Abstract
Background
It has been postulated that patient’s sex impacts response to immunotherapy. Sex modulation of immunotherapy benefit, however, has not yet been explored using patient-level data, where potential confounders, as well as histologic type, can be accounted for. Here we investigated the association between sex and chemoimmunotherapy efficacy for non-small cell lung cancer (NSCLC) using a large, nation-wide dataset.
Patients & methods
Stage IV NSCLC patients diagnosed in 2015 were identified in the National Cancer Database (NCDB). Patients were treated with either chemoimmunotherapy or chemotherapy alone. The efficacy of the addition of immunotherapy treatment by sex was investigated using both an adjusted Cox proportional hazards model and propensity-score matching, in both the overall cohort and stratified by histological subtype.
Results
2064 (16%) patients received chemoimmunotherapy and10,733 (84%) received chemotherapy alone. Adjusted survival analysis in the overall cohort showed that both males (hazards ratio (HR)adj: 0.80, 95% CI: 0.74–0.87) and females (HRadj: 0.83, 95% CI: 0.76–0.90) had better OS when treated with chemoimmunotherapy than chemotherapy alone, with no statistically significant interaction between sex and receipt of immunotherapy (p = 0.63). Propensity matching confirmed these results. However, for those with squamous cell histology, male patients derived more benefit from chemoimmunotherapy treatment than females (HRadj: 0.73, 95% CI: 0.58–0.91 vs HRadj: 1.03, 95% CI: 0.76–1.38; p for interaction = 0.07).
Conclusion
Male patients with squamous cell carcinoma may derive more benefit from chemoimmunotherapy treatment. Histology likely plays an important role in how sex modulates immunotherapy efficacy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Platinum-based doublet chemotherapy was the mainstay treatment for advanced, non-small cell lung cancer (NSCLC) for decades, until, in 2015, the FDA approved Pembrolizumab for patients with metastatic disease who had: 1) failed to respond to other treatments and 2) had tumors expressing PD-L1 [1]. Immune checkpoint inhibitors (either anti-CTLA-4 or anti-PD-1/PD-L [Pembrolizumab]) work by allowing T-lymphocytes to overcome checkpoints imposed by tumor cells, thus galvanizing the anti-tumor immune response [2]. Advanced NSCLC patients treated through immune-checkpoint inhibition show significantly improved survival rates [3,4,5]. While treatment paradigms continue to evolve, most patients with advanced-stage NSCLC without targetable driver mutations receive a combination of immunotherapy and chemotherapy as front-line treatment.
However, not all NSCLC patients experience benefit from immunotherapy, suggesting factors modulate immunotherapy response, with clinical characteristics acting as surrogates for underlying biological processes [6]. Sex, specifically, may play an important role in immunotherapy efficacy. Females in general are known to mount stronger innate and adaptive immune responses, as evidenced by their: 1) ability to clear pathogens faster; 2) greater antibody production in response to vaccinations; and 3) higher rates of autoimmune disorders compared to males [7,8,9,10]. A stronger anti-tumor immune response in females may be responsible for the improved cancer-related outcomes seen across several cancer types and stages. Moreover, experimental evidence from animal models suggests sex-hormone modulation of the PD-1–PD-L1 pathway of immune regulation [11, 12]. Conversely, cancers in males may have higher immunogenicity as a result of sex-related differences in mutagenic risk factors, mainly smoking and occupational exposure [13].
A recent meta-analysis of randomized clinical trials (RCTs) suggested that male patients with advanced solid malignancies derive more benefit from immune checkpoint inhibitors than females [12]. However, the same group reported the converse to be true when analyzing the effect of the combination of PD-L1/PD-1 inhibitors and chemotherapy, with female patients experiencing a greater degree of benefit [14]. These results imply that any postulated sex-based differences in immunotherapy response result from complex interactions of underlying biological and environmental factors. However, these and other prior analyses exploring the role of sex and immunotherapy response have not accounted for key patient-level data [12, 15] such as age, comorbidity, and histologic type, which may be modifying the relationship between patients’ sex and immunotherapy efficacy.
In this study we used hospital-based, individual-level data to investigate whether the efficacy of chemoimmunotherapy compared to chemotherapy alone differs according to sex in stage IV NSCLC patients, adjusting for key clinical covariates. Because histology is an important factor in treatment decision, safety and efficacy in NSCLC, [16] we also stratified by histological type. As a secondary aim, we limited to the subset of NSCLC patients treated with chemoimmunotherapy to assess which sex, on average, had better survival outcomes.
Methods
Study population
The study cohort was identified from the National Cancer Database (NCDB), a joint project between the American College of Surgeons and the American Cancer Society, which provides clinical information for over 70% of annual incident cancer diagnoses nationwide [17]. We included all patients with pathologically confirmed, primary stage IV NSCLC (American Joint Committee on Cancer staging manual, 7th edition), who were diagnosed in 2015, and treated with either chemotherapy alone or combination of chemotherapy with immunotherapy as first line treatment. 2015 was the most recent year of NCDB data available to us with sufficient follow-up information for survival analysis.
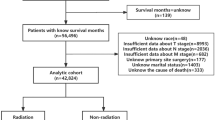
Patients without complete treatment information were excluded. Patients were also excluded if they received doses of radiotherapy greater than what would be given for palliative care (> 4000 Gy) or if radiation dosage was unknown. Patients with a recorded brain metastasis at the time of diagnosis and subsequent brain radiation were also excluded due to the historically worse outcomes these patients experience regardless of systemic treatment choice. Lastly, patients who had a contraindication to immunotherapy or had missing data to confirm whether they received immunotherapy as first line were also excluded (Supplemental Fig. 1).
Variables
From the NCDB we extracted information on patient’s sex, age at diagnosis, race (white, Black or Asian/other), Charlson-Deyo comorbidity index score, tumor histology (adenocarcinoma, squamous or large cell/other), receipt of palliative radiation, insurance status (uninsured, private, public or unknown), median household income for the patient area of residence and year of diagnosis. NCDB provides first line cancer-directed treatment, which we used to classify patients as receiving either chemotherapy alone, or chemoimmunotherapy. Receipt of immunotherapy was specifically determined by using the NCDB variable RX_SUMM_IMMUNOTHERAPY, which is defined as receiving “biological or chemical agents that alter the immune system or change the host’s response to tumor cells” [17, 18]. However, the specific type of immunotherapy received by each study patient is not provided. Agents included in the NCDB immunotherapy variable include immune checkpoint inhibitors (e.g., anti-PD1/PDL1 or anti-CTLA4 inhibitors), tumor vaccines, and other immunomodulatory drugs (Supplemental Table 1) [17,18,19]; many of these agents are described in the code book as being used as part of clinical trials. A complete list of agents classified as immunotherapy according to the NCDB are listed in their Participant User File (PUF) data dictionary [17].
Statistical analysis
We compared two groups: patients receiving chemoimmunotherapy versus those receiving chemotherapy alone; baseline clinical and demographic characteristics were compared using χ2tests for categorical variables and t-tests for continuous variables.
We performed multivariable Cox-Proportional Hazards regression to assess the association of chemoimmunotherapy treatment and overall survival (OS) according to sex, and adjusting for age, histology, race, comorbidity index, receipt of palliative radiation, insurance status, median household income and year of diagnosis. An interaction term between sex and receipt of chemoimmunotherapy was added to the model and a p interaction < 0.05 was considered statistically significant. Subsequently, propensity scores estimating the likelihood that each patient received immunotherapy were calculated separately for males and females, based on all other covariates. Within the male and female subpopulations, an optimal algorithm was used to create a 1:1 match to create balanced cohorts within each sex, as described by Greene and Stuart [20, 21]. Cox proportional hazards regression, accounting for matching, was run on the combined (male and female) propensity-matched cohort to assess the association of immunotherapy and OS by sex; an interaction term of sex*immunotherapy was added and considered significant at a p value < 0.05. As an additional sensitivity analysis, we also stratified both the adjusted and propensity matched analyses by histological type. As a secondary objective, for the subset of patients receiving immunotherapy, we used multivariable Cox proportional hazards regression to assess the independent association of gender with overall survival.
All statistical analysis was performed using SAS version 9.4 (Cary, NC: SAS Institute Inc.). The American College of Surgeons and the Commission on Cancer have not verified and are not responsible for the analytic or statistical methodology used, or the conclusions drawn from these data by the investigator. This study was determined to be human subject research exempt by the institutional review board of Mount Sinai Hospital. All methods were carried out in accordance with relevant guidelines and regulations.
Results
Patient characteristics
Of the 12,797 patients that met selection criteria, 10,733 (84%) received chemotherapy alone and 2064 (16%) received chemoimmunotherapy. Those receiving chemoimmunotherapy were significantly more likely to be younger (p < 0.0001), have adenocarcinoma (p < 0.0001), be white (p < 0.0001), and have private health insurance (p < 0.0001) (Table 1), than those receiving chemotherapy alone.
Survival
In the full cohort, the median OS those receiving just chemotherapy alone and chemoimmunotherapy was 9.20 and 12.58 months, respectively. Median OS for males and females was and 8.51 and 11.53 months, respectively. Adjusted survival analysis showed that both males (hazard ratio (HR)adj: 0.80, 95% CI: 0.74–0.87) and females (HRadj: 0.83, 95% CI: 0.76–0.90) had better OS when treated with chemoimmunotherapy, compared to chemotherapy alone. There was no statistically significant interaction between sex and receipt of immunotherapy (p for interaction = 0.63). These findings were consistent in the propensity-score matched analysis (HR: 0.80, 95% CI: 0.72–0.88; HR: 0.88, 95% CI: 0.79–0.99 for males and females, respectively; p for interaction = 0.21) (Table 2).
In the adenocarcinoma subgroup, chemoimmunotherapy treatment was associated with better OS for both males (HRadj: 0.82, 95% CI: 0.75–0.90) and females (HRadj: 0.85, 95% CI: 0.77–0.94), with no statistically significant interaction between sex and receipt of immunotherapy (p for interaction = 0.65) in the adjusted survival model. These results were consistent after propensity score matching (HR: 0.79, 95% CI: 0.70–0.88; HR: 0.85, 95% CI: 0.74–0.96 for males and females, respectively; p for interaction = 0.43). In patients with squamous histology, males derived more benefit from the addition of immunotherapy to chemotherapy treatment (HRadj: 0.73, 95% CI: 0.58–0.91 and HR: 0.86, 95% CI: 0.61–1.21, adjusted and propensity matched models, respectively). Female benefit was not apparent (HRadj: 1.03, 95% CI: 0.76–1.38 and HR: 0.97, 95% CI: 0.62–1.53, adjusted and propensity matched). In the adjusted model, the efficacy of chemoimmunotherapy treatment was marginally statically significantly different between male and female patients (p for interaction = 0.07) The p for interaction in the propensity matched model (n = 276) was not statistically significant (p = 0.67) (Table 3).
Among the subset of patients who received chemoimmunotherapy female sex (HRadj 0.79, 95% CI: 0.71–0.88), was associated with better OS. After propensity matching to balance the cohort across sex, females had significantly better OS than males (HR 0.84, 95% CI: 0.72–0.97; Table 4).
Discussion
In this study, both males and female stage IV NSCLC patients treated with chemoimmunotherapy were found to have better overall survival compared to those treated with chemotherapy alone. In the overall patient cohort, benefit from the addition of immunotherapy was similar between sexes. However, when stratifying by the main histological subtypes of NSCLC, we did not observe any difference in immunotherapy efficacy between male and female adenocarcinoma patients, although our results preliminarily suggest a greater degree of benefit in male versus female squamous cell patients. Lung adenocarcinoma and squamous cell carcinoma, while subtypes of the same disease, are in fact known to vary dramatically both in terms of their genomic and clinical attributes [22]. More recently, key differences between these histological subtypes has been observed in terms of immune host response, with implications for immunotherapy response [22]. Sample size of this sub-group was small, however, especially in the propensity-matched cohort; replication of this finding in a much larger cohort of squamous cell patients is necessary.
In meta-analyses conducted by Conforti et al., they found that males derive significantly more clinical benefit than females when treated with immune checkpoint inhibitors for NSCLC, yet found the opposite to be true when studying the effects of the addition of immunotherapy to chemotherapy, reporting pooled survival estimates of 0.76 (95% CI = 0.66 to 0.87) and 0.48 (95% CI = 0.35 to 0.67) for men and women, respectively [12, 14]. By comparison, our analysis showed the addition of immunotherapy treatment as having a smaller impact on survival, and we did not find any evidence of female NSCLC patients deriving more benefit from chemoimmunotherapy. Estimates from Conforti et al. are based on results of randomized clinical trials, the patients of which are traditionally known to differ both clinically and demographically from patients in real-world settings. The authors also acknowledge as a major limitation the use of data extracted from published studies, which precluded them from being able to adjust for patient-level characteristics that differ by sex and may affect treatment outcomes. Our study used population-based, patient-level data that included key clinical and demographic information that allowed for adjustment for potential confounders, such as age, comorbidity, and income, using several different statistical modeling techniques. Consideration of these confounders is critical when investigating the impact of sex on immunotherapy response; we show here the tremendous importance of taking into account histological subtype, which isn’t possible in most meta-analyses. Moreover, even when clinical trials are stratified by histological subtype, such as the KEYNOTE-407 trial investigating pembrolizumab plus chemotherapy in patients with metastatic squamous NSCLC, female patients are often dramatically underrepresented [23]. In this recent trial, just 19% of study participants were female [23]. While a limitation of our analysis is that only 2015 data was available, with FDA-approval of immunotherapy treatment for NSCLC beginning later in that year, the high percentage (47%) of chemoimmunotherapy patients being female attests to the enrichment of real-world patients over RCT participants in our data. Using real-world, patient-level data is necessary is necessary to more fully understand disparities in chemotherapy plus immunotherapy response, and we hope to see this work replicated in larger, more recent datasets in future.
NCDB is in fact one of the first large clinical datasets to include data for immunotherapy treatment along with long-term survival data. A significant limitation of immunotherapy trials is the lack of long-term follow up, resulting in the use of surrogate endpoints such as response rates and progression free survival to estimate benefit, [24] which may not be entirely representative of actual benefit [25]. We consider it a notable strength of our study that NCDB has highly accurate mortality data that spans multiple years on a large sample size, creating an opportunity to assess the true benefits of immunotherapy in specific patient subsets.
While our results did benefit from the comprehensiveness of the NCDB data, there were important variables missing from the data, the exclusion of which may be influencing the results. Specifically, we did not have key elements such as ECOG status; if patients with lower ECOG status were less likely to receive immunotherapy, the results could be biased towards showing the combination of immunotherapy + chemotherapy to be more efficacious than it actually is. We were able, however, to adjust for comorbidity status which should be a good proxy for EGOG performance. In addition, patients’ sex is not known to be associated with ECOG status, [26] thus ECOG should not have affected the observed relative difference in treatment efficacy between the sexes. Because the NCDB is a clinical database sourced from registry data, other potential confounders, such as EGFR, ALK, ROS mutational status, which are known predictive biomarkers for NSCLC, and differ by sex, were missing in the NCDB. Since women are more likely to harbor these mutations [27] the inability to adjust for these markers is a considerable limitation. However, the incidence of driver mutations in squamous cell lung cancers is extremely low, [28] therefore EGFR/ALK/ROS1 mutations should have no impact on the findings reported for the stratified analysis on squamous cell lung cancer. Smoking status, too, was missing from the NCDB data. While all histologic types of lung cancer are significantly associated with cigarette smoking, this association is strongest for squamous cell carcinoma [29]. Additionally, smoking history is more commonly reported for male patients than female. Stratifying according to histology and sex should reduce some bias, but we acknowledge that smoking status is an important potential confounder we could not fully adjust for. We were also unable to study the role of tumor mutation burden and the tumor microenvironment, which may be impacted by smoking [30]. While the results reported here of our analysis using individual patients’ data are meant to overcome some of the limitations of the previous meta-analyses conducted on this topic, future research is needed to explore how some of the covariates lacking in the NCDB might influence immunotherapy response according to sex. As larger, more detailed datasets containing immunotherapy information become available, we recommend that this analysis be repeated. Use of electronic health registry data, for example, might be one avenue to overcome these limitations.
Another major limitation to this work is that the specific type of immunotherapy agent used was not reported in the NCDB. Moreover, several of the drugs included in the NCDB immunotherapy variable are not FDA-approved or conventional immunotherapies, although all agents included have been shown in preclinical and/or clinical studies to modulate the anti-tumor immune response. Never-the-less, we have reason to believe that this patient population is enriched for those who did in fact receive immune checkpoint inhibitors. The patient selection helped us to reduce the heterogeneity of drugs included under the “immunotherapy” variable in the NCDB. By limiting the analysis to only those patients diagnosed in 2015, the year the FDA approved the first immunotherapy drugs for NSCLC treatment, we have enriched for patients receiving immune checkpoint inhibition drugs compared to patients diagnosed in previous years. We also tried to get an estimate of which types of drugs would have been available for clinical use in 2015 and onward, and how likely it is that patients included in the present analysis were treated with immunotherapeutic agents that are now excluded from clinical use. We observed that many of the immunotherapeutic treatments included as part of the NCBD’s immunotherapy variable have never been approved for use among NSCLC patients, making it unlikely that our patient population were treated with these. For instance, the NCDB immunotherapy variable is inclusive of EGFR antibodies, but these drugs were never FDA approved for standard of care therapy in NSCLC, so it is doubtful that the patients in our dataset received this form of treatment. Moreover, we completed an extensive search of the literature, including clinicaltrails.gov and PubMed, looking for clinical trials using EGFR antibody treatment for NSCLC during our study period [31]. All trials inclusive of EGFR antibodies were conducted only in combination with chemotherapy treatment. We therefore conduced a sensitivity analysis on immunotherapy only vs chemotherapy only treatment, and found that there was no statistically significant interaction between sex and immunotherapy efficacy (p > 0.05, data not shown). Stratification according to histologic type should have also helped to provide a cleaner picture of immunotherapy efficacy by sex. In squamous cell carcinoma cases angiogenesis inhibitors are contraindicated due to increased risk of bleeding, [16] thus we expect that the squamous cell lung cancer patients recorded as treated with immunotherapy would not have received anti-VEGF treatment. In this stratified analysis we observed a difference in treatment efficacy between sexes when immunotherapy was added to chemotherapy. Ideally this analysis will be replicated in a larger patient-level dataset reporting specific immune checkpoint inhibitor information; it would be interesting to see if the difference in efficacy observed among squamous cell patients is seen among those with adenocarcinoma when immunotherapy drugs are limited concisely to immune checkpoint inhibitors. The lack of details on type of immunotherapy remains a notable limitation of our work, yet we believe that our findings contribute to the general understanding of the association of sex and immunotherapy, and raise important questions for future research.
The role of sex as it pertains to immunotherapy response remains an important clinical question. The patient-level nature of our data allowed us to also do a head-to-head comparison of survival outcomes of females vs males receiving immunotherapy in addition to chemotherapy. We found that females in fact experienced improved survival with immunotherapy compared to males, after adjusting for potentially important clinical variables. This finding may be expected given that females experience better cancer outcomes overall than males [32]. Lung cancers of male and females are known to have distinctive clinical and biological differences, notably in terms of histology, driver mutations and smoking exposure history, [33, 34] all of which may impact immunotherapy efficacy. We would like to note, however, that the major aim this work is not demonstrate the value of chemoimmunotherapy treatment, generally or for specific subgroups, but instead to investigate how chemoimmunotherapy treatment efficacy may vary by sex and/or histology.
Conclusion
Immune checkpoint inhibitors and other immunotherapeutical approaches have revolutionized cancer treatment, and understanding which patients will be most likely to benefit from these treatments remains crucial to improving lung cancer outcomes. The study adds new data and should be regarded as an important contribution to the ongoing discussion on sex and immunotherapy treatment in NSCLC. How histology impacts sex*immunotherapy efficacy is a subject warranting future research.
The biological mechanisms whereby sex may impact immunotherapy benefit is an important scientific question, but one that may not be answerable when looking at NSCLC as a whole, and instead may require more specific subtype analysis in real-world, patient-level datasets.
Availability of data and materials
National Cancer Database (NCDB) data is available at no cost to members of the American College of Surgeons through an application process. A public access database may be made available in the near future. For more information: https://www.sgim.org/communities/research/dataset-compendium/national-cancer-database-ncdb.
Views expressed in this article do not communicate an official position of the NIH nor the American College of Surgeons.
References
Timeline of Progress in Immunotherapy - Cancer Research Institute (CRI) [Internet]. [cited 2020 Nov 10]. Available from: https://www.cancerresearch.org/immunotherapy/timeline-of-progress
Immune Checkpoint Inhibitors - National Cancer Institute [Internet]. 2019 [cited 2020 Nov 10]. Available from: https://www.cancer.gov/about-cancer/treatment/types/immunotherapy/checkpoint-inhibitors
Wojas-Krawczyk K, Kalinka E, Grenda A, Krawczyk P, Milanowski J. Beyond PD-L1 markers for lung Cancer immunotherapy. Int J Mol Sci. 2019;18:20(8).
Schiller JH, Harrington D, Belani CP, Langer C, Sandler A, Krook J, et al. Comparison of four chemotherapy regimens for advanced non–small-cell lung Cancer. N Engl J Med. 2002;346(2):92–8.
Chiang AC, Herbst RS. Frontline immunotherapy for NSCLC — the tale of the tail. Nat Rev Clin Oncol. 2020;17(2):73–4.
Kanwal B, Biswas S, Seminara RS, Jeet C. Immunotherapy in Advanced Non-small Cell Lung Cancer Patients: Ushering Chemotherapy Through the Checkpoint Inhibitors? Cureus [Internet];10(9). [cited 2019 May 6]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6217867/
Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016;16(10):626–38.
Zuk M. The Sicker Sex. PLoS Pathog. 2009;5(1):e1000267.
Klein SL, Jedlicka A, Pekosz A. The Xs and Y of immune responses to viral vaccines. Lancet Infect Dis. 2010;10(5):338–49.
Whitacre CC, Reingold SC, O’Looney PA. A gender gap in autoimmunity. Science. 1999;283(5406):1277–8.
Polanczyk MJ, Hopke C, Vandenbark AA, Offner H. Estrogen-mediated immunomodulation involves reduced activation of effector T cells, potentiation of Treg cells, and enhanced expression of the PD-1 costimulatory pathway. J Neurosci Res. 2006;84(2):370–8.
Conforti F, Pala L, Bagnardi V, Pas TD, Martinetti M, Viale G, et al. Cancer immunotherapy efficacy and patients’ sex: a systematic review and meta-analysis. Lancet Oncol. 2018;19(6):737–46.
Xiao D, Pan H, Li F, Wu K, Zhang X, He J. Analysis of ultra-deep targeted sequencing reveals mutation burden is associated with gender and clinical outcome in lung adenocarcinoma. Oncotarget. 2016;7(16):22857–64.
Conforti F, Pala L, Bagnardi V, Viale G, De Pas T, Pagan E, et al. Sex-based heterogeneity in response to lung cancer immunotherapy: a systematic review and meta-analysis. J Natl Cancer Inst. 2019;20:772–81.
Botticelli A, Onesti CE, Zizzari I, Cerbelli B, Sciattella P, Occhipinti M, et al. The sexist behaviour of immune checkpoint inhibitors in cancer therapy? Oncotarget. 2017;8(59):99336–46.
Langer CJ, Besse B, Gualberto A, Brambilla E, Soria J-C. The evolving role of histology in the management of advanced non-small-cell lung cancer. J Clin Oncol. 2010;28(36):5311–20.
National Cancer Database [Internet]. American College of Surgeons. [cited 2019 May 7]. Available from: https://www.facs.org/quality-programs/cancer/ncdb
Verma V, Haque W, Cushman TR, Lin C, Simone CB, Chang JY, et al. Racial and insurance-related disparities in delivery of immunotherapy-type compounds in the United States. J Immunother. 2019;42(2):55–64.
SEER*Rx Interactive Antineoplastic Drugs Database [Internet]. SEER. [cited 2019 May 20]. Available from: https://seer.cancer.gov/seertools/seerrx/#.
Green KM, Stuart EA. Examining moderation analyses in propensity score methods: application to depression and substance use. J Consult Clin Psychol. 2014;82(5):773–83.
Murphy B, Fraeman K. A General SAS® Macro to Implement Optimal N:1 Propensity Score Matching Within a Maximum Radius. :13.
A General SAS Macro to Implement Optimal N:1 Propensity Score Matching Within a Maximum Radius - PDF Free Download [Internet]. [cited 2022 Jan 16]. Available from: https://docplayer.net/54384962-A-general-sas-macro-to-implement-optimal-n-1-propensity-score-matching-within-a-maximum-radius.html.
Paz-Ares L, Vicente D, Tafreshi A, Robinson A, Soto Parra H, Mazières J, et al. A randomized, placebo-controlled trial of Pembrolizumab plus chemotherapy in patients with metastatic squamous NSCLC: protocol-specified final analysis of KEYNOTE-407. J Thorac Oncol. 2020;15(10):1657–69.
Wolchok JD, Hoos A, O’Day S, Weber JS, Hamid O, Lebbé C, et al. Guidelines for the evaluation of immune therapy activity in solid tumors: immune-related response criteria. Clin Cancer Res. 2009;15(23):7412–20.
Graeber C. The breakthrough: immunotherapy and the race to cure Cancer. 1st ed. New York: Twelve; 2018. p. 320.
Wakelee HA, Wang W, Schiller JH, Langer CJ, Sandler AB, Belani CP, et al. Survival differences by sex for patients with advanced non-small cell lung cancer on eastern cooperative oncology group trial 1594. J Thorac Oncol. 2006;1(5):441–6.
Korpanty GJ, Graham DM, Vincent MD, Leighl NB. Biomarkers That Currently Affect Clinical Practice in Lung Cancer: EGFR, ALK, MET, ROS-1, and KRAS. Front Oncol. 2014;4 [cited 2019 Dec 4]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4127527/.
Joshi A, Zanwar S, Noronha V, Patil VM, Chougule A, Kumar R, et al. EGFR mutation in squamous cell carcinoma of the lung: does it carry the same connotation as in adenocarcinomas? Onco Targets Ther. 2017;10:1859–63.
Khuder SA. Effect of cigarette smoking on major histological types of lung cancer: a meta-analysis. Lung Cancer. 2001;31(2–3):139–48.
Davis AA, Chae YK, Agte S, Pan A, Mohindra NA, Villaflor VM, et al. Association of tumor mutational burden with smoking and mutation status in non-small cell lung cancer (NSCLC). JCO. 2017;35(7_suppl):24.
Home - ClinicalTrials.gov [Internet]. [cited 2019 Dec 16]. Available from: https://clinicaltrials.gov/ct2/home
Cook MB, McGlynn KA, Devesa SS, Freedman ND, Anderson WF. Sex disparities in cancer mortality and survival. Cancer Epidemiol Biomark Prev. 2011;20(8):1629–37.
Patel JD, Bach PB, Kris MG. Lung cancer in US women: a contemporary epidemic. JAMA. 2004;291(14):1763–8.
Kiyohara C, Ohno Y. Sex differences in lung cancer susceptibility: a review. Gend Med. 2010;7(5):381–401.
Acknowledgements
Dr. Chi-fu Jeffrey Yang, Department of Surgery, Division of Thoracic Surgery, Massachusetts General Hospital, Boston, Massachusetts, is a participating investigator acknowledged for his role in data obtainment.
Authors’ information (optional)
Stephanie Tuminello is currently a PhD student at New York University School of Medicine.
Funding
This work was funded in part by NIH/NCI grant 5P30 CA196521–03; RV was partially supported by an internal grant KL02539874.
Author information
Authors and Affiliations
Contributions
Stephanie Tuminello, Rajwanth Veluswamy, Jorge E. Gomez, Raja Flores & Emanuela Taioli conceptualized the study design. Naomi Alpert and Arvind Kuman handled data acquisition, abstraction and cleaning. Stephanie Tuminello and Naomi Alpert conducted the statistical analysis. All authors played a role in results interpretation, manuscript preparation and revision, and have approved this final version of the manuscript. All authors agree to be held accountable for this work; Dr. Taioli, as the corresponding author, vouches for the integrity of this work from inception to publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was determined to be human subject research exempt by the institutional review board of Mount Sinai Hospital.
Consent for publication
Not Applicable.
Competing interests
Rajwanth Veluswamy has received consulting honorarium from Onconova Pharmaceuticals. All the other authors have no interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplemental Fig. 1.
Patient Selection. Supplemental Table 1. Drug agents classified as immunotherapy according to the NCDB.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tuminello, S., Alpert, N., Veluswamy, R.R. et al. Modulation of chemoimmunotherapy efficacy in non-small cell lung cancer by sex and histology: a real-world, patient-level analysis. BMC Cancer 22, 80 (2022). https://doi.org/10.1186/s12885-022-09187-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-022-09187-y