Abstract
Background
The aim of this study was to evaluate the efficacy and safety of nab-paclitaxel plus cisplatin in chemotherapy-naïve patients with advanced non-small-cell lung cancer (NSCLC).
Methods
Chemotherapy-naïve patients with advanced NSCLC were eligible. In the phase I dose-escalation cohort (3 + 3 design), patients received nab-paclitaxel (80 or 100 mg/m2 given intravenously on days 1, 8 and 15) plus cisplatin (60 or 75 mg/m2 given intravenously on day 1) every 4 weeks. The maximum tolerated dose was not reached. Nab-paclitaxel (100 mg/m2 given intravenously on days 1, 8 and 15) plus cisplatin (75 mg/m2 given intravenously on day 1) every 4 weeks was selected for the phase II cohort. The primary endpoint was the objective response rate (ORR).
Results
Twenty-three patients (phase I, n = 6; phase II, n = 17) were enrolled, and 22 patients were eligible. The median age was 67.5 years (range 37–75), 90.9% were males, 45.5% had adenocarcinoma and 81.8% had stage IV disease. The ORR was 59.1% (90% confidence interval (CI); 41.8–74.4), and the disease control rate was 86.4% (95% CI; 66.7–95.3). The median progression-free survival was 5.1 months (95% CI; 4.0–6.7), and the median overall survival was 24.2 months (95% CI; 8.4 months to not estimable). The common grade ≥ 3 adverse events were neutropenia (31.8%), leukopenia (27.3%), lung infection (18.2%) and hyponatremia (18.2%). There was one instance of grade 2 interstitial pneumonia and no treatment-related death.
Conclusions
Nab-paclitaxel plus cisplatin was well tolerated and associated with encouraging response outcomes in chemotherapy-naïve patients with advanced NSCLC. Further investigation is warranted.
Trial registration
UMIN Clinical Trials Registry: UMIN000011776; Date of registration: 17 September 2013; Date of enrolment of the first participant to the trial: 23 January 2014.
Similar content being viewed by others
Background
It is difficult to cure advanced non-small-cell lung cancer (NSCLC); however, especially in the last few years, the first-line treatment strategies in NSCLC have undergone significant changes. Prior to first-line treatment, mutations in driver oncogenes such as EGFR and ALK were analyzed, and if they were positive, a molecular targeting agent was selected. For patients in which the driver oncogene is negative or unknown, immune checkpoint inhibitors (ICIs) alone or in combination with cytotoxic drugs, depending on the programmed cell death-ligand 1 (PD-L1) status in the tumor and the tissue type, have been introduced as first-line treatments. However, treatment with cytotoxic drugs remains one of the standard therapies because sometimes it is difficult to use ICIs as the first-line treatment (e.g., in patients with interstitial pneumonia or autoimmune disease).
Nab-paclitaxel is a 130 nm uniform nanoparticle paclitaxel formulation comprised of paclitaxel and human serum albumin. It does not require Cremophor or anhydrous ethanol solvents to formulate, meaning that steroids or antihistamines do not necessarily have to be taken as pretreatments to suppress anaphylactic symptoms. It also allows for quicker administration than solvent-based paclitaxel (sb-paclitaxel). It may also improve the delayed sensory impairment caused by Cremophor [1,2,3]. The different properties of nab-paclitaxel compared to sb-paclitaxel also point to its better distribution within tumors than sb-paclitaxel (in vitro) [4]. Meanwhile, in terms of toxicity, the incidence of peripheral neuropathy, which is a concern with sb-paclitaxel, was significantly lower with weekly nab-paclitaxel plus carboplatin than with sb-paclitaxel, and it resulted in a shorter time to recovery from grade ≥ 3 neuropathy to grade 1.
It has been reported that sb-paclitaxel plus cisplatin extends median overall survival (mOS) more than etoposide plus cisplatin (9.9 months vs. 7.6 months; p = 0.48); as such, it has come to be considered a SOC [5].
Meanwhile, carboplatin, a derivative of cisplatin, does not require large-volume transfusion to prevent renal dysfunction and came into widespread clinical application in the 2000s. As reported by Rosell et al. in a phase III clinical study comparing sb-paclitaxel plus cisplatin to sb-paclitaxel plus carboplatin [6], sb-paclitaxel plus cisplatin was shown to be noninferior in terms of the primary endpoint of response rate (p = 0.45), but the mOS was 9.8 months in the sb-paclitaxel plus cisplatin arm (95% confidence interval (CI); 8.2–11 months) as opposed to 8.2 months in the sb-paclitaxel plus carboplatin arm (95% CI; 7.4–9.6 months), indicating that the sb-paclitaxel plus carboplatin arm was significantly inferior (hazard ratio (HR) 1.22; 90% CI 1.06–1.40; p = 0.019). The toxicity profile, however, was generally favorable in the sb-paclitaxel plus carboplatin arm, and it is easy to administer; as such, the platinum agent that is usually combined with sb-paclitaxel is carboplatin (more so than cisplatin). Moreover, a Japanese phase II study on sb-paclitaxel plus cisplatin also showed promising results; the response rate was 31% (95% CI; 16–50%), and the mOS was 14.8 months [7]. There have been, however, reports of grade ≥ 3 neuropathy at incidences ranging between 23 and 40% [5], highlighting the strong neurotoxicity issues. As such, the combination has not been used in the real-world clinical setting.
There have been multiple meta-analysis reports of comparisons between cisplatin and carboplatin to date, and they have reported no significant difference in survival [8,9,10]. The meta-analysis conducted by Ardizzoni et al. featured a cisplatin combination displaying a superior response rate to carboplatin (HR 1.37; 95% CI 1.16–1.61; p < 0.001). Moreover, when combined with a 3rd generation anticancer agent, cisplatin allowed for significantly more favorable survival than carboplatin (HR 1.11; 95% CI 1.01–1.21) [10]. Weekly nab-paclitaxel plus carboplatin actually displayed superiority over sb-paclitaxel plus carboplatin in CA031 [11], a multicenter international phase III controlled trial on lung cancer (the response rates were 33 and 25%, respectively; p = 0.005), in terms of all-grade sensory neuropathy (47 and 62%, respectively) as well as grade ≥ 3 adverse events (3 and 11%, respectively). The use of FACT-taxane also showed significantly more favorable results in the weekly nab-paclitaxel plus carboplatin arm than in the control arm. Accordingly, the neurotoxicity issue seen with sb-paclitaxel plus cisplatin conceivably could be reduced by switching the sb-paclitaxel to weekly nab-paclitaxel. Weekly nab-paclitaxel plus cisplatin may improve the toxicity profile compared with sb-paclitaxel plus cisplatin and may be a more effective therapy. As such, we planned a phase I/II study of the efficacy and safety of weekly nab-paclitaxel plus cisplatin in advanced NSCLC.
Methods
Patient eligibility
Eligible patients had histologically or cytologically confirmed NSCLC, stage IIIB or IV disease (diagnosed according to the seventh edition of the Union for International Cancer Control staging system) or suffered a recurrence after surgery, had no driver oncogenes (e.g., EGFR, ALK, ROS1, or RET) and were aged ≥20 years. Patients were also required to have measurable lesions as defined by Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1; an Eastern Cooperative Oncology Group (ECOG) PS of 0 or 1; a life expectancy ≥3 months; and adequate bone marrow, hepatic, and renal function. Patients with interstitial pneumonia or pulmonary fibrosis recognized on computed tomography (CT) scans, uncontrolled pleural effusions or symptomatic brain metastases were deemed to be ineligible.
The protocol was approved by institutional ethical review boards in each of the participating institutes, and all patients provided written informed consent before enrollment. The study was conducted in accordance with the ethical principles in the Declaration of Helsinki. The study has been registered under the University Medical Hospital Information Network (UMIN) Clinical Trials Registry: identifier UMIN 000011776.
Study design and treatment
The study was designed as a prospective, multicenter, single-arm phase I/II study of first-line combination therapy with nab-paclitaxel and cisplatin. The recommended dose (RD) was determined in phase I, and the efficacy and safety were assessed in phase II. Study design and treatment are presented in Fig. 1. The primary endpoint was treatment efficacy measured as the objective response rate (ORR) in patients who had received at least one cycle of the initial combination therapy. Disease control rate (DCR), overall survival (OS), progression-free survival (PFS), and adverse events (AEs) were also evaluated as secondary endpoints.
Patients received cisplatin at a dose of 60–75 mg/m2 given intravenously on day 1 and nab-paclitaxel at a dose of 80–100 mg/m2 given intravenously on days 1, 8, and 15. The combination therapy was repeated every 28 days for up to six cycles unless there was evidence of PD or intolerance of the study treatment. Subsequent cycles of treatment were withheld until the following criteria were satisfied: leucocyte count ≥3000/μL; neutrophil count ≥1500/μL; platelet count ≥100,000/μL; PS 0–1; aspartate aminotransferase ≤3.0 × upper limit of normal (ULN); alanine aminotransferase ≤3.0 × ULN; serum total bilirubin ≤1.5 × ULN; serum creatinine ≤1.2 mg/dL; grade ≤ 2 nonhematological toxicities; grade ≤ 2 peripheral neuropathy; and no infection with fever of at least 38 °C.
Dose-escalation scheme
In phase I, treatment was started at level 1 (cisplatin 75 mg/m2, nab-paclitaxel 80 mg/m2 q4w). Three patients were initially treated, and if dose-limiting toxicity (DLT) was not observed, we decided to move to level 2 (cisplatin 75 mg/m2, nab-paclitaxel 100 mg/m2 q4w). If DLT was observed in 1/3 patients at level 1, 3 patients were added. If DLT was observed in 2/6 patients or less, we moved to level 2. If DLT was observed in 3/6 patients or more, we considered level 1 as the MTD, and we decided to examine level 0 (cisplatin 60 mg/m2, nab-paclitaxel 80 mg/m2 q4w). If DLT was observed in 0/3 patients at level 2, we considered level 2 as the RD. If DLT was observed in 1/3 patients at level 1, 3 patients were added. If DLT was observed in 2/6 patients or less, we considered level 2 as the RD. If DLT was observed in 3/6 patients or more, we considered level 2 as the MTD and level 1 as the RD.
DLT was evaluated by the National Cancer Institute Common Terminology Criteria (NCI-CTC) for Adverse Events version 4.0 and was defined as any of the following during the first cycle of the protocol treatment at each level: leukopenia of grade 4 that lasted more than 4 days, febrile neutropenia, thrombocytopenia of grade 4 or requirement of platelet transfusion, nonhematological toxicity of grade 3 or higher (without nausea, vomiting, anorexia, constipation, and electrolyte abnormalities), and no administration of nab-paclitaxel on days 8 and 15.
Baseline and treatment assessments
The baseline evaluations included medical history, physical examination, electrocardiogram, ECOG performance status, and laboratory analyses. CT scans of the chest and the upper abdomen, magnetic resonance imaging (MRI) studies or CT scans of the brain, and bone scintigraphy or positron emission tomography (PET)-CT studies were performed for tumor assessment within 28 days of initiation of the study treatment. Tumor measurements were assessed with chest X-ray, CT scans, MRI studies, or bone scintigraphy or PET-CT studies. CT scans were repeated every 2 cycles until PD, MRI studies or CT scans of the brain were repeated every 3 months or upon the appearance of any neurologic symptoms, and bone scintigraphy or PET-CT studies were performed every 6 months or upon the appearance of any bone-related symptoms. Objective tumor responses were based on RECIST version 1.1. The ORR was confirmed via extramural review. Toxicity evaluations were based on NCI-CTC version 4.0.
Statistical analysis
Analyses of efficacy and safety were based on a December 2017 database lock. On the basis of previous studies [7], we assumed that an ORR of 40% in eligible patients would indicate potential usefulness, while an ORR of 20% would be the lower limit of interest. The number of patients needed to provide 80% power with a one-sided significance level of 5% was calculated to be 32. Taking ineligible patients into account, we intended to enroll 35 patients. Efficacy and safety analyses were planned for patients who received at least one dose of the treatment. Efficacy analysis included patients enrolled in phase I and phase II. The ORR was defined as the proportion of patients achieving the best response of complete response (CR) or partial response (PR) and summarized by a binomial response rate. The two-sided 90% CI, which corresponded to a one-sided significance level of 0.10, was presented using the Wilson method [12] with respect to the efficacy primary endpoint of ORR. The DCR was defined as the proportion of patients achieving CR/PR or stable disease (SD), summarized by a binomial response rate, and assessed with the corresponding 95% CIs. PFS and OS were analyzed using the Kaplan-Meier method to estimate the median values with the corresponding 95% CIs using the Brookmeyer-Crowley method [13]. All analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA).
Results
Dose escalation
First, 3 patients were treated with level 1, and DLT was not observed. Next, we moved to level 2, and 3 patients were treated, but DLT was not observed. Therefore, level 2 was decided as the RD.
Patient characteristics and treatment
Twenty-three patients (phase I cohort, n = 6; phase II cohort, n = 17) were enrolled from October 2013 to September 2017. The study was terminated before the targeted initial sample size was met because of poor accrual. One patient was excluded from the analysis because of disease progression before the protocol treatment was started. After excluding 1 ineligible patient, 22 patients were ultimately evaluated. The baseline characteristics are shown in Table 1. The median age was 67.5 years (range, 37–75 years), 10 patients (45.5%) had adenocarcinoma histology, 18 patients (81.8%) had stage IV disease, and all patients (100%) were smokers. The median number of treatment cycles was 4 (range, 1–6).
Efficacy
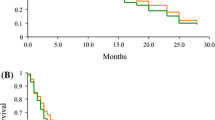
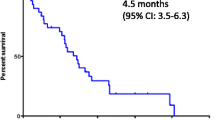
Tumor responses are shown in Table 2. The ORR was 59.1% (90% CI; 41.8–74.4%), and the DCR was 86.4% (95% CI; 66.7–95.3%). The maximum changes in tumor measurements are presented in Fig. 2. The median PFS was 5.1 months (95% CI; 4.0–6.7 months) (Fig. 3a), and the median OS was 24.2 months (95% CI; 8.4 months to not estimable (NE)) (Fig. 3b). The OS was 19.8 months (95% CI; 6.7 months to NE) in squamous cell lung cancer (SqCC) and 24.2 months (95% CI; 6.3 months to NE) in non-SqCC (Fig. 3c).
Toxicity
Twenty-two patients who received the study treatment were deemed eligible for safety analysis. Hematologic AEs and nonhematologic AEs that occurred in ≥10% of patients are shown in Table 3. The grade 3/4 hematologic AEs were neutropenia (31.8%), leukopenia (27.3%), anemia, and febrile neutropenia (4.5% each). The grade 3/4 nonhematologic AEs were hyponatremia and lung infection (18.2% each) and anorexia, fatigue, hyperkalemia, increased serum amylase, increased lipase, seizure, glaucoma, retinopathy, and hypoxia (4.5% each). There was one instance of grade 2 interstitial pneumonia, and there was no treatment-related death.
Discussion
We conducted a phase I/II multicenter joint clinical study on weekly nab-paclitaxel plus cisplatin in treatment-naïve advanced NSCLC patients. The issue, however, was the rapid development of ICIs during the study, including robust development of treatment with combinations of ICIs and chemotherapy, which resulted in slow accrual and eventual completion of the study with a smaller sample than originally planned.
The primary endpoint, ORR, was 59.1%, which was higher than that observed in the CA031 study (33%) and its Japanese subset (35%). While weekly nab-paclitaxel plus carboplatin has displayed a more favorable response rate in SqCC (41% in the CA031 study and 50% in its Japanese subset), the proportion of SqCC in this study (31.8%) was not so high as compared to the CA031 study (44%) and its Japanese subset (14%).
The median PFS (mPFS) was 5.1 months, as opposed to 6.3 and 6.9 months in CA031 and the Japanese subset, respectively, indicating an inferior mPFS. The study enrolled a small number of patients, and the confidence interval was relatively large, making it difficult to determine the quality of these outcomes. It is conceivable that the fact that our study established a maximum of 6 cycles, whereas CA031 did not have a set maximum in place, could have had an influence on the outcomes. Meanwhile, considering that the OS in our study was relatively favorable, weekly nab-paclitaxel plus cisplatin most likely had a minimal impact on subsequent treatments.
Pemetrexed maintenance is one of the standard regimens for first-line treatment of nonsquamous NSCLC. The OS of nonsquamous NSCLC in this study seems to be comparable to the that found in the PARAMOUNT trial [14]. However, it is a limitation that the sample size of our study was small.
No particularly new toxicities were observed above and beyond those seen in other studies to date. Analysis of the Japanese subset in CA031 showed a delay in the initiation of a subsequent course of treatment in 64.3% of the patients, and the median delay was 8 days. Based on these findings, we administered nab-paclitaxel on days 1, 8, and 15, skipping 1 week, in a 4-week cycle. We feel that this maintained the dose intensity that was seen in CA031. Due to the altered schedule, the incidence of all-grade hematological toxicity was virtually the same as that in previous reports. The incidence of grade 3/4 neutropenia was slightly higher (31.8%) than that in CA031 but lower than that in the Japanese subset of CA031 (69% of ≥ Grade 3). In general, myelosuppression in Japanese patients tends to be strong, but it is considered acceptable. There was no hematological toxicity, as in CA031, which frequently requires dose delays and reductions, which facilitated handling. In regard to nonhematological toxicity, there was no particular increase in sensory peripheral neuropathy compared with CA031. While hyponatremia was observed in a relatively large percent of patients, it was adequately manageable. Additionally, while grade ≥ 3 lung infections were observed in 4 patients (18.2%), they all improved. Although grade 2 ILD was observed in 1 patient, there were no treatment-related deaths; safety was within the permissible range.
In recent years, combination therapies consisting of platinum-based combination therapy and ICIs have been developed. In fact, the outcomes from the KEYNOTE-407 trial showed that pembrolizumab added to weekly nab-paclitaxel plus carboplatin prolonged survival [15] and improved health-related quality of life (HRQoL) [16], and it is being introduced into the clinical setting. Recently, the results of the IMpower130 trial also demonstrated the efficacy of the nab-paclitaxel regimen in nonsquamous NSCLC, which has also been introduced into the clinical setting [17]. Moreover, the efficacy and safety of nab-paclitaxel plus carboplatin have been reported in patients with NSCLC with interstitial lung disease [18]. Given that the combination of nab-paclitaxel and platinum salts has been reported to be effective, the results of our study are promising for the future treatment of NSCLC. With reports stating that the combination of nab-paclitaxel and platinum is effective, the results of our study may be promising in the future treatment of NSCLC.
Myelosuppression was mild, and the response rate was promising. As such, weekly nab-paclitaxel plus cisplatin with few treatment delays/skipped treatments (which rarely require schedule changes) could conceivably be a promising candidate for combination therapy with anti-PD-1/PD-L1 antibodies.
Conclusions
Accordingly, weekly nab-paclitaxel plus cisplatin could be an easy-to-handle treatment option that is highly efficacious with a low incidence of hematological toxicity. Since weekly nab-paclitaxel plus cisplatin is considered promising as a base regimen in combination with ICIs, we would like to conduct a clinical trial of anti-PD-1/−PD-L1 antibodies combined with weekly nab-paclitaxel plus cisplatin for NSCLC in the future.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AE:
-
Adverse event
- CI:
-
Confidence interval
- CR:
-
Complete response
- CT:
-
Computed tomography
- DCR:
-
Disease control rate
- DLT:
-
Dose-limiting toxicity
- ECOG:
-
Eastern Cooperative Oncology Group
- HR:
-
Hazard ratio
- HRQoL:
-
Health-related quality of life
- ICI:
-
Immune checkpoint inhibitor
- ILD:
-
Interstitial lung disease
- MRI:
-
Magnetic resonance imaging
- NCI-CTC:
-
National Cancer Institute Common Terminology Criteria
- NSCLC:
-
Non-small-cell lung cancer
- ORR:
-
Objective response rate
- OS:
-
overall survival
- PD:
-
Progressive disease
- PD-1:
-
Programmed cell death-1
- PD-L1:
-
Programmed cell death-ligand 1
- PET:
-
Positron emission tomography
- PFS:
-
Progression-free survival
- PR:
-
Partial response
- PS:
-
Performance status
- RD:
-
Recommended dose
- RECIST:
-
Response Evaluation Criteria in Solid Tumors
- SD:
-
Stable disease
- SOC:
-
Standard of care
- SqCC:
-
Squamous cell lung cancer
- ULN:
-
Upper limit of normal
- UMIN:
-
University Medical Hospital Information Network
References
Boer HH, Moorer-van Delft CM, Muller LJ, Kiburg B, Vermorken JB, Heimans JJ. Ultrastructural neuropathologic effects of Taxol on neurons of the freshwater snail Lymnaea stagnalis. J Neuro-Oncol. 1995;25(1):49–57.
Windebank AJ. The vehicle for cyclosporine is neurotoxic in vitro. Ann Neurol. 1997;41(4):563–4.
Authier N, Gillet JP, Fialip J, Eschalier A, Coudore F. Description of a short-term Taxol-induced nociceptive neuropathy in rats. Brain Res. 2000;887(2):239–49.
Desai N, Trieu V, Yao Z, Louie L, Ci S, Yang A, Tao C, De T, Beals B, Dykes D, et al. Increased antitumor activity, intratumor paclitaxel concentrations, and endothelial cell transport of cremophor-free, albumin-bound paclitaxel, ABI-007, compared with cremophor-based paclitaxel. Clin Cancer Res. 2006;12(4):1317–24.
Bonomi P, Kim K, Fairclough D, Cella D, Kugler J, Rowinsky E, Jiroutek M, Johnson D. Comparison of survival and quality of life in advanced non-small-cell lung cancer patients treated with two dose levels of paclitaxel combined with cisplatin versus etoposide with cisplatin: results of an eastern cooperative oncology group trial. J Clin Oncol. 2000;18(3):623–31.
Rosell R, Gatzemeier U, Betticher DC, Keppler U, Macha HN, Pirker R, Berthet P, Breau JL, Lianes P, Nicholson M, et al. Phase III randomised trial comparing paclitaxel/carboplatin with paclitaxel/cisplatin in patients with advanced non-small-cell lung cancer: a cooperative multinational trial. Ann Oncol. 2002;13(10):1539–49.
Sakai H, Yoneda S, Tamura T, Nishiwaki Y, Yokoyama A, Watanabe K, Saijo N. A phase II study of paclitaxel plus cisplatin for advanced non-small-cell lung cancer in Japanese patients. Cancer Chemother Pharmacol. 2001;48(6):499–503.
Hotta K, Matsuo K, Ueoka H, Kiura K, Tabata M, Tanimoto M. Meta-analysis of randomized clinical trials comparing Cisplatin to carboplatin in patients with advanced non-small-cell lung cancer. J Clin Oncol. 2004;22(19):3852–9.
Ardizzoni A, Boni L, Tiseo M, Fossella FV, Schiller JH, Paesmans M, Radosavljevic D, Paccagnella A, Zatloukal P, Mazzanti P, et al. Cisplatin- versus carboplatin-based chemotherapy in first-line treatment of advanced non-small-cell lung cancer: an individual patient data meta-analysis. J Natl Cancer Inst. 2007;99(11):847–57.
Jiang J, Liang X, Zhou X, Huang R, Chu Z. A meta-analysis of randomized controlled trials comparing carboplatin-based to cisplatin-based chemotherapy in advanced non-small cell lung cancer. Lung Cancer. 2007;57(3):348–58.
Socinski MA, Bondarenko I, Karaseva NA, Makhson AM, Vynnychenko I, Okamoto I, Hon JK, Hirsh V, Bhar P, Zhang H, et al. Weekly nab-paclitaxel in combination with carboplatin versus solvent-based paclitaxel plus carboplatin as first-line therapy in patients with advanced non-small-cell lung cancer: final results of a phase III trial. J Clin Oncol. 2012;30(17):2055–62.
Wilson EB. Probable inference, the law of succession, and statistical inference. J Am Stat Assoc. 1927;22(158):209–12.
Brookmeyer RC, J. A confidence interval for the median survival time. Biometrics. 1982;38(1):29–41.
Paz-Ares LG, de Marinis F, Dediu M, Thomas M, Pujol JL, Bidoli P, Molinier O, Sahoo TP, Laack E, Reck M, et al. PARAMOUNT: final overall survival results of the phase III study of maintenance pemetrexed versus placebo immediately after induction treatment with pemetrexed plus cisplatin for advanced nonsquamous non-small-cell lung cancer. J Clin Oncol. 2013;31(23):2895–902.
Paz-Ares L, Luft A, Vicente D, Tafreshi A, Gumus M, Mazieres J, Hermes B, Cay Senler F, Csoszi T, Fulop A, et al. Pembrolizumab plus chemotherapy for squamous non-small-cell lung Cancer. N Engl J Med. 2018;379(21):2040–51.
Mazieres J, Kowalski D, Luft A, Vicente D, Tafreshi A, Gumus M, Laktionov K, Hermes B, Cicin I, Rodriguez-Cid J, et al. Health-Related Quality of Life With Carboplatin-Paclitaxel or nab-Paclitaxel With or Without Pembrolizumab in Patients With Metastatic Squamous Non-Small-Cell Lung Cancer. J Clin Oncol. 2020;38(3):271-80.
West H, McCleod M, Hussein M, Morabito A, Rittmeyer A, Conter HJ, Kopp H-G, Daniel D, McCune S, Mekhail T, et al. Atezolizumab in combination with carboplatin plus nab-paclitaxel chemotherapy compared with chemotherapy alone as first-line treatment for metastatic non-squamous non-small-cell lung cancer (IMpower130): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2019;20(7):924–37.
Kenmotsu H, Yoh K, Mori K, Ono A, Baba T, Fujiwara Y, Yamaguchi O, Ko R, Okamoto H, Yamamoto N, et al. Phase II study of nab-paclitaxel + carboplatin for patients with non-small-cell lung cancer and interstitial lung disease. Cancer Sci. 2019;110(12):3738–45.
Acknowledgements
We thank all patients and investigators who participated in this study. This study was partially presented at the European Lung Cancer Conference 2018, Geneva, Switzerland (April 13, 2018) and the 2018 Japanese Society of Medical Oncology Annual Meeting, Kobe, Japan (July 19, 2018).
Funding
Financial support for this research was provided by Taiho Pharmaceutical, which had no role in the design of the study; collection, analysis, and interpretation of the data; or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
YH, RU, SM, SN, FI and MS carried out the study design. YH, RU, SM and MS analyzed and interpreted the study data. YK1, SI, TI, YU, YK2, RT, TK and KN provided the study materials or patients. YH and MS prepared and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethical review board of Hyogo Cancer Center (approval reference number R-111), the ethical review board of Saitama Cancer Center (approval reference number CA013–22), and the Ethics Committee, Osaka International Cancer Institute (approval reference number 1311253188). This study was conducted in accordance with the ethical principles in the Declaration of Helsinki. The study has been registered under the University Medical Hospital Information Network (UMIN) Clinical Trials Registry: identifier UMIN 000011776. All patients provided written informed consent before enrollment. The informed consent form also contained an agreement for the publication of the study results.
Consent for publication
Not applicable.
Competing interests
YH has received grants and personal fees from Ono Pharmaceutical and MSD as well as personal fees from AstraZeneca, Boehringer Ingelheim, Chugai Pharmaceutical, Eli Lilly, Novartis and Taiho Pharmaceutical. TI has received personal fees from AstraZeneca, Chugai Pharmaceutical, Ely Lilly, MSD and Ono Pharmaceutical. TK has received grants and personal fees from AstraZeneca, Boehringer Ingelheim, Chugai Pharmaceutical, Eli Lilly, MSD, Novartis, Ono Pharmaceutical, Pfizer, and Taiho Pharmaceutical as well as grants from Merck Serono, Regeneron Pharmaceuticals, and Takeda Pharmaceutical as well as personal fees from Bristol-Myers Squibb and TEIJIN PHARMA. KN has received grants and personal fees from Boehringer Ingelheim as well as personal fees from AstraZeneca and Chugai Pharmaceutical. RU has received personal fees from Eisai and CAC Croit. SM has received grants and personal fees from Boehringer Ingelheim as well as personal fees from AstraZeneca, Bristol-Myers Squibb, Chugai Pharmaceutical, Eli Lilly, MSD, Ono Pharmaceutical, Pfizer and Taiho Pharmaceutical. FI has received grants and personal fees from AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, Chugai Pharmaceutical, MSD, and Ono Pharmaceutical as well as personal fees from Eli Lilly, Kyowa Hakko Kirin, Novartis, Pfizer and Taiho Pharmaceutical. MS has received grants and personal fees from AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, Chugai Pharmaceutical, Eli Lilly, MSD, Novartis, Ono Pharmaceutical, and Pfizer as well as grants from AbbVie and Ignyta. All remaining authors have declared no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Hattori, Y., Kono, Y., Itoh, S. et al. A phase I/II study of weekly nab-paclitaxel plus cisplatin in chemotherapy-naïve patients with advanced non-small-cell lung cancer. BMC Cancer 20, 115 (2020). https://doi.org/10.1186/s12885-020-6588-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-020-6588-y