Abstract
Background
Long-term antiviral treatments are associated with a significantly lower hepatocellular carcinoma (HCC) incidence in chronic hepatitis B (CHB) patients by reducing HBV DNA concentrations. However, it is still controversial whether antiviral strategies affect HCC development in antiviral treatment-naïve CHB patients. This study aimed to estimate the incidence of HCC in antiviral treatment-naïve CHB patients who were treated with Entecavir (ETV) and Tenofovir Disoproxil Fumarate (TDF) and compare the efficacy of two treatment regimens in HCC reduction.
Methods
The PubMed, Embase, China National Knowledge Infrastructure, and Wanfang databases were systematically searched until June 24, 2021. The pooled incidence and 95% confidence interval of HCC were calculated by the Freeman-Tukey double arcsine transformation method. The efficacies of ETV and TDF treatments in HCC reduction were compared through a network meta-analysis.
Results
A total of 27 studies were identified as eligible for this systematic review. The incidence densities in the ETV and TDF treatment groups were 2.78 (95% CI: 2.21-3.40) and 2.59 (95% CI: 1.51-3.96) per 100 persons-year among patients with preexisting cirrhosis and 0.49 (95% CI: 0.32-0.68) and 0.30 (95% CI: 0.06-0.70) per 100 persons-year among patients without preexisting cirrhosis. As the proportion of CHB patients with preexisting cirrhosis increased, the incidence density of HCC also increased gradually. Compared with other Nucleos(t)ide analogs (NAs) treatments, ETV and TDF treatments significantly lowered the risk of HCC, with hazard ratios (HRs) of 0.60 (95% CI: 0.40-0.90) and 0.56 (95% CI: 0.35-0.89), respectively. However, there was no difference in the incidence density of HCC between ETV and TDF treatments (HR = 0.92, 95% CI: 0.71-1.20) regardless of preexisting cirrhosis.
Conclusion
ETV and TDF treatments were associated with significantly lower risks of HCC than other NAs treatments. However, no difference was observed between ETV and TDF treatments in the risk of HCC development regardless of preexisting cirrhosis among treatment-naïve CHB patients.
Similar content being viewed by others
Background
Hepatitis B virus (HBV) infection remains a major global health problem, with 296 million people living with chronic hepatitis B (CHB) infection in 2019,with 1.5 million new infections each year [1]. CHB patients are at high risk of progression to cirrhosis and hepatocellular carcinoma (HCC) [2]. The Global Burden of Disease study estimated that HBV accounts for 33% of liver cancer-related deaths globally and 41% in Asia [3]. Nucleos(t)ide analogs (NAs) with a high barrier to HBV resistance, entecavir (ETV) or tenofovir disoproxil fumarate (TDF), are currently recommended as the first-line treatments for adults with immune-active CHB [4,5,6]. Long-term antiviral treatments are associated with a significantly lower HCC incidence in CHB patients by reducing HBV DNA concentrations [7]. However, HCC may still develop after antiviral treatment. Recent studies have suggested that there may be differences in the effects of ETV and TDF on the occurrence of HCC among CHB patients [8,9,10,11]. However, it is still controversial whether antiviral strategies affect HCC development in CHB patients [12].
Currently, meta-analyses on the effectiveness of TDF versus ETV on the incidence of HCC in CHB patients are derived from head-to-head comparisons among both antiviral treatment-naïve and antiviral therapy-experienced CHB patients [10, 13,14,15]. However, the efficacy of TDF and ETV treatment may be different in antiviral therapy-experienced CHB patients, since they may experience viral resistance before switch therapy [16]. Studies that directly compare the relative effect of ETV and TDF on the reduction of HCC development in antiviral treatment-naïve CHB patients are currently limited. Network meta-analysis can combine sources of both direct and indirect evidence [17] and provide estimates of the efficacy of multiple treatment regimens in antiviral treatment-naïve CHB patients [18].
In this study, we aimed to estimate the incidence of HCC in antiviral treatment-naïve CHB patients who were treated with ETV and TDF and compare the efficacy of two treatment regimens in HCC reduction through a systematic review and network meta-analysis.
Methods
Search strategy
We conducted a systematic literature search in the PubMed, Embase, China National Knowledge Infrastructure, and Wanfang databases until June 24, 2021. The search terms included the following: (‘chronic hepatitis B’ OR ‘hepatitis B virus infection, chronic’ OR ‘CHB’ OR ‘hepatitis B, chronic’ OR ‘Hepatitis B AND Chronic’) AND ((‘entecavir’ OR ‘Baraclude’ OR ‘ETV’) OR (‘Tenofovir disoproxil’ OR ‘Tenofovir’ OR ‘Viread’ OR ‘TDF’)) AND (‘Hepatocellular carcinoma’ OR ‘hepatocarcinoma’ OR ‘hepatic cellular cancer’ OR ‘HCC’). And the full search strategies for English databases were shown in the supplement. The reference lists from relevant articles were also screened. This study was registered in PROSPERO (No. CRD42019132954).
Selection criteria
According PICOS framework, studies were included if they met the following criteria: 1) Patients: those on antiviral treatment-naïve chronic hepatitis B patients (HBsAg and/or HBV DNA positive and related symptoms and signs for at least 6 months, not treated with antiviral therapy previously); 2) Interventions and Comparisons: ETV monotherapy or TDF monotherapy; 3) Outcomes: HCC diagnosis met one of the following criteria: a) two typical imaging findings, such as those on ultrasound, enhanced computed tomography, and magnetic resonance imaging and lesion > 2 cm; b) one typical imaging finding, lesion > 2 cm, AFP > 400 ng/ml; c) liver biopsy was positive; and 4) Study design: randomized controlled trial or cohort study. Studies including CHB patients who had a history of aflatoxin exposure or coinfection with other viruses (HAV, HCV, HDV, HEV, HIV) or preexisting HCC were excluded.
Data extraction and quality assessment
Two researchers independently assessed the eligibility of articles and extracted the required information using a standardized form. The differences were examined and settled through discussion with other authors. The information extracted from studies included the author names, publication year, study location, study design, sample size, characteristics of patients (HBeAg status, preexisting cirrhosis status), median duration of treatment, antiviral therapy and corresponding outcomes (number of patients with HCC, hazard ratio (HR)).
Quality was evaluated by Cochrane Collaboration’s tool for randomized controlled trials [19] and Newcastle-Ottawa Scale for cohort studies [20]. For randomized controlled trials, the following parameters were included when evaluating study quality: generation of the random sequence number, allocation concealment, blinding, data integrity, and selective reporting. For cohort studies, the following parameters were included when evaluating study quality: selection of the study population, comparability between groups, and measurement of the outcomes. The Newcastle-Ottawa Scale ranged from 0 to 9.
Statistical analysis
R (version 3.6.1) was used for the statistical analysis. The pooled incidence and 95% confidence interval of HCC were calculated by the Freeman-Tukey double arcsine transformation method. The efficacy of the two treatment regimens in HCC reduction was compared through network meta-analysis. For the studies that included both entire cohorts and propensity score-matched cohorts, we prioritized the latter to reduce potential bias. For studies that reported only the HR, Review Manager 5.3 was employed to restore the number of outcomes. For studies with a value of 0, we adjusted the value to 0.01. Both the cumulative incidence and incidence density of HCC were calculated and compared. For the incidence density calculation, if the total persons-year follow-up was not reported, we estimated the total persons-year by multiplying the number of subjects by the mean or median treatment duration. Heterogeneity between studies was quantified with the I2 statistic (value greater than 50% was considered substantial heterogeneity). Subgroup analyses were conducted according to treatment duration and the preexisting cirrhosis status to explore the source of heterogeneity among studies. And the sensitivity analysis was conducted based on head-to-head comparison studies that reported the adjusted HRs by propensity score-matching analysis or multivariate Cox proportional hazard analysis.
Result
Study selection and characteristics
A total of 3113 articles were initially identified. After excluding 651 duplicates, 2310 articles were excluded after reading the title and abstract. The full texts of the remaining 152 articles were reviewed, of which 27 were considered eligible for this systematic review. The study selection process is shown in Fig. 1.
The characteristics of the studies are shown in Table 1. All 27 studies were cohort studies and included a total of 52,373 chronic hepatitis B patients. Most studies (25, 93%) were from Asia, including South Korea, China, and Japan. The median treatment duration was 4.17 years (range: 0.92 to 7.29) for ETV, 3.18 years (range: 2.80 to 6.06) for TDF and 5.00 years (range: 0.92 to 6.80) for other NAs. Among all the subjects, males accounted for 62%. There were 16,490 (31%) HBeAg-positive patients, and 16,596 (32%) had preexisting cirrhosis. In total, 29, 13 and 7 studies separately analyzed HCC incidence among treatment-naïve CHB patients receiving ETV, TDF, and other NA (including lamivudine, telbivudine and adefovir) regimens. A total of 20 studies that provided comparisons of two or more treatments were used for the network meta-analysis.
HCC incidence in treatment-naïve CHB patients receiving different treatments
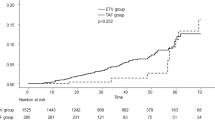
As shown in Fig. 2, the pooled estimates of the cumulative incidence of HCC among the ETV and TDF treatment groups increased with longer treatment durations and a higher proportion of CHB patients with preexisting cirrhosis. The median treatment duration and preexisting cirrhosis rate were the main sources of heterogeneity in the pooled estimation of HCC incidence (R2 = 68.11 and 64.29% in the ETV and TDF group estimations). To reduce bias in the estimation of HCC incidence, we calculated the pooled cumulative incidence and incidence density among patients with and without preexisting cirrhosis separately.
Bubble charts of the cumulative incidence by different (A) median treatment duration and (B) the proportion of CHB patients with preexisting cirrhosis subgroups. Trend lines fitted linearly represent the predicted HCC incidence according to different treatments. ETV, Entecavir; TDF, Tenofovir disoproxil fumarate; Other NAs, Nucleos(t)ide Analogues other than ETV and TDF (including Lamivudine, Telbivudine and Adefovir). The bubble size represents the sample size for each study
For patients with preexisting cirrhosis, the pooled estimates of cumulative incidence of HCC among the ETV treatment groups increased from 5.01% (95% CI: 1.32-10.49%) within 3 years of treatment to 14.21% (95% CI: 10.87-17.91%) after 5 years of treatment. For the patients treated with TDF, the cumulative incidence was 7.76% (95% CI: 5.46-10.42) at 3 to 4 years of treatment and 12.48% (95% CI: 5.86-21.11) at 4 to 5 years of treatment (Table 2).
Similar trends were also observed in patients without preexisting cirrhosis; however, the cumulative incidence of HCC was significantly lower than that in patients with preexisting cirrhosis. The cumulative incidence of HCC increased from 0.66% (95% CI: 0.19-1.38) within 3 years of ETV treatment to 3.04% (95% CI: 2.05-4.21) after 5 years of ETV treatment. For patients receiving TDF treatment, the cumulative incidence was 0.09% (95% CI: 0.02-0.20) within 3 years of treatment and 2.26% (95% CI: 1.17-3.68) at 4 to 5 years of treatment (Table 2).
The incidence densities in the ETV and TDF treatment groups were 2.78 (95% CI: 2.21-3.40) and 2.59 (95% CI: 1.51-3.96) per 100 persons-year among patients with preexisting cirrhosis and 0.49 (95% CI: 0.32-0.68) and 0.30 (95% CI: 0.06-0.70) per 100 persons-year among patients without preexisting cirrhosis, respectively (Table 2). Treatment duration and the baseline cirrhosis rate were positively associated with HCC incidence in CHB patients treated with ETV or TDF (Fig. 2). As the proportion of CHB patients with preexisting cirrhosis increased, the incidence density of HCC also increased gradually (Fig. 3). In addition, the incidence of HCC among the ETV and TDF treatment groups was lower than that in the other NA treatment group (Table 2).
Bubble charts of incidence density according to preexisting cirrhosis proportion. Trend lines fitted linearly represent the predicted HCC incidence density according to different treatments. ETV, Entecavir; TDF, Tenofovir disoproxil fumarate; Other NAs, Nucleos(t)ide Analogues other than ETV and TDF (including Lamivudine, Telbivudine and Adefovir). The bubble size represents the sample size for each study
Comparison of HCC risk in CHB patients receiving different treatments
Twenty studies [12, 21,22,23,24,25,26,27,28, 32, 34,35,36, 38, 39, 41, 43,44,45,46] provided enough data for to compare HCC risk through network meta-analysis (Fig. 4). To reduce bias due to different treatment durations, the incidence density was used to compare the HCC risk in CHB patients receiving different treatments. Detailed results are shown in Fig. 4. Compared with other NA treatments, ETV and TDF treatments significantly lowered the HCC risk, with hazard ratios (HRs) of 0.60 (95% CI: 0.40-0.90) and 0.56 (95% CI: 0.35-0.89). However, there was no difference in the incidence density of HCC between ETV and TDF treatments (HR = 0.92, 95% CI: 0.71-1.20) regardless of preexisting cirrhosis. Similar results were observed in patients with and without preexisting cirrhosis (HR = 1.07, 95% CI: 0.66-1.74; HR = 0.89, 95% CI: 0.50-1.59).
Network plot and forest plots from the network meta-analysis of HCC risk in CHB patients receiving different treatments. A Results of the total analysis. B Results of the subgroup analysis of patients with cirrhosis. C Results of the subgroup analysis of patients without cirrhosis. Control, no treatment or expectant treatment; ETV, Entecavir treatment; TDF, Tenofovir disoproxil fumarate treatment; Other NAs, Nucleos(t)ide Analogue treatments other than ETV and TDF (including Lamivudine, Telbivudine and Adefovir)
Sensitivity analysis
We conducted sensitivity analysis based on six head-to-head comparison studies that reported the adjusted HRs by propensity score-matching analysis or multivariate Cox proportional hazard analysis (Fig. 5). Moderate heterogeneity was observed (I2 = 66%), so the result from the random effects model was appropriated. The pooled adjusted HR was 0.84 (95% CI: 0.65-1.08, p = 0.18).
Discussion
Through this systematic review and network meta-analysis, we provided some important findings. First, ETV and TDF treatments were associated with a significantly lower risk of HCC than other NA treatments. Second, no difference was observed between ETV and TDF in the risk of HCC development among treatment-naïve CHB patients. Third, the proportion of CHB patients with preexisting cirrhosis was significantly associated with the incidence of HCC development, and this proportion should be balanced in future studies when comparison HCC risk according to ETV and TDF treatment.
A previous study demonstrated that other NA treatments can reduce HCC risk by 51% compared with no treatment [8, 9]. The current study showed that ETV and TDF treatments further reduced the incidence of HCC by more than 40%, from 2.84% per year in other NA-treated CHB patients to 1.10 ~ 1.71% per year in ETV- or TDF-treated patients. The annual incidence of HCC in CHB patients who received ETV or TDF was reported to range from 0.01% ~ 1.4 and 0.9% ~ 5.4 in noncirrhotic and cirrhotic patients, respectively [7]. In this study, the annual incidence densities in the ETV and TDF treatment groups were 0.49 and 0.30 per 100 persons-year among patients without preexisting cirrhosis and 2.78 and 2.59 per 100 persons-year among patients with preexisting cirrhosis, respectively. The downregulation of hepatic inflammation, reversal of fibrosis and reduction in regenerative stimuli at the tissue level, as well as reduction of HBx protein expression to levels insufficient to promote HCC development, may be the mechanisms by which NAs reduce HCC risk [47,48,49]. Achieving a virological response was significantly associated with the effectiveness of different NAs in HCC risk [7]. ETV and TDF were associated with a lower risk of viral resistance and higher virological response than other NAs, such as lamivudine and adefovir [2, 5, 50], which may contribute to the lower risk of HCC development after long-term treatment. In line with other studies, the residual risk of HCC in patients with preexisting cirrhosis was substantially higher than that in patients without preexisting cirrhosis [51]. Additionally, among patients with preexisting cirrhosis, the risk of HCC decreased over time with antiviral treatments. Studies have indicated that long-term antiviral treatments can result in the regression of liver fibrosis, which may lead to a reduction in HCC risk [52].
There was no significant difference in virological response between ETV and TDF treatments [44, 50, 53], and viral resistance to ETV and TDF is rare [54, 55]. Therefore, a similar incidence density of HCC was found among treatment-naïve CHB patients receiving ETV and TDF treatments in our study (1.43 vs 1.07 per 100 persons-year, HR = 0.92, 95% CI: 0.71-1.20). The results from recent meta-analyses on the comparison of the effectiveness of ETV and TDF for HCC reduction among both antiviral treatment-naïve and antiviral therapy-experienced CHB patients remain controversial [10, 13,14,15, 50, 56,57,58,59,60,61]. Our results were consistent with two meta-analyses [50, 56]. Meta-analyses [10, 57] that used raw data to compare the cumulative incidence of HCC among ETV and TDF treatment groups were inappropriate, since the duration of treatment was longer for ETV than for TDF in the majority of studies. The cumulative incidence of HCC among the ETV and TDF treatment groups increased with longer treatment durations. The remaining two meta-analyses used the log-transformed HR and 95% CI or incidence density to pool the overall HR for the comparison of ETV and TDF to reduce bias attributable to different treatment durations [13, 14]. These two meta-analyses included some studies on treatment-experienced patients (40% for Choi et al., 21% for Dave et al). Due to the earlier release of ETV than TDF, more patients experience viral resistance after switching to ETV than TDF, which may underestimate the effectiveness of ETV in HCC risk reduction [16]. In addition, HCC risk was not significantly different between ETV and TDF treatments in the unadjusted meta-analysis of 14 studies described by Dave et al. [14]. However, in his study, the risk of HCC among patients treated with ETV was higher than that among patients treated with TDF using a fixed-effects model with moderate heterogeneity (P = 0.04) from the available adjusted data of 7 studies. The sensitivity analysis indicated that the findings of Dave et al. were not robust. In our study, the findings are relatively robust, which are enhanced from following two aspects. First. compared to previous meta-analysis, this study is the first network meta-analysis comparing the risk of HCC between ETV and TDF monotherapy in antiretroviral treatment-naïve CHB patients that combines both direct and indirect sources of evidence. So this study included the largest target sample size. Second, this study assessed the bias introduced by inconsistent follow-up times and proportion of CHB patients with preexisting cirrhosis within patients treated with ETV and TDF monotherapy by using incidence density and subgroup analysis based on baseline cirrhosis status.
This study had some limitations. First, due to limitations of existing studies, only cohort studies were available, as randomized controlled trials are currently lacking. The selection bias between studies and differences in study design might have affected HCC risk in CHB patients treated with different antivirals. Second, due to the lack of sufficient studies, we were unable to distinguish additional subgroups, such as those with renal disease, different HBV DNA genotypes, obesity and smoking, to further compare the effects of different treatments on the risk of HCC in CHB patients with different subtypes. Third, medication adherence has a significant impact on the risk of HCC, and information on medication adherence was missing in most studies [62]. In addition, not all studies provided persons-year in the follow-up data, which may have led to bias in the estimation of the incidence density of HCC.
Conclusion
In conclusion, antiviral treatment-naïve CHB patients treated with TDF or ETV had a lower HCC risk than those treated with other NAs. CHB patients with preexisting cirrhosis had a substantially higher residual risk of HCC. No significant difference was found in the risk of HCC development between antiviral treatment-naïve CHB patients treated with ETV or TDF. These results were derived from observational studies, so higher-quality randomized controlled trials may be needed in the future to enhance the reliability of the results.
Availability of data and materials
Upon publication raw data from individual studies will be made available by the corresponding author to interested researchers requesting data for bona fide scientific purposes.
Abbreviations
- CHB:
-
Chronic hepatitis B
- ETV:
-
Entecavir
- HCC:
-
Hepatocellular carcinoma
- HRs:
-
Hazard ratios
- NAs:
-
Nucleos(t)ide analogs
- TDF:
-
Tenofovir disoproxil fumarate
References
Hepatitis B [https://www.who.int/news-room/fact-sheets/detail/hepatitis-b]. Accessed 23 Feb 2022.
Lampertico P, Agarwal K, Berg T, Buti M, Janssen HLA, Papatheodoridis G, et al. EASL 2017 clinical practice guidelines on the management of hepatitis B virus infection. J Hepatol. 2017;67(2):370–98.
Akinyemiju T, Abera S, Ahmed M, Alam N, Alemayohu MA, Allen C, et al. The burden of primary liver Cancer and underlying etiologies from 1990 to 2015 at the global, regional, and National Level: results from the global burden of disease study 2015. JAMA Oncol. 2017;3(12):1683–91.
Sarin SK, Kumar M, Lau GK, Abbas Z, Chan HLY, Chen CJ, et al. Asian-Pacific clinical practice guidelines on the management of hepatitis B: a 2015 update. Hepatol Int. 2016;10(1):1–98.
Terrault NA, Lok ASF, McMahon BJ, Chang KM, Hwang JP, Jonas MM, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology. 2018;67(4):1560–99.
Guiqiang W, Fusheng W, Hui Z, Taisheng L, Sujun Z, Hong Z, et al. Gulidelines for the prevention and treatment of chronic hepatitis B (version 2019). J Clin Hepatol. 2019;27(12):938–61.
Papatheodoridis GV, Chan HL, Hansen BE, Janssen HL, Lampertico P. Risk of hepatocellular carcinoma in chronic hepatitis B: assessment and modification with current antiviral therapy. J Hepatol. 2015;62(4):956–67.
Papatheodoridis GV, Lampertico P, Manolakopoulos S, Lok A. Incidence of hepatocellular carcinoma in chronic hepatitis B patients receiving nucleos(t)ide therapy: a systematic review. J Hepatol. 2010;53(2):348–56.
Singal AK, Salameh H, Kuo YF, Fontana RJ. Meta-analysis: the impact of oral anti-viral agents on the incidence of hepatocellular carcinoma in chronic hepatitis B. Aliment Pharmacol Ther. 2013;38(2):98–106.
Zhang Z, Zhou Y, Yang J, Hu K, Huang Y. The effectiveness of TDF versus ETV on incidence of HCC in CHB patients: a meta analysis. BMC Cancer. 2019;19(1):511.
Li SY, Li H, Xiong YL, Liu F, Peng ML, Zhang DZ, et al. Peginterferon is preferable to entecavir for prevention of unfavourable events in patients with HBeAg-positive chronic hepatitis B: a five-year observational cohort study. J Viral Hepat. 2017;24(Suppl 1):12–20.
Lee SW, Kwon JH, Lee HL, Yoo SH, Nam HC, Sung PS, et al. Comparison of tenofovir and entecavir on the risk of hepatocellular carcinoma and mortality in treatment-naive patients with chronic hepatitis B in Korea: a large-scale, propensity score analysis. Gut. 2020;69(7):1301–8.
Choi W-M, Choi J, Lim Y-S. Effects of Tenofovir vs Entecavir on risk of hepatocellular carcinoma in patients with chronic HBV infection: a systematic review and Meta-analysis. Clin Gastroenterol Hepatol. 2021;19(2):246–58.e9.
Dave S, Park S, Murad MH, Barnard A, Prokop L, Adams LA, et al. Comparative effectiveness of Entecavir vs Tenofovir for preventing hepatocellular carcinoma in patients with chronic hepatitis B: a systematic review and Meta-analysis. Hepatology. 2021;73(1):68–78.
Liu H, Shi Y, Hayden JC, Ryan PM, Rahmani J, Yu G. Tenofovir treatment has lower risk of hepatocellular carcinoma than Entecavir treatment in patients with chronic hepatitis B: a systematic review and Meta-analysis. Liver Cancer. 2020;9(4):468–76.
Lim YS, Ko MJ. Notice of retraction and replacement. Choi et al. risk of hepatocellular carcinoma in patients treated with entecavir vs tenofovir for chronic hepatitis B: a Korean nationwide cohort study. JAMA Oncol. 2019;5(1):30-36. JAMA Oncol. 2019;5(6):913–4.
Thijs V, Lemmens R, Fieuws S. Network meta-analysis: simultaneous meta-analysis of common antiplatelet regimens after transient ischaemic attack or stroke. Eur Heart J. 2008;29(9):1086–92.
Rücker G. Network meta-analysis, electrical networks and graph theory. Res Synth Methods. 2012;3(4):312–24.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. Br Med J. 2011;343:d5928.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Choi J, Kim HJ, Lee J, Cho S, Ko MJ, Lim YS. Risk of hepatocellular carcinoma in patients treated with Entecavir vs Tenofovir for chronic hepatitis B: a Korean Nationwide cohort study. JAMA Oncol. 2019;5(1):30–6.
Coffin CS, Rezaeeaval M, Pang JX, Alcantara L, Klein P, Burak KW, et al. The incidence of hepatocellular carcinoma is reduced in patients with chronic hepatitis B on long-term nucleos(t)ide analogue therapy. Aliment Pharmacol Ther. 2014;40(11-12):1262–9.
Güzelbulut F, Gökçen P, Can G, Adalı G, Değirmenci Saltürk AG, Bahadır Ö, et al. Validation of the HCC-RESCUE score to predict hepatocellular carcinoma risk in Caucasian chronic hepatitis B patients under entecavir or tenofovir therapy. J Viral Hepat. 2021;28(5):826–36.
Ha I, Chung JW, Jang ES, Jeong SH, Kim JW. Comparison of the on-treatment risks for hepatocellular carcinoma between entecavir and tenofovir: a propensity score matching analysis. J Gastroenterol Hepatol. 2020;35(10):1774–81.
Hosaka T, Suzuki F, Kobayashi M, Seko Y, Kawamura Y, Sezaki H, et al. Long-term entecavir treatment reduces hepatocellular carcinoma incidence in patients with hepatitis B virus infection. Hepatology. 2013;58(1):98–107.
Hsu YC, Jun T, Huang YT, Yeh ML, Lee CL, Ogawa S, et al. Serum M2BPGi level and risk of hepatocellular carcinoma after oral anti-viral therapy in patients with chronic hepatitis B. Aliment Pharmacol Ther. 2018;48(10):1128–37.
Hsu YC, Wong GL, Chen CH, Peng CY, Yeh ML, Cheung KS, et al. Tenofovir versus Entecavir for hepatocellular carcinoma prevention in an international consortium of chronic hepatitis B. Am J Gastroenterol. 2020;115(2):271–80.
Kim DS, Jeon MY, Lee HW, Kim BK, Park JY, Kim DY, et al. Influence of hepatic steatosis on the outcomes of patients with chronic hepatitis B treated with entecavir and tenofovir. Clin Mol Hepatol. 2019;25(3):283–93.
Kim EJ, Yeon JE, Kwon OS, Lee HN, Shin SK, Kang SH, et al. Rapid alanine aminotransferase normalization with Entecavir and hepatocellular carcinoma in hepatitis B virus-associated cirrhosis. Dig Dis Sci. 2017;62(3):808–16.
Kim GA, Han S, Kim HD, An J, Lim YS. Higher risk of hepatocellular carcinoma in chronic hepatitis B vs chronic hepatitis C after achievement of virologic response. J Viral Hepat. 2017;24(11):990–7.
Kim JH, Sinn DH, Kang W, Gwak GY, Paik YH, Choi MS, et al. Low-level viremia and the increased risk of hepatocellular carcinoma in patients receiving entecavir treatment. Hepatology. 2017;66(2):335–43.
Kim SU, Seo YS, Lee HA, Kim MN, Lee YR, Lee HW, et al. A multi-center study of entecavir vs. tenofovir on prognosis of treatment-naive chronic hepatitis B in the Republic of Korea. J Hepatol. 2019;71(3):456–64.
Lee J, Yoo SH, Sohn W, Kim HW, Choi YS, Won JH, et al. Obesity and hepatocellular carcinoma in patients receiving entecavir for chronic hepatitis B. Clin Mol Hepatol. 2016;22(3):339–49.
Lei L, Wei L, Yuhan C, Peng L, Feili W, Chunlei F, et al. Increased incidence of hepatocellular carcinoma due to antiviral drug resistance in patients with hepatitis B-related ecompensated cirrhosis. Infect Dis Inform. 2012;25(05):287–91.
Yi L. Observation on the incidence of primary liver cancer after chronic hepatitis B patients treated with Entecavir and Adefovir. Guide China Med. 2013;34:434–5.
Lim YS, Han S, Heo NY, Shim JH, Lee HC, Suh DJ. Mortality, liver transplantation, and hepatocellular carcinoma among patients with chronic hepatitis B treated with entecavir vs lamivudine. Gastroenterology. 2014;147(1):152–61.
Lin TC, Chiu YC, Chiu HC, Liu WC, Cheng PN, Chen CY, et al. Clinical utility of hepatitis B surface antigen kinetics in treatment-naive chronic hepatitis B patients during long-term entecavir therapy. World J Gastroenterol. 2018;24(6):725–36.
Oh H, Yoon EL, Jun DW, Ahn SB, Lee HY, Jeong JY, et al. No difference in incidence of hepatocellular carcinoma in patients with chronic hepatitis B virus infection treated with Entecavir vs Tenofovir. Clin Gastroenterol Hepatol. 2020;18(12):2793–802.
Ying O, Wei L, Yuhan C, Feili W, Lei L, Chunlei F, et al. Comparing the efficacy of monotherapy versus combination therapy of nucleos(t)ide analogues for decompensated HBV liver cirrhosis. Beijing Med J. 2011;33(12):966–9.
Sou FM, Hu TH, Hung CH, Lai HC, Wang JH, Lu SN, et al. Incidence and predictors of hepatocellular carcinoma beyond year 5 of entecavir therapy in chronic hepatitis B patients. Hepatol Int. 2020;14(4):513–20.
Shin JW, Jeong J, Jung SW, Lee SB, Park BR, Kim MJ, et al. Comparable incidence of hepatocellular carcinoma in chronic hepatitis B patients treated with Entecavir or Tenofovir. Dig Dis Sci. 2020;10:10.
Sohn W, Cho JY, Kim JH, Lee JI, Kim HJ, Woo MA, et al. Risk score model for the development of hepatocellular carcinoma in treatment-naive patients receiving oral antiviral treatment for chronic hepatitis B. Clin Mol Hepatol. 2017;23(2):170–8.
Su TH, Hu TH, Chen CY, Huang YH, Chuang WL, Lin CC, et al. Four-year entecavir therapy reduces hepatocellular carcinoma, cirrhotic events and mortality in chronic hepatitis B patients. Liver Int. 2016;36(12):1755–64.
Wu IT, Hu TH, Hung CH, Lu SN, Wang JH, Lee CM, et al. Comparison of the efficacy and safety of entecavir and tenofovir in nucleos(t)ide analogue-naive chronic hepatitis B patients with high viraemia: a retrospective cohort study. Clin Microbiol Infect. 2017;23(7):464–9.
Yip TC, Wong VW, Chan HL, Tse YK, Lui GC, Wong GL. Tenofovir is associated with lower risk of hepatocellular carcinoma than Entecavir in patients with chronic HBV infection in China. Gastroenterology. 2020;158(1):215–25 e216.
Yu JH, Jin YJ, Lee JW, Lee DH. Remaining hepatocellular carcinoma risk in chronic hepatitis B patients receiving entecavir/tenofovir in South Korea. Hepatol Res. 2018;48(11):862–71.
Arzumanyan A, Reis HM, Feitelson MA. Pathogenic mechanisms in HBV- and HCV-associated hepatocellular carcinoma. Nat Rev Cancer. 2013;13(2):123–35.
But DY, Lai CL, Yuen MF. Natural history of hepatitis-related hepatocellular carcinoma. World J Gastroenterol. 2008;14(11):1652–6.
Kew MC. Hepatitis B virus x protein in the pathogenesis of hepatitis B virus-induced hepatocellular carcinoma. J Gastroenterol Hepatol. 2011;26(Suppl 1):144–52.
Wang X, Liu X, Dang Z, Yu L, Jiang Y, Wang X, et al. Nucleos(t)ide analogues for reducing hepatocellular carcinoma in chronic hepatitis B patients: a systematic review and Meta-analysis. Gut Liver. 2020;14(2):232–47.
Tseng CH, Tseng CM, Wu JL, Hsu YC, El-Serag HB. Magnitude of and prediction for risk of hepatocellular carcinoma in patients with chronic hepatitis B taking Entecavir or Tenofovir therapy: a systematic review. J Gastroenterol Hepatol. 2020;35(10):1684–93.
Okada M, Enomoto M, Kawada N, Nguyen MH. Effects of antiviral therapy in patients with chronic hepatitis B and cirrhosis. Expert Rev Gastroenterol Hepatol. 2017;11(12):1095–104.
Guzelbulut F, Ovunc AO, Oetinkaya ZA, Senates E, Gokden Y, Salturk AG, et al. Comparison of the efficacy of entecavir and tenofovir in chronic hepatitis B. Hepatogastroenterology. 2012;59(114):477–80.
Chang TT, Liaw YF, Wu SS, Schiff E, Han KH, Lai CL, et al. Long-term entecavir therapy results in the reversal of fibrosis/cirrhosis and continued histological improvement in patients with chronic hepatitis B. Hepatology. 2010;52(3):886–93.
Buti M, Tsai N, Petersen J, Flisiak R, Gurel S, Krastev Z, et al. Seven-year efficacy and safety of treatment with tenofovir disoproxil fumarate for chronic hepatitis B virus infection. Dig Dis Sci. 2015;60(5):1457–64.
Li M, Lv T, Wu S, Wei W, Wu X, Ou X, et al. Tenofovir versus entecavir in lowering the risk of hepatocellular carcinoma development in patients with chronic hepatitis B: a critical systematic review and meta-analysis. Hepatol Int. 2020;14(1):105–14.
Gu L, Yao Q, Shen Z, He Y, Ng DM, Yang T, et al. Comparison of tenofovir versus entecavir on reducing incidence of hepatocellular carcinoma in chronic hepatitis B patients: a systematic review and meta-analysis. J Gastroenterol Hepatol. 2020;35(9):1467–76.
Tseng CH, Hsu YC, Chen TH, Ji F, Chen IS, Tsai YN, et al. Hepatocellular carcinoma incidence with tenofovir versus entecavir in chronic hepatitis B: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5(12):1039–52.
Yuan BH, Li RH, Huo RR, Li MJ, Papatheodoridis G, Zhong JH. Lower risk of hepatocellular carcinoma with tenofovir than entecavir treatment in subsets of chronic hepatitis B patients: an updated meta-analysis. J Gastroenterol Hepatol. 2022 (Online ahead of print)
Yuan J, Peng Y, Hao FB, Wang YQ, Wang CR, Zhong GC. No difference in hepatocellular carcinoma risk in chronic hepatitis B patients treated with tenofovir vs entecavir: evidence from an updated meta-analysis. Aging. 2021;13(5):7147–65.
Teng YX, Li MJ, Xiang BD, Zhong JH. Tenofovir may be superior to entecavir for preventing hepatocellular carcinoma and mortality in individuals chronically infected with HBV: a meta-analysis. Gut. 2020;69(10):1900–2.
Lee J, Cho S, Kim HJ, Lee H, Ko MJ, Lim YS. High level of medication adherence is required to lower mortality in patients with chronic hepatitis B taking entecavir: a nationwide cohort study. J Viral Hepat. 2021;28(2):353–63.
Acknowledgements
Not applicable.
Funding
This work was funded by National Natural Science Foundation of China (U1905205 and 81871316) and CAMS Innovation Fund for Medical Sciences (2019RU022).
Author information
Authors and Affiliations
Contributions
ZHH and GYL are co-first author. ZHH, GYL, TW, YQ, YBW, YYS, JZ, NSX conceived and designed the study. YQ and NSX obtained funding. ZHH, GYL, LXQ, GHZ, YH, XMY, XHL and SJH acquired, analyzed and interpreted the data. ZHH and YYS wrote the paper. All authors critically reviewed the different drafts of the manuscript and approved the final version.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
All the author declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Huang, ZH., Lu, GY., Qiu, LX. et al. Risk of hepatocellular carcinoma in antiviral treatment-naïve chronic hepatitis B patients treated with entecavir or tenofovir disoproxil fumarate: a network meta-analysis. BMC Cancer 22, 287 (2022). https://doi.org/10.1186/s12885-022-09413-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-022-09413-7