Abstract
Background
Accumulation of the signal adaptor protein p62 has been demonstrated in many forms of cancer, including pancreatic ductal adenocarcinoma (PDAC). Although data from experimental studies suggest that p62 accumulation accelerates the development of PDAC, the association between p62 protein expression and survival in PDAC patients is unclear.
Methods
Thirty-three tumor specimens from PDAC patients treated by primary surgery were obtained. Immunohistochemical expression of p62, microtubule-associated protein 1A/1B-light chain 3 (LC3), and nuclear factor-erythroid factor 2-related factor 2 (NRF2) in tumor tissue was examined for associations with clinicopathological characteristics and disease-specific survival (DSS).
Results
There was no association between p62 expression and any of the clinicopathological variables. However, high p62 protein expression in tumor cells was significantly associated with shorter DSS (7 months vs. 29 months, p = 0.017). The hazard ratio for death in patients with high p62 protein expression in tumor cells was 2.88 (95% confidence interval: 1.17–7.11, p = 0.022). In multivariable analysis, high p62 expression was an independent prognostic factor for shorter DSS (p = 0.020) when follow up time was more than 5 years. LC3 and NRF2 staining was not associated with survival or other clinicopathological parameters.
Conclusion
Our results show that high p62 protein expression in tumor cells is associated with shorter survival following pancreatic tumor resection. This association supports a role for p62 as a prognostic marker in patients with PDAC treated by primary surgery.
Similar content being viewed by others
Introduction
The stress-inducible adaptor protein p62/SQSTM1 (hereafter p62) plays important roles in the development of pancreatic cancer [1, 2]. P62 is a multi-domain protein that was originally defined as an autophagy receptor. In autophagy, p62 targets proteins and organelles for lysosomal degradation by linking cargo to microtubule-associated protein 1A/1B-light chain 3 (LC3) in the membrane of autophagosomes. However, p62 also can induce downstream signaling pathways, including NF-κB, mTORC1, and nuclear factor-erythroid factor 2-related factor 2 (NRF2), to influence inflammation, nutrient sensing, and the oxidative stress defense, which all may affect tumorigenesis [3, 4]. Experimental studies using mouse models have shown that accumulation of p62 activates NF-κB and NRF2 signaling and accelerates the development of pancreatic cancer [1, 2, 5]. Although both NRF2 and NF-κB are elevated in human pancreatic cancer [1, 6,7,8], little is known about the role of p62 accumulation and associations with its downstream pathways in the development of human pancreatic cancer.
Immunohistochemical staining for p62 has been detected in many human cancers including esophageal, gastric, and large intestinal cancers, hepatocellular carcinoma, and pancreatic ductal adenocarcinoma (PDAC) [9, 10], suggesting an association of cancer with p62 accumulation. Expression of p62 also has been linked to tumor grade, distant metastasis [11], and higher risk of metastasis and poor prognosis, particularly in breast cancer [12]. Few studies have examined the expression of p62 in PDAC tissue from patients. Although the available data indicate increased expression of p62 [2, 10], there is little information about the role of p62 accumulation in PDAC prognosis.
To elucidate the relevance of p62 expression in PDAC tissue and its prognostic value, we examined expression of p62 protein in tumor tissue sections from patients with PDAC and analyzed the association between the immunoreactivities and clinicopathological parameters. We also investigated whether an association between p62 protein expression and patient outcomes was independent of LC3 (autophagy) and NRF2 (antioxidant pathway activation).
Material and methods
All methods were carried out in accordance with SAMPL Guidelines.
Patients and tumor tissue samples
This study was conducted in accordance with the principles of the Declaration of Helsinki and approved by the Regional Ethical Review Board at the University of Gothenburg, Gothenburg, Sweden (reference number 002–06), and all participants gave written informed consent. Data were analyzed anonymously. Whole pancreatic tumor tissue sections were obtained from 33 patients (15 female/18 male) diagnosed with PDAC who underwent surgical tumor resection in 1998 to 2005 at Sahlgrenska University Hospital, Gothenburg, Sweden. Patients were included in the study based on the availability of enough archived tumor material to prepare high-quality whole tumor tissue sections for IHC analysis at the hospital pathology department. All patients underwent surgery as the primary treatment, and none had received irradiation or chemotherapy before surgery. Clinical information and follow-up data were obtained from medical records. Resection margin status was R0 for all patients, and all tumors were histologically diagnosed as ductal adenocarcinoma and classified according to the pTNM staging system (sixth edition of the AJCC) by the pathology department.
Disease-specific survival (DSS) was defined as the time between surgery and death attributable to PDAC. Three patients were still alive at the time of analysis. Of the 30 patients who died, 22 died because of PDAC. The remaining eight deaths were attributable to cardiovascular causes (n = 3), lung cancer (n = 1), neuroendocrine cancer (n = 1), postoperative complications (n = 1), chronic sub-ileus (n = 1), and an unknown cause (n = 1). The cause of death for each patient was confirmed by data obtained from the National Board of Health and Welfare in Sweden (reference number 35835/2020).
Immunohistochemistry
Immunohistochemistry was performed on 4-μm sections of formalin-fixed paraffin-embedded pancreatic tumor tissue. After xylene deparaffinization, ethanol dehydration, and antigen retrieval (microwave oven at 500 W for 2 × 5 min in citrate buffer pH 6.0), endogenous peroxidase activity was quenched by incubation in hydrogen peroxide solution (Peroxidazed 1, PX 968, Biocare Medical, Pacheco, CA, USA) for 5 min. To reduce non-specific background, sections were incubated in casein solution (Background Sniper, BS966, Biocare Medical) for 15 min. Then sections were incubated with primary antibodies in dilution buffer (Da Vinci Green Diluent, PD900, Biocare Medical) overnight at 4 °C, followed by incubation with probe (MACH 1 Mouse probe, UP537, Biocare Medical) for 15 min at room temperature (p62 only) and HRP-polymer (MACH 1 Universal HRP-Polymer, MRH538, Biocare Medical) for 30 min at room temperature. Bound peroxidase was visualized by incubation for 1–10 min in a 3,3′-diaminobenzidine (DAB) solution (Betazoid DAB Chromogen, BDB900 diluted in Betazoid DAB Substrate Buffer, DS900, Biocare Medical). Sections were washed in Tris-buffered saline, counterstained with hematoxylin, dehydrated, and mounted. Slides were photographed on an upright Nikon Eclipse E400 light microscope using a DXM1200 camera with ACT-1 version 2.0 software (Nikon, Japan). The following primary antibodies were used: monoclonal mouse anti-human p62/SQSTM1, raised against amino acids 151–440 of p62/SQSTM1 of human origin, clone D-3, (sc-28,359, Santa Cruz Biotechnology, Dallas, TX, USA), dilution 1:100; polyclonal rabbit anti-LC3B, raised against a synthetic peptide corresponding to the amino terminus of LC3B, (#2775, Cell Signaling Technology, Danvers, MA, USA), dilution 1:100; and polyclonal rabbit anti-NRF2, raised against a synthetic peptide corresponding to amino acids 569–588 of human NRF2 (ab31163, Abcam, Cambridge, UK), dilution 1:200. Normal pancreas was used as positive control for p62 and NRF2, and pancreatic tumor tissue containing β islets with endocrine cells was used as positive control for LC3. Negative controls were performed by replacing primary antibodies with matching isotype control antibodies diluted to the same protein concentration as the primary antibody. The following isotype control antibodies were used: for p62, normal mouse IgG1 (sc-3877, Santa Cruz Biotechnology, Dallas, TX, USA) and for LC3 and NRF2, polyclonal rabbit IgG (ab171870, Abcam, Cambridge, UK).
Scoring of immunohistochemical staining
Tumor tissue samples were scored semi-quantitatively under light microscopy for cytoplasmic and nuclear staining (p62 and NRF2) or cytoplasmic staining (LC3) in a blinded manner without knowledge of pathological and clinical data. A modified labeling score (H score) was calculated as previously described [13]. Separate scoring of the dominant staining intensity and the percentage of positive tumor cells (glandular or abnormal shape, high nuclear-to-cytoplasmic ratio, abnormal nuclei, i.e., pleomorphic, larger, and darker than in normal cells [14]) was performed using 10 high-magnification (× 200) fields per patient, and scores for each field were averaged. The final staining scores were determined by multiplying the percentage of positive tumor cells (0 to 100%) by the dominant staining intensity (0 = no staining, similar to negative control; 1 = weak staining, weaker than the positive control; 2 = intermediate staining, similar to the positive control; and 3 = strong staining, stronger than the positive control). Resulting scores ranged from 0 to 270 [15]. For statistical analysis, p62, LC3, and NRF2 staining scores were classified into two grades with the mean staining score as the cutoff point (high grade ≥ mean; low grade < mean) and for detailed analysis p62 staining was divided into three grades using staining scores 40 and 140 as cutoff points (p62 low ≤40; p62 intermediate > 40 and ≤ 140; p62 high > 140).
Statistical analyses
Data are presented as medians and ranges (continuous data) or as numbers and percentages (categorical data). Mann–Whitney U and Pearson’s chi-square tests were used to determine the association between p62 protein expression in tumor cells and clinicopathological and molecular parameters. The correlations of p62, LC3, and NRF2 expression were evaluated using Spearman’s rank correlation coefficient. DSS was evaluated using Kaplan–Meier survival plots, and differences in survival were tested using log-rank (Mantel–Cox) tests. Univariable Cox proportional hazards regression analysis was used to estimate hazard ratios (HRs) and 95% confidence intervals (95% CIs). Multivariable Cox proportional hazards regression analysis was performed to assess independent prognostic factors for survival using the following covariables: p62, age, sex, tumor stage, differentiation, lymph node metastasis, and adjuvant therapy. All p values corresponded to two-sided tests, and p values less than 0.05 were considered statistically significant. All statistical analyses were made using either SPSS version 25 (IBM Corp, Armonk, NY, USA) or GraphPad Prism 9 (GraphPad Software, Inc., La Jolla, CA, USA).
Results
Patient characteristics
A total of 33 patients with PDAC were included in this study. The clinical information for all cases is summarized in Table 1. The median patient age was 62 years (range, 50–80 years), and the median survival was 22.6 months (range, 1.1–212.2 months) after surgery. Among the 33 patients, 7 had received postoperative adjuvant treatment with gemcitabine.
Correlation between p62 protein expression in tumor cells and clinicopathological features
To assess the protein expression of p62, LC3, and NRF2 in pancreatic tumor cells, we performed immunohistochemistry on sections of whole pancreatic tumor tissue from the 33 patients. p62 and NRF2 were expressed in the cytoplasm and in the nucleus. LC3 was mainly expressed in the cytoplasm (Fig. 1A). Positive staining was scored according to the dominant intensity (Fig. 1B) and the percentage of positive tumor cells. The two scores were combined into a staining score.
Immunohistochemical staining for p62, LC3, and NRF2. A Representative photomicrographs of positive control staining of human normal pancreas (p62 and NRF2) and human pancreatic tumor tissue containing β islets with endocrine cells (LC3). Negative controls were stained with matching isotype control antibodies. B Representative cases illustrating the scores based on immunostaining intensity. Scale bars, 100 μm (brown: positive antibody staining, blue: hematoxylin for nuclei staining)
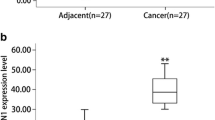
The mean staining scores of p62, LC3, and NRF2 expression were 92, 86, and 154, respectively (Fig. 2). There was no significant correlation between p62 and LC3 (rs = 0.325, p = 0.065), between p62 and NRF2 (rs = 0.117, p = 0.518), or between LC3 and NRF2 (rs = 0.045, p = 0.805).
Using the mean staining score as a cutoff point, we classified the PDAC samples into two grades: low grade and high grade (Fig. 3).
Immunohistochemical staining for p62, LC3, and NRF2 in whole pancreatic tumor tissue sections. Representative areas of pancreatic cancers stained for p62, LC3, and NRF2 and degree of staining scored as low or high. Negative controls were stained with matching isotype control antibodies. Scale bars, 100 μm (brown: positive antibody staining; blue: hematoxylin for nuclei staining)
We found no significant correlations between p62 protein expression in tumor cells and clinicopathological characteristics (Table 2).
High expression of p62 in tumor cells is a prognostic factor for survival in patients with resected PDAC
To examine the prognostic impact of p62, LC3, and NRF2 on survival outcome, we analyzed DSS according to p62, LC3, and NRF2 protein expression in tumor cells. Kaplan–Meier survival analysis using the log-rank test showed that high p62 expression in tumor cells was significantly associated with shorter DSS (Fig. 4A), whereas high LC3 or NRF2 was not (Fig. 4B, C).
p62 expression correlates with shorter survival in patients with pancreatic cancer. Kaplan–Meier curves of disease-specific survival (n = 25) according to p62 (A), LC3 (B), and NRF2 (C). Solid lines represent the survival curves, and the dotted lines indicate the 95% confidence intervals for the survival curves
The remaining clinicopathologic factors did not correlate with survival (Table 3).
To assess the relationships between p62 expression, clinicopathological variables, and survival, we performed univariable Cox proportional hazards regression analyses. The HR for death in patients with high p62 protein expression in tumor cells (when compared with low p62 protein expression in tumor cells) was 2.88 (1.17–7.11, p = 0.022; Table 4). In multivariable analysis (using a model that included p62, age, sex, tumor stage, lymph mode metastasis, differentiation, and adjuvant therapy), p62 was an independent prognostic factor for DSS (Table 4).
To assess the prognostic value of p62 expression in more detail, we used two staining score cutoffs to divide the patients into 3 groups (p62 low, p62 intermediate, and p62 high) and performed 2-year and 5-year DSS analyses using Kaplan-Meier curves and Cox proportional hazards regression analyses. Patients in the p62 high group tended to have shorter 2-year survival compared with patients in the p62 low group (HR: 3.67 [0.88–15.28], p = 0.074, Fig. 5A). Analysis of 5-year DSS showed that patients in the p62 high group had significantly shorter survival compared with patients in the p62 low group (HR: 3.99 [1.12–14.24], p = 0.033, Fig. 5B). Patients in the p62 high group had a prognosis comparable to the patients in the p62 intermediate group with a 2-year and 5-year DSS HR of 2.16 (0.63–7.39) and 2.16 (0.76–6.12), respectively (p = 0.222 and p = 0.148, respectively). In multivariable analysis (using a model that included p62, age, sex, tumor stage, lymph mode metastasis, differentiation, and adjuvant therapy), p62 expression level was not found to be an independent prognostic factor for DSS (2-year and 5-year DSS, p62 high vs p62 low: p = 0.125 and p = 0.129, respectively).
Discussion
In this study, we show that high p62 protein expression predicts shorter survival of patients with resected PDAC, supporting a role for p62 as a prognostic marker in PDAC treated with primary surgery.
To the best of our knowledge, this study is the first to show an association between high expression of p62 protein in tumor cells and survival in patients with resected PDAC. Although previous studies have reported positive p62 staining in PDAC tissue [2, 10], none has shown a significant association with survival. One group reported that p62 staining was significantly stronger in PDAC than in normal tissue or tissue with pre-malignant pancreatic intraepithelial neoplasia lesions [2]. Another study showed positive p62 staining in a majority of PDAC cases without any significant association with clinicopathological variables or overall survival [10].
In contrast, recent experimental studies have provided better insight into the biology of p62-mediated signaling in PDAC. One group reported that accumulation of p62 in stressed pancreatic acinar cells harboring mutated Kras was associated with PDAC development in mice and maintenance of malignancy in human PDAC cells [2]. An earlier study showed that p62 supports Kras-induced inflammation, which promotes PDAC development in mice [1]. Together, these findings highlight a crucial role for p62 in KRAS-driven pancreatic tumorigenesis. Because most human PDACs carry mutations in KRAS [16], p62 accumulation and activation of downstream tumor-promoting signaling also likely play an important role in the pathogenesis and progression of human PDAC.
Our finding of no significant association between high LC3 protein in tumor cells and survival is in contrast with some reports of a link between LC3 staining and patient outcomes [17, 18]. One study showed that high LC3 staining in patient tumors was significantly associated with shorter survival and that LC3 is an independent prognostic factor for survival [18]. Another group similarly found a correlation of strong positive staining for LC3 overall and in the peripheral tumor area with poor patient outcome [17]. However, in agreement with our results, another study showed no significant association between LC3 and survival [19]. Furthermore, we found no significant association between survival and staining for NRF2, one of the possible downstream signaling pathways of p62. Only one previous study has indicated an association between increased nuclear NRF2 and poor survival [7].
Our results suggest that p62 is an independent prognostic factor for shorter DSS when follow up time was more than 5 years, at least in our small patient cohort. However, the small numbers of patients in this study may explain why we found no significant associations between well-established prognostic factors such as tumor differentiation, lymph node metastasis, and survival [20,21,22]. Other reasons for these discrepancies could be the use of different antibodies or in the evaluation of the immunohistochemical staining. We used a histoscore system, in which staining intensity and percentage of tumor cells showing positive staining were assessed separately before being combined into a staining score, in which relatively more weight was given to higher-intensity staining in a given tumor sample. In addition, in contrast to our study relying on whole tissue sections, some previous groups performed immunohistochemical analysis on tissue microarrays, which can have limitations in survival analyses of small numbers of patients and when the number of tumor cores is limited [23, 24].
Our finding of an association between high p62 protein expression in tumor cells and shorter survival among patients with PDAC treated with primary surgery may be highly relevant for ongoing clinical studies of autophagy inhibitors, such as chloroquine and hydroxychloroquine in adjuvant therapies combined with chemotherapy [25, 26]. Because p62 is a signaling adaptor protein and is itself degraded by autophagy, autophagy inhibition may increase p62 levels and thereby activate p62-mediated signaling [4, 27, 28] in tumor cells. Although the mechanisms for how high expression of p62 in tumor cells causes shorter survival remain unknown, our results suggest a need for ongoing and future clinical investigations of autophagy inhibitors to monitor p62 levels in PDAC tumor cells, as too high levels may be devastating for patients.
In conclusion, we found that high p62 protein expression in tumor cells is associated with shorter survival following pancreatic tumor resection. These results support a role for p62 as a prognostic marker in patients with PDAC treated with primary surgery.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- PDAC:
-
Pancreatic ductal adenocarcinoma
- LC3:
-
Microtubule-associated protein 1A/1B-light chain 3
- NRF2:
-
Nuclear factor erythroid 2-related factor 2
- SQSTM1:
-
Sequestosome-1
- IHC:
-
Immunohistochemistry
- DAB:
-
3,3′-Diaminobenzidine
- H-score:
-
Histoscore
- OS:
-
Overall survival
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
References
Ling J, Kang Y, Zhao R, Xia Q, Lee DF, Chang Z, et al. KrasG12D-induced IKK2/beta/NF-kappaB activation by IL-1alpha and p62 feedforward loops is required for development of pancreatic ductal adenocarcinoma. Cancer Cell. 2012;21(1):105–20.
Todoric J, Antonucci L, Di Caro G, Li N, Wu X, Lytle NK, et al. Stress-activated NRF2-MDM2 Cascade controls neoplastic progression in pancreas. Cancer Cell. 2017;32(6):824–39.
Moscat J, Karin M, Diaz-Meco MT. p62 in Cancer: signaling adaptor beyond autophagy. Cell. 2016;167(3):606–9.
Sánchez-Martín P, Saito T, Komatsu M. p62/SQSTM1: ‘Jack of all trades’ in health and cancer. FEBS J. 2019;286(1):8–23.
Duran A, Linares JF, Galvez AS, Wikenheiser K, Flores JM, Diaz-Meco MT, et al. The signaling adaptor p62 is an important NF-kappaB mediator in tumorigenesis. Cancer Cell. 2008;13(4):343–54.
Lister A, Nedjadi T, Kitteringham NR, Campbell F, Costello E, Lloyd B, et al. Nrf2 is overexpressed in pancreatic cancer: implications for cell proliferation and therapy. Mol Cancer. 2011;10:37.
Soini Y, Eskelinen M, Juvonen P, Karja V, Haapasaari KM, Saarela A, et al. Nuclear Nrf2 expression is related to a poor survival in pancreatic adenocarcinoma. Pathol Res Pract. 2014;210(1):35–9.
Weichert W, Boehm M, Gekeler V, Bahra M, Langrehr J, Neuhaus P, et al. High expression of RelA/p65 is associated with activation of nuclear factor-kappaB-dependent signaling in pancreatic cancer and marks a patient population with poor prognosis. Br J Cancer. 2007;97(4):523–30.
Su Y, Qian H, Zhang J, Wang S, Shi P, Peng X. The diversity expression of p62 in digestive system cancers. Clin Immunol. 2005;116(2):118–23.
Mohamed A, Ayman A, Deniece J, Wang T, Kovach C, Siddiqui MT, et al. P62/ubiquitin IHC expression correlated with Clinicopathologic parameters and outcome in gastrointestinal carcinomas. Front Oncol. 2015;5:70.
Rolland P, Madjd Z, Durrant L, Ellis IO, Layfield R, Spendlove I. The ubiquitin-binding protein p62 is expressed in breast cancers showing features of aggressive disease. Endocr Relat Cancer. 2007;14(1):73–80.
Luo RZ, Yuan ZY, Li M, Xi SY, Fu J, He J. Accumulation of p62 is associated with poor prognosis in patients with triple-negative breast cancer. Onco Targets Ther. 2013;6:883–8.
Fagman JB, Ljungman D, Falk P, Iresjo BM, Engstrom C, Naredi P, et al. EGFR, but not COX-2, protein in resected pancreatic ductal adenocarcinoma is associated with poor survival. Oncol Lett. 2019;17(6):5361–8.
Hruban RH, Fukushima N. Pancreatic adenocarcinoma: update on the surgical pathology of carcinomas of ductal origin and PanINs. Modern Pathol. 2007;20(Suppl 1):S61–70.
Valsecchi ME, McDonald M, Brody JR, Hyslop T, Freydin B, Yeo CJ, et al. Epidermal growth factor receptor and insulinlike growth factor 1 receptor expression predict poor survival in pancreatic ductal adenocarcinoma. Cancer. 2012;118(14):3484–93.
Almoguera C, Shibata D, Forrester K, Martin J, Arnheim N, Perucho M. Most human carcinomas of the exocrine pancreas contain mutant c-K-ras genes. Cell. 1988;53(4):549–54.
Fujii S, Mitsunaga S, Yamazaki M, Hasebe T, Ishii G, Kojima M, et al. Autophagy is activated in pancreatic cancer cells and correlates with poor patient outcome. Cancer Sci. 2008;99(9):1813–9.
Yang YH, Liu JB, Gui Y, Lei LL, Zhang SJ. Relationship between autophagy and perineural invasion, clinicopathological features, and prognosis in pancreatic cancer. World J Gastroenterol. 2017;23(40):7232–41.
Ko YH, Cho YS, Won HS, Jeon EK, An HJ, Hong SU, et al. Prognostic significance of autophagy-related protein expression in resected pancreatic ductal adenocarcinoma. Pancreas. 2013;42(5):829–35.
Lim JE, Chien MW, Earle CC. Prognostic factors following curative resection for pancreatic adenocarcinoma: a population-based, linked database analysis of 396 patients. Ann Surg. 2003;237(1):74–85.
Wasif N, Ko CY, Farrell J, Wainberg Z, Hines OJ, Reber H, et al. Impact of tumor grade on prognosis in pancreatic cancer: should we include grade in AJCC staging? Ann Surg Oncol. 2010;17(9):2312–20.
Petrou A, Soonawalla Z, Silva MA, Manzelli A, Moris D, Tabet PP, et al. Prognostic indicators following curative pancreatoduodenectomy for pancreatic carcinoma: a retrospective multivariate analysis of a single Centre experience. J BUON. 2016;21(4):874–82.
Khouja MH, Baekelandt M, Sarab A, Nesland JM, Holm R. Limitations of tissue microarrays compared with whole tissue sections in survival analysis. Oncol Lett. 2010;1(5):827–31.
Tahkola K, Leppänen J, Ahtiainen M, Väyrynen J, Haapasaari K-M, Karttunen T, et al. Immune cell score in pancreatic cancer-comparison of hotspot and whole-section techniques. Virchows Archiv. 2019;474(6):691–9.
Boone BA, Bahary N, Zureikat AH, Moser AJ, Normolle DP, Wu W-C, et al. Safety and biologic response of pre-operative autophagy inhibition in combination with gemcitabine in patients with pancreatic adenocarcinoma. Ann Surg Oncol. 2015;22(13):4402–10.
Rangwala R, Chang YC, Hu J, Algazy KM, Evans TL, Fecher LA, et al. Combined MTOR and autophagy inhibition. Autophagy. 2014;10(8):1391–402.
Ichimura Y, Komatsu M. Activation of p62/SQSTM1-Keap1-nuclear factor Erythroid 2-related factor 2 pathway in Cancer. Front Oncol. 2018;8:210.
Wang Y, Xiong H, Liu D, Hill C, Ertay A, Li J, et al. Autophagy inhibition specifically promotes epithelial-mesenchymal transition and invasion in RAS-mutated cancer cells. Autophagy. 2019;15(5):886–99.
Acknowledgements
We would like to thank Lena Hallsberg for excellent technical assistance with immunohistochemistry and research nurse Christina Biörserud for help with patient data. No preregistration exists for the studies reported in this article.
Funding
Open access funding provided by University of Gothenburg. Grants from the Swedish Society of Medicine (SLS-685981 and SLS-783971 to JBF) and Assar Gabrielsson’s (FB17–17 and FB18–14 to JBF) and Lundgren’s Foundations (2017–1691 and 2018–2314 to JBF) supported this study.
Author information
Authors and Affiliations
Contributions
EP, CE, PN, and JBF conceived the study and designed the experiments. JBF performed the experiments. EP, CE, and JBF analyzed the data and performed statistical analyses. EP, CE, PN, and JBF interpreted the data. JBF drafted the manuscript. EP, CE, PN, and JBF revised the manuscript critically for important intellectual content. All authors read, reviewed, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Human pancreatic tumor tissue sections were obtained from the pathology department at Sahlgrenska University Hospital, Gothenburg, Sweden. The study was approved by the Regional Ethical Review Board at the University of Gothenburg, Gothenburg, Sweden (reference number 002–06), and all participants gave written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Philipson, E., Engström, C., Naredi, P. et al. High expression of p62/SQSTM1 predicts shorter survival for patients with pancreatic cancer. BMC Cancer 22, 347 (2022). https://doi.org/10.1186/s12885-022-09468-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-022-09468-6