Abstract
Background
Salvage external beam radiotherapy (sEBRT) for patients with a biochemical recurrence (BCR) after radical prostatectomy provides a 5-year biochemical progression-free survival up to 60%. Multiple studies have shown that dose escalation to the primary prostate tumour improves treatment outcome. However, data is lacking on the role of dose escalation in the recurrent salvage setting. The main objective of the PERYTON-trial is to investigate whether treatment outcome of sEBRT for patients with a BCR after prostatectomy can be improved by increasing the biological effective radiation dose using hypofractionation. Moreover, patients will be staged using the PSMA PET/CT scan, which is superior to conventional imaging modalities in detecting oligometastases.
Methods
The PERYTON-study is a prospective multicentre open phase III randomised controlled trial. We aim to include 538 participants (269 participants per treatment arm) with a BCR after prostatectomy, a PSA-value of < 1.0 ng/mL and a recent negative PSMA PET/CT scan. Participants will be randomised in a 1:1 ratio between the conventional fractionated treatment arm (35 × 2 Gy) and the experimental hypofractionated treatment arm (20 × 3 Gy). The primary endpoint is the 5-year progression-free survival after treatment. The secondary endpoints include toxicity, quality of life and disease specific survival.
Discussion
Firstly, the high rate of BCR after sEBRT may be due to the presence of oligometastases, for which local sEBRT is inappropriate. With the use of the PSMA PET/CT before sEBRT, patients with oligometastases will be excluded from intensive local treatment to avoid unnecessary toxicity. Secondly, the currently applied radiation dose for sEBRT may be too low to achieve adequate local control, which may offer opportunity to enhance treatment outcome of sEBRT by increasing the biologically effective radiotherapy dose to the prostate bed.
Trial registration
This study is registered at ClinicalTrials.gov (Identifier: NCT04642027). Registered on 24 November 2020 – Retrospectively registered. The study protocol was approved by the accredited Medical Ethical Committee (METc) of all participating hospitals (date METc review: 23-06-2020, METc registration number: 202000239). Written informed consent will be obtained from all participants.
Highlights
• This is the first PSMA PET/CT based study addressing the role of hypofractionation in salvage external beam radiation therapy (sEBRT);
• Participants will be randomised 1:1 to conventional fractionated sEBRT (35 × 2 Gy) or hypofractionated sEBRT (20 × 3 Gy);
• The PSMA PET/CT-scan will be used for staging of all participants at baseline;
• The primary endpoint is 5-year progression-free survival after treatment;
• All participants will receive early sEBRT (PSA < 1.0 ng/mL) without the use of androgen deprivation therapy;
• A quality assurance program was undertaken, to ensure protocol compliance within the PERYTON-trial;
• An interim analysis will be performed after the inclusion of 25% (n = 135) of the total number of required participants, to identify any early signs of excessive (unexpected) acute toxicity.
Similar content being viewed by others
Background
According to the Dutch Cancer Registry, prostate cancer (PCa) is the first most diagnosed cancer in men with 12.800 new cases and 2.954 deaths in 2018 in the Netherlands [1]. Radical prostatectomy (RP) as primary treatment provides excellent control in localized PCa. After RP, however, approximately 20-40% of patients will develop a biochemical recurrence (BCR) within 5 years. The site of relapse is predominately local (35 to 54%) [2,3,4]. The only curative treatment option for BCR after RP is salvage external beam radiation therapy (sEBRT). However, 40-50% of the patients treated with sEBRT develop a secondary BCR [5]. This relatively high percentage of a secondary BCR after sEBRT necessitates the need to improve the treatment outcome of sEBRT and subsequently to reduce the need for more aggressive palliative treatment strategies.
Since the introduction of the prostate-specific membrane antigen (PSMA) positron emission tomography (PET)/computed tomography (CT) scan, the detection of oligometastases at very low prostate specific antigen (PSA) levels has significantly improved [6]. PSMA PET/CT can detect nodal metastases as small as 2.4 mm with up to 80% sensitivity and 97% specificity [7]. Recent studies have demonstrated significant changes (30 to 76%) in management decisions for recurrent PCa by incorporating PSMA-PET/CT in an early stage of BCR after RP [6, 7].
Firstly, the high rate of BCR after sEBRT may be due to the presence of oligometastases, for which local sEBRT is inappropriate. With the use of the PSMA PET/CT before commencing sEBRT, patients with oligometastases will be excluded from intensive local treatment to avoid unnecessary toxicity [7,8,9,10]. Furthermore, the absence of active disease on PSMA PET/CT scans is an independent prognostic factor for high response to sEBRT [11]. These findings support applying sEBRT in patients with BCR without evidence of distant metastasis on PSMA-PET/CT scan in whom local recurrence in the prostate bed cannot be detected.
Secondly, the currently applied conventional radiation schedule for local sEBRT may be insufficient. This may offer opportunities to improve biochemical progression-free survival (bPFS) by increasing the biologically effective radiotherapy dose to the prostate bed using hypofractionation. Studies have shown that the α/β-ratio for PCa cells is 1.5 Gy, which is lower than that of surrounding normal tissues [12]. This means that PCa cells are more sensitive to fraction dose than surrounding tissues, which is the rationale for increasing the dose-per-fraction (hypofractionation) instead of the total dose. In doing so, the biological dose to the tumour cells, but not to the surrounding normal tissues (bladder and rectum), is expected to increase. Assuming an α/β of 4 Gy for bladder and rectum, the equivalent dose at 2 Gy (EQD2) of the hypofractionated schedule of 20 × 3 Gy is 70 Gy, which is equal to the 70 Gy in the standard arm [12].
In primary PCa, multiple randomised controlled trials (RCT) have shown non-inferiority of a 20 × 3.0 Gy = 60 Gy schedule over 39 × 2.0 Gy = 78 Gy, confirming its biological equivalence of both schedules regarding oncologic outcome and toxicity [13, 14]. Based on these results, we expect the experimental study regimen (20 × 3 Gy) will be biologically equivalent to 78 Gy: 8 Gy higher than the current standard of 70 Gy standard. Although hypofractionation is standard of care in the primary PCa setting, data on hypofractionated sEBRT are scarce. A recently published systematic review supports the tolerance of hypofractionated sEBRT, but stresses the importance of conducting RCTs comparing hypofractionated with standard fractionated sEBRT [15].
To investigate the potential benefit of hypofractionated sEBRT, we will start a phase III RCT (the PERYTON-trial, ClinicalTrials.gov Identifier: NCT04642027). The aim of the PERYTON-trial is to assess whether a dose escalated hypofractionated regimen will improve the 5-year progression-free survival of sEBRT selected with PSMA PET/CT. Furthermore, we will assess the influence of hypofractionation on toxicity, quality of life (QoL) and survival.
Methods/design
Study design
The PERYTON-trial is a prospective multicentre phase III randomised controlled trial. (Fig. 1).

Fig. 1 The design of the PERYTON-trial
Participating centres are radiotherapy treatment centres in the Netherlands (updated list available on ClinicalTrials.gov).
All eligible participants will be randomly assigned (1:1) to receive:
-
1.
Current standard: conventional sEBRT, 35 × 2 Gy, biologically equivalent dose: 70 Gy.
-
2.
Experimental arm: hypofractionated sEBRT, 20 × 3 Gy, biologically equivalent dose: 78 Gy.
Participants will be stratified by PSA level (≤0.2 ng/mL vs > 0.2- ≤0.5 ng/mL vs > 0.5- < 1.0 ng/mL) and local recurrence on the PSMA PET/CT (presence versus absence).
Participants
All patients with a BCR, with a PSA value < 1.0 ng/mL, after radical prostatectomy for PCa and staged using a PSMA PET/CT scan (without any evidence of lymph nodes or distant metastases) are eligible for inclusion. Detailed in-and exclusion criteria are summarized in Table 1.
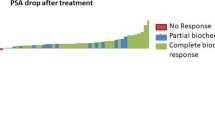
Primary endpoint
The primary endpoint is 5-year progression-free survival (PFS), defined as biochemical progression, clinical progression, loco-regional progression, distant progression or the start with hormonal therapy, whichever occurs first. Biochemical progression will be defined as a PSA value of 0.2 ng/mL higher than the PSA Nadir (defined as the lowest PSA value ≥3 months after completion of treatment). Participants with no change or an increase in PSA level after sEBRT will be defined as non-responders.
Secondary endpoints
-
Acute grade ≥ 2 gastrointestinal (GI) and genitourinary (GU) toxicities measured 3 months after treatment using both physician-reported score (Common Terminology Criteria for Adverse Events (CTCAE), version 5.0) and patient-reported questionnaires (RTOG Acute Radiation Morbidity Criteria using adapted RTOG/EORTC acute Radiation Morbidity questionnaires);
-
3- and 5-year late grade ≥ 2 GI and GU toxicities, measured using both physician-reported score (CTCAE version 5.0 criteria) and patient-reported questionnaires (RTOG/EORTC criteria);
-
QoL, using the European Organization for Research and Treatment of Cancer (EORTC) QoL thirty item score questionnaires (QLQ-C30) for health-related QoL and the EORTC QoL prostate carcinoma module (QLQ-PR25) is used;
-
Metastasis-free survival: Randomisation date to the date of metastases reported by imaging;
-
PCa-specific mortality;
-
Overall survival at 5 years from date of randomisation.
Time schedule
The PERYTON-trial started with patient accrual in September 2020. The follow-up starts from the last treatment day, and the main analysis addressing the primary endpoint (5-year PFS) is planned after 5 years of follow-up (i.e., 5 years since the inclusion of the last participant in the study).
Radiotherapy
Radiation dose in sEBRT
A dose–effect relationship has been reported in sEBRT, indicating a 2.0% improvement in bPFS for each additional Gy [16]. One recent RCT, the SAKK-trial 09/10, compared conventional dose schedule (32 × 2 Gy = 64 Gy) to a dose-escalated schedule (35 × 2 Gy = 70 Gy) and showed that dose-intensified sEBRT was not superior to conventional-dose sEBRT [17]. However, this escalated dose of only 4 Gy in the SAKK-trial is probably too low to improve outcome. Studies on dose escalation in primary PCa radiotherapy reported higher GI toxicity, while hypofractionation is proven effective with comparable acute and late toxicity results [13, 14]. This positive experience with hypofractionated radiotherapy in primary PCa may give the opportunity to apply hypofractionation as a dose escalation technique in sEBRT. Data on hypofractionated sEBRT are scarce with only few non-randomised reports. These reports showed adequate disease control and acceptable rates of acute and late side effects, indicating the need to investigate the role of hypofractionation in sEBRT in an RCT [18,19,20,21].
Quality assurance
A pre-trial quality assurance (QA) process was undertaken to ensure validity and reliability of radiation therapy treatment data to improve protocol compliance within all including centres within this trial. Completion of the pre-trial QA program is mandatory before a centre can start with accrual. At this moment, 6 centres completed the pre-trial QA program. Analyses of the pre-trial QA showed that the dose constraints of the PERYTON-trial are feasible [22].
Preparations and positioning
It is recommended to scan and treat patients with a comfortably full bladder. The use of an endorectal balloon is allowed. Local daily online position verification and correction protocols may be applied, being identical in both treatment arms. The use of feet and knee support is recommended.
Delineation
Gross tumour volume (GTV) is defined, if present, as the visible local lesion on planning CT (matched with the positive PSMA PET/CT scan). Clinical target volume (CTV) will be defined by any of the published consensus guidelines such as EORTC [23], RTOG [24] or Wiltshire et al. [25] The planning target volume (PTV) margin is according to the local verification protocol. The organs at risk (OAR) include the bladder, rectum, bilateral femora, penile bulb and the large and small bowel.
Planning
Highly conformal treatment techniques are used, i.e., intensity modulated radiation therapy (IMRT) or volumetric modulated arc therapy (VMAT). The prescribed dose to the prostate bed is:
-
Arm 1: 35 × 2.0 Gy = 70 Gy.
-
Arm 2: 20 × 3.0 Gy = 60 Gy.
If a local recurrence is detected within the prostatic bed on PSMA PET/CT-scan, it is recommended to deliver a boost to the GTV. This boost should consist of:
-
Arm 1: An equivalent dose of 74 – 78 Gy (concomitant or sequential);
-
Arm 2: An equivalent dose of 62 – 63 Gy (concomitant or sequential).
Target coverage
At least 99% of the PTV should receive 95% of the prescribed dose: PTV V95% ≥ 99%. Variation of 4% in the V95% (95-99%) is acceptable if necessary to keep the OAR dose within the protocol constraints. Furthermore, 100% of the CTV should receive 95% of the prescribed dose: CTV V95% = 100%.
Organ at risk constraints
All OAR constraints are summarized in Table 2. A variation of ≤5% of rectal and bladder volumes exceeding the protocol dose constraints are accepted, if needed to reach an acceptable target coverage. The acceptance of rectal volumes beyond this additional 5% of the constraints will be considered a major protocol violation.
Systemic treatment: no androgen deprivation therapy within the PERYTON-study
Two phase III RCTs have shown superior outcomes after postoperative sEBRT when androgen deprivation therapy (ADT) was added (6 months of LHRH-analogues or 24 months of bicalutamide) [26, 27]. However, both trials used low dose sEBRT (64.8 – 66 Gy) and included patients with high PSA levels (2.0 to 4.0 ng/mL). Therefore, the reported benefit of ADT was probably at least partly compensating for low dose sEBRT. Additionally, the benefit was limited to those patients with a high PSA level, so at higher risk for metastases, rather than an additive local benefit. This hypothesis is supported by the use of conventional imaging modalities in both studies to exclude metastases, which could enhance the benefit of ADT in both trials. Post hoc analysis by Shipley et al. showed no benefit of ADT for patients with a PSA level < 0.7 ng/mL [27]. This PSA level will apply to the majority of our population. Using the PSMA PET/CT in an early salvage setting, at low PSA levels of ≤1.0 ng/mL, it is very likely that the use of ADT in the PERYTON-trial will have no added value. In conclusion, the use of ADT is not allowed within the PERYTON-trial.
Follow-up evaluation
Participants will be followed according to the time schedule in Table 3.
Sample size considerations
A systematic review and meta-analysis reported that each additional Gy in the conventional sEBRT-arm is possibly associated with a 2% higher bPFS, independent of other factors. These results imply that our biological dose escalated effect with hypofractionation will result in 16% higher bPFS (8 Gy × 2% per Gy). However, this meta-analysis did not include series using a radiotherapy dose above 70 Gy. In higher dose series as proposed in this study, the relative benefit may be lower and consequently an expected benefit of 16% may be too optimistic. Therefore, a conservative 12% higher 5-year bPFS in the experimental arm of 20 fractions of 3 Gy compared to the conventional sEBRT schedule of 35 fractions of 2 Gy (70 Gy) has been chosen. This estimated benefit of 12% is also supported by a meta-analysis including conventional and hypofractionated regimens addressing the influence of fraction size and the total dose effect on bPFS and toxicity [28].
The results of the GETUG-AFU 16 trial showed a 5-year bPFS of 62% with the conventional fractionated radiotherapy protocol [26]. We used this percentage (62%) for the 5-year bPFS in our conventional sEBRT treatment arm. Following the above mentioned literature, we hypothesize that with the experimental regimen the bPFS can be improved from 62 to 74%. Using an alpha of 5% and a study power of 81%, the required sample size is 235 participants per treatment arm. Assuming a dropout of 12%, we need to recruit 269 participants per treatment arm: 538 in total.
Statistical analysis
The incidence of progression-free survival will be compared between the two treatment arms using Cox proportional hazards regression analysis to calculate hazard ratios and 95% confidence intervals. Acute and late toxicity rates will be summarized in terms of the proportion of participants in each arm. Log-binominal regression will be used to compare the individual highest grade of acute toxicity and the individual highest grade of late toxicity between both treatment arms. Relative risks will be calculated with 95% confidence intervals. For the analysis of QoL data, a comparison of the change in QoL from baseline level and at different time points will be performed between both treatment arms. The statistical analysis of QoL will be performed by a random effects linear regression model. Stratified randomisation will be taken into account in all analyses by adding the stratification variables to the respective regression models.
In sensitivity analyses, we will repeat all analyses, but with adjustment for potentially prognostic factors (age, pre-operative tumour stage, PSA level, time between radical prostatectomy and biochemical relapse, and comorbidity) or confounding factors (treatment centre).
Interim analysis
Dose-limiting constraints for rectum and bladder will be used (Table 2) and a QA process is mandatory before the start of inclusion in the participating centres. Toxicity is expected to be equivalent in both arms. Nevertheless, a slight increase in acute toxicity in the experimental arm might be expected due to the short overall treatment time [29]. Therefore, we will perform an interim analysis after the inclusion of 25% of the estimated number of participants (135 participants) to identify any early signs of excessive (unexpected) acute toxicity. Grade 3 CTCAE acute toxicity will be used for this interim analysis; i.e., > 5% difference in grade 3 toxicity between the experimental and control arm. If this acute toxicity difference exceeds 5%, a formal interim analysis will be performed with a nominal p value < 0.001 according to the Haybittle-Peto alpha spending function, to indicate statistical significance [30]. The interim analysis will be performed by an independent statistician, and the results will be shared with the principal investigators who will judge after informing the ethical committee whether continuation of the study is safe.
Discussion
Salvage external beam radiation therapy (sEBRT) is an established treatment option for BCR after RP, with a 5-year bPFS up to 60%. Which means that 40% of the patients receiving sEBRT experience a second BCR after radiotherapy. This suggests that sEBRT does not benefit those patients with a second BCR, while exposing them to treatment-related side effects. Hence, there is a need to improve the treatment outcome of sEBRT.
Predisposing factors for BCR after sEBRT may either originate at the primary tumour site, indicating insufficient local treatment, or from disease outside the prostate bed (i.e., occult metastases), suggesting metastatic disease for which local sEBRT is not appropriate.
The PERYTON-study aims to increase the effectiveness of sEBRT after radical prostatectomy by:
-
1.
Excluding patients with metastatic disease for sEBRT with the (early) use of the PSMA-PET/CT scan as screening imaging modality before the inclusion of patients.
-
2.
Using an hypofractionated radiotherapy schedule of 20 × 3 Gy in sEBRT to escalate the biological effective radiation dose to the prostate bed.
In conclusion, the PERYTON-trial is, to our knowledge, the first prospective phase III RCT, using the PSMA PET/CT-scan as standard imaging modality and investigating the potential benefit of a hypofractionated sEBRT schedule of 20 × 3 Gy = 60 Gy compared to the conventional fractionated standard of 35 × 2 Gy = 70 Gy.
Availability of data and materials
Not applicable.
Abbreviations
- PCa:
-
Prostate cancer
- RP:
-
Radical prostatectomy
- BCR:
-
Biochemical recurrence
- sEBRT:
-
Salvage external beam radiotherapy
- PSMA PET/CT:
-
Prostate-specific membrane antigen positron emission tomography/computed tomography
- bPFS:
-
Biochemical progression-free survival
- EQ D2:
-
Equivalent Dose at 2 Gy
- QoL:
-
Quality of life
- RCT:
-
Randomised controlled trial
- PFS:
-
Progression-free survival
- PSA:
-
Prostate specific antigen
- GI:
-
Gastrointestinal
- GU:
-
Genitourinary
- QA:
-
Quality assurance
- GTV:
-
Gross tumour volume
- CT-scan:
-
Computed tomography scan
- CTV:
-
Clinical target volume
- PTV:
-
Planning target volume
- IMRT:
-
Intensity modulated radiation therapy
- VMAT:
-
Volumetric modulated arc therapy
- OAR:
-
Organ at risk
- ADT:
-
Androgen deprivation therapy
References
Integraal Kanker Centrum Nederland Prostaatkanker Database 2018. https://iknl.nl/kankersoorten/prostaatkanker. Accessed 5 May 2020.
Ward JFMJ. Rising prostate-specific antigen after primary prostate cancer therapy. Nat Clin Pract Urol. 2005;2(4):174–82.
Swanson GP, Hussey MA, Tangen CM, Chin J, Messing E, Canby-Hagino E, et al. Predominant treatment failure in postprostatectomy patients is local: analysis of patterns of treatment failure in SWOG 8794. J Clin Oncol. 2007;25(16):2225–9.
Swanson GPRM, Hermans M. Pathologic findings at radical prostatectomy: risk factors for failure and death. Urol Oncol. 2007;25(2):110–4.
Abdollah F, Suardi N, Cozzarini C, Gallina A, Capitanio U, Bianchi M, et al. Selecting the optimal candidate for adjuvant radiotherapy after radical prostatectomy for prostate cancer: a long-term survival analysis. Eur Urol. 2013;63(6):998–1008.
Hofman MSLNFR, Tang C, Vela I, Thomas P, Rutherford N, Martin JM, et al. proPSMA study group collaborators. Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): a prospective, randomised, multicentre study. Lancet. 2020;395(10231):1208–16.
Luiting HB, vLP, Busstra MB, Brabander T, van der Poel HG, Donswijk ML, Vis AN, Emmett L, Stricker PD, Roobol MJ. Use of gallium-68 prostate-specific membrane antigen positron-emission tomography for detecting lymph node metastases in primary and recurrent prostate cancer and location of recurrence after radical prostatectomy: an overview of the current literature. BJU Int. 2020;125(2):206–14.
Ekmekcioglu O, Busstra M, Klass MD, Verzijlbergen F. Bridging the imaging gap: PSMA PET/CT has a high impact on treatment planning in prostate cancer patients with biochemical recurrence-a narrative review of literature. J Nucl Med. 2019;60(10):1394–8.
Shakespeare TP. Effect of prostate-specific membrane antigen positron emission tomography on the decision-making of radiation oncologists. Radiat Oncol. 2015;10:233.
Bashir U, Tree A, Mayer E, Levine D, Parker C, Dearnaley D, et al. Impact of Ga-68-PSMA PET/CT on management in prostate cancer patients with very early biochemical recurrence after radical prostatectomy. Eur J Nucl Med Mol Imaging. 2019;46:901–7.
Emmett L, van Leeuwen PJ, Nandurkar R, Scheltema MJ, Cusick T, Hruby G, et al. Treatment outcomes from 68Ga-PSMA PET/CT-informed salvage radiation treatment in men with rising PSA after radical prostatectomy: prognostic value of a negative PSMA PET. J Nucl Med. 2017;58(12):1972–6.
Carlson DJ, Stewart RD, Li XA, Jennings K, Wang JZ, Guerrero M. Comparison of in vitro and in vivo alpha/beta ratios for prostate cancer. Phys Med Biol. 2004;49(19):4477–91.
Catton CN, Lukka H, Gu CS, Martin JM, Supiot S, Chung PWM, et al. Randomized trial of a Hypofractionated radiation regimen for the treatment of localized prostate Cancer. J Clin Oncol. 2017;35(17):1884–90.
Dearnaley D, Syndikus I, Mossop H, Khoo V, Birtle A, Bloomfield D, et al. Conventional versus hypofractionated high-dose intensity-modulated radiotherapy for prostate cancer: 5-year outcomes of the randomised, non-inferiority, phase 3 CHHiP trial. Lancet. 2016;17(8):1047–60.
Siepe G, Buwenge M, Nguyen NP, Macchia G, Deodato F, Cilia S, et al. Postoperative Hypofractionated radiation therapy in prostate carcinoma: a systematic review. Anticancer Res. 2018;38:1221–30.
King C. The dose-response of salvage radiotherapy following radical prostatectomy: a systematic review and meta-analysis. Radiother Oncol. 2016;121(2):199–203.
Ghadjar PSH, Hayoz S, Bernhard J, et al. Dose-intensified versus conventional-dose salvage radiotherapy for biochemically recurrent prostate cancer after prostatectomy: the SAKK 09/10 randomized phase 3 trial. Eur Urol Eur Urol. 2021;80(2):306–15.
Macchia G, Siepe G, Capocaccia I, Nguyen NP, Schiavina R, Cammelli S, et al. Hypofractionated postoperative IMRT in prostate carcinoma: a phase I/II study. Anticancer Res. 2017;37:5821–8.
Cozzarini C, Fiorino C, Di Muzio N, Valdagni R, Salonia A, Alongi F, et al. Hypofractionated adjuvant radiotherapy with helical Tomotherapy after radical prostatectomy: planning data and toxicity results of a phase I-II study. Radiother Oncol. 2008;88:26–33.
Kruser TJ, Jarrard DF, Graf AK, Hedican SP, Paolone DR, Wegenke JD, et al. Early hypofractionated salvage radiotherapy for post-prostatectomy biochemical recurrence. Cancer. 2011;117:2629–36.
Alongi F, Cozzi L, Fogliata A, Iftode C, Comito T, Clivio A, et al. Hypofractionation with VMAT versus 3DCRT in postoperative patients with prostate Cancer. Anticancer Res. 2013;33:4537–44.
Staal F, Ng Wei Siang K, Brouwer CL, Vanneste B, de Jong M, Budiharto T, et al. A pre-trial quality assurance for salvage radiotherapy of the multi-institutional. PERYTON-trial ESTRO. 2021; 2021;Presentation Number: PO-1745.
Poortmans P, Vandeputte K, Bosset M, Miralbell R, Maingon P, Boehmer D, et al. EORTC radiation oncology group. Guidelines for target volume definition in post-operative radiotherapy for prostate cancer, on behalf of the EORTC radiation oncology group. Radiother Oncol. 2007;84(2):121–7.
Michalski JMLC, El Naqa I, Ritter M, O'Meara E, Seider MJ, Lee WR, et al. Development of RTOG consensus guidelines for the definition of the clinical target volume for postoperative conformal radiation therapy for prostate cancer. Int J Radiat Oncol Biol Phys. 2010;76(2):361–8.
Wiltshire KLBK, Haider MA, Zwahlen D, Kong V, Chan E, Moseley J, et al. Anatomic boundaries of the clinical target volume (prostate bed) after radical prostatectomy. Int J Radiat Oncol Biol Phys. 2007;69(4):1090–9.
Carrie CHA, de Laroche G, Richaud P, Guerif S, Latorzeff I, Supiot S, et al. Salvage radiotherapy with or without short-term hormone therapy for rising prostate-specific antigen concentration after radical prostatectomy (GETUG-AFU 16): a randomised, multicentre, open-label phase 3 trial. Lancet Oncol. 2016;17(6):747–56.
Shipley WU, Seiferheld W, Lukka HR, Major PP, Heney NM, Grignon DJ, et al. Radiation with or without antiandrogen therapy in recurrent prostate Cancer. N Engl J Med. 2017;376:417–28.
Zaorsky NGPJ, Hurwitz MD, Keith SW, Dicker AP, Den RB. What is the ideal radiotherapy dose to treat prostate cancer? A meta-analysis of biologically equivalent dose escalation. Radiother Oncol. 2015;115(3):295–300.
Vogelius IR, Bentzen SM. Dose response and fractionation sensitivity of prostate Cancer after external beam radiation therapy: a Meta-analysis of randomized trials. Int J Radiat Oncol. 2018;100(4):858–65.
Pocock S. When (not) to stop a clinical trial for benefit. JAMA. 2005;294:2228–30.
Acknowledgements
We thank all scientific staff; Prof. dr. Jourik Gietema,1 Dr. Walter Noordzij2 , drs. Christian Hammer,3 Dr. Derya Yakar4 and Dr. Alphonsus van den Bergh.3 We also thank the participating centres and their local investigators; Ben Vanneste,5 Tom Budiharto,6 Dorien Haverkort,7 Marianne de Jong,8 Birgit Hollman,9 Mariska van der Sande10 and Robert Jan Smeenk.11
1University Medical Centre Groningen, Medical Oncology, Groningen, the Netherlands.
2University Medical Centre Groningen, dept. Of Nuclear Medicine, Groningen, the Netherlands.
3University Medical Centre Groningen, dept. Of Radiation Oncology, Groningen, the Netherlands.
4University Medical Centre Groningen, dept. Of Radiology, Groningen, the Netherlands.
5Department of Radiation Oncology (MAASTRO Clinic), GROW - School for Oncology and Developmental Biology, Maastricht, the Netherlands.
6Catharina Hospital, Radiation Oncology, Eindhoven, The Netherlands.
7Radiotherapiegroep, Radiation Oncology, Arnhem/Deventer, The Netherlands.
8Radiotherapeutic Institute Friesland, Radiation Oncology, Leeuwarden, The Netherlands.
9Haga Hospital in The Hague, dept. Of Radiation Oncology, Den Haag, the Netherlands.
10Institute Verbeeten, dept. Of Radiation Oncology, Tilburg, The Netherlands.
11Radboud University Medical Centre, dept. Of Radiation Oncology, Nijmegen, The Netherlands.
Funding
This work was supported and sponsored by Dutch Cancer Society (KWF Kanker Bestrijding grant number 12649). The study protocol has undergone full external peer review by the funding body as part of the peer review process.
Author information
Authors and Affiliations
Contributions
Initial draft of the protocol: SA, RJS, JFV, IJJ, CB, ES. Revision of the protocol: SA, FS, JJ, CB, KNWS, RJS, JFV, IJJ. Final approval of the manuscript: FS, JJ, CB, JL, KNWS, ES, RJS, JFV, IJJ, SA. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol is approved by the accredited Medical Ethical Committee (METc) of all participating hospitals (date METc review: 23-06-2020, METc registration number: 202000239). Written informed consent will be obtained from all patients prior to study participation. Participants will be made aware that participation is strictly voluntary. Participants may withdraw from the study at any time.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Staal, F.H.E., Janssen, J., Brouwer, C.L. et al. Phase III randomised controlled trial on PSMA PET/CT guided hypofractionated salvage prostate bed radiotherapy of biochemical failure after radical prostatectomy for prostate cancer (PERYTON-trial): study protocol. BMC Cancer 22, 416 (2022). https://doi.org/10.1186/s12885-022-09493-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-022-09493-5