Abstract
Background
Acute myeloid leukemia (AML) remains one of the most common hematological malignancies, posing a serious challenge to human health. HSPA8 is a chaperone protein that facilitates proper protein folding. It contributes to various activities of cell function and also is associated with various types of cancers. To date, the role of HSPA8 in AML is still undetermined.
Methods
In this study, public datasets available from the TCGA (Cancer Genome Atlas) and GEO (Gene Expression Omnibus) were mined to discover the association between the expression of HSPA8 and clinical phenotypes of CN-AML. A series of bioinformatics analysis methods, including functional annotation and miRNA-mRNA regulation network analysis, were employed to investigate the role of HSPA8 in CN-AML.
Results
HSPA8 was highly expressed in the AML patients compared to the healthy controls. The high HSPA8 expression had lower overall survival (OS) rate than those with low HSPA8 expression. High expression of HSPA8 was also an independent prognostic factor for overall survival (OS) of CN-AML patients by multivariate analysis. The differential expressed genes (DEGs) associated with HSPA8 high expression were identified, and they were enriched PI3k-Akt signaling, cAMP signaling, calcium signaling pathway. HSPA8 high expression was also positively associated with micro-RNAs (hsa-mir-1269a, hsa-mir-508-3p, hsa-mir-203a), the micro-RNAs targeted genes (VSTM4, RHOB, HOBX7) and key known oncogenes (KLF5, RAN, and IDH1), and negatively associated with tumor suppressors (KLF12, PRKG1, TRPS1, NOTCH1, RORA).
Conclusions
Our research revealed HSPA8 as a novel potential prognostic factor to predict the survival of CN-AML patients. Our data also revealed the possible carcinogenic mechanism and the complicated microRNA-mRNA network associated with the HSPA8 high expression in AML.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
AML (Acute myeloid leukemia) is a common type of myeloid neoplasms with highly heterogeneous clinical outcomes [1]. The majority of AML patients are with normal karyotype, some of these patients do well with chemotherapeutic consolidation, but others have a poor clinical outcome. Besides, the treatment of old or ineligible for receiving intensive chemotherapy remains a challenge [2, 3], as well as those relapsed and refractory AML patients [4,5,6]. Discovering new biomarkers for AML patients to stratify the prognosis system has been one of the hotspots in recent years. Cytogenetic normal AML (CN-AML) provided an ideal platform for biomarker recognition since no chromosome abnormalities exist.
Heat shock 70 kDa protein (HSP70) is reported to be involved in tumor cell proliferation and metastasis [7]. Heat shock 70 kDa protein 8 (HSPA8) is a member of HSP70 belonging to the heat shock protein family. It is a constitutively expressed molecular chaperone, which plays an integral role in cellular stress response [8]. HSPA8 has been found overexpressed in various cancer cells, which was indispensable to the growth of cancer cells [7]. Furthermore, depletion of HSPA8 could suppress cell growth, induce apoptosis, and cell cycle arrest in solid human tumors [9]. However, the role of HSPA8 expression in AML is still poorly understood.
In this study, we identified a global gene expression profiling of HSPA8 in AML patients. HSPA8 was highly expressed in the AML cohort compared to the healthy cohort. The HSPA8 high expression was significantly associated with the adverse prognosis. In addition, our study revealed that HSPA8 expression might serve as an independent predictor for the OS of CN-AML, and HSPA8 high expression was linked to cancer-related genomic alteration. The above findings correspond to the predictive capability of HSPA8 high expression in terms of 1-year and 3-year survival.
Materials and methods
Patients and sources
The first CN-AML cohort (n = 77) was derived from the TCGA dataset (n = 151) (detailed information in Additional file 5: Table S1), age ranged from 21 to 88 years of old, all of which were collected and diagnosed from Washington University between 2001 to 2010 [1]. Following the Declaration of Helsinki, all subjects provided written consent of the study and received traditional induction and consolidation regimen following the guideline of AML treatment. Samples were derived from the peripheral blood at the time of diagnosis. All information on the clinical, cytogenetic characteristics and survival information could be downloaded from the cancer genome atlas (TCGA). CN-AML patients with complete clinical data and RNA sequencing data were included in this study, AML-M3 patients were not included in this study.
Other AML cohort patients were collected from Gene Expression Omnibus (GEO)(GEO accession number: GSE12417 [10], GSE7186 [11], GSE9476 [12], GSE8970 [5], GSE5122 [6]). All patients also signed the written consent of the treatment and the study. Gene expression data and corresponding clinical characteristics could be downloaded from the GEO dataset.
Bone marrow samples of 32 healthy adult donors and 47 newly diagnosed adult AML patients (non-M3, 26 CN-AML patients) hospitalized from 2014 to 2019 from the hematology department, Zhongda Hospital of Southeast University (Nanjing, China) were collected for research. All patients signed with written informed consents in accordance with the Declaration of Helsinki before enrollment of the study.
Reverse transcribed quantitative PCR (RT-qPCR)
The total RNA was extracted from bone marrow using Trizol agent (Invitrogen, USA) following the manufacture’s protocol. Then the mRNA was reverse transcribed into cDNA using the PrimeScript™ RT Master Mix (TaKaRa Dalian, China). The real-time PCR was performed on a StepOne Plus analysis system (Applied Biosystems 7300, Foster City, CA, USA), using TaKaRa SYBR Supermix (TaKaRa, Dalian, China). The amplification conditions of qPCR were as follows:95 °C for 30 s (pre-denaturation), 40 cycles of 95 °C for 5 s (denaturation) and 60 °C for 30 s (extension). The primers sequences were as follows:
-
(HSPA8) Forward: 5′- CACTTGGGTGGAGAAGATTTTG-3′; Reverse: 5′- CTGATGTCCTTCTTATGCTTGC-3′. (GAPDH) Forward: 5′-GCAAATTCCATGGCACCGT-3′; Reverse: 5′- GACTCCACGACGTACTCAGC-3′.
The relative expression levels of the target genes were calculated by the 2−ΔΔCt method.
Bioinformatics analysis of transcriptome sequencing (RNA-seq) data
Differential expression analyses of the two groups (HSPA8high and HSPA8low group) from public datasets were conducted using the edgeR package. Benjamini and Hochberg’s approach were used to control the FDR (false discovery rate). Genes with an adjusted P-value < 0.05, FDR < 0.1 found by edgeR were considered statistically significant. The cluster profiler R package was used to assess DEGs’ statistical enrichment (differential expressed genes) in KEGG pathways. miRNA- mRNA regulation network was constructed on the Cytoscape platform based on the miRNA predicting targets (miRTarBase, miRDB, TargetScan datasets), common targets from the three datasets will be finally included.
Statistical analysis
All the analyses were performed on the R 3.6.1 software platform. Data were presented as the mean ± SD. The overall survival (OS) was referred to as the time from the beginning of diagnosis to the death, induced by any causes. The correlation analysis of HSPA8 and OS was estimated by the K-M (Kaplan-Meier) method. ANOVA method was used to compare several groups (> 2 groups). t-test and False Discovery Rate (FDR) was used to identify differences in sequencing profiles of coding and non-coding RNAs between HSPA8high and HSPA8low groups. Annotation files for microRNAs targets could be fully downloaded from the database of miRDB, miRTarBase, and TargetScan. The Cytoscape software was applied for the molecular networks. Data analysis was all conducted on the R 3.6.1 platform and Perl script.
Results
High expression of HSPA8 is associated with adverse clinical outcome of AML
CN-AML patients derived from the TCGA dataset were divided into two groups according to the median expression level of HSPA8 (CN-AML, cutoff value: 7.71(FPKM)). The baseline clinical and molecular characteristics of the two groups were compared in Table 1. There were no significant differences in terms of age, gender, bone marrow blast percentage, WBC counting, hemoglobin, platelet counting (P > 0.05) between the two groups. Genetic mutations (KRAS, CEBPA, TET2, TP53, NRAS, IDH1, IDH2, RUNX1, NPM1) were also presented with no significant difference, while the mutation frequency of FLT3 increased significantly in the HSPA8high group (P < 0.0001).
Two datasets derived from the GEO were mined to compare the expression level of HSPA8 between AML patients and healthy controls (GSE9476 and GSE7186). The result indicated that the HSPA8 mRNA level was significantly increased in the AML cohort compared to that of healthy peripheral blood (GSE9476) and bone marrow (GSE7186) controls (P < 0.0001) (Fig. 1a, b).
HSPA8 high expression in AML compared to the healthy controls. Samples of GSE9476 were derived from peripheral blood (a), while samples of GSE7186 were derived from bone marrow (b). c The HSPA8 mRNA expression level of bone marrow samples derived from patients hospitalized in Zhongda Hospital from 2014 to 2019(Nanjing, China) was statistically higher in de novo AML, than in the healthy cohort
We further collected bone marrow samples of healthy donors and AML patients (non-M3) from Zhongda hospital (Nanjing, China) and examined the HSPA8 expression to validate the above findings. The baseline data of 32 healthy donors and 47 AML patient were presented in Table 2. As expected, we observed a higher expression level of HSPA8 in the de novo AML cohort, comparing to the healthy cohort (Fig. 1c) (P < 0.0001). Besides, we also observed a higher expression in the cytogenetic abnormal AML patients, though without significance (P = 0.1874) (Additional file 1).
Kaplan-Meier survival analysis indicated that HSPA8 high expression in CN-AML patients was significantly associated with the shorter OS (overall survival) (Fig. 2a-d, cutoff value for GSE12417-GPL570:11.73(FPKM), GPL96:12.46(FPKM), GPL97:12.97(FPKM)). Besides, an impaired survival benefit was observed among non-FLT3 mutant CN-AML patients (Fig. 2e). Furthermore, shorter OS was also observed in other AML groups such as cytogenetic abnormal, old AML, etc., not only the CN-AML group (Additional file 2A, B, C, D). The above findings indicated that the high HSPA8 expression was significantly correlated with worse OS in AML.
HSPA8 acts as an adverse prognostic factor for CN-AML patients. a OS analysis of HSPA8 in CN- AML group patients (GSE12417- GPL96 HSPA8high group = 21, HSPA8low group = 42); b OS analysis of HSPA8 in CN-AML group patients (GSE12417- GPL570 HSPA8high group = 41, HSPA8low group = 38); c OS analysis of HSPA8 in CN- AML group patients (GSE12417- GPL97 HSPA8high group = 52, HSPA8low group = 111); d OS analysis of HSPA8 in CN- AML group patients (TCGA dataset, HSPA8high group = 38, HSPA8low group = 39); e OS analysis of HSPA8 in CN- AML (non-FLT3 mutant) patients (TCGA dataset, HSPA8high group = 16, HSPA8low group = 34)
Univariable and multivariate Cox analysis of HSPA8 in CN-AML patients
We next conducted univariate Cox analysis for 77 TCGA CN-AML patients, including 17 variables (HSPA8 expression, age, gender, WBC counting, BM-blast, hemoglobin, platelet counting and genes mutation (FLT3, KRAS, CEBPA, TET2, TP53, NRAS, IDH1, IDH2, RUNX1, NPM1, mutation vs. wild type)). As is shown in Table 3, age, FLT3 mutation, RUNX1 mutation, platelet counting and HSPA8 expression were associated with shorter OS (HSPA8, HR = 2.042, P = 0.031; age, HR = 1.026, P = 0.003; FLT3 mutation, HR = 2.6, P = 0.001; RUNX1 mutation, HR = 2.22, P = 0.028). Whereas other variables (KRAS, CEBPA, TET2, TP53, NRAS, IDH1, IDH2, NPM1 (mutation vs. wild type), bone marrow blasts, WBC counting, hemoglobin, platelet counting) showed no statistical significance.
We further conducted the multivariate Cox analysis of OS (Table 3). Parameters with P value less than 0.2 during the univariate analysis were included in the Cox proportional hazards model. The result manifested that the age and HSPA8 expression level were independent risk factors (Fig. 3) (P < 0.05). Besides, the high expression of HSPA8 turned out to be the highest risk factor with an HR value of 2.408 (P = 0.032). Together, these results denoted that HSPA8 high expression showed an independent risk factor affecting the survival of CN-AML patients.
HSPA8 high expression is a potential marker for shorter OS of CN-AML
Based on the above results, we further hypothesized that the HSPA8 expression could well predict the survival of CN-AML patients. Herein, we used AUC-ROC (Area under the receiver operating characteristic curve) of the survival model to investigate the potential prognostic value of HSPA8 expression. The Youden index was calculated to dichotomize the cutoff point. The cutoff point in the 1-year survival data statistics is 7.812 (FPKM), while the 3-year survival cutoff point is 7.831; both were very similar to the median point of 7.71. The area under the ROC curve of HSPA8 reached 0.7264 and 0.7450 in 1-year OS (P = 0.0014) and 3 years OS (P = 0.0088), respectively, indicating a better predictive performance, compared with other clinical variables (age, gene mutation (FLT3, RUNX1, mutation vs. wild type)) (Fig. 4). These results suggested that the high expression of HSPA8 could serve as a valuable biomarker for predicting both the short- term and long- term survival of CN-AML patients. The result for HSPA8 expression predicting other AML groups was presented in Additional file 3. Similar predictive capacity was observed in terms of 1-year and 3-year survival in old AML patients (age > 60 years old), but HSPA8 had a lower predictive capacity for AML with karyotype abnormalities.
ROC curves of survival in TCGA CN-AML patients. The X-axis represents specificity, and the Y-axis represents sensitivity. ROC curves for gene mutation (RUNX1 (a), FLT3 (c), mutation vs. wild), age (b), HSPA8 expression (d) in OS of TCGA CN-AML patients were performed. AUC-ROC of HSPA8 expression reached 0.7264 (1-year survival, P = 0.0014), and 0.7450 (3-year survival, P = 0.00088), respectively
Molecular characteristics and GO, KEGG pathways correlated with HSPA8 expression
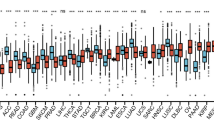
To make a full overview of the role of HSPA8 in the pathogenesis of AML, we identified the differential expressed genes (DEGs) using R software (edgeR package). Total 261 DEGs, including 131 upregulated genes and 130 downregulated genes, were identified (|log2FC| > 2, P < 0.01, FDR < 0.1) (Additional file 5). To delineate the role of HSPA8 in the CN-AML, we carried out the gene ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) analysis. The GO analysis data revealed that the HSPA8-based gene-sets were significantly associated with multiple biological procedures, including protein folding, unfolded protein binding and metabolic process, etc. (Fig. 5a, b); the enriched gene-sets of GSEA result were presented in Additional files 7 and 8. The result of KEGG analysis indicated that HSPA8-based DEGs were significantly enriched in several critical signaling pathways, including the PI3k-Akt signaling, cAMP signaling, focal adhesion, calcium signaling pathway (Fig. 5c). The above results were validated by the GSEA analysis of a separate CN-AML dataset (GSE12417-GPL570, Additional file 4A, B).
Function and pathway of HSPA8 involved in the CN- AML. a Top 9 enriched GSEA-GO terms in the HSPA8high group; b Top 9 enriched GSEA-GO terms in the HSPA8low group; c Enriched KEGG terms of DEGs (differential expressed genes) (log2FC > 2.0, p < 0.01, FDR < 0.1) in the HSPA8high group versus HSPA8low group
Genome-wide microRNA profiles linked to HSPA8 expression
The association of HSPA8 expression with the genome-wide expression profile was conducted based on the differential expressed micro- RNAs and DEGs (|log2FC| > 1, P < 0.01, FDR < 0.1) (Fig. 6a, b) to clarify the upstream regulation network. Finally, nine upregulated and seven downregulated micro-RNAs were included in this study. Three micro- RNAs (hsa-mir-1269a, hsa-mir-508-3p, hsa-mir-203a) were the most positively correlated with HSPA8 expression.
HSPA8 associated miRNA-mRNA network in CN-AML. a Volcano plot of differently expressed genes after comparing the HSPA8high group with the HSPA8low group among CN-AML patients. b Volcano plot of differently expressed miRNAs after comparing the HSPA8high group with the HSPA8low group among CN-AML patients. c miRNA- mRNA regulation and its correlation with HSPA8. Red nodes- upregulation in the HSPA8high group; green nodes- downregulation
Furthermore, we constructed the regulatory network of microRNA- mRNA network to clarify the biological functions associated with HSPA8 expression. The network was analyzed by overlapping of the DEGs (including 53 upregulated genes and 83 downregulated genes) and the microRNA targeted mRNAs (|log2FC| > 1, P < 0.01, FDR < 0.1), based on the predicting algorithm (Fig. 6c).
Notably, HSPA8high group was significantly associated with the upregulated level of many known oncogenes and the micro-RNAs’ predicted targets. Many oncogenes, including VSTM4, RHOB, HOBX7, were significantly upregulated in the HSPA8high group. Other important oncogenes, including KLF5, RAN, and IDH1, were significantly upregulated in the HSPA8high group. Meanwhile, tumor suppressors, including KLF12, PRKG1, TRPS1, NOTCH1, RORA, were downregulated in the HSPA8high group.
Discussion
The clinical outcome of cytogenetic normal AML (CN-AML) is significantly heterogeneous, accounted for nearly half of total AML patients [1, 13], which provided a good platform for the study of biomarker recognition since no chromosome abnormalities could be detected.
HSPA8 is a fascinating chaperone protein and plays an essential role in many biological processes [9]. Decreased expression of HSPA8 is beneficial for suppressing the proliferation of cancer cells, inducing cell proliferation arrest, and acting as a modulator of viability and autophagy for cancer cells [9]. HSPA8 could enhance the stability of BCL2L11/BIM mRNA stability, which could regulate the total counts of hematopoietic cells with the help of BAG4, STUB1, HIP, HSP40 proteins [14]. Besides, HSPA8 high expression has been identified in various cancer cells, including hepatocellular carcinoma and endometrial carcinoma, and is involved in cancer cell growth [15, 16] and regulating the autophagy in tumor cells [17]. Previous studies have reported that HSPA8 can promote BCR/ABL-induced chronic myeloid leukemia cells’ survival [18].
In this study, we found that the expression level of HSPA8 was higher in AML cohort than that in the healthy cohort. In addition, HSPA8 high expression was associated with poor clinical outcomes in multiple AML datasets. Moreover, HSPA8 high expression turned out to be the one of the highest risk factors related to a shorter OS by univariate and multivariate COX analysis and acted as an independent prognostic factor of the survival of patients with CN-AML. The AUC-ROC survival model analysis further revealed that HSPA8 expression was presented as a valuable variable to predict the prognosis of CN-AML and old AML in terms of 1-year and 3-year survival. These findings highlighted the potential role of HSPA8 in the pathogenesis of AML. Besides, we also observed a higher expression level among cytogenetic abnormal AML patients. This results indicated that the HSPA8 high expression could be associated with adverse outcome of cytogenetic abnormal AML patients. However, more details need to be delineated in the future.
We further analyzed the predictive role of HSPA8 expression in the survival of other AML subgroups. We found that it was not capable of predicting the survival for AML patients with karyotype abnormalities. However, a higher incidence of FLT3 mutation was found in HSPA8high group patients. It is reported that a combination of HSPA8/HSC70 with HSP90 may form the HSP90/HSC70 protein complex, which remarkably enhances their ATPase activities [19]. Meanwhile, FLT3 protein and HSP90 could be included in a multiprotein complex [20]. These reports highlighted the potential relationship between FLT3 and HSPA8, the further details need to be further delineated in future studies.
We also investigated the correlation between the high expression of HSPA8 and several oncogenic activities and signaling pathways, including PI3K-Akt and calcium signaling pathways. Specifically, constitutive PI3K activation was linked to reduced overall (OS) and disease-free survival (DFS) of 60% AML patients [21, 22]. Our data is consistent with the previous studies. For example, targeting the PI3k-Akt signaling pathway results in an anti-leukemic effect by activating oncogenes upstream (FLT3-ITD, KIT, NRAS, etc.) [23, 24]; and dysregulated Ca2+ homeostasis plays a crucial role in the pathogenesis of various cancers [25].
We further explored the possible underlying mechanisms for the high expression of HSPA8 by analysis of the miRNA-mRNA regulatory network in CN-AML patients. The top deferentially expressed micro-RNAs were hsa-mir-1269a, hsa-mir-508-3p, and hsa-mir-203a. They were aberrantly expressed in various malignancies and played roles in tumorigenesis’s pathogenesis [26,27,28]. Interestingly, the hsa-mir-1269a and hsa-mir-203a were not present in the miRNA-mRNA network, underling the unknown regulatory mechanism or indirect regulation associated with the HSPA8 expression, more details need to be clarified in the future. Besides, we did observe the reported/predicted targets of these miRNAs such as RHOB, VSTM4, HOXB7 were increased in the patients. RHOB, the predicted target of hsa-mir-153-5p, was reported to stimulate relapse of the disease in RUNX1-RUNX1T1 rearranged AML patients [29]. The ectopic expression of VSTM4, another target of hsa-mir-153-5p, could impair the anti-tumor immunity with robust T cell inhibitory activity [30]. Meanwhile, HOXB7, the target of mir-196a-5p, was overexpressed in various tumors and associated with a shorter OS [31].
We also observed that tumor suppressors, including KLF12, PRKG1, TRPS1, NOTCH1, and RORA, were downregulated in the HSPA8high group. Notably, TRPS1, predicted targeted by hsa-mir-374c-5p and has-mir-218-5p, could inhibit GATA transcription [32], which could, in turn, prolong the OS of AML patients [33]. NOTCH1, the predicted target of hsa-mir-30a-5p, was downregulated in the HSPA8high group; and overexpression of NOTCH1 may result in the inhibition of AML cell growth in vivo. Another interesting finding is that the hsa-mir-153-5p has downregulated the expression of RORA, of which the increased expression is associated with the improved overall survival of AML [34].
These results together revealed the possible relationship of these miRNAs and transcription factors associated with HSPA8 high expression and the complicated networks associated with HSPA8 oncogenesis in AML.
In the clinical practice, the gene expression cannot be compared horizontally among multi- clinical centers, using standard quantitative RT-PCR or real time PCR method, based on the principle of relative quantification. One promising solution could be the application of digital-PCR, a third generation PCR for the quantification of gene expression, claimed to have unprecedented sensitivity, reproducibility and linearity [35, 36]. Herein, we believe it is necessary to launch a multi-center joint research to detect the expression of HSPA8 in a large population, using digital-PCR method. Thus, it will be helpful to determine the diagnostic criteria of high HSPA8 expression with multi-center clinical data which will serve as a foundation for further risk stratification.
In summary, we observed the HSPA8 high expression in AML and have identified HSPA8 high expression as a potential independent prognostic factor in CN-AML patients. HSPA8 high expression is associated with cancer-related genomic alteration, including up- and downregulation of oncogenes and tumor suppressors, revealing the possible upstream signaling responsible for HSPA8 high expression and downstream networks. Future studies will elucidate more details about in the function and oncogenesis of AML.
Availability of data and materials
The datasets generated and analyzed during the current study are available in the TCGA and GEO repository (https://portal.gdc.cancer.gov/;https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi); Other datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Genomic and epigenomic landscapes of adult de novo acute myeloid leukemia. N Engl J Med. 2013;368(22):2059–74. https://doi.org/10.1056/NEJMoa1301689.
Büchner T, Hiddemann W, Schoch C, Haferlach T, Sauerland M-C, Heinecke A. Acute myeloid leukaemia (AML): treatment of the older patient. Best Pract Res Clin Haematol. 2001;14(1):139–51. https://doi.org/10.1053/beha.2000.0120.
Kantarjian H, O'Brien S, Cortes J, Giles F, Faderl S, Jabbour E, et al. Results of intensive chemotherapy in 998 patients age 65 years or older with acute myeloid leukemia or high-risk myelodysplastic syndrome. Cancer. 2006;106(5):1090–8. https://doi.org/10.1002/cncr.21723.
Shaffer BC, Gillet J-P, Patel C, Baer MR, Bates SE, Gottesman MM. Drug resistance: still a daunting challenge to the successful treatment of AML. Drug Resist Updat. 2012;15(1-2):62–9. https://doi.org/10.1016/j.drup.2012.02.001.
Raponi M, Lancet JE, Fan H, et al. A 2-gene classifier for predicting response to the farnesyltransferase inhibitor tipifarnib in acute myeloid leukemia. Blood. 2008;111:2589–96.
Raponi M, Harousseau J-L, Lancet JE, et al. Identification of molecular predictors of response in a study of tipifarnib treatment in relapsed and refractory acute myelogenous leukemia. Clin Cancer Res. 2007;13:2254–60.
Calderwood SK, Khaleque MA, Sawyer DB, Ciocca DR. Heat shock proteins in cancer: chaperones of tumorigenesis. Trends Biochem Sci. 2006;31:164–72.
Urquhart KR, Zhao Y, Baker JA, et al. A novel heat shock protein alpha 8 (Hspa8) molecular network mediating responses to stress- and ethanol-related behaviors. Neurogenetics. 2016;17:91–105.
Nirdé P, Derocq D, Maynadier M, et al. Heat shock cognate 70 protein secretion as a new growth arrest signal for cancer cells. Oncogene. 2010;29:117–27.
Metzeler KH, Hummel M, Bloomfield CD, et al. An 86-probe-set gene-expression signature predicts survival in cytogenetically normal acute myeloid leukemia. Blood. 2008;112:4193–201.
Lilljebjörn H, Heidenblad M, Nilsson B, et al. Combined high-resolution array-based comparative genomic hybridization and expression profiling of ETV6/RUNX1-positive acute lymphoblastic leukemias reveal a high incidence of cryptic Xq duplications and identify several putative target genes within the commonly gained region. Leukemia. 2007;21:2137–44.
Stirewalt DL, Meshinchi S, Kopecky KJ, et al. Identification of genes with abnormal expression changes in acute myeloid leukemia. Genes Chromosomes Cancer. 2008;47:8–20.
Döhner H, Estey EH, Amadori S, et al. Diagnosis and management of acute myeloid leukemia in adults: recommendations from an international expert panel, on behalf of the European LeukemiaNet. Blood. 2010;115:453–74.
Bouillet P, Metcalf D, Huang DC, Tarlinton DM, Kay TW, Köntgen F, et al. Proapoptotic Bcl-2 relative Bim required for certain apoptotic responses, leukocyte homeostasis, and to preclude autoimmunity. Science. 1999;286(5445):1735–8. https://doi.org/10.1126/science.286.5445.1735.
Xiang X, You X-M, Li L-Q. Expression of HSP90AA1/HSPA8 in hepatocellular carcinoma patients with depression. Onco Targets Ther. 2018;11:3013–23. https://doi.org/10.2147/OTT.S159432.
Shan N, Zhou W, Zhang S, Zhang Y. Identification of HSPA8 as a candidate biomarker for endometrial carcinoma by using iTRAQ-based proteomic analysis. Onco Targets Ther. 2016;9:2169–79. https://doi.org/10.2147/OTT.S97983.
Tian Y, Xu H, Farooq AA, Nie B, Chen X, Su S, et al. Maslinic acid induces autophagy by down-regulating HSPA8 in pancreatic cancer cells. Phytother Res. 2018;32(7):1320–31. https://doi.org/10.1002/ptr.6064.
José-Enériz ES, Román-Gómez J, Cordeu L, Ballestar E, Gárate L, Andreu EJ, et al. BCR-ABL1-induced expression of HSPA8 promotes cell survival in chronic myeloid leukaemia. Br J Haematol. 2008;142(4):571–82. https://doi.org/10.1111/j.1365-2141.2008.07221.x.
Woo JA, Liu T, Zhao X, Trotter C, Yrigoin K, Cazzaro S, et al. Enhanced tau pathology via RanBP9 and Hsp90/Hsc70 chaperone complexes. Hum Mol Genet. 2017;26(20):3973–88. https://doi.org/10.1093/hmg/ddx284.
Yao Q, Nishiuchi R, Li Q, Kumar AR, Hudson WA, Kersey JH. FLT3 expressing Leukemias are selectively sensitive to inhibitors of the molecular chaperone heat shock protein 90 through destabilization of signal transduction-associated kinases. Clin Cancer Res. 2003;9:4483.
Herschbein L, Liesveld JL. Dueling for dual inhibition: means to enhance effectiveness of PI3K/Akt/mTOR inhibitors in AML. Blood Rev. 2018;32(3):235–48. https://doi.org/10.1016/j.blre.2017.11.006.
Lindblad O, Cordero E, Puissant A, Macaulay L, Ramos A, Kabir NN, et al. Aberrant activation of the PI3K/mTOR pathway promotes resistance to sorafenib in AML. Oncogene. 2016;35(39):5119–31. https://doi.org/10.1038/onc.2016.41.
Park S, Chapuis N, Tamburini J, Bardet V, Cornillet-Lefebvre P, Willems L, et al. Role of the PI3K/AKT and mTOR signaling pathways in acute myeloid leukemia. Haematologica. 2010;95(5):819–28. https://doi.org/10.3324/haematol.2009.013797.
Martelli AM, Evangelisti C, Chiarini F, Grimaldi C, Manzoli L, McCubrey JA. Targeting the PI3K/AKT/mTOR signaling network in acute myelogenous leukemia. Expert Opin Investig Drugs. 2009;18(9):1333–49. https://doi.org/10.1517/14728220903136775.
Chen Y-F, Chen Y-T, Chiu W-T, Shen M-R. Remodeling of calcium signaling in tumor progression. J Biomed Sci. 2013;20(1):23. https://doi.org/10.1186/1423-0127-20-23.
Jin RH, Yu DJ, Zhong M. MiR-1269a acts as an onco-miRNA in non-small cell lung cancer via down-regulating SOX6. Eur Rev Med Pharmacol Sci. 2018;22(15):4888–97. https://doi.org/10.26355/eurrev_201808_15625.
Zhao L, Wang W, Xu L, Yi T, Zhao X, Wei Y, et al. Integrative network biology analysis identifies miR-508-3p as the determinant for the mesenchymal identity and a strong prognostic biomarker of ovarian cancer. Oncogene. 2019;38(13):2305–19. https://doi.org/10.1038/s41388-018-0577-5.
Chen L, Gao H, Liang J, Qiao J, Duan J, Shi H, et al. miR-203a-3p promotes colorectal cancer proliferation and migration by targeting PDE4D. Am J Cancer Res. 2018;8(12):2387–401.
Martina P, Matteo Z, Tregnago C, et al. Rhob overexpression boosts relapse of t(8;21) RUNX1-RUNX1T1 rearranged acute myeloid leukemia. Blood. 2017;130:1192.
Wang J, Manick B, Renelt M, et al. VSTM4 is a novel negative regulator of T cell activation. J Immunol. 2019;202:124.4.
Errico MC, Jin K, Sukumar S, Carè A. The widening sphere of influence of HOXB7 in solid tumors. Cancer Res. 2016;76(10):2857–62. https://doi.org/10.1158/0008-5472.CAN-15-3444.
Chen JQ, Bao Y, Litton J, Xiao L, Zhang HZ, Warneke CL, et al. Expression and relevance of TRPS-1: a new GATA transcription factor in breast cancer. Horm Cancer. 2011;2(2):132–43. https://doi.org/10.1007/s12672-011-0067-5.
Vicente C, Vazquez I, Conchillo A, García-Sánchez MA, Marcotegui N, Fuster O, et al. Overexpression of GATA2 predicts an adverse prognosis for patients with acute myeloid leukemia and it is associated with distinct molecular abnormalities. Leukemia. 2012;26(3):550–4. https://doi.org/10.1038/leu.2011.235.
Snider C, Fung K, Gould F, et al. RORA is a potential prognostic biomarker and therapeutic target for patients with acute myeloid leukemia. Blood. 2019;134:2696.
Hindson CM, Chevillet JR, Briggs HA, et al. Absolute quantification by droplet digital PCR versus analog real-time PCR. Nat Methods. 2013;10:1003–5.
Huggett JF, Whale A. Digital PCR as a novel technology and its potential implications for molecular diagnostics. Clin Chem. 2013;59(12):1691–3.
Acknowledgments
We acknowledged all the researchers and institutes for the published original datasets that we used in this study.
Funding
This work is supported in part by The National Natural Science Foundation of China (81770172); Jiangsu Provincial Special Program of Medical Science (BE2017747); Jiangsu Province “333” project (BRA2019103); The Fundamental Research Funds for the Central Universities (2242019K3DZ02); Milstein Medical Asian American Partnership (MMAAP) Foundation Research Project Award in Hematology (2017); Key Medical of Jiangsu Province (ZDXKB2016020).
Author information
Authors and Affiliations
Contributions
JL collected and analyzed data and wrote the manuscript; ZG supervised data analysis and corrected the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The institutional research ethics board at the Zhongda Hospital (Nanjing, China) reviewed and approved the study. Our research has been performed in accordance with the Declaration of Helsinki. Our team has acquired the administrative permissions to access the clinical patient data used in this research from the ethics board of Zhongda Hospital (Grant No. 2019ZDSYLL211-P01). All participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Comparison of HSPA8 expression among different AML subgroups. (A) The HSPA8 expression level of cytogenetic normal AML and cytogenetic abnormal AML. (B) The violin plot of HSPA8 expression level among AML subgroups (5q-, 7q-, inv(16), t(15, 17), t(8, 21), t(9, 11), > 3 abnormalities, and cytogenetic normal type).
Additional file 2: Figure S2.
HSPA8 acts as an adverse prognostic factor for AML patients. (A) OS analysis of HSPA8 in 34 relapsed/refractory AML patients (GSE8970 HSPA8high group = 9, HSPA8low group = 25) (P = 0.059). (B) OS analysis of HSPA8 in 58 relapsed/refractory AML patients (GSE5122 HSPA8high group = 7, HSPA8low group = 51) (P < 0.0001). (C) OS analysis of HSPA8 in cytogenetic abnormal AML patients (TCGA, P = 0.029). (D) OS analysis of HSPA8 in 52 old AML patients (TCGA, age > 60s, non-M3, P = 0.0052).
Additional file 3: Figure S3.
ROC curves of survival in AML patients. (A) 1-year and 3- year ROC analysis of HSPA8 expression in old AML patients (age over 60s). (B) 1-year and 3- year ROC analysis of HSPA8 expression in AML patients with karyotype abnormalities. The X-axis represents specificity, and the Y-axis represents sensitivity.
Additional file 4: Figure S4.
Function and signaling pathway of HSPA8 involved in the CN- AML (GSE12417-GPL570). (A) Top enriched GSEA-KEGG terms associated with the HSPA8 expression. (B) Top enriched GSEA-GO terms associated with the HSPA8 expression.
Additional file 5: Table S1.
Clinical profiles of 151 AML patients derived from the TCGA dataset.
Additional file 6: Table S2.
List of differentially expressed genes.
Additional file 7: Table S3.
Enriched gene sets of GSEA analysis in HSPA8high group.
Additional file 8: Table S4.
Enriched gene sets of GSEA analysis in HSPA8low group.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.