomization. Researchers or study participants were not blinded to their allocation. Patients could only participate once in the study.
Imaging technique and interpretation
All mammographic examinations were performed using a full-field digital technique (Hologic, Bedford, MA, USA) in accordance with national guidelines. Standard two-dimensional craniocaudal (CC) and mediolateral oblique (MLO) views were obtained.
All abbreviated dynamic contrast material-enhanced breast MRIs were performed with one 3 T system (Magnetom TrioTim Syngo, Siemens). The standardized protocol consisted of 8-channel breast coil (Sentinelle Medical Inc.), T1 localizer, T1 dynamic contrast-enhanced fat-suppressed with one precontrast and one 2 min postcontrast (3D transverse, phase encoding direction right to left, phase resolution of 60%, phase partial Fourier 6/8, no interpolation, FA 10 degrees, TR 4.07 ms and TE 1.96 ms, no IR, NEX 1, Voxel size: 1 × 1x1 mm, acceleration factor 4, no interpolation, base resolution 448,1:01 min, slice thickness 1 mm). Post-processing axial subtracted sequences and axial and sagittal maximum intensity projection were generated of the subtracted images. No T2-weighted sequences were obtained. For all examinations, gadolinium contrast material (Gadovist) was power injected (0.1 mmol/kg at 2 mL/s) followed by a 20 mL saline flush. The entire protocol took 3 min.
Surveillance MG and A-MRI were reviewed by one of two breast radiologists independently (the first with 8 years of experience reading mammography and breast MRI and the second reader with 20 years reading mammography and breast MRI) using ACR Breast Imaging-Reporting Data System (BI-RADS) lexicon[22]. For patients in the A-MRI group, MG and A-MRI studies were performed on the same day according to the protocol. Radiologists were not blinded but reported each modality separately according to the imaging modality findings, with the mammograms interpreted first. Based on the imaging findings, additional mammographic images, including diagnostic tomosynthesis, or targeted ultrasound were requested at the discretion of the interpreting radiologist. Findings and management were communicated to the patient by telephone by the reporting radiologist. Subsequent imaging was performed on separate visits, within 3 weeks of the MG or A-MRI. Histologic samples for pathologic diagnosis were obtained under ultrasound (14G, 5–6 cores), stereotactic (10G, 6–12 cores) or MRI (10G, 6–12 cores) guidance.
Anxiety measures
Patients in both groups were asked to fill out four validated self-report questionnaires that measure anxiety level and overall health [23,24,25,26]) (see supplemental materials). The primary outcome was the State-Trait Anxiety Inventory (STAI) [23]. This STAI consists of two separate 20-item scales that assess state anxiety (S-Anxiety) (i.e., how the person feels at this moment) and trait anxiety (T-Anxiety) (i.e., how the personal generally feels). The items are rated on a 1 to 4 scale with total scores ranging from 20–80. Cut-off scores of ≥ 32.2 and ≥ 31.8 indicate elevated levels of state and trait anxiety, respectively. Both STAI scales have solid psychometric properties and are sensitive to assessment of longitudinal change. There are no validated cutoff scores for the STAI scales in women with PHBC, however a cutoff score of 41 on the trait form of the STAI and 44 on the state form of the STAI have been used in previous research to identify clinical levels of anxiety in women with breast cancer [27, 28]. Other psychological measures included the Penn State Worry Questionnaire (PSWQ) [24], Breast Cancer Worry Scale (BCWS) [25], and the Health Status Questionnaire 12 (HSQ-12) [26]. The PSWQ [24] is a 16-item self-report questionnaire which measures frequency and intensity of worry symptoms. Items are rated on a 5-point scale, with total scores ranging from 16–80. A score between 16–39 indicates low worry, 40–59 moderate worry and 60–80 high worry. The BCWS [25] is a 3-item scale which measures frequency of breast cancer worry and the impact of worrying on mood and ability to perform daily activities. Higher scores indicate greater cancer worry. The HSQ-12 [26] assesses the impact of health on social, emotional and physical functioning over the past four weeks. Depending on the item, questions are rated of a 3-point, 5-point and 6-point scale. Items were recoded using the method described by Barry et al. [26]. Total HSQ scores range from 0 to 800, with higher scores indicating better health status. The questionnaires were completed upon enrolment during consultation at time 1 (T1) when the patients were due for their surveillance test(s) to measure baseline levels of anxiety, at time 2 (T2) that occurred after the patient received of their surveillance MG and/or MRI test results, and then 6 months later at time 3 (T3), to determine if there was a sustained effect observed from the type of surveillance test. T3 questionnaires were mailed to patients and returned to the study coordination center.
Data collection and statistical analysis
Medical records were reviewed to determine patient age, family history of breast and/or ovarian cancer in a first-degree relative, surgery modality, initial breast tumor stage (TNM), histology, hormone receptor status, months since diagnosis of breast cancer and breast density. Results were compared between the two groups. For malignant or atypical/high-risk lesions, surgical pathologic results were reviewed when available. Imaging and clinical follow-up were determined by review of the hospital picture archiving system (PACS) and medical records as well as the digital imaging repository which includes all clinics and hospitals that serve the region’s population of 1.2 million. The emigration rate in the region is < 0.5% per year [29]. Imaging follow-up for all patients with benign imaging or pathology was documented with the date of the most recent negative mammogram.
The anxiety measures were analyzed using SPSS Statistics version 25. Analysis was based on intent-to-treat (ITT) principles. Data were analyzed using linear mixed models, with surveillance groups (MG only versus MG plus A-MRI), time of assessment (T1, T2, T3), and Intervention by Time interaction as fixed factors. Models were estimated using Restricted Maximum Likelihood (REML) with an unstructured covariance structure to account for correlations among repeated measures over time. A significant Time by surveillance group interaction would suggest that changes in measures over time were different between the surveillance method; significant interactions were further analyzed with pairwise least square mean comparisons. Data from missing questionnaires were not imputed because our analytical strategy using REML allowed the estimation of reliable parameters without the need for imputation of the data under an assumption of missing at random (MAR) [30]. Descriptive statistics were calculated using a spreadsheet software program (Excel, Version 2013, Microsoft). Screening outcomes were compared between groups using Fisher’s exact test. Sample size calculation was based on primary outcome the STAI. There is no generally accepted minimal clinically important difference in the STAI subscales and a 4-point difference was selected to be a minimal clinically important difference. This was based on previous study by Millar et al. [28] which used a 4-point difference in the STAI and on consensus with the research team and the experience of the psychologist researcher. In order to have 80% power to detect a 4-point difference between the groups at any of the three time points, we planned 134 patients per group. Recruitment stopped early due to differences in cancer detection rates (CDR). Results were considered significant if p < 0.05.
Imaging modalities (MG, A-MRI), and BI-RADS final assessment categories for each modality were noted. Imaging findings and outcomes were documented for all BI-RADS 3, 4 and 5 lesions, including suspicious extra-mammary findings. Results were compared between MG and A-MRI. A screening examination was considered as positive when additional diagnostic imaging was recommended prior to the next routine screening examination and included BI-RADS 0, 3, 4 and 5, defined as abnormal interpretations. True positive findings were defined as a cancer diagnosis within 12 months of a positive screening examination. Imaging studies were considered false negatives if there was a tissue diagnosis of cancer within 12 months of a negative study, or in the surveillance groups if there was a tissue diagnosis of cancer in the follow-up period. The following performance metrics were calculated for each modality: CDR, abnormal interpretation rate (AIR), biopsy rate, positive predictive value for biopsy recommendations (PPV2 = biopsies recommended/cancers diagnosed), positive predictive value for biopsies performed (PPV3 = biopsies performed/cancers diagnosed), sensitivity and specificity.
Results
A total of 202 of 1000 patients fulfilled the eligibility criteria (Fig. 1) between 2/1/2015 and 4/30/2019. At enrollment, 94 were randomized to surveillance with MG alone and 108 to MG plus A-MRI. Of these, four patients from MG plus A-MRI group withdrew from the study a few days before undergoing the imaging for different reasons: two patients were discovered to have breast cancer metastases on separate imaging done prior to undergoing the surveillance imaging, one patient developed sepsis before the imaging was performed and her doctor decided to postpone contrast injection and one patient opted to withdraw from the study before undergoing the imaging. Accordingly, the study population consisted of 198 patients: 47.5% (94/198) randomized to regular surveillance with MG and 52.5% (104/198) to surveillance with MG plus A-MRI. All patients completed the imaging to which they were randomized and there were no patient crossovers from the MG only group to A-MRI. Among the 104 patients who had MG plus A-MRI, 82.7% (86/104) had both imaging exams the same day and 17.3% (18/104) on different days (average 33.2 days (range: 1–147)) due to various scheduling conflicts.
Baseline demographic and clinical characteristics
Patients’ demographic and clinical characteristics are presented in Table 1. No important differences in age, family history of breast and/or ovarian cancer, surgery modality, months since diagnosis, breast density, initial tumor histology, stage, or hormone receptor status were noted between the two groups, although a nonsignificant higher number of patient with triple negative cancers was observed in the group that received A-MRI.
Results regarding anxiety
The observed means (± standard deviations) for the self-report questionnaires and least square mean difference between the surveillance groups at T2 and T3 are displayed in Table 2. 197 participants completed questionnaires at T1 (Baseline), 92 patients in MG only and 105 in MG plus A-MRI groups. At Time 2, data were available for 143 participants; 60 in MG and 83 in MG plus A-MRI groups. At T3 data were available for 102 participants; 38 women in MG and 64 in MG plus A-MRI groups. The surveillance groups did not differ significantly on any of the baseline measures. Linear mixed models revealed that our primary outcome STAI-Trait Anxiety did not change over time (Time main effect p = 0.51) and did not differ between the groups (Time x Surveillance Group interaction p = 0.20). However, there was a significant Time main effect (p < 0.001) and Time x Surveillance Group interaction (p = 0.022) for the STAI-State Anxiety. Post-hoc tests revealed that for both groups, state anxiety decreased significantly between T1 and T2 (estimated mean change = -6.80 [95% CI, -8.58 to -5.02] for MG only (p < 0.001) and -8.17 [95% CI, -9.70 to -6.34] for MG plus A-MR (p < 0.001), and increased significantly from T2 to T3 (estimated mean change 5.86 [95% CI, 3.97 to 7.76] for MG only (p < 0.001) and 8.12 [95% CI, 7.23 to 10.40] for MG plus A-MRI (p < 0.001). Between groups comparisons indicated that state anxiety at T2 was significantly lower in the MG plus A-MRI group (p = 0.03), but less than a 4-point difference. Levels of worry did not significantly change over time (Time main effect p = 0.14 and p = 0.73 for the PSWQ and BCWQ, respectively) and did not differ between the groups (Time x Surveillance Group interaction p = 0.57 and p = 0.48 for the PSWQ and BCWQ, respectively). There was a significant Time main effect for self-report health status (p < 0.05), but no significant Time x Surveillance Group interaction (p = 0.13). Overall, HSQ-12 scores decreased from T1 to T3 (estimated mean change -0.27.91 [95% CI -47.60 to -8.22], p < 01).
Using the cutoff score of 41 on the trait form of the STAI, the percentage of women with anxiety in the clinical range was 100% at T1 and T2 and T3 for both the MG and the MG + A-MRI groups. Using a cutoff score of 44 on the state form of the STAI, the majority of women in the MG and MG + A-MRI groups had scores in the clinical range at T1 (100% and 99%) and T3 (95.9% and 100%). At T2 however, more (57.1% (32/56)) women in the MG group than those in MG + A-MRI group (32.9% (27/82)) had scores in the clinical range, with the difference between groups statistically significant (p < 0.01). Within the MRI group, the 23 recalled patients had significantly higher PSWQ scores at T2 when compared with the 80 patients who were not recalled (mean score: 47.16 ± 14.7 vs 39.33 ± 14.08, p < 0.05, Cohen’s d = 0.55), with a similar trend found for State STAI scores (45.22 ± 7.1 vs 42.23 ± 5.95, p = 0.075, Cohen’s d = 0.48). However, the recalled women had scores that returned to baseline by T3 with no lasting effect on PSWQ (mean score: 48.66 ± 16.29 vs 43.30 ± 13.51, p > 0.05) or State STAI (52.20 ± 2.32 vs 51.58 ± 2.63, p > 0.05).
Outcomes according to surveillance groups
There was 1 cancer (DCIS) detected in the MG group during the study, and 3 cancers (2 invasive and 1 DCIS) were diagnosed at follow-up. In the MG plus A-MRI surveillance group, 5 breast cancers (1 DCIS and 4 invasive cancers) and 1 breast cancer metastasis to the lung were detected, with no cancers diagnosed at follow-up. The outcomes for each group are provided in Table 3. Although there were significantly more recalls and biopsies performed in the MG plus A-MRI than the MG group (recalls of 27/104 (26%) vs 4/94 (4.26%) (p < 0.05) and biopsies of 20/104 (19.2%) vs 2/94 (2.13%)(p = 0.001) respectively), with lower specificity (77.8% MG + A-MRI vs 96.7% MG (p = 0.0001), the sensitivity for the MG plus A-MRI group was higher 5/5(100%) than the MG group 1/4 (25%)(p = 0.048) and there was a higher CDR in the MG plus A-MRI group (5/104 (48.1/1000)) than the MG group (1/94 (10.6/1000) (p = 0.1294)).
Findings according to imaging modality
Outcomes according to imaging modality are presented in Table 4. Among the 302 imaging examinations performed (198 MG and 104 A-MRI), 9 MG and 29 A-MRI were interpreted as abnormal (17%) (Fig. 2).
Woman (60–70 years old) with PHBC treated by right mastectomy 12 years prior to study. A MLO and B CC Left surveillance mammograms show heterogeneously dense breast tissue (BI-RADS C) with normal, stable findings. C Axial 3D MIP at 2 min post contrast performed after mammograms shows right mastectomy with no chest wall abnormalities and an irregular 4.5 cm enhancing mass (circle) in the medial left breast reported as BI-RADS 4B. The second circumscribed mass in the lateral breast corresponded with a benign fibroadenoma (arrow). D Axial 2 min post contrast subtracted image demonstrates the spiculated enhancing mass in the upper medial quadrant of the left breast (circle). E Axial image from MRI biopsy demonstrates the needle sampling the mass (circle), diagnostic for pleomorphic lobular carcinoma in situ, which was confirmed at surgical excision to be associated with invasive lobular carcinoma
Mammography
There were 198 mammographic examinations performed: 94 MG alone and 104 MG with A-MRI; 95.5% (189/198) were negative or benign (BI-RADS 1 and 2), 4.5% (9/198) were recalled (BI-RADS 0) and 3.0% (6/198) presented findings suspicious for malignancy (BI-RADS 4) and underwent biopsy. One cancer was detected (Table 5) and no high-risk lesions were identified.
MRI
104 A-MRI studies were performed; 72.1% (75/104) were negative or benign (BI-RADS 1 and 2); 27.9% (29/104) were abnormal including extra-mammary findings, of which 19.2% (20/104) had suspicious breast lesions (BI-RADS 4 or 5); and 18.2% (19/104) underwent breast biopsy. One breast mass detected by A-MRI was not seen at the time of MRI-guided biopsy and showed stability on 6-month follow-up MRI. Breast cancers were detected in 5 patients; 4 invasive carcinomas and one DCIS (Table 4). All five cancers were only detected with A-MRI, 2 of which were in patients with original triple negative breast cancers (Fig. 2). Three patients had suspicious extra mammary findings: one lung mass seen in the right middle lobe on the A-MRI, and two bone lesions seen in the sternum and manubrium, respectively. The lung mass was confirmed to be a metastatic carcinoma from breast primary on CT guided transthoracic lung biopsy, the manubrial lesion was confirmed to be a hemangioma on bone scan and the sternal lesion was confirmed to be a hibernoma on CT guided biopsy. Of the MRI detected breast cancers, none was identified on mammography, even in retrospect. No high-risk lesions were detected.
The mammographic CDR of 5/1000 (1/98) was significantly lower than the CDR of 58/1000 (6/104, p = 0.003) for A-MRI including the extramammary findings, and CDR of 48/1000 (5/104, p = 0.0109) for MRI including only the breast findings. The diagnostic indicators for both modalities are presented in Table 6. Sensitivity for MG 14.2% (1/6)) was lower than A-MRI 100% (5/5) (p < 0.004); specificity for MG 95.8% (183/191) higher than MRI 76.5% (78/99) (p < 0.00001) and PPV3 for MG 16.7% (1/6) was lower than MRI 28.6% (5/19) (p = 0.55).
Necessity for full diagnostic or repeat MRI
Three patients required further investigation requiring diagnostic full MRI based on the radiologist’s uncertainty of the findings seen on the A-MRI: 1 had a mass which was benign on assessment (fat necrosis) determined by the full protocol, one was a BI-RADS 3 lesion which showed stability on 12- month follow-up and one had BI-RADS 4B lesion that led to a benign MRI-guided biopsy of Pseudoangiomatous stromal hyperplasia. A fourth patient had motion artifact and required a repeat abbreviated MRI that was normal and of high technical quality.
Follow-up
All 191 patients with benign imaging or pathology results underwent clinical and imaging follow-up at the same center, for an average 24 months (10–56 months). There were no cancers found retrospectively as false negatives on follow-up. 1.57% (3/191) had breast cancer on follow-up, all from the surveillance MG only group. Of the 3 cancers diagnosed on subsequent surveillance imaging with MG, two were diagnosed at 26 and 27 months with MG (DCIS and invasive ductal carcinoma (IDC), T1N0M0) and one was diagnosed at 50 months on MRI (IDC, T2N0M0). Two were new cancers in the contralateral breast and one DCIS was in the ipsilateral breast; no cancer was seen retrospectively on initial MG and/or MRI. Of the remaining 188 patients with no cancer diagnosed on follow-up, 98.9% (186/188) had follow up of 12 months or longer and 1.06% (2/188) had follow-up of shorter than 12 months. There were no patients lost to follow-up.
Discussion
This prospective randomized controlled trial showed that undergoing A-MRI had no demonstrable impact on psychological well-being in women with a history of breast cancer. Our primary outcome trait anxiety was moderately high in all patients at baseline and did not change significantly over time; the average score of trait anxiety at the 6-month follow-up was 50.99 ± 4.6 with MG vs 51.73 ± 2.56 with A-MRI, p > 0.05. Similarly, self-report worry, including worry of breast cancer recurrence, did not change over time for both conditions. Although there was some benefit of A-MRI over MG alone in reducing state anxiety when participants received their results (T2), which may reflect a higher confidence in women undergoing A-MRI, the difference was less than 4 points and therefore not considered clinically meaningful. Nevertheless, it should be noted that compared to women in the MG alone group, significantly fewer women in the A-MRI group had state anxiety scores in the clinical range. Despite higher rates of biopsies and abnormal interpretations with A-MRI, it is notable that breast A-MRI was not associated with an increase in psychological distress that was sustained over the three time periods. Considering the sustained elevated levels of anxiety and worsening in quality of health in these patients, ongoing consideration and monitoring of mental health issues is recommended. PHBC patients may benefit from psychologist counselling and ongoing support.
Our results support other studies on the impact of breast MRI on anxiety. The Dutch MRI screening (MRISC) study of patients at high risk for breast cancer found that the addition of breast MRI did not affect quality of life or anxiety [20]. In a more recent prospective non-randomized multicentre study, 1561 women at intermediate and high breast cancer risk were noted to have similar moderate distress levels, and there were no more harmful psychological effects observed between standard MG plus ultrasound as compared with the addition of MRI to standard imaging [1].
A significantly higher CDR was noted in the patients who underwent A-MRI as compared with MG only, despite similar baseline demographic and clinical characteristics. We expected a recurrence rate of 1% per year after breast cancer diagnosis [31, 32]. Eighty percent of patients were within 5 years of their breast cancer diagnosis, and 9 in-breast recurrences and 1 lung metastasis were observed, within the expected range. Our study demonstrated A-MRI had a sensitivity of 100% and CDR 48/1000 as compared to mammography’s sensitivity of 14.2% and CDR 5/1000. The low sensitivity of mammography of 14% may be attributed to an early stage of diagnosis of breast cancer in most patients with A-MRI as well as the fact that 49% of women had dense breast tissue, which lowers mammographic sensitivity, with four patients with invasive carcinomas found with A-MRI in women with dense breast tissue (Table 5). The abnormal interpretation and biopsy rates were significantly higher for A-MRI than MG, 25% and 18.3% for A-MRI and 4.5% and 3% for MG, respectively. PPV3 was higher with A-MRI than MG, 26.3% vs 16.7%, although this difference did not reach statistical significance. When extra-mammary findings were included, A-MRI offered the benefit of detecting an incidental lung metastasis.
There have been multiple studies of A-MRI since Dr. Kuhl published her landmark study [13, 15,16,17,18,19, 33,34,35]. In a similar study of 725 women with PHBC, Choi et al. found 12 cancers using A-MRI, for a CDR 15 per 1000 [34], with comparable sensitivity of 100% and specificity of 89.2%. The results of A-MRI in our study are comparable to reported sensitivities (86–100%) and specificities (45–95.3%). However, our specificity of 76.5% was lower than the ACR benchmark for screening breast MRI 85–90% [22]. PPV3 26.3% was in the reported range for A-MRI (9.2–70.2%) and met the ACR benchmark of 20–50% [22]. In 2020, Park et al. retrospectively compared abbreviated to full MRI in 1200 women with PHBC, 656 with A-MRI vs 656 patients with full protocol and found no significant differences in sensitivity (70% vs 100%) or specificity (98% vs 96.9%), negative predictive values (99.5 and 100%) and PPV (35% vs 23%) (all p > 0.05) [36].
We recognize some limitations of our study. Patients were recruited by their oncologists or treating surgeons, which could have introduced a bias in patient selection. This may have partly explained the CDR in the MG plus A-MRI group. Nonetheless, the fact that randomization was blinded mitigated any potential bias of intervention arm selection and there were no clinical differences between the two surveillance groups. As well, in follow-up, similar numbers of cancers were detected in each surveillance group. This may indicate earlier detection of cancers with A-MRI than interval cancers in the MG group. Because of the CDRs and minimal effect on anxiety in the MRI group we stopped the clinical trial early. Additionally, some patients could have developed breast cancer after the follow up period, which might have been missed with mammography. Given that the majority of patients were followed for over 24 months, this is less likely. Another limitation is that the radiologists were not blinded to the allocation arm, which could have influenced their reporting of the mammogram, if they knew that an MRI would be done. However, given similar recall rates for mammography within both groups, this is unlikely to have been present. The high biopsy rate in the MRI group may be perceived as a limitation, but this was related to the high CDR with an acceptable PPV3. In this study, all additional biopsies and follow-up imaging were fully covered by the publicly funded health care system, as per standard of care. However, more research is required to find ways to further reduce the rate of false positives. There is likely a learning curve with A-MRI and the addition of T2 sequences may help to improve PPV3 without significant time cost [16]. We have subsequently adapted an abbreviated protocol to include T2 sequence and two more post contrast sequences to improve the specificity of MRI [37]. This was a short-term trial and did not account for long-term follow-up for anxiety measures and other clinical outcomes with repeated breast imaging. For example, the false positive rate is often higher for the baseline screening breast MRI and specificity tends to increase with repeated breast imaging with a baseline for comparison. Another limitation is that assessment of anxiety was based on self-report questionnaires and limited by the time points in which it is measured. The study was powered to 134 patients per group to measure a clinically meaningful difference in anxiety and it is possible that the study was underpowered. There was also a loss of data of the primary outcome for participants over time, which could have led to underestimation of the effect of the surveillance group on levels of anxiety. A more objective measure would be to evaluate adherence to follow-up rounds of screening, which may address poor compliance with MRI screening [14]. This is recommended for future study. Also, our study lacked the sample size and enough long-term follow-up to be able to say whether the earlier detection in the A-MRI group led to any difference in survival. This trial was conducted at a single institution, tertiary care academic center with 2 breast radiologists reviewing all the breast imaging. Therefore, these trial results may not be generalizable to other clinical settings. The imaging surveillance tests in the study were usually done on the same day although in some (17% (18/104)), the studies were performed on different days with a large interval time between MG and A-MRI (average 33.2 days (range: 1–147). Among women at high-risk for breast cancer, annual mammograms and breast MRIs are often staggered every 6 months to try to reduce the incidence of interval cancers and would reflect clinical differences from our study.
In conclusion, the addition of A- MRI to surveillance mammography did not impact patient anxiety in women with PHBC, regardless of the significantly higher recall and biopsy rates. A-MRI showed significantly higher cancer detection rate compared to mammography alone, which is consistent with recent recommendations. Although further study with larger cohorts is warranted, an abbreviated protocol may be considered for surveillance in this population.
Availability of data and materials
The data will be deposited in the uOttawa—Dataverse (Université d’Ottawa / University of Ottawa): https://borealisdata.ca/ and data are available upon request.
Change history
23 September 2022
A Correction to this paper has been published: https://doi.org/10.1186/s12885-022-10108-2
Abbreviations
- A-MRI:
-
Abbreviated breast magnetic resonance imaging
- MG:
-
Mammography
- CDR:
-
Cancer detection rate
- DCIS :
-
Ductal carcinoma in situ
- IDC:
-
Invasive ductal carcinoma
- PHBC:
-
Prior (personal) history of breast cancer
- BI-RADS:
-
Breast Imaging-Reporting Data System
- CDR:
-
Cancer detection rate
- AIR:
-
Abnormal interpretation rate
- PPV:
-
Positive predictive value
References
Bredart A, Kop JL, Fall M, et al. Anxiety and specific distress in women at intermediate and high risk of breast cancer before and after surveillance by magnetic resonance imaging and mammography versus standard mammography. Psychooncology. 2012;21:1185–94.
Davies C, Godwin J, Gray R, et al. Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. Lancet. 2011;378:771–84.
Pedersen RN, Esen BO, Mellemkjaer L, et al. The Incidence of Breast Cancer Recurrence 10–32 Years After Primary Diagnosis. J Natl Cancer Inst. 2022;114:391–9.
Brewster AM, Hortobagyi GN, Broglio KR, et al. Residual risk of breast cancer recurrence 5 years after adjuvant therapy. J Natl Cancer Inst. 2008;100:1179–83.
Pan H, Gray R, Braybrooke J, et al. 20-Year Risks of Breast-Cancer Recurrence after Stopping Endocrine Therapy at 5 Years. N Engl J Med. 2017;377:1836–46.
Tabar L, Vitak B, Chen TH, et al. Swedish two-county trial: impact of mammographic screening on breast cancer mortality during 3 decades. Radiology. 2011;260:658–63.
Coldman A, Phillips N, Wilson C, et al. Pan-Canadian study of mammography screening and mortality from breast cancer. J Natl Cancer Inst. 2014;106(11):dju261.
Duffy SW, Tabar L, Chen HH, et al. The impact of organized mammography service screening on breast carcinoma mortality in seven Swedish counties. Cancer. 2002;95:458–69.
Lu WLJL, Post WJ, Bonnema J, Van de Velde JC, De Bock GH. Impact on survival of early detection of isolated breast recurrences after the primary treatment for breast cancer: a meta-analysis. Breast Cancer Res Treat. 2009;114(3):403–12.
Houssami NAL, Miglioretti DL, Sickles EA, Kerlikowske K, Buist DS, Geller BM, Muss HB, Irwig L. Accuracy and outcomes of screening mammography in women with a personal history of early-stage breast cancer. JAMA. 2011;305(8):790–9.
Houssami N, Ciatto S, Macaskill P, et al. Accuracy and surgical impact of magnetic resonance imaging in breast cancer staging: systematic review and meta-analysis in detection of multifocal and multicentric cancer. J Clin Oncol. 2008;26:3248–58.
Monticciolo DL, Newell MS, Moy L, Niell B, Monsees B, Sickles EA. Breast Cancer Screening in Women at Higher-Than-Average Risk: Recommendations From the ACR. J Am Coll Radiol. 2018;15:408–14.
Kuhl CK, Schrading S, Strobel K, Schild HH, Hilgers RD, Bieling HB. Abbreviated breast magnetic resonance imaging (MRI): first postcontrast subtracted images and maximum-intensity projection-a novel approach to breast cancer screening with MRI. J Clin Oncol. 2014;32:2304–10.
Do WSWJ, McGregor HF, Forte DM, Sheldon RR, Sohn VY. Poor compliance despite equal access: Military experience with screening breast MRI in high risk women. Am J Surg. 2019;217(5):843–7.
Mango VL, Morris EA, David Dershaw D, et al. Abbreviated protocol for breast MRI: are multiple sequences needed for cancer detection? Eur J Radiol. 2015;84:65–70.
Grimm LJ, Soo MS, Yoon S, Kim C, Ghate SV, Johnson KS. Abbreviated screening protocol for breast MRI: a feasibility study. Acad Radiol. 2015;22:1157–62.
Harvey SC, Di Carlo PA, Lee B, Obadina E, Sippo D, Mullen L. An Abbreviated Protocol for High-Risk Screening Breast MRI Saves Time and Resources. J Am Coll Radiol. 2016;13:374–80.
Heacock L, Melsaether AN, Heller SL, et al. Evaluation of a known breast cancer using an abbreviated breast MRI protocol: Correlation of imaging characteristics and pathology with lesion detection and conspicuity. Eur J Radiol. 2016;85:815–23.
Moschetta M, Telegrafo M, Rella L, Stabile Ianora AA, Angelelli G. Abbreviated Combined MR Protocol: A New Faster Strategy for Characterizing Breast Lesions. Clin Breast Cancer. 2016;16:207–11.
Rijnsburger AJ, Essink-Bot ML, van Dooren S, et al. Impact of screening for breast cancer in high-risk women on health-related quality of life. Br J Cancer. 2004;91:69–76.
Lee AJ, Cunningham AP, Kuchenbaecker KB, et al. BOADICEA breast cancer risk prediction model: updates to cancer incidences, tumour pathology and web interface. Br J Cancer. 2014;110:535–45.
D’Orsi CJ, Sickles EA, Mendelson EB, Morris EA, et al. ACR BI-RADS® Atlas, Breast Imaging Reporting and Data System. Reston, VA: American College of Radiology; 2013.
Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983.
Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behav Res Ther. 1990;28:487–95.
Lerman C, Trock B, Rimer BK, Jepson C, Brody D, Boyce A. Psychological side effects of breast cancer screening. Health Psychol. 1991;10:259–67.
Barry TL, Kaiser KL, Atwood JR. Reliability, validity, and scoring of the Health Status Questionnaire-12 version 20. J Nurs Meas. 2007;15:24–35.
Keyzer-Dekker CM, de Vries J, Mertens MC, Roukema JA, van der Steeg AF. Cancer or no cancer: the influence of trait anxiety and diagnosis on quality of life with breast cancer and benign disease: a prospective, longitudinal study. World J Surg. 2013;37:2140–7.
Millar K, Jelicic M, Bonke B, Asbury AJ. Assessment of preoperative anxiety: comparison of measures in patients awaiting surgery for breast cancer. Br J Anaesth. 1995;74:180–3.
Ontario Demographic Quarterly: Highlights of first quarter. Learn about key facts and figures of the province's demographics for the first quarter of 2021, Ontario government publications, Updated: September 22, 2021. Published: June 23, 2020, last accesssed July 3, 2022. https://www.ontario.ca/page/ontario-demographic-quarterly-highlights-first-quarter.
R.A L, Rubin GD. Statistical Analysis with Missing Data, Second Edition ed. Hoboken, New Jersey: Wiley Inc, 2002, in Wiley Series in Probability and Statistics.
Cuzick J, Sestak I, Pinder SE, et al. Effect of tamoxifen and radiotherapy in women with locally excised ductal carcinoma in situ: long-term results from the UK/ANZ DCIS trial. Lancet Oncol. 2011;12:21–9.
Darby S, McGale P, Correa C, et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet. 2011;378:1707–16.
Chen SQ, Huang M, Shen YY, Liu CL, Xu CX. Abbreviated MRI Protocols for Detecting Breast Cancer in Women with Dense Breasts. Korean J Radiol. 2017;18:470–5.
Choi BH, Choi N, Kim MY, Yang JH, Yoo YB, Jung HK. Usefulness of abbreviated breast MRI screening for women with a history of breast cancer surgery. Breast Cancer Res Treat. 2018;167:495–502.
Petrillo A, Fusco R, Sansone M, et al. Abbreviated breast dynamic contrast-enhanced MR imaging for lesion detection and characterization: the experience of an Italian oncologic center. Breast Cancer Res Treat. 2017;164:401–10.
Park KW, Han SB, Han BK, et al. MRI surveillance for women with a personal history of breast cancer: comparison between abbreviated and full diagnostic protocol. Br J Radiol. 2020;93:20190733.
Lukaszewicz A, Lamb L, Healey P, Alie E, Seely J. RC215-04 Breast Imaging and Interventional Abstract: Abbreviated Screening Breast MRI Protocol: Impact on Cancer Detection and Biopsy Rates. RSNA 2019 105th Scientific Assembly and Annual Meeting, Dec 1-6, McCormick Place, Chicago, USA. https://archive.rsna.org/2019/BreastImagingandInterventional.pd.
Acknowledgements
Not applicable.
Funding
Support for this study provided by The Ottawa Hospital Cancer Program to perform the Abbreviated MRI and cover the costs of the contrast injections (Cost no. 717602446). The funding body had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
JS, DK, TR and BS participated in the conception and design of the study, and in drafting the manuscript. MF, TA, JL, AA, RS, and YN participated in the conception and design of the study, and in revising the manuscript critically for important intellectual content. All authors read and approved the final manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Institutional Ethics Board “Ottawa Hospital Research Institute (REB approval number: 20140103-01H) with each participant providing informed written consent. All modifications in the protocol were transmitted to the Ethics Board.
Consent for publication
Not applicable.
Competing interests
The author(s) declare(s) that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author Note
This study has been presented previously at the European Congress of Radiology, in Clinical Trials of Radiology, July 2020.
The original version of this article was revised: The given name of Tasneem Alhassan has been corrected.
Supplementary Information
Additional file 1.
Questionnaires used in the study. Description of the questionnaires used in the study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fonseca, M.M., Alhassan, T., Nisha, Y. et al. Randomized trial of surveillance with abbreviated MRI in women with a personal history of breast cancer– impact on patient anxiety and cancer detection. BMC Cancer 22, 774 (2022). https://doi.org/10.1186/s12885-022-09792-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-022-09792-x