Abstract
Background
To assess the impact of PET/CT functional parameters on survival, locoregional, and distant failure according to the most distant level of lymph node [18F]FDG uptake in patients with locally advanced cervical cancer (LACC).
Methods
Retrospective study including 148 patients with LACC treated with concurrent chemoradiotherapy after PET/CT and para-aortic lymph node (PALN) surgical staging. Two senior nuclear medicine physicians reviewed all PET/CT exams and retrieved tumor and lymph node metabolic parameters: SUVmax, MTV, TLG. Oncological outcomes according to metabolic parameters and level of lymph node spread on PET/CT were assessed.
Results
In patients without lymph node uptake on PET/CT, high MTV values of the cervical tumor were associated with DFS (HR = 5.14 95%CI = [2.15–12.31]), OS (HR = 6.10 95%CI = [1.89–19.70]), and time to distant (HR = 4.73 95%CI = [1.55–14.44]) and locoregional recurrence (HR = 5.18 95%CI = [1.72–15.60]). In patients with pelvic lymph node (PLN) uptake but without PALN uptake on [18F]FDG-PET/CT, high MTV values of the cervical tumor were associated with DFS (HR = 3.17 95%CI = [1.02–9.83]) and OS (HR = 3.46 95%CI = [0.96–12.50]), and the number of PLN fixations was associated with DFS (HR = 1.30 95%CI = [1.10–1.53]), OS (HR = 1.35 95%CI = [1.11–1.64]), and time to distant (HR = 1.35 95%CI = [1.08–1.67]) and locoregional recurrence (HR = 1.31 95%CI = [1.08–1.59]). There was no significant association between cervical tumor metabolic or lymph node metrics and survival outcome in patients with PALN uptake.
Conclusions
Cervical MTV is more accurate than SUVmax to predict survival outcome in patients with locoregional disease confined to the pelvis and should be implemented in routine clinical practice. Prognostic value of metabolic metrics disappears with PALN uptake, which is associated with distant failure in nearly half of patients.
Graphical Abstract

Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Key points
-
Metabolic tumor volume of the cervical tumor is more accurate than SUVmax to predict survival outcome in patients with locoregional disease confined to the pelvis without paraaortic lymph node uptake.
-
Prognostic value of metabolic metrics disappears in patients with paraaortic lymph node uptake, which is associated with distant failure in nearly half of them.
Background
Cervical cancer is one of the most common malignant diseases worldwide and is one of the most common causes of death among women [1]. Although cervical cancer is often curable if detected early, more than one third of patients present a locally advanced cervical cancer (LACC) at diagnosis in developed countries [2]. Among several prognostic factors, lymph node status is the most important, and patients with extension up to the paraaortic area have a 3-year survival rate of approximately 30%. Most recurrences in these patients are distant failures [3, 4]. Assessment of lymph node involvement with different imaging modalities was evaluated in a meta-analysis including 41 studies [5]. Results showed a higher overall diagnostic performance of positron emission tomography/computed tomography (PET/CT) in a per-patient and a region or node-based analysis. Sensitivity was 82%, 50%, and 56%, and specificity was 95%, 90%, and 91% for PET/CT, computed tomography (CT), and magnetic resonance imaging (MRI), respectively [5].
In previous studies, our group and others demonstrated that tumor and lymph node metabolic parameters are able to predict treatment response and recurrence risk in patients treated with surgery or chemoradiotherapy (CRT) for cervical cancer [6,7,8,9]. Even if tumor metrics correlate with the presence of lymph node involvement [10,11,12,13], the prognostic value of tumor metabolic activity is probably dependent on locoregional extension, and on the level of lymph node metastases. There are some series addressing this question, but they are relatively old and include patients with early- and advanced-stage cervical cancer, and with variable degrees of lymph node extension. The magnitude to which PET/CT tumor and lymph node functional parameters influence patients’ outcome in relation to lymph node extension is unclear.
We studied the influence of metabolic parameters according to the level of lymph node spread on LACC, and on locoregional and metastatic progression.
Materials and methods
This retrospective study included patients with LACC (clinical FIGO stage 2009 IB2-IVA, except IIA1 without lymph node involvement) who received pre-therapeutic fluorodeoxyglucose [18F]FDG-PET/CT imaging at the French Referral Cancer Center from January 2006 through March 2015. The project was approved by the Institutional Review Board.
Preoperative work-up in all cases included physical examination, cervical biopsy, pelvic MRI, [18F]FDG-PET/CT, and laparoscopic paraaortic lymph node (PALN) retroperitoneal staging. Surgery began with a transperitoneal diagnostic laparoscopy to rule out occult carcinomatosis. A 10-mm port was inserted by open laparoscopy, and a 5-mm operative right lateral trocar was used to improve peritoneal evaluation. When peritoneal carcinomatosis was identified, the patient was excluded from the study and referred to palliative chemotherapy. If no anomaly was found, an extraperitoneal PALN dissection was performed through an extraperitoneal approach, as previously described [14]. During surgical staging, a frozen section was performed in cases of macroscopically suspicious lymph nodes. The surgical procedure was aborted if lymph node involvement was confirmed. Pelvic lymph nodes (PLN) were those situated in the pelvic region caudally to the common iliac bifurcation. PET/CT para-aortic lymph nodes included nodes from the bifurcation of the common iliac artery caudally to the left renal vein cranially. Para-aortic surgical dissection was performed using the same PET/CT anatomic limits, and included lympho-fatty tissue form the common iliac vessels, the aorta, aorto-caval space, and the vena cava.
Patients underwent pelvic with or without paraaortic external beam radiotherapy combined with chemotherapy. Radiotherapy was administered to the whole pelvic region in 25 fractions of 1.8 Gray (Gy) for a total dose of 45 Gy within 5 weeks. The paraaortic area also received 45 Gy in 25 fractions when PALN retroperitoneal staging was found to be positive. Concomitant chemotherapy with cisplatin 40 mg/m2 was administered weekly during radiotherapy for five courses. The treatment was then completed with additional pulse dose rate intracavitary brachytherapy for an equivalent total dose of 80–90 Gy. Before 2008, additional boosts up to an equivalent total dose of 65 Gy were sometimes given at the end of brachytherapy in the event of macroscopic lymph node and/or parametrial involvement. When Intensity-Modulated Radiation Therapy (IMRT) became available, a simultaneous integrated boost was performed on positive PLN at doses of 57.5 Gy in 25 fractions. PLN were considered positive when confirmed by pathology exam, or when there was a moderately to markedly deviation of the [18F]FDG uptake from the physiological distribution on pre-treatment PET/CT.
Follow-up included clinical examination of patients every four months for two years, and every six months for the following three years. Additional imaging was performed if clinically indicated using MRI for local evaluation and PET/CT for distant disease.
Exclusion criteria consisted of non-available images of [18F]FDG-PET/CT for double reading, distant metastasis at diagnosis, or peritoneal carcinomatosis found at laparoscopic examination of the abdominal cavity.
Medical data were extracted from computerized medical records and included demographics, clinical characteristics, imaging, surgical staging, histological findings, treatment and follow-up data, as well as recurrence and survival status at the end of the study.
[ 18 F]FDG-PET/CT modalities and review
Prior to any treatment, [18F]FDG-PET/CT was performed in the initial work-up according to the standardized institutional protocol. [18F]FDG-PET/CT whole-body images were obtained using a full-ring PET/CT scanner. Patients fasted for at least six hours before scanning. Blood glucose levels were checked before [18F]FDG injection, and injected dose and time between injection and acquisition were noted. If necessary, regarding bladder repletion and urinary activity, complementary pelvic acquisitions could be done after administering 20 mg of furosemide. PET data were reconstructed using an iterative, fully 3D algorithm with CT images for attenuation correction. A senior nuclear medicine physician expert in gynecologic cancer analyzed all [18F]FDG-PET/CT images in standard clinical fashion. All patients had a double-blinded review of metabolic parameters performed by another senior nuclear medicine specialist. Segmentation of cervical tumor volumes and PLN was done using General Electric AW server 3.0 software with an automatic thresholding at 40% of maximum standardized uptake value (SUVmax), following European Association of Nuclear Medicine (EANM) guidelines [15]. Manual correction was used in a few cases to exclude urinary tract activity, mostly in patients who had not received furosemide and whose bladder activity was equal or superior to tumor uptake. This was also the case when the AW Server automatic thresholding process was not suitable. For this modification, we used CT scan and visual uptake differences between tumor and urinary activity. Other tumor contours were not modified. Lymph nodes were considered as involved if they showed any uptake superior to background activity. The metabolic parameters studied for primary cervical tumor and/or for PLN when positive were as follows: SUVmax, mean standardized uptake value (SUVmean), metabolic tumor volume (MTV), total lesion glycolysis (TLG), and number of PLN fixations. The size of PLN was measured on CT imaging. The MTV and TLG of PLN used in our study were measured from the most [18F]FDG avid lesion, allowing for quick assessment by means of a procedure that can be used in daily clinical practice. A high MTV value was defined as a value above the median MTV of the whole cohort.
Statistical analysis
Qualitative variables were described by frequencies and percentages and compared using the Chi-squared or Fisher’s exact test. Continuous variables were summarized by median and range (min–max) and compared using the Kruskal–Wallis test. All survival times were calculated from the initiation of CRT and were estimated by the Kaplan–Meier method with 95% confidence intervals (CI), using the following definitions of first event: loco-regional relapse for time to loco-regional relapse, metastatic relapse for time to distant metastasis, relapse or death for disease-free survival (DFS) and death for overall survival (OS). Patients who did not experience the event of interest were censored at their last follow-up. Univariate analyses were performed using the Cox proportional hazard model for continuous variables and the Log-rank test for qualitative variables. Hazard Ratios (HR) with their 95% CI based on the Cox proportional hazards model were calculated for each variable. All statistical tests were two-sided and a p-value < 0.05 was considered statistically significant. Statistical analyses were performed using the STATA software version 16 (StataCorp LLC, College Station, TX).
Results
During the study period, 148 patients met the inclusion criteria. Clinical characteristics are presented in Table 1. Among the 148 patients, [18F]FDG-PET/CT showed no lymph node involvement in 71, 45 had exclusive PLN involvement on [18F]FDG-PET/CT, and there was PALN involvement with or without PLN involvement in 32. PALN dissection was performed in 133 patients and 15 were considered metastatic on the PALN based on pretreatment PET/CT results. The median number of PALN removed was 18 (range 5–48). One patient had macroscopic lymph node involvement confirmed by frozen section, so PALN dissection was aborted. The proportion of patients without PALN uptake on [18F]FDG-PET/CT and with pathology-proven lymph node involvement after surgical staging (false-negative rate) was 4.2% (3/71) in patients without PLN [18F]FDG-PET/CT uptake, and 24.4% (11/45) in patients with PLN [18F]FDG-PET/CT uptake. In total, 46 patients had PALN involvement: 3 in the negative FDG-PET/CT group, 11 in the positive PLN but negative PALN [18F]FDG-PET/CT group, and 32 in the positive PALN [18F]FDG-PET/CT group (15 only on imaging and 17 confirmed on PALN dissection). Among the 3 patients with negative PLN and positive PALN, one presented with micro-metastasis and the other two had macro-metastases. Among the remaining 28 patients with positive PALN confirmed histologically (11 patients with positive PLN but negative PALN [18F]FDG-PET/CT and 17 with positive PALN [18F]FDG-PET/CT), all had macro-metastases. Clinical characteristics, histological subtype, and clinical FIGO stage were similar between patients with and without PALN involvement.
Metabolic parameters of cervical tumor and pelvic lymph nodes
Median values of cervical tumor SUVmax, MTV and TLG for the overall cohort were 14.8 (range 2.1–46.3), 39.2 cc (range 0.8–299.0) and 263.0 g/mL*cm3 (range 1.2–3181.0), respectively. Median values of cervical tumor SUVmax, MTV and TLG in patients without lymph node involvement on [18F]FDG-PET/CT were significantly lower than in patients with positive lymph nodes on [18F]FDG-PET/CT. Seventy-two patients had abnormal PLN uptake: 27 (37.5%) with positive PALN and 45 (62.5%) with negative PALN. Cervical tumor and PLN metabolic parameters according to lymph node status on PET/CT are displayed in Table 2.
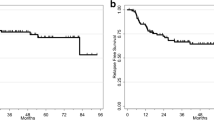
After a median follow-up of 39.3 months (95% CI 33.4–47.9), 42 patients (28.4%) died from the disease. During the study period, 55 patients (37.2%) recurred: 18 (32.7%) had a locoregional recurrence, 20 (36.4%) had distant metastases and 17 (30.9%) patients presented with both locoregional and distant disease. The 2- and 5-year OS rates were 80.2% (95% CI 72.0–86.2) and 59.8% (95% CI 48.4–69.5) respectively. Figure 1 shows Kaplan–Meier OS and DFS estimated curves according to lymph node spread on [18F]FDG-PET/CT and MTV values of cervical tumor.
In univariate analysis, FIGO stage IIB-IVA, pretherapeutic tumor size measured by MRI, tumor SUVmax, MTV of cervical tumor, PLN SUVmax, and the number of PLN with uptake at [18F]FDG-PET/CT were significantly associated with decreased DFS and OS (Table 3). In multivariate analysis, the only metabolic parameter that remained significantly associated with DFS in the whole cohort was the number of [18F]FDG-PET/CT PLN abnormal uptake. MTV of the cervical tumor and the number of PLN fixations were the only two metabolic parameters which remained significantly associated with OS.
In the group of patients with no lymph node involvement on [18F]FDG-PET/CT, 15 patients (21.1%, 15/71) and 14 patients (19.7%, 14/71) had loco-regional and distant failures, respectively, compared to 9 loco-regional (28.1%, 9/32) and 14 distant failures (43.8%, 14/32) in patients with PALN involvement.
To evaluate the influence of metabolic parameters on survival and on locoregional and distant recurrence, we grouped patients by [18F]FDG uptake on the most distant level of lymph node activity. MTV and high MTV values of the cervical tumor were significantly associated with the risk of recurrence in patients without lymph node involvement on [18F]FDG-PET/CT. In patients with PLN uptake and without PALN uptake, tumor SUVmax, MTV, high MTV values, tumor size, number of PLN with uptake, PLN SUV mean and SUVmax were significantly associated with the risk of recurrence. No significant association was found between tumor or lymph node metabolic parameters and DFS in patients with PALN uptake with or without PLN uptake. The risk of death was significantly associated with tumor SUVmax and high MTV values in patients without lymph node involvement on [18F]FDG-PET/CT. Tumor SUVmax, MTV, high MTV values, number of PLN with uptake, PLN SUVmean and SUVmax were significantly associated with the risk of recurrence in patients with PLN uptake but without PALN uptake. No significant association between tumor metabolic or lymph node metrics and OS was found in patients with PALN uptake with or without PLN uptake (Table 4).
HR for time to distant metastasis in patients without lymph node metastasis on [18F]FDG-PET/CT was 4.73 (CI 95% [1.55–14.44] p = 0.003) for high MTV values of the cervical tumor. HR for time to distant metastasis in patients with PLN uptake and without PALN uptake were 1.35 (CI 95% [1.08–1.67] p = 0.007) for the number of PLN with uptake and 1.97 (CI 95% [0.49–7.97] p = 0.334) for high MTV values of the cervical tumor. Tumor SUVmax was significantly associated with time to loco-regional relapse in the overall cohort (HR 1.05 CI 95% [1.00–1.10] p = 0.049), but not in subgroup analysis. High MTV values of the cervical tumor also correlated with time to locoregional relapse in [18F]FDG-PET/CT node-negative patients (HR 5.18 [1.72–15.60] p = 0.001, but not in [18F]FDG-PET/CT node-positive patients. The number of PLN with uptake was associated with time to locoregional relapse in patients with PLN uptake but without PALN uptake (HR 1.31 CI 95% [1.08–1.59] p = 0.007). No significant association between tumor metabolic or lymph node metrics and time to distant or locoregional metastasis was found in patients with PALN uptake.
Discussion
PET/CT provides non-invasive information on what to expect from disease evolution according to the pattern of metabolic locoregional uptake (Fig. 2). We studied the extent to which tumor and lymph node metabolic activity determines recurrence risk. As demonstrated in previous series [10,11,12,13], higher tumor metabolic uptake was found in patients with lymph node involvement. The HR for disease recurrence, distant failure and death were significantly increased in patients with high MTV of the cervical tumor and in patients with a higher number of PLN fixations. Metabolic parameters did not predict prognostic outcome in patients with PALN metastasis. The prognostic value of PET/CT tumor and lymph node metabolic activity disappeared with PALN positivity, which was associated with distant failure in nearly half of patients.
PET images of a patient presenting with a cervical tumor with left pelvic lymph node involvement. a) cervical tumor contouring with semi-automatic tumor thresholding method at 40% of the SUVmax (SUVmax 22.8; TLG 372.9 g/ml*cm3; MTV 37.16 cm3); b) the same procedure with a left pelvic involved lymph node with SUVmax 7.9; TLG 8.7 g/ml*cm3; MTV 1.65 cm3; c) Maximum intensity projection showing the absence of distant metastasis
High tumor metabolic activity has been correlated with poor prognostic factors such as high grade, poorly differentiated histology, depth of invasion, tumor size and lymph node involvement [6, 8, 10, 12, 16, 17]. In patients without lymph node spread, both SUVmax and MTV of the cervical tumor were correlated with shorter survival, but only high MTV values of the cervical tumor were associated with distant failure in our series. The prognostic value of tumor [18F]FDG uptake within tumor sites on pretreatment PET/CT has been shown in several reports [11, 18]. A recent meta-analysis demonstrated that patients with high tumor or lymph node SUVmax are at higher risk of adverse events or death [19]. In a previous study by our group, we showed that cervical metabolic activity was the main predictive factor of OS in patients with no para-aortic extension [6]. In the present series, our results also show an association between high SUVmax and locoregional recurrence risk in the overall cohort. Among metabolic parameters, high MTV of the primary tumor significantly increased the risk of locoregional, distant failure, and death. Volume-based metabolic parameters were associated with outcome after CRT in several studies [20,21,22]. Our results confirm those from a recent meta-analysis comprising 660 patients from 12 studies, which showed an increased risk of recurrence and death in patients with high values of MTV and TLG [22]. All except one of the studies included showed a survival effect of volumetric parameters in multivariate analysis, including additional prognostic, clinical and PET/CT parameters [22]. The authors suggested that cervical intratumor heterogeneity is associated with the underlying tumor biology, such as variable hypoxia, cellular proliferation, and blood flow, resulting in varying levels of [18F]FDG avidity. A correlation between volume-based parameters and both size and uptake distribution within the tumor was also found [23].
The method of measuring MTV varies across studies and a wide range of different MTV prognostic cut-off values have been reported [20]. Miller et al. reported shorter DFS and OS in node-negative patients with MTV ≥ 60 cm3 treated with CRT [20]. Chung et al. found that preoperative MTV ≥ 23.4 ml was an independent factor for DFS in multivariate analysis in patients treated with radical surgery [24]. Sun et al. also reported that MTV values above 53.75 ml were an independent factor for OS [25]. Other series failed to demonstrate a significant prognostic value of metabolic parameters when compared to other clinical prognostic factors such as tumor size or lymph node involvement in multivariate analysis [26]. Even if there are several prognostic MTV cut-off values and various methods for estimating and interpreting MTV, high MTV values have more impact on survival than SUVmax [27].
According to data provided by several series, high lymph node metabolic activity portends an increased risk of recurrence and death in patients with LACC treated with CRT [8, 28]. Kidd et al. showed in a prospective study that the risk of pelvic recurrence is significantly related to high PLN SUVmax but not to cervical tumor SUVmax, although their study also included higher levels of lymph node spread [8]. Nakamura et al. also found that high PLN SUVmax were associated with decreased DFS and OS in patients treated with CRT for cervical cancer with locoregional spread confined to the pelvis [29]. Another series provided evidence for the independent predictive value of the ratio [PLN SUVmax]/[cervical tumor SUVmax] for the risk of recurrence in the multivariate analysis of patients with pelvic and/or para-aortic extension [30]. Our results also showed a significant association between PLN SUV mean and survival in patients with no para-aortic extension on PET/CT. However, multivariate analysis showed that only MTV of the cervical tumor and the number of PLN with uptake remained as significant predictors of survival.
Our results are consistent with other studies that found MTV of the cervical tumor and PALN metastases to be the best predictors of OS [31]. The prognostic value of metabolic metrics disappeared in the presence of PALN involvement. Furthermore, PALN uptake avidity was not associated with prognostic outcome, as PALN involvement was itself more predictive of distant failure and death than any metabolic parameter of the tumor or lymph node. In contrast with our results, an association between OS and para-aortic SUV and TLG values was reported in a retrospective study including 68 patients with PALN extension [32]. Another study identified an SUVmax threshold above 3.3 of the PALN as a significant factor for OS [33]. PALN metastasis is a major outcome determinant, with decreased 5-year OS at approximately 30%, and a majority of patients with distant recurrent disease. Information on PALN status enables treatment intensification by extension of the radiotherapy field and the optional addition of adjuvant chemotherapy. In our series, we only found 3 patients (4.2%) with isolated PALN involvement, which is lower than other reports of patients with no PLN extension [12, 34, 35].
This and other studies indicate that MTV of the cervical tumor and the number of PLN fixations are independent factors for OS. However, to date, few studies have addressed the recurrence risk of functional PET/CT parameters according to the level of lymph node disease in LACC prior to CRT. High MTV values of the cervical tumor were associated with decreased DFS and OS in patients with disease confined to the pelvic region. They were also related to time to distant and locoregional recurrence in PET/CT lymph node-negative patients. Even if SUVmax has been widely and systematically used to define cervical tumor metabolic activity, MTV is more accurate to estimate relapse risk. Pretreatment PET/CT should include MTV measurement in routine practice in PALN-negative patients in order to tailor follow-up and intensify treatment modalities or favor inclusion in clinical trials for patients with high MTV values.
The main limitation of the study is its retrospective design, which could have induced a selection bias in the patient population. Additionally, dose levels and radiotherapy techniques have evolved during the last years and can influenced survival results. The long inclusion period can explain the lower survival rates than those reported in the EMBRACE studies [36]. This is the first study to estimate specifically cervical tumor and lymph node metabolic parameters to define the risk of distant failure depending on the pattern of retroperitoneal lymph node metastasis. A major strength of the study is lymph node surgical staging of all patients included in this series. To increase the reproducibility of metabolic parameter measurements, to facilitate their use in daily practice and to limit inter-observer variability, dedicated artificial intelligence thresholding software could prove valuable in the future.
In conclusion, MTV of the cervical tumor and number of PLN fixations were the best predictors of survival. MTV correlated with locoregional and distant failure in patients with LACC without lymph node involvement and the number of PLN fixations was associated with locoregional and distant failure in patients without PALN extension. The prognostic value of metabolic metrics disappeared with PALN positivity, which was associated with distant failure in nearly half of patients. Our results and previous studies demonstrate that MTV of the cervical tumor is a more accurate parameter than SUVmax to predict survival outcome and should be implemented in routine practice.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- LACC:
-
Locally Advanced Cervical Cancer
- PET/CT:
-
Positron Emission Tomography/computed Tomography
- CT:
-
Computed Tomography
- MRI:
-
Magnetic Resonance Imaging
- CRT:
-
Chemoradiotherapy
- [18F]FDG-PET/CT:
-
Fluorodeoxyglucose-PET/CT
- PALN:
-
Paraaortic lymph node
- Gy:
-
Gray
- IMRT:
-
Intensity-Modulated Radiation Therapy
- PLN:
-
Pelvic Lymph Node
- SUVmax:
-
Maximum Standardized Uptake Value
- EANM:
-
European Association of Nuclear Medicine
- SUVmean:
-
Mean Standardized Uptake Value
- MTV:
-
Metabolic Tumor Volume
- TLG:
-
Total Lesion Glycolysis
- CI:
-
Confidence Interval
- DFS:
-
Disease-Free Survival
- OS:
-
Overall Survival
- HR:
-
Hazard Ratio
References
Global Cancer Observatory, OMS. Estimated number of incident cases, worldwide ( top 10 cancer sites ) in 2012. Disponible sur http://gco.iarc.fr/today/online-analysis-multi-bars?mode=cancer&mode_population=continents&population=900&sex=2&cancer=16&type=0&statistic=0&prevalence=0&color_palette=default. 2017. p. 2012.
Quinn M a, Benedet JL, Odicino F, Maisonneuve P, Beller U, Creasman WT, et al. Carcinoma of the cervix uteri. FIGO 26th Annual Report on the Results of Treatment in Gynecological Cancer. Int J Gynaecol Obstet. 2006;95(Suppl 1):S43-103.
Manders DB, Sims TT, Bailey A, Hwang L, Richardson DL, Miller DS, et al. The Significance of Para-Aortic Nodal Size and the Role of Adjuvant Systemic Chemotherapy in Cervical Cancer. Am J Clin Oncol. 2018;41(12):1225–30.
Querleu D, Dargent D, Ansquer Y, Leblanc E, Narducci F. Extraperitoneal endosurgical aortic and common iliac dissection in the staging of bulky or advanced cervical carcinomas. Cancer. 2000;88(8):1883–91.
Choi HJ, Ju W, Myung SK, Kim Y. Diagnostic performance of computer tomography, magnetic resonance imaging, and positron emission tomography or positron emission tomography/computer tomography for detection of metastatic lymph nodes in patients with cervical cancer: Meta-analysis. Cancer Sci. 2010;101(6):1471–9. https://doi.org/10.1111/j.1349-7006.2010.01532.x.
Voglimacci M, Gabiache E, Lusque A, Ferron G, Ducassou A, Querleu D, et al. Chemoradiotherapy for locally advanced cervix cancer without aortic lymph node involvement: can we consider metabolic parameters of pretherapeutic FDG-PET/CT for treatment tailoring? Eur J Nucl Med Mol Imaging. 2019;46(7):1551–9. https://doi.org/10.1007/s00259-018-4219-5.
Khiewvan B, Atorigian D, Emamzadehfard S, Paydary K, Salavati A, Houshmand S, et al. Update of the role of PET/CT and PET/MRI in the management of patients with cervical cancer. Hell J Nucl Med. 2016;19(3):254–68.
Kidd EA, Siegel BA, Dehdashti F, Grigsby PW. Pelvic lymph node F-18 fluorodeoxyglucose uptake as a prognostic biomarker in newly diagnosed patients with locally advanced cervical cancer. Cancer. 2010;116(6):1469–75. https://doi.org/10.1002/cncr.24972.
Woo S, Atun R, Ward ZJ, Scott AM, Hricak H, Vargas HA. Diagnostic performance of conventional and advanced imaging modalities for assessing newly diagnosed cervical cancer: systematic review and meta-analysis. Eur Radiol. 2020;30(10):5560–77. Available from: http://www.ncbi.nlm.nih.gov/pubmed/32415584.
Nakamura K, Okumura Y, Kodama J, Hongo A, Kanazawa S, Hiramatsu Y. The predictive value of measurement of SUVmax and SCC-antigen in patients with pretreatment of primary squamous cell carcinoma of cervix. Gynecol Oncol. 2010;119(1):81–6. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0090825810003525.
Kidd EA, Siegel BA, Dehdashti F, Grigsby PW. The standardized uptake value for F-18 fluorodeoxyglucose is a sensitive predictive biomarker for cervical cancer treatment response and survival. Cancer. 2007;110(8):1738–44. https://doi.org/10.1002/cncr.22974.
Martinez A, Voglimacci M, Lusque A, Ducassou A, Gladieff L, Dupuis N, et al. Tumour and pelvic lymph node metabolic activity on FDG-PET/CT to stratify patients for para-aortic surgical staging in locally advanced cervical cancer. Eur J Nucl Med Mol Imaging. 2020. https://doi.org/10.1007/s00259-019-04659-z
Yilmaz M, Adli M, Celen Z, Zincirkeser S, Dirier A. FDG PET-CT in cervical cancer: Relationship between primary tumor FDG uptake and metastatic potential. Nucl Med Commun. 2010;31(6):526–31.
Sonoda Y, Leblanc E, Querleu D, Castelain B, Papageorgiou T, Lambaudie E, et al. Prospective evaluation of surgical staging of advanced cervical cancer via a laparoscopic extraperitoneal approach. Gynecol Oncol. 2003;91(2):326–31.
Boellaard R, Delgado-Bolton R, Oyen WJG, Giammarile F, Tatsch K, Eschner W, et al. FDG PET / CT : EANM procedure guidelines for tumour imaging : version 2.0. Eur J Nucl Med Mol Imaging. 2015;42:328–54.
Netzer I, Sobeh S, Keidar Z, Lowenstein L, Lavie O, Yosef R Ben, et al. To operate or to radiate: the added value of the maximal standardized uptake value in PET–FDG in cervical cancer patients. Med Oncol. 2013;30(2):558. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23549865.
Kidd EA, Spencer CR, Huettner PC, Siegel BA, Dehdashti F, Rader JS, et al. Cervical cancer histology and tumor differentiation affect 18 F-fluorodeoxyglucose uptake. Cancer. 2009;115(15):3548–54. https://doi.org/10.1002/cncr.24400.
Onal C, Reyhan M, Parlak C, Guler OC, Oymak E. Prognostic Value of Pretreatment F-18-fluorodeoxyglucose Uptake in Patients With Cervical Cancer Treated With Definitive Chemoradiotherapy. Int J Gynecol Cancer. 2013;23(6):1104–10.
Sarker A, Im H-J, Cheon GJ, Chung HH, Kang KW, Chung J-K, Kim EE, Lee DS. Prognostic Implications of the SUVmax of Primary Tumors and Metastatic Lymph Node Measured by 18F-FDG PET in Patients With Uterine Cervical Cancer. Clin Nucl Med. 2016;41:34–40. https://doi.org/10.1097/RLU.0000000000001049.
Miller TR, Grigsby PW. Measurement of tumor volume by PET to evaluate prognosis in patients with advanced cervical cancer treated by radiation therapy. Int J Radiat Oncol. 2002;53(2):353–9. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0360301602027050.
Chong GO, Lee WK, Jeong SY, Park S-H, Lee YH, Lee S-W, et al. Prognostic value of intratumoral metabolic heterogeneity on F-18 fluorodeoxyglucose positron emission tomography/computed tomography in locally advanced cervical cancer patients treated with concurrent chemoradiotherapy. Oncotarget. 2017;8(52):90402–12. https://doi.org/10.18632/oncotarget.18769.
Han S, Kim H, Kim YJ, Suh CH, Woo S. Prognostic Value of Volume-Based Metabolic Parameters of 18 F-FDG PET/CT in Uterine Cervical Cancer: A Systematic Review and Meta-Analysis. Am J Roentgenol. 2018;211(5):1112–21. https://doi.org/10.2214/AJR.18.19734.
Chong GO, Lee WK, Jeong SY, Park S-H, Lee YH, Lee S-W, et al. Prognostic value of intratumoral metabolic heterogeneity on F-18 fluorodeoxyglucose positron emission tomography/computed tomography in locally advanced cervical cancer patients treated with concurrent chemoradiotherapy. Oncotarget. 2017;8(52):90402–12.
Chung HH, Kwon HW, Kang KW, Park N, Song Y-S, Chung J, et al. Prognostic Value of Preoperative Metabolic Tumor Volume and Total Lesion Glycolysis in Patients with Epithelial Ovarian Cancer. Ann Surg Oncol. 2012;19:1966–72.
Sun Y, Lu P, Yu L. The Volume-metabolic Combined Parameters from 18F-FDG PET/CT May Help Predict the Outcomes of Cervical Carcinoma. Acad Radiol. 2016;23(5):605–10. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1076633216000234.
Guler OC, Torun N, Yýldýrým BA, Onal C. Pretreatment metabolic tumor volume and total lesion glycolysis are not independent prognosticators for locally advanced cervical cancer patients treated with chemoradiotherapy. Br J Radiol. 2018;20170552. https://doi.org/10.1259/bjr.20170552
Han S, Kim H, Kim YJ, Suh CH, Woo S. Prognostic value of volume-based metabolic parameters of 18F-FDG PET/CT in ovarian cancer: a systematic review and meta-analysis. Ann Nucl Med. 2018;32(10):669–77.
Vergote I, Tsolakidis D, Mortier D, Neven P, Amant F, Mottaghy F, et al. Value of Positron Emission Tomography of the Para-Aortic Lymph Nodes in Cervical Carcinoma Stage IB2-IIIB. J Clin Oncol. 2008;26(34):5654–5. https://doi.org/10.1200/JCO.2008.19.5883.
Nakamura K, Joja I, Nagasaka T, Haruma T, Hiramatsu Y. Maximum standardized lymph node uptake value could be an important predictor of recurrence and survival in patients with cervical cancer. Eur J Obstet Gynecol Reprod Biol. 2014;173:77–82. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0301211513005526.
Chung HH, Cheon GJ, Kim J-W, Park N-H, Song YS. Prognostic importance of lymph node-to-primary tumor standardized uptake value ratio in invasive squamous cell carcinoma of uterine cervix. Eur J Nucl Med Mol Imaging. 2017;44(11):1862–9.
Son SH, Jeong SY, Chong GO, Lee YH, Park S-H, Lee C-H, et al. Prognostic Value of Pretreatment Metabolic PET Parameters in Cervical Cancer Patients With Metabolic Complete Response After Concurrent Chemoradiotherapy. Clin Nucl Med. 2018;43(9):e296-303. Available from: http://jnm.snmjournals.org/lookup/doi/10.2967/jnumed.119.238824.
Leray H, Gabiache E, Courbon F, Brenot-Rossi I, Colineaux H, Lepage B, et al. FDG-PET/CT identifies predictors of survival in patients with locally advanced cervical carcinoma and para-aortic lymph node involvement to increase treatment. J Nucl Med [Internet]. 2020;jnumed.119.238824. https://doi.org/10.2967/jnumed.119.238824
Yen T-C, See L-C, Lai C-H, Tsai C-S, Chao A, Hsueh S, et al. Standardized uptake value in para-aortic lymph nodes is a significant prognostic factor in patients with primary advanced squamous cervical cancer. Eur J Nucl Med Mol Imaging. 2008;35(3):493–501. Available from: http://link.springer.com/10.1007/s00259-007-0612-1.
Gouy S, Morice P, Narducci F, Uzan C, Gilmore J, Kolesnikov-Gauthier H, et al. Nodal-staging surgery for locally advanced cervical cancer in the era of PET. Lancet Oncol. 2012;13(5):e212–20. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1470204512700116.
Leblanc E, Gauthier H, Querleu D, Ferron G, Zerdoud S, Morice P, et al. Accuracy of 18-Fluoro-2-deoxy-d-glucose Positron Emission Tomography in the Pretherapeutic Detection of Occult Para-aortic Node Involvement in Patients with a Locally Advanced Cervical Carcinoma. Ann Surg Oncol. 2011;18(8):2302–9. Available from: http://link.springer.com/10.1245/s10434-011-1583-9.
Pötter R, Tanderup K, Kirisits C, de Leeuw A, Kirchheiner K, Nout R, et al. The EMBRACE II study: The outcome and prospect of two decades of evolution within the GEC-ESTRO GYN working group and the EMBRACE studies. Clin Transl Radiat Oncol. 2018;9:48–60. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2405630817300757.
Acknowledgements
Not Applicable.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Contributions
All the authors included in this article adequately contributed to the production of this manuscript: AM, EC, MAA, GF, AD, MD, JA, SB, AL, EG. All authors contributed to the study conception and design: AM, EC, MAA, GF, AD, MD, JA, SB, AL, EG. Material preparation, data collection and analysis were performed by MAA, AD, MD, JA, SB and EG. Statistical analysis was done by AL. The first draft of the manuscript was written by AM, MAA and EG and all authors (AM, EC, MAA, GF, AD, MD, JA, SB, AL, EG) commented on previous versions of the manuscript. All authors read and approved the final manuscript: AM, EC, MAA, GF, AD, MD, JA, SB, AL, EG.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Board (Comité d'Éthique IUCT-O, Reference: CRE IUCT-O : 2-22-01).
Due to the retrospective nature of our study, written informed consent was waived by the Institutional Review Board (Comité d'Éthique IUCT-O, Reference: CRE IUCT O : 2-22-01).
Consent for publication
Not applicable.
Competing interests
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Martinez, A., Chantalat, E., Angeles, M.A. et al. Metabolic activity determines survival depending on the level of lymph node involvement in cervical cancer. BMC Cancer 22, 810 (2022). https://doi.org/10.1186/s12885-022-09785-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-022-09785-w