Abstract
Background
Window-of-opportunity trials, evaluating the engagement of drugs with their biological target in the time period between diagnosis and standard-of-care treatment, can help prioritise promising new systemic treatments for later-phase clinical trials. Renal cell carcinoma (RCC), the 7th commonest solid cancer in the UK, exhibits targets for multiple new systemic anti-cancer agents including DNA damage response inhibitors, agents targeting vascular pathways and immune checkpoint inhibitors. Here we present the trial protocol for the WIndow-of-opportunity clinical trial platform for evaluation of novel treatment strategies in REnal cell cancer (WIRE).
Methods
WIRE is a Phase II, multi-arm, multi-centre, non-randomised, proof-of-mechanism (single and combination investigational medicinal product [IMP]), platform trial using a Bayesian adaptive design. The Bayesian adaptive design leverages outcome information from initial participants during pre-specified interim analyses to determine and minimise the number of participants required to demonstrate efficacy or futility. Patients with biopsy-proven, surgically resectable, cT1b+, cN0–1, cM0–1 clear cell RCC and no contraindications to the IMPs are eligible to participate. Participants undergo diagnostic staging CT and renal mass biopsy followed by treatment in one of the treatment arms for at least 14 days. Initially, the trial includes five treatment arms with cediranib, cediranib + olaparib, olaparib, durvalumab and durvalumab + olaparib. Participants undergo a multiparametric MRI before and after treatment. Vascularised and de-vascularised tissue is collected at surgery. A ≥ 30% increase in CD8+ T-cells on immunohistochemistry between the screening and nephrectomy is the primary endpoint for durvalumab-containing arms. Meanwhile, a reduction in tumour vascular permeability measured by Ktrans on dynamic contrast-enhanced MRI by ≥30% is the primary endpoint for other arms. Secondary outcomes include adverse events and tumour size change. Exploratory outcomes include biomarkers of drug mechanism and treatment effects in blood, urine, tissue and imaging.
Discussion
WIRE is the first trial using a window-of-opportunity design to demonstrate pharmacological activity of novel single and combination treatments in RCC in the pre-surgical space. It will provide rationale for prioritising promising treatments for later phase trials and support the development of new biomarkers of treatment effect with its extensive translational agenda.
Trial registration
ClinicalTrials.gov: NCT03741426 / EudraCT: 2018–003056-21.
Similar content being viewed by others
Background
Renal cell carcinoma (RCC) is the 12th commonest solid cancer globally (> 400,000 cases/year) and the 7th commonest in the United Kingdom (~ 14,000 cases/year) [1]. Clear cell RCC (ccRCC), is the commonest histological subtype found in 75–80% of patients with RCC, and presents with metastatic disease in 16% of patients [2, 3].
Surgery is the treatment of choice in medically-fit patients whose disease burden is amenable to resection [4]. Consequently, 56% of patients undergo partial or radical resection of the tumour-bearing kidney as part of their treatment [5]. Currently guidelines recommend no peri-operative treatment in patients undergoing surgery with curative intent; however, 30% of patients will experience recurrence [6, 7]. For patients whose disease is not amenable to surgery, first-line treatment options for medically fit patients consist of immune-checkpoint inhibitors and/or vascular endothelial growth factor (VEGF) tyrosine kinase inhibitors (TKIs) [8, 9].
The increasing number of possible single-agent and combination therapeutic options makes it very challenging to prioritise agents in combination for further development in large randomised clinical trials. Therefore, novel trial designs, such as this window-of-opportunity trial assessing promising new combination treatments in the period of time between diagnosis and surgery, are required to determine if the combination results in the hypothesised mechanistic pharmacology [10]. A further advantage of the window-of-opportunity design allows assessing the biological activity of drugs in treatment naïve patients and ensures that translational analyses are not biased by previous treatments [10]. In the United Kingdom, Canada and the United States, patients often wait 1 month or more between the decision to proceed with nephrectomy and their surgery [11,12,13], making a window-of-opportunity trial design appropriate for the clinical pathway.
Genomic instability is a hallmark of cancer which chemo- and radiotherapy exploit while causing significant collateral damage to normal tissues [14]. More recently, targeted DNA damage response inhibitors (DDRi) and immune checkpoint inhibitors have taken advantage of tumour genomic instability and the resulting high mutational burden resulting in higher tumour specificity and efficacy in a range of different tumour types [15,16,17]. DDRi cause synthetic lethality in cells genetically lacking specific DNA repair mechanisms [18]. In contrast to this, contextual synthetic lethality occurs synergistically between a pharmacological DDRi and a second agent [19]. While ccRCC is not commonly associated with DDR deficiency, recent in-vitro and in-vivo data demonstrating replication stress as a consequence of common mutations associated with RCC (VHL loss: 85% of ccRCC, SETD2 mutations: 12% of ccRCC) and VEGF inhibition suggest that DDR-targeted treatment may be an effective and relevant therapeutic strategy [20, 21]. The initial arms of the WIndow-of-opportunity clinical trial platform for evaluation of novel treatment strategies in REnal cell cancer (WIRE) will evaluate the pharmacological activity of DDRi (Olaparib) alone and in combination with drug classes well established to be active in ccRCC including TKIs (cediranib) and immune checkpoint inhibitors (durvalumab), in patients with surgically resectable ccRCC.
Olaparib inhibits poly (ADP-ribose) polymerases (PARP 1–3) which are central to DNA damage repair and genomic stability. It inhibits the repair of single-strand DNA breaks specifically in cells deficient in homologous recombination, resulting in double strand-breaks, subsequent accumulation of mutations and cell death [22]. Olaparib has demonstrated improved progression-free survival (PFS) in placebo-controlled phase III studies in BRCA-mutated ovarian cancer [23, 24] and prolonged PFS in a phase III trial of patients with human epidermal growth factor receptor 2 (HER2)-negative breast cancer with a germline BRCA1/2 mutation compared to standard-of-care treatment [16]. In patients with metastatic prostate cancer and deleterious alterations in genes involved in homologous recombination repair, olaparib conferred prolonged overall survival (OS) and PFS compared to abiraterone or enzalutamide [25]. Meanwhile, cediranib, a potent VEGF-A and VEGFR-2 inhibitor causing a significant and rapid reduction in tumour blood-flow measured by dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI), has demonstrated activity against ccRCC among other cancer types [26,27,28]. Cediranib in combination with olaparib improved PFS in ovarian cancer [29]. Given the replication stress induced by VEGF inhibition, the combination of cediranib + olaparib was prioritized as a potential therapeutic strategy for this platform trial [20, 21]. Finally, the immune checkpoint inhibitor durvalumab prolonged OS in patients with non-small cell lung cancer undergoing chemoradiotherapy in a placebo-controlled phase III trial [30]. The established efficacy of PD1/PD-L1 inhibitors in metastatic RCC [31, 32], coupled with increased anti-tumour activity of immune checkpoint inhibitors in combination with DDRi, owing to the increased expression of PD-L1 and activation of the stimulator of interferon genes (STING) pathway observed pre-clinically, rationalises this combination treatment [33, 34]. Here we present the trial protocol for the WIRE trial platform evaluating these novel treatment strategies in renal cancer and describe associated translational analyses.
Methods/design
Objectives
Primary objective
The WIRE trial aims to determine proof-of-mechanism for several agents (cediranib, olaparib and durvalumab) used as single or combination therapies by demonstrating engagement with the expected cellular pathways. Changes in capillary permeability will be determined in the cediranib, olaparib and cediranib + olaparib arms and changes to intra-tumoral CD8+ T-cell infiltration will be determined in the durvalumab and durvalumab + olaparib arms.
Secondary objectives
Secondary objectives will aim to investigate the safety of the investigational medicinal products (IMP) in the preoperative period and determine changes in primary tumour size and overall response measured according to the Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1 [35]. Where they are not primary objectives, changes in intratumoral CD8+ T-cells and capillary permeability will be assessed as secondary objectives.
Exploratory objectives
Exploratory objectives will aim to define the molecular biological response to the IMPs for candidate markers of biological effects in blood, urine, and tissue samples. Additionally, the relationship of the primary endpoints with genetic mutations in related genes will be investigated. Finally, the ability of automated histological image analysis and hyperpolarised [1-13C] pyruvate MRI imaging to detect biological treatment response will be explored.
Trial design and participants
WIRE is a Phase II, multi-arm, multi-centre, non-randomised, proof-of-mechanism (single and combination IMPs), platform trial using a Bayesian adaptive design (ClinicalTrials.gov Identifier: NCT03741426) with sample size chosen to control frequentist statistical characteristics. It will be conducted at academic medical centres in the United Kingdom.
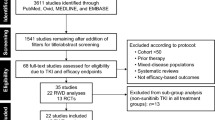
The Bayesian adaptive design leverages outcome information from initial participants to determine the recruitment target for each treatment arm (see Fig. 1). After reaching the recruitment target of six participants into single agent and ten participants into combination treatment arms in the initial stage, recruitment will continue into subsequent arms until the interim analysis is complete. Depending on the number of patients achieving the primary endpoint during these pre-planned interim analyses, the independent data monitoring committee (IDMC) may close the arm for reaching statistical efficacy or futility. If recruiting additional participants is likely to confer statistical efficacy, additional patients will be recruited into an arm until the target for the second interim analysis is reached. Each arm may proceed through up to three recruitment stages.
Potential participants will be identified during multi-disciplinary team case discussions and invited to participate in the trial during their standard clinical care visit. Participants will be provisionally assigned to the currently recruiting arm and provided a screening identifier. Upon successfully completing screening, participants will be allocated a trial identifier and continue with the arm allocated at screening. Participants may not cross to another arm or enter a reserve pool if they are ineligible for the current arm.
Eligibility criteria
Key inclusion criteria include age ≥ 18 years, biopsy-proven, surgically resectable, cT1b+, cN0–1, cM0–1 ccRCC, Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1, at least one measurable lesion according to RECIST 1.1, adequate organ and bone marrow function and contraception. Patients may not have been exposed to any PARP, tyrosine kinase, immune checkpoint or mammalian target of rapamycin (mTOR) inhibitors.
Key exclusion criteria include cT1a, N0, M0 ccRCC, brain metastasis, spinal cord compression unless definitely treated and non-progressive for 28 days and leptomeningeal involvement. Furthermore, patients with a bodyweight ≤30 kg, contraindication for any of the trial compounds, other invasive malignancy within the last 2 years, concurrent participation in another interventional clinical trial, cardio- or cerebrovascular complications within the last 12 months, immunosuppression or active infection, pregnancy or contraindications for MRI are excluded from participation. Women of childbearing potential must use two highly effective forms of contraception from consent until 3 months after the end of the trial.
Detailed reference values for adequate organ and bone marrow function as well as in- and exclusion criteria specific to individual treatment arms can be found in the Additional file 2.
Informed consent
A trial entrant will provide written informed consent before any trial-specific intervention in accordance with the principles of the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use – Good Clinical Practice (IHC-GCP) [36]. Translation of the patient information and consent form will be provided if necessary and trial entrants will have at least 24 h to consider the patient information materials. Additional consent for the collection of blood, urine and tissue samples as well as genetic analyses will be sought. Consent documents are available in the Additional file 3.
Interventions
Intervention description
This trial includes five sequential treatment arms: 1) cediranib; 2) cediranib + olaparib; 3) olaparib; 4) durvalumab and 5) olaparib + durvalumab. IMPs for the individual arms are summarized in Table 1.
Regardless of the treatment arm, patients will undergo nephrectomy between 17 and 28 days after the first day of IMP (Fig. 1).
Criteria for discontinuing or modifying allocated interventions
In the case of toxicity, oral IMPs may be interrupted and can be dose-reduced as detailed in Table 1. If the toxicity persists, the IMP should be discontinued. In the combination arms, the doses of cediranib and olaparib will both be reduced unless the toxicity can be attributed to the toxicity profile of one of the IMPs. In case of discontinuation, both IMPs will be discontinued.
Participants will have their IMP discontinued if they experience unacceptable toxicity despite dose reductions, disease progression per RECIST 1.1, pregnancy, weight loss to ≤30 kg or withdraw consent. Participants receiving olaparib will have their IMP discontinued if they develop myelodysplastic syndrome or acute myeloid leukemia.
Relevant concomitant care permitted or prohibited during the trial
All routinely used supportive care will be allowed during WIRE, except for certain medications prohibited and restricted for safety or efficacy reasons. These are detailed in the Additional file 2.
Participant timeline
Figure 2 summarises the participant timelines for all arms.
Outcomes
Primary outcomes
Reduction in tumour vascular permeability by > 30% measured by median Ktrans on DCE-MRI between the baseline and pre-surgical MRI will be the primary endpoint for the cediranib, olaparib and cediranib + olaparib treatment arms. Ktrans is a sensitive and early marker of response to VEGFR TKI in renal cancer and to olaparib in ovarian cancer [37, 38]. Additionally, pre-clinical research has demonstrated that the impaired vascular endothelial cell migration resulting from PARP inhibition has an anti-angiogenic effect [39]. The primary endpoint for the durvalumab containing arms will be an increase in CD8+ T-cells on immunohistochemistry (IHC) assessed by histoscore between the baseline biopsy and samples taken at nephrectomy. The rationale for this endpoint is based on evidence in melanoma that an increased number of tumour infiltrating CD8+ T-cells is associated with a better response to immune checkpoint inhibitors [40, 41].
Secondary outcomes
-
Adverse events assessed according to the Common Terminology Criteria for Adverse Events (CTCAE) Toxicity Criteria (Version 5.0)
-
Tumour size change between pre- and post-treatment MRI
-
Tumour response according to RECIST v1.1 on pre- and post-treatment MRI in participants with M0 disease and pre-and post-treatment contrast-enhanced CT in participants with M1 disease
-
Changes in Ktrans and tumour infiltrating CD8+ T-cells where these are not primary outcomes
Exploratory outcomes
Exploratory outcomes will include the assessment of blood, urine, tissue and imaging-based biomarkers of drug mechanism and treatment response.
Data collection and management
Assessment and collection of outcomes
Primary endpoints will be assessed centrally for all trial sites when the number of participants required for an interim or final analysis has been reached.
All pseudo-anonymised imaging data will be transferred to the trial radiologist for the measurement of the tissue transfer constant Ktrans on DCE-MRI. Following motion correction, the MiStar software (Apollo Medical, Melbourne, Australia) will be used for kinetic modelling of the contrast-enhancement data using the extended Tofts model [42] and a model arterial input function [43]. Regions of interest encompassing the entire tumour will be defined and independently reviewed by two radiologists. Two radiologists verify the correct recording of the median Ktrans value independently.
The CD8+ T-cell count will be established centrally following transfer of the formalin-fixed paraffin-embedded tissue blocks. Following slicing of the block, endogenous peroxidase suppression and heat-mediated antigen retrieval, the mouse monoclonal anti-human CD8 (DAKO Cytomation, Glostrup, Denmark, 1:100 dilution) will be the primary antibody. Slides will be scanned and two board-certified uro-pathologists will quantify the CD8+ T-cells in ten random fields of view per tumour sample, expressed as the median number of cells/mm2 before and after treatment.
Participant replacement
Participants will be replaced and not evaluated for the primary endpoint if they have not received at least 14 days of IMP and/or a single infusion of durvalumab, had to interrupt the IMP for > 7 consecutive days, had a compliance rate of < 70% in the 7 days preceding the pre-surgical imaging, had no pre-surgical imaging or had surgery more than 28 days after the first day of IMP.
Data management and confidentiality
All trial-related information will be stored securely at the trial site and transferred pseudo-anonymised through an encrypted electronic case report form (eCRF). The eCRF has inbuilt mechanisms to validate the integrity of data entries. Data will be checked for clarity, errors and completeness ahead of data export by two independent staff members. A pseudo-anonymised copy of imaging data used to obtain the primary endpoint will be retained centrally.
Collection, evaluation and storage of biological specimens and translational analyses
During screening, patients will undergo urine and blood collection followed by ultrasound-guided, multi-regional biopsy of the renal tumour. The biopsy procedure will be carried out by a consultant interventional radiologist. Additional blood and urine samples will be collected after 14 days of IMP and immediately before surgery. At surgery, samples will be collected from the vascularized (i.e. during the nephrectomy) and devascularised (i.e. ex vivo) tumour. 3D-printed, patient-specific tumour moulds will be used to collect devascularised samples from locations spatially registered to pre-surgical imaging at one of the trial sites. If lesions have a major axis > 20 cm, biopsies will be taken without the mould. All trial samples will be stored and analysed in a pseudo-anonymised manner.
The translational analysis aims to explore potential future endpoint markers and determine the response of molecular markers in DDR-, immune-, apoptosis- and cell-cycle pathways.
DNA and RNA analyses in tissue, blood and urine will attempt to explore signatures of response and resistance to IMPs and confirm the IMP’s mechanism of action. Additionally, intratumor genetic heterogeneity will be assessed from multi-regional tumour biopsies and compared to the genetic landscape observed in cell-free tumour DNA. Furthermore, WIRE aims to investigate the applicability of the NEAT (N-cadherin, EPCAM, Age, mTOR) proteomic score [44], which was developed for survival prediction in patients receiving sunitinib, in the IMPs under investigation, including the TKI cediranib. WIRE can explore immune- and cytokine-based signatures in peripheral blood mononucleocytes (PBMCs), plasma or urine which may predict response, resistance, or toxicity. These will be complemented by metabolomics analyses using mass-spectrometry and nuclear magnetic resonance on matched biopsy and surgical tumour tissue pairs, plasma, and urine. Finally, translational research within WIRE aims to address the unmet need for new in-vivo and in-vitro models of RCC, generating reproducible patient-derived xenograft (PDX) and cell line models to support the rational design of future therapies.
Statistical methods
Sample size and power
Up to a maximum of 76 evaluable participants will be recruited into the initial five arms and across all stages.
Monotherapy arms (Arm 1 [Cediranib], Arm 3 [Olaparib], Arm 4 [Durvalumab])
Each monotherapy arm will enrol a maximum of 12 evaluable participants with interim analyses after 6 and 9 evaluable participants have primary outcome data available.
The null hypothesis is 20% or less of participants show a response on the primary outcome. The alternative hypothesis is that more than 20% of participants show a response:H0: p ≤ 0.2 H1: p > 0.2with the power calculated as the probability of rejecting H0 when p = 0.5.
The IMP will be recommended as promising (null hypothesis rejected) if the arm stops after stage 1 or 2 for efficacy (see Interim Analyses). If the IMP continues to stage 3, a p-value will be found by calculating the tail probability of seeing that many or more responses if the distribution were binomial with p = 0.2. The treatment will be recommended as promising if the p-value is ≤0.1.
The overall type I error rate for monotherapy arms is 20%; the overall power is 92% when p = 0.5. The ‘overall type I error rate’ for an arm is defined as the probability of an inefficacious arm (p < =0.2) having its null hypothesis rejected. This is the sum of the probabilities of meeting an efficacy stopping rule after stage 1 or 2 and reaching the final analysis and having a final p-value of ≤0.1. The overall power is this sum of probabilities when the arm is efficacious (p = 0.5).
Although 20% type I error rate is higher than traditional in phase II, each monotherapy is tested again within the combination IMP arms.
Each combination arm will enrol a maximum of 20 evaluable participants with interim analyses after 10 and 15 evaluable participants have primary outcome data available
The null hypothesis is 30% or less of participants show a response on the primary outcome. The alternative hypothesis is that more than 30% of participants show a response:
-
H0: p ≤ 0.3
-
H1: p > 0.3
with the power calculated as the probability of rejecting H0 when p = 0.6.
The combination will be recommended as promising (null hypothesis rejected) if the arm stops after stage 1 or 2 for efficacy (see Interim Analyses). If the combination continues to stage 3, a p-value will be found by calculating the tail probability of seeing that many or more responses if the distribution were binomial with p = 0.3. The IMP will be recommended as promising if the p-value is ≤0.05.
The overall type I error rate for combination IMP arms is 10%; the overall power is 93% when p = 0.6.
Simulation code in R to recreate the statistical properties is provided as Additional file 1.
Interim analyses
Interim data analyses at predefined points will decide whether the recruitment of additional patients into an arm should occur. The Bayesian analysis will use a Beta (0.3, 0.7) prior for the biological response rate (the p parameter). Through updating this prior with the observed number of biological responders using a Beta-Binomial conjugate distribution we will calculate a Beta posterior distribution p.
For monotherapy arms, if the calculated posterior probability of the biological response rate being above 0.2 is above 98%, the arm will be closed early for efficacy. If the predictive probability that the IMP would be found to be promising (i.e. the final one-sided p-value would be ≤0.1) if the full enrolment of 12 was reached is < 2%, then the arm will be closed early for futility. This use of the posterior distribution for efficacy stopping and predictive distribution for futility stopping is as recommended by Berry et al. [45].
For combination IMP arms, if the calculated posterior probability of the biological response rate being above 0.3 is above 98%, the arm will be closed early for efficacy. If the predictive probability that the IMP would be found to be promising (i.e. the final one-sided p-value would be ≤0.05) if the full enrolment of 20 was reached is < 2%, then the arm will be closed early for futility.
The final p-value thresholds are chosen to control the overall type I error rate at 20% for monotherapy arms and 10% for combination arms.
We note that the efficacy stopping rule is provided as a recommendation to the IDMC (see Additional file 2). The IDMC may decide that continuing to recruit participants to an arm that meets the efficacy stopping rules is warranted. If this occurs, then the type I error rate and power will both be lower than the aforementioned levels.
The recruitment targets for the interim analyses are summarised in Fig. 1. No subgroup analysis beyond the treatment arms is planned for this trial.
Statistical methods for primary and secondary outcomes and missing data
A Statistical Analysis Plan (SAP) will define appropriate 95% two-sided Confidence Intervals for primary and secondary endpoint quantities prior to the first interim analysis. The extent of missing data will be reported however no imputation of missing data is planned.
Plans to give access to the full protocol, participant level-data and statistical code
The full protocol and participant level-data will not be made available. A more detailed description of the development of the Bayesian adaptive statistics used in the design of this trial will be available in an independent publication. Statistical code will be made available upon reasonable request.
Oversight and monitoring
Adverse event reporting and harms
Adverse events will be monitored and recorded from the time of consent until 90 days after the last administration of IMP. Any adverse event will be recorded in the patient notes and the eCRF. The principal investigators will report serious adverse events (SAEs) to the chief investigator within 24 h of awareness. The chief investigator will subsequently assess SAEs for expectedness and relatedness prior to onwards notification to the sponsor within a further 24 h. The chief investigator will additionally report SAEs to AstraZeneca within 24 h. The CI must report suspected unexpected serious adverse reactions (SUSARs) to the Medicines and Healthcare products Regulatory Agency (MHRA) and the ethics committee within 7 to 15 days depending on the severity. Reporting of SAEs which are attributable to any of the IMPs (i.e. serious adverse reactions) and SUSARs continues beyond the 90-day monitoring period and after withdrawal of consent by the participant, where investigators become aware of any new events.
More details on trial oversight are available in the Additional file 2.
Dissemination plans
The clinical and exploratory endpoints are anticipated to be of great interest to the RCC research community due to the novel combinations being used. The results will be reported at major oncology conferences and then published in high-impact journals. Patient facing publications will be made available to interested trial participants and via our website.
Discussion
Here we present an adaptive and expandable phase II clinical trial platform to demonstrate proof-of-mechanism for single-agent and combination treatments in ccRCC.
The Bayesian statistics-based adaptive trial design optimises the number of trial participants in each arm, ensuring that no more participants than necessary are recruited to demonstrate proof of mechanism or futility of any arm [45]. This accelerates the screening of agents and combinations. Also, the Bayesian framework allows adjusting for the uncertainty arising from the unknown variability of emerging endpoints in the context of new treatments. In addition to prioritising promising treatment arms for later phase clinical trials, the extensive liquid and tumour bio-sampling and use of advanced imaging support the identification of new biomarkers of response, which are an area of unmet clinical need in RCC. The platform design of the trial also allows learning from and defining new endpoints based on accumulating study data. We have previously shown the benefit of using imaging biomarkers as part of an adaptive trial design protocol in the assessment of patients with RCC in the metastatic setting [46].
The window-of-opportunity design of this trial exposes patients to the trial medication for a brief period, prior to standard-of-care nephrectomy. While this will allow measuring the engagement of IMPs with their biological target, this trial is neither designed nor powered to accrue evidence of long-term treatment benefit, although there may be unmeasurable survival advantages for patients. Therefore, larger studies in patients who are not surgical candidates will be required to investigate survival benefits of promising treatment arms. Furthermore, the brief treatment may lead to an underestimation of the treatment effects.
A limitation inherent to the window-of-opportunity design is the risk of delaying standard-of-care treatment when serious adverse reactions occur. This risk is mitigated by the strict inclusion criteria, close oncology supervision to pre-empt and identify early any significant toxicity events, and the Bayesian adaptive trial design which leverages information gained during interim analyses to reduce the number of participants compared to conventional trial designs. This is also an advantage compared to other, slowly accruing window-of-opportunity trials. The risk of delaying surgery is discussed with potential participants in detail. On the other hand, an advantage of the window-of-opportunity design is that it increases the possibility to detect biological treatment effects quickly and in a small number of patients. Specifically, examining previously untreated patients who will undergo standard-of-care nephrectomy allows the investigation of IMPs in the absence of mutations induced by previous treatment(s) as well as access to tissue at surgery for extensive translational analyses.
This is the first clinical trial we are aware of using this pre-surgical window-of-opportunity to investigate novel agents and combination therapies in RCC with a Bayesian design. In the future, additional treatment arms may be added to this trial. In addition to studying new systemic anti-cancer agents, synergistic effects between radiation therapy localised to the tumour and DDR inhibition could be investigated.
In summary, WIRE will provide an important impetus for future phase II/III clinical trials to prioritise treatment regimens that show biological efficacy. Additionally, it will be able to inform the optimal choice of treatment response biomarkers.
Trial status
Version 3.0 of the trial protocol (05/12/2019) has received ethical approval and is in date as of publication of this trial protocol. Recruitment for WIRE commenced on the 12/08/2020 and is estimated to be completed in 12/2022.
Availability of data and materials
Not applicable.
Abbreviations
- ccRCC:
-
Clear cell Renal Cell Carcinoma
- DCE-MRI:
-
Dynamic Contrast Enhanced Magnetic Resonance Imaging
- DDRi:
-
DNA Damage Response inhibitor
- eCRF:
-
Electronic Case Report Form
- ECOG:
-
Eastern Cooperative Oncology Group
- IDMC:
-
Independent Data Monitoring Committee
- IHC:
-
Immuno Histochemistry
- IMP:
-
Investigational Medicinal Product
- OS:
-
Overall survival
- PARP:
-
Poly (ADP-Ribose) Polymerase
- PFS:
-
Progression-Free Survival
- RECIST:
-
Recponse Criteria in Solid Tumours
- SAE:
-
Serious Adverse Event
- SUSAR:
-
Suspected Unexpected Serious Adverse Reaction
- TKI:
-
Tyrosine Kinase Inhibitor
- VEGF(R):
-
Vascular Endothelial Growth Factor (Receptor)
References
Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, et al. Global Cancer Observatory: Cancer Today. Int Agency Res Cancer. 2018; [cited 2020 Mar 23]. Available from: https://gco.iarc.fr/today/home.
Cheville JC, Lohse CM, Zincke H, Weaver AL, Blute ML. Comparisons of outcome and prognostic features among histologic subtypes of renal cell carcinoma. Am J Surg Pathol. 2003;27(5):612–24. https://doi.org/10.1097/00000478-200305000-00005.
Howlader N, Noone A, Krapcho M, Miller D, Brest A, Yu M, et al. SEER Cancer Statistics Review, 1975–2017: Kidney and Renal Pelvis Cancer — Cancer Stat Facts. Bethesda: National Cancer Institute; 2020. [cited 2020 Aug 5]. Available from: https://seer.cancer.gov/statfacts/html/kidrp.html
Campbell S, Uzzo RG, Allaf ME, Bass EB, Cadeddu JA, Chang A, et al. Renal mass and localized renal Cancer: AUA guideline. J Urol. 2017;198(3):520–9. https://doi.org/10.1016/j.juro.2017.04.100.
National Cancer Registration and Analysis Service Public Health England. Chemotherapy, Radiotherapy and Surgical Tumour Resections in England 2013–2016. 2020 [cited 2020 Sep 10]. Available from: https://www.cancerdata.nhs.uk/treatments
Ljungberg B, Albiges L, Abu-Ghanem Y, Bensalah K, Dabestani S, Montes SFP, et al. European Association of Urology Guidelines on Renal Cell Carcinoma: The 2019 Update. Eur Urol. 2019;75(5):799–810 [cited 2021 Feb 12]. Available from: https://pubmed.ncbi.nlm.nih.gov/30803729/.
Rini BI, Campbell SC, Escudier B. Renal cell carcinoma. Lancet. 2009;373(9669):1119–32. https://doi.org/10.1016/S0140-6736(09)60229-4.
Motzer RJ, Penkov K, Haanen J, Rini B, Albiges L, Campbell MT, et al. Avelumab plus axitinib versus sunitinib for advanced renal-cell carcinoma. N Engl J Med. 2019;380(12):1103–15. https://doi.org/10.1056/NEJMoa1816047.
ESMO Guidelines Committee. eUpdate – Renal Cell Carcinoma Treatment Recommendations | ESMO. [cited 2018 Jun 13]. Available from: http://www.esmo.org/Guidelines/Genitourinary-Cancers/Renal-Cell-Carcinoma/eUpdate-Renal-Cell-Carcinoma-Treatment-Recommendations
Glimelius B, Lahn M. Window-of-opportunity trials to evaluate clinical activity of new molecular entities in oncology. Ann Oncol. 2011;22(8):1717–25. https://doi.org/10.1093/annonc/mdq622.
Subramonian KR, Puranik S, Mufti GR. How will the two-weeks-wait rule affect delays in management of urological cancers? J R Soc Med. 2003;96(8):398–9. https://doi.org/10.1177/014107680309600809.
Stec AA, Coons BJ, Chang SS, Cookson MS, Herrell SD, Smith JA, et al. Waiting time from initial urological consultation to nephrectomy for renal cell carcinoma-does it affect survival? J Urol. 2008;179(6):2152–7. https://doi.org/10.1016/j.juro.2008.01.111.
Shiff B, Breau R, Patel P, Kapoor A, Pouliot F, So A, et al. Impact of time-to-surgery and surgical delay on oncologic outcomes for renal cell carcinoma. J Urol. 2019;201(1):78-85. https://doi.org/10.1097/JU.0000000000001230.
Chen Y, Jungsuwadee P, Vore M, Butterfield DA, St. Clair DK. Collateral damage in cancer chemotherapy: oxidative stress in nontargeted tissues. Mol Interv. 2007;7(3):147–56. https://doi.org/10.1124/mi.7.3.6.
Golan T, Hammel P, Reni M, Van Cutsem E, Macarulla T, Hall MJ, et al. Maintenance olaparib for germline BRCA-mutated metastatic pancreatic cancer. N Engl J Med. 2019;381(4):317–27. https://doi.org/10.1056/NEJMoa1903387.
Robson M, Im S-A, Senkus E, Xu B, Domchek SM, Masuda N, et al. Olaparib for metastatic breast Cancer in patients with a germline BRCA mutation. N Engl J Med. 2017;377(6):523–33. https://doi.org/10.1056/NEJMoa1706450.
Ledermann J, Harter P, Gourley C, Friedlander M, Vergote I, Rustin G, et al. Olaparib maintenance therapy in platinum-sensitive relapsed ovarian Cancer. N Engl J Med. 2012;366(15):1382–92. https://doi.org/10.1056/NEJMoa1105535.
Lord CJ, Ashworth A. PARP inhibitors: Synthetic lethality in the clinic. Science (80- ). 2017;355(6330):1152–8.
Nowsheen S, Cooper T, Stanley JA, Yang ES. Synthetic Lethal Interactions between EGFR and PARP Inhibition in Human Triple Negative Breast Cancer Cells. PLoS One. 2012;7(10):e46614.
Espana-Agusti J, Warren A, Chew SK, Adams DJ, Matakidou A. Loss of PBRM1 rescues VHL dependent replication stress to promote renal carcinogenesis. Nat Commun. 2017;8(1):1–11. https://doi.org/10.1038/s41467-017-02245-1.
Kanu N, Grönroos E, Martinez P, Burrell RA, Yi Goh X, Bartkova J, et al. SETD2 loss-of-function promotes renal cancer branched evolution through replication stress and impaired DNA repair. Oncogene. 2015;34(46):5699–708. https://doi.org/10.1038/onc.2015.24.
Helleday T. The underlying mechanism for the PARP and BRCA synthetic lethality: clearing up the misunderstandings. Mol Oncol. 2011;5(4):387–93. https://doi.org/10.1016/j.molonc.2011.07.001.
Moore K, Colombo N, Scambia G, Kim B-G, Oaknin A, Friedlander M, et al. Maintenance Olaparib in patients with newly diagnosed advanced ovarian Cancer. N Engl J Med. 2018;379(26):2495–505. https://doi.org/10.1056/NEJMoa1810858.
Pujade-Lauraine E, Ledermann JA, Selle F, Gebski V, Penson RT, Oza AM, et al. Olaparib tablets as maintenance therapy in patients with platinum-sensitive, relapsed ovarian cancer and a BRCA1/2 mutation (SOLO2/ENGOT-Ov21): a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Oncol. 2017;18(9):1274–84. https://doi.org/10.1016/S1470-2045(17)30469-2.
Hussain M, Mateo J, Fizazi K, Saad F, Shore N, Sandhu S, et al. Survival with Olaparib in metastatic castration-resistant prostate Cancer. N Engl J Med. 2020;383(24):2345–57. https://doi.org/10.1056/NEJMoa2022485.
Messiou C, Orton M, Ang JE, Collins DJ, Morgan VA, Mears D, et al. Advanced solid tumors treated with Cediranib: comparison of dynamic contrast-enhanced MR imaging and CT as markers of vascular activity. Radiology. 2012;265(2):426–36. https://doi.org/10.1148/radiol.12112565.
Mulders P, Hawkins R, Nathan P, De Jong I, Osanto S, Porfiri E, et al. Cediranib monotherapy in patients with advanced renal cell carcinoma: results of a randomised phase II study. Eur J Cancer. 2012;48(4):527–37. https://doi.org/10.1016/j.ejca.2011.12.022.
Powles T, Brown J, Larkin J, Jones R, Ralph C, Hawkins R, et al. A randomized, double-blind phase II study evaluating cediranib versus cediranib and saracatinib in patients with relapsed metastatic clear-cell renal cancer (COSAK). Ann Oncol. 2016;27(5):880–6. https://doi.org/10.1093/annonc/mdw014.
Liu JF, Barry WT, Birrer M, Lee JM, Buckanovich RJ, Fleming GF, et al. Combination cediranib and olaparib versus olaparib alone for women with recurrent platinum-sensitive ovarian cancer: a randomised phase 2 study. Lancet Oncol. 2014;15(11):1207–14. https://doi.org/10.1016/S1470-2045(14)70391-2.
Antonia SJ, Villegas A, Daniel D, Vicente D, Murakami S, Hui R, et al. Overall survival with durvalumab after chemoradiotherapy in stage III NSCLC. N Engl J Med. 2018;379(24):2342–50. https://doi.org/10.1056/NEJMoa1809697.
Motzer RJ, Tannir NM, McDermott DF, Arén Frontera O, Melichar B, Choueiri TK, et al. Nivolumab plus Ipilimumab versus Sunitinib in advanced renal-cell carcinoma. N Engl J Med. 2018;378(14):1277–90. https://doi.org/10.1056/NEJMoa1712126.
Motzer RJ, Escudier B, McDermott DF, George S, Hammers HJ, Srinivas S, et al. Nivolumab versus Everolimus in advanced renal-cell carcinoma. N Engl J Med. 2015;373(19):1803–13. https://doi.org/10.1056/NEJMoa1510665.
Shen J, Zhao W, Ju Z, Wang L, Peng Y, Labrie M, et al. PARPI triggers the STING-dependent immune response and enhances the therapeutic efficacy of immune checkpoint blockade independent of BRCANEss. Cancer Res. 2019;79(2):311–9. https://doi.org/10.1158/0008-5472.CAN-18-1003.
Jiao S, Xia W, Yamaguchi H, Wei Y, Chen MK, Hsu JM, et al. PARP inhibitor upregulates PD-L1 expression and enhances cancer-associated immunosuppression. Clin Cancer Res. 2017;23(14):3711–20. https://doi.org/10.1158/1078-0432.CCR-16-3215.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47. https://doi.org/10.1016/j.ejca.2008.10.026.
ICH GCP - ICH harmonised guideline integrated addendum to ICH E6(R1): Guideline for Good Clinical Practice ICH E6(R2) ICH Consensus Guideline - ICH GCP [Internet]. 2016 [cited 2021 Feb 15]. Available from: https://ichgcp.net/
Welsh S, Fife K, Matakidou A, Mullin J, Machin A, Qian W, et al. A phase II clinical study evaluating the efficacy and safety of neoadjuvant and adjuvant sunitinib in previously untreated patients with metastatic renal cell carcinoma. J Clin Oncol. 2017;35(15):16087. https://doi.org/10.1200/JCO.2017.35.15_suppl.e16087.
Lee JM, Trepel JB, Choyke P, Cao L, Sissung T, Houston N, et al. CECs and IL-8 have prognostic and predictive utility in patients with recurrent platinum-sensitive ovarian cancer: biomarker correlates from the randomized phase-2 trial of olaparib and cediranib compared with olaparib in recurrent platinum-sensitive Ovar. Front Oncol. 2015;5. https://doi.org/10.3389/fonc.2015.00123.
Tentori L, Lacal PM, Muzi A, Dorio AS, Leonetti C, Scarsella M, et al. Poly (ADP-ribose) polymerase (PARP) inhibition or PARP-1 gene deletion reduces angiogenesis. Eur J Cancer. 2007;43(14):2124–33. https://doi.org/10.1016/j.ejca.2007.07.010.
Tumeh PC, Harview CL, Yearley JH, Shintaku IP, Taylor EJM, Robert L, et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature. 2014;515(7528):568–71. https://doi.org/10.1038/nature13954.
Huang AC, Postow MA, Orlowski RJ, Mick R, Bengsch B, Manne S, et al. T-cell invigoration to tumour burden ratio associated with anti-PD-1 response. Nature. 2017;545(7652):60–5. https://doi.org/10.1038/nature22079.
Tofts PS, Brix G, Buckley DL, Evelhoch JL, Henderson E, Knopp MV, et al. Estimating kinetic parameters from dynamic contrast-enhanced T1- weighted MRI of a diffusable tracer: standardized quantities and symbols. J Magn Reson Imaging. 1999;10(3):223–32. https://doi.org/10.1002/(SICI)1522-2586(199909)10:3<223::AID-JMRI2>3.0.CO;2-S.
Fritz-Hansen T, Rostrup E, Larsson HBW, Søndergaard L, Ring P, Henriksen O. Measurement of the arterial concentration of Gd-DTPA using MRI: a step toward quantitative perfusion imaging. Magn Reson Med. 1996;36(2):225–31. https://doi.org/10.1002/mrm.1910360209.
Lubbock ALR, Stewart GD, O’Mahony FC, Laird A, Mullen P, O’Donnell M, et al. Overcoming intratumoural heterogeneity for reproducible molecular risk stratification: a case study in advanced kidney cancer. BMC Med. 2017;15(1):118. https://doi.org/10.1186/s12916-017-0874-9.
Berry SM, Carlin BP, Lee JJ, Muller P. Bayesian adaptive methods for clinical trials: CRC press; 2010. https://doi.org/10.1201/EBK1439825488.
Gerety EL, Lawrence EM, Wason J, Yan H, Hilborne S, Buscombe J, et al. Prospective study evaluating the relative sensitivity of 18F-NaF PET/CT for detecting skeletal metastases from renal cell carcinoma in comparison to multidetector CT and 99mTc-MDP bone scintigraphy, using an adaptive trial design. Ann Oncol. 2015;26(10):2113–8. https://doi.org/10.1093/annonc/mdv289.
Acknowledgements
We thank Prof Kevin Brindle, Dr. Nitzan Rosenfeld, Dr. Christopher Smit, Mr. Tevita Aho, Mr. Antony Riddick, Mr. James Armitage and Dr. Jessica Brown for their support in the development of the WIRE trial protocol.
Sponsor
The trial is sponsored by Cambridge University Hospitals NHS Foundation Trust (CUH) and University of Cambridge (UoC). The sponsors will retain full control of the data, its analysis and interpretation, writing of the report. Sponsor contact: Cambridge University Hospitals NHS Foundation Trust, Research and Development Department, Box 277, Cambridge Biomedical Campus, Hills Road, Cambridge CB2 0QQ.
Funding
The trial is sponsored by Cambridge University Hospitals NHS Foundation Trust (CUH) and University of Cambridge (UoC). The trial will be part funded by AstraZeneca UK and Cancer Research UK. Olaparib, cediranib and durvalumab will be supplied free of charge by AstraZeneca UK. This work is supported by The Mark Foundation Institute for Integrated Cancer Medicine (MFICM). MFICM is hosted at the University of Cambridge, with funding from The Mark Foundation for Cancer Research (NY, USA) and the Cancer Research UK Cambridge Centre [C9685/A25177] (UK). This research was supported by the NIHR Cambridge Biomedical Research Centre (BRC-1215-20014). The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Author information
Authors and Affiliations
Contributions
S.U. has drafted the manuscript and supported the development of the protocol and radiology manual of the WIRE trial. S.J.W is the principal investigator for the Cambridge site, medical oncology lead and translational lead of the trial, has contributed the development of the trial protocol and the writing of this manuscript. G.D.S. is the chief investigator, conceived the trial and had the idea for this manuscript. F.A.G. and E.S. are the trial radiologists, have supported the development of the protocol and radiology manual. A.Y.W is the trial pathologist, supported the development of the protocol and laboratory manual. H. M and J. W are the trial statisticians and have supported the development of the protocol and statistical analysis plan. G.Y. (senior), R. S (senior), M.G.T. (senior) and J.A.N.S. are trial coordinators and supported the development and running of the trial. A.C. is the trial pharmacist and supported the design of the trial. J.S., T.E. and M.C.O. provided scientific input. T.J.M, K.F., A.W. and A.M. supported the design of the trial. A.P. and B.V. are the leading trial oncologists at secondary trial sites and supported the design of the trial. M.S. and G.O. are the leading trial urological surgeons at secondary trial sites and supported the design of the trial. All authors have critically reviewed the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This trial has received ethical approval from the London - Harrow Research Ethics Committee (19/LO/1461) and the Health Research Authority (HRA) in the United Kingdom. Written informed consent to participate will be obtained from all participants.
Consent for publication
Not applicable.
Competing interests
This trial received funding from AstraZeneca, Cambridge, UK. G.D.S. declares educational grants from Pfizer, AstraZeneca, and Intuitive Surgical; consultancy fees from Pfizer, Merck, EUSA Pharma, and CMR Surgical; travel expenses from Pfizer; and speaker fees from Pfizer. S.J.W. has received travel support from Ipsen. E.S. declares being a co-founder and shareholder of Lucida Medical, consultancy fees from Amazon and speaker fees from GSK. S.U., M.G.T, R.S., G.Y. and J.A.N.S. declare no competing interests. T.E. was employed by and has stock in AstraZeneca, is employed by and has stock in Roche, has received research support from AstaZeneca, Bayer and Pfizer. K.F. has received advisory, consultancy or speaker fees from ESAI, Ipsen, Roche, Novartis, Merck, Pfizer, Eusa, BMS, conference support from Novartis, Ipsen and EUSA and institutional research funding from Roche, Merck, Exelixis. B.V. has received advisory, consultancy or speaker fees from Bristol Myers Squibb (BMS), Eisai, EUSA pharma, Ipsen, Merck Sorono, Merck Sharp & Dohme (MSD), Pfizer; conference support from Ipsen and Institutional research funding from Exelixis, Ipsen, MSD, Pfizer. A.P. has received advisory, consultancy or speaker fees from Eisai, BMS, Ipsen, MSD, Novartis, Roche, Astellas, Bayer, and Pfizer. Conference support from Pfizer, Ipsen, MSD, Roche, Astellas. Research funding from MSD. F.A.G. has research grants from GSK, research support from GE Healthcare and has consulted for AstraZeneca. M.C.O. has received research funding from Lilly. JS is an employee and stockholder in AstraZeneca, Cambridge, UK and a stockholder in GSK.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ursprung, S., Mossop, H., Gallagher, F.A. et al. The WIRE study a phase II, multi-arm, multi-centre, non-randomised window-of-opportunity clinical trial platform using a Bayesian adaptive design for proof-of-mechanism of novel treatment strategies in operable renal cell cancer – a study protocol. BMC Cancer 21, 1238 (2021). https://doi.org/10.1186/s12885-021-08965-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-021-08965-4