Abstract
Background
Men who have sex with men (MSM) living with HIV are at increased risk for anal cancer. We evaluated satisfaction with first-time anal cancer screening using high resolution anoscopy (HRA) as a cross sectional survey among men who have sex with men (MSM) attending a community-engaged clinic in Abuja, Nigeria.
Methods
Between March and August 2017, 342 MSM underwent screening and 307 (89%) completed a satisfaction survey that evaluated 8 domains related to expectations, convenience, staff interpersonal skills, physical surroundings, technical competence, pain/discomfort, general satisfaction, and intention to re-screen if symptomatic. The 22-item questionnaire used 5-point Likert scales ranging from 1 (strongly disagree) to 5 (strongly agree). For each domain, responses to specific items were averaged, aggregated, and converted to a 100-point scaled score (SS) with 25 and 75 corresponding to disagree and agree, respectively.
Results
Median age was 24 years (interquartile range [IQR]: 22–28), median years since anal coital debut was 7 (IQR: 4–12), and 58% (95% confidence interval [CI]: 52–64%) were living with HIV. Despite respondents reporting pre-procedure anxiety (SS:73), most were comfortable with the setting and procedure and reported overall satisfaction (SS:74–76). Willingness to undergo future screening had the lowest score (SS:69) within the general satisfaction domain. The lowest scoring domains were pain/discomfort (SS:57) and agreement to re-screen if symptomatic (SS:59), which correlated with lower overall satisfaction (p < 0.001). Domain responses did not differ by HIV infection after adjusting for multiple comparisons (p > 0.006) or number of anal biopsies (all p > 0.05).
Conclusions
Overall, HRA was satisfactory for those naïve to screening but moving forward necessitates monitoring levels of discomfort with pain scales and normalizing dialogue around clinical symptoms of anal cancer and overall anal health to sustain future screening.
Similar content being viewed by others
Background
Persistent high-risk human papillomavirus (HPV) infection is associated with the development of high-grade squamous intraepithelial lesions (HSIL), particularly among men who have sex with men (MSM) living with HIV. HSIL has the potential to regress with an effective immune response, but the 5-year progression rate of anal cancer from HSIL has been estimated to be 2–3% among men living with HIV [1, 2]. A recent study suggested anal cancer incidence is rising steeply for younger black men beginning at age 30 and is 5-fold higher among those born in the mid-eighties compared to those born in mid-forties in the United States [3]. Without clinical evidence demonstrating that screening prevents anal cancer there are no national guidelines to standardize screening practices and set age limits for screening [4]. However, recommendations exist for those at highest risk, including MSM and persons living with HIV [5,6,7,8]. High resolution anoscopy (HRA) and directed biopsy are currently used for early detection of HSIL, which if present, can be treated or actively monitored for natural regression. These strategies potentially improve long-term health outcomes given the complications of treating invasive cancer [9, 10].
During HRA examinations, a physician observes a magnified and illuminated view of the anal canal with a colposcope. A lubricated tube, known as an anoscope, is manipulated around the circumference to flatten anal folds for identification and treatment of HSIL. The procedures may be perceived as invasive and cause pain, resulting in an unfavorable response to screening, ultimately reducing participation and sustainability of a screening program. A few studies have evaluated patient level satisfaction with HRA and found that participants who underwent the procedure generally reported little pain and 92–99% agreed to future HRA examinations [11,12,13,14]. However, the prior satisfaction surveys were conducted in developed countries such as the United States, United Kingdom, and Canada, where the majority of screening programs exist for at-risk populations [12, 15, 16]. In sub-Saharan Africa, where there is an unknown burden of anal cancer [17, 18], the limited knowledge about the disease and lack of screening programs could impact acceptability. This is particularly relevant in an environment where engagement of MSM in healthcare settings is challenged by pervasive stigma against same-sex practices [19, 20]. This study assessed satisfaction with anal cancer screening using HRA among MSM living with or at risk for HIV in Abuja, Nigeria.
Methods
Study population and screening
Anal cancer screening was conducted as a primary analysis for a year in the TRUST/RV368 cohort in Abuja, Nigeria [21,22,23]. The purpose of the TRUST/RV368 cohort, was to engage men who have sex with men in an HIV treatment-as-prevention study at “trusted” community centers that specialized in the clinical care and sexual health needs of sexual and gender minorities. In brief, TRUST/RV368 participants were educated on the rationale and procedures of the anal cancer screening study. Men who volunteered to participate in the screening study, aged ≥18 years, and provided informed consent in English or Hausa were enrolled. Exclusion criteria included any medical condition that would increase risk associated with HRA or anal biopsy, such as a bleeding disorder or an allergy to lidocaine or iodine. Enrolled men underwent swabbing for cytology and future HPV testing, digital ano-rectal examination (DARE), HRA and HRA-directed biopsies of gross abnormalities for histologic evaluation. Two percent lidocaine was mixed with lubricant and used for DARE and HRA. Five percent acetic acid and Lugol’s iodine were used to visualize abnormalities and only men with acetowhite lesions were biopsied. MSM diagnosed with HSIL were offered ablative treatment with an infrared hyfrecator. Beginning in March 2017 through August 2017, the self-administered satisfaction questionnaire was available for completion after HRA screening. Additional demographic, clinical and behavioral data were obtained from interviewer-administered questionnaires collected by the TRUST/RV368 cohort and the anal cancer screening study.
Screening assessment
The 22-item questionnaire evaluated 8 domains relating to satisfaction with anal cancer screening: expectations, convenience, staff interpersonal skills, physical surroundings, perceived technical competence, pain/discomfort, general satisfaction, and intention to screen if symptomatic. Eighteen of the questions were previously used by Kwong et al. to assess patient satisfaction during the implementation of an anal cancer screening program at the University of Colorado [11]. They modified a validated scale for assessing satisfaction with colon cancer screening [24] to reflect anal cancer screening procedures. They reviewed the scale’s internal consistency with factor analysis and Cronbach’s alpha and found high factor loading for two subscales, the satisfaction with clinical program and satisfaction with exam experience (Cronbach α = 0.866 and α = 0.873, respectively) with values of at least 0.6 indicative of internal consistency. The third subscale was distress and included only two questions (anxious and embarrassed by the procedure) and had lower internal consistency (Cronbach α = 0.550) [11]. In our study, an additional 4 questionnaire items were added. One item, “Observing the procedure on the monitor made me more comfortable during the exam” was added to evaluate whether being engaged visually relaxed patients during the exam. Three items were added to assess likelihood of pursuing screening if presented with clinical symptoms of anal cancer (“If I had rectal or abdominal pain; bleeding either from wiping after a bowel movement or on my stool; constipation or straining or smaller/unusually shaped stools, then I would seek screening”). All questionnaire items were posed on a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). Reverse coding was applied to some of the responses to maintain a consistent direction of response favorability for the analyses. These included the following statements: “I found it hard to find a convenient time to come for screening”, “The staff seemed to hurry me through too quickly”, “The staff used words that were hard to understand”, “The physician was too rough when performing the screening”, “I had a lot of pain during the procedure”, “The procedure caused me great discomfort” and “I was embarrassed by the procedure”.
Statistical analyses
Distributions of baseline demographics by HIV status were evaluated using Pearson’s Chi-square and Fisher’s exact tests. Data on age, years since anal coital sexual debut, sexual position (insertive only, receptive only or both) any transactional sex in the past year, and laboratory diagnosed HIV and/or rectal sexually transmitted infections were obtained from TRUST/RV368 cohort [21, 22]. Transactional sex was defined as having exchanged anal or oral sex for things wanted or needed such as money, drugs, food, shelter or transportation [25]. HIV was diagnosed from finger stick blood samples using a parallel testing algorithm [26]. Nucleic acid amplification diagnoses of rectal Neisseria gonorrhoeae and Chlamydia trachomatis [26] were further categorized as none, individual infections, or both. Data on smoking, lifetime number of receptive partners, external warts, number of anal biopsies and anal biopsy results were obtained from the anal cancer screening study [23]. Anal biopsy results were a composite variable defined as worst diagnosis from either cytology or histology. A sensitivity analysis was conducted to look at the distribution of demographic, behavioral and clinical characteristics for those who responded to the satisfaction survey as compared to the non-responders.
Means and standard deviations of each 5-point Likert response and for the overall eight evaluated domains were calculated and converted to an aggregated scaled score (0, 25, 50, 75, 100) using the following formulas: scaled mean = [raw mean-1] × 25 and scaled standard deviation = raw standard deviation* [scaled mean/raw mean]. To assess concordance between responses within domains, the coefficient of variation was calculated by dividing the standard deviation of the raw mean scores by the overall mean and multiplying by 100. To evaluate differences in satisfaction by HIV status or recent HIV diagnosis, domain means were compared using Wilcoxon rank-sum test and adjusted for multiple comparisons using Bonferroni’s correction. To evaluate differences in satisfaction by number of biopsies experienced during HRA, the domain means were dichotomized as having any agreement (raw mean ≥ 3.5) or no agreement (raw mean < 3.5). Proportional differences in agreement by number of biopsies were evaluated using Chi-square and Fisher’s exact tests. We also explored whether the two lower scored domains (pain/discomfort and intention to screen if presented with clinical symptoms of anal cancer) correlated with overall satisfaction and with each other using Spearman’s rank correlation. Data were analyzed using Stata Statistical Software: Release 13 (Stata Corp LP, College Station, TX) and will be made available upon request.
Results
Of 355 MSM offered HRA, 13 (3%) refused, 342 (96%) engaged, and 307 (86%) completed the self-administered satisfaction survey after HRA and were included in these analyses. The majority of men who completed the satisfaction survey were under the age of 35 (90%) and 58% were living with HIV (95% confidence interval [CI]: 53–64%). Median years since anal coital debut was 7 (interquartile range [IQR]: 4–12). Of the 178 living with HIV, 60% self-reported being told by a doctor that they had HIV prior to entry into TRUST/RV368 and 40% were newly diagnosed at enrollment in TRUST/RV368. Twenty-two percent of participants were current smokers and an additional 5% had smoked in the past. MSM living with HIV had been engaged in anal sex for longer and with more lifetime partners as compared to MSM not living with HIV (Table 1). MSM living with HIV were more likely to have external warts and anal dysplasia as compared to those not living with HIV (Table 1). Compared to men living with HIV, MSM without HIV were younger and were more likely to report exclusively insertive sexual positioning. In the sensitivity analysis, responders to the satisfaction survey were similar to non-responders on all demographic, clinical and behavioral characteristics listed in Table 1 (all p > 0.05, data not shown).
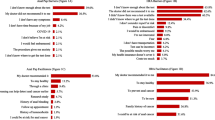
Participants reported anxiety surrounding the procedure (scaled mean:73), but expressed positive agreement with the convenience/accessibility, staff interpersonal skills, physical surroundings, technical competence, and general satisfaction towards HRA screening (74–76) (Table 2). Willingness to have another procedure if necessary had the lowest reported score within the general satisfaction domain (69). For each domain with multiple questions, concordance was high for the individual responses (range: 0.2 to 6.0%) with the exception of pain/discomfort (12.5%). Responses to each of the questions when averaged within the domains did not differ for those living with or without HIV (Fig. 1) or if they had been recently diagnosed with HIV after adjusting for multiple comparisons (all p > 0.006). Overall agreement was also similar irrespective of the number of biopsies (0 to 3) undergone during HRA (all p > 0.05) (Table 3). The pain/discomfort and intention to screen if symptomatic had much lower domain scores (scaled means of 57 and 59, respectively) (Table 2). Only 31% of the men agreed HRA did not cause pain and discomfort and less than 40% would seek screening when presented with clinical symptoms of anal cancer (Table 3). Both domains were correlated with lower overall satisfaction (pain and discomfort Rs = 0.28, intention to screen if symptomatic Rs = 0.63, all p < 0.001) Pain/discomfort was also correlated with intention to screen if symptomatic (Rs = 0.27, p < 0.001).
Likert Responses for Each Satisfaction Question Stratified by HIV Infection. Note: Numbers to the right of the bars indicate the total percent with any agreement (agree and strongly agree) and the numbers to the left indicate the total percent with any disagreement (disagree and strongly disagree). The percentages on the x axis indicate the cumulative proportion of Likert responses either in the agree or disagree direction. The neither agree or disagree proportion is centered at 0% and evenly split towards the agree or disagree direction
Discussion
This cross-sectional study among Nigerian MSM attests to the acceptability of HRA for those who volunteered for their first anal cancer screening even though nearly all were anxious about having the procedure. Our findings also indicate that MSM living with HIV should be prioritized in screening programs, as they had significantly more sexual experience and HPV-associated morbidity relative to participants who were not living with HIV. One of the least agreeable components of the satisfaction survey was the domain related to pain and discomfort which is consistent with other studies [11,12,13]. Our pain and discomfort domain contained five questions as opposed to two from a similar survey in a previous study of HRA satisfaction at an anal health clinic in the United States, and yet the average score and standard deviation were nearly identical, suggesting the level of discomfort was comparable [11]. Other studies used a 10-point scale and found participants on average reported pain and discomfort levels of 2–4 with 6% of men reporting problematic pain, at a cutoff of ≥7 [6, 12, 13]. When these averages are converted to a 100-point scale, our scaled score of 57 is slightly higher but is not considered problematic (scaled score of 70). More importantly, similar to our findings, there was no correlation between the number of biopsies and pain scores [13]. The pain or discomfort felt during HRA may be from pressure on the sphincter or an exam that took longer than the IANS recommended guidelines of less than 15 min; data not collected in our study [5, 6]. These results emphasize the importance of talking with the patient throughout the process: prior to the procedure, during the exam, and a couple weeks after the exam. Physicians can quantify pain by using a pain scale of 0 to 10 with ≥7 suggestive of problematic pain [6]. Documenting the duration of the HRA exam, particularly for those on the early part of the learning curve, would also help improve the assessment of pain or discomfort and potentially improve its success and sustainability.
But despite these indications of pain and discomfort, our study along with others (80–91%) report a remarkably high proportion of participants who were satisfied with the procedure [12, 13]. However, participants in our study indicated less willingness to undergo future procedures if necessary when compared to previous estimates (92–99%) [12, 13]. These differences may be in part due to our study population being naïve to screening, while other studies included experienced screeners who may have been more likely to respond favorably to future screening as a result of their familiarity with procedures [13]. In another study, only 60% (168/281) of those who were screened completed a willingness questionnaire, potentially inflating the positive responses due to the high proportion of missing data [12]. Regardless of sample differences, open discussions about hesitations with screenings and highlighting the benefits of treating HSIL earlier when it is smaller, if proven to prevent anal cancer, may enhance patient experiences and begin to normalize the importance of anal health among the community.
In order to assess retention of anal cancer-related knowledge after HRA, we added questions about whether HRA would be sought with specific symptoms such as rectal or abdominal pain, bleeding, constipation, and unusually shaped stools. The majority of participants did not agree to seek out screening if faced with these symptoms, especially among those who reported lower levels of general satisfaction. This may be partially attributed to lack of communication regarding anal cancer symptoms from physician to patient during the screening visit or higher levels of pain and discomfort, but there may also be a poor understanding of anal cancer risk in general among MSM. Prior studies of MSM in the United States and Australia have shown that the majority of participants were unaware of anal cancer and its associated risks and qualitatively suggested a perception that HPV-associated cancers only affected women and caused cervical cancer [27, 28]. Knowledge and awareness of HPV as a risk factor for anal cancer may be even more scarce in sub-Saharan Africa where it is rarely reported in cancer registries [29]. A systematic review on HPV-associated cancers from sub-Saharan Africa found 7 of 8 included articles focused on cervical cancer and only 1 included data on anal cancer [30]. The estimates of anal cancer were rare, comprising 1% (21/1627) of the reported male cancers [31]. This highlights the need to increase awareness about the risks and symptoms of anal cancer for healthcare providers and MSM at HIV clinics in sub-Saharan Africa.
This study had a few limitations. First, pain levels and psychological impact of screening procedures were not assessed, and would have enhanced the findings related to pain and discomfort. Questions related to anxiety about cancer were not collected and may have confounded willingness to seek further screening. However, participants overwhelmingly indicated agreed that undergoing screening benefited their health and that they would strongly recommend screening to friends. Because few studies have assessed satisfaction with HRA screening, the questionnaire was minimally modified in order to allow comparison with prior work [11]. The inclusion of general knowledge questions about anal cancer might have provided context to the data collected regarding willingness to seek HRA upon recognition of specific anal cancer symptoms. This study was cross-sectional and could not assess whether pain and discomfort were associated with subsequent screening behavior. The data generated from the responses is only generalizable to those who volunteered to engage in screening and completed the satisfaction survey and does not reflect the views of those who refused screening or those who had not completed the survey. Lastly, even though the questionnaire was self-administered, rather than by a healthcare provider, there may have been positive response bias, which would have inflated measures of satisfaction.
Conclusions
This study found acceptability with HRA for Nigerian MSM who volunteered to be screened, despite high levels of anxiety. Monitoring pain scales and ensuring the procedure lasts no longer than 15 min could minimize discomfort and would help strengthen the success of a screening program. Integrating anal cancer screening within a community-engaged MSM-friendly clinic offers an opportunity for physicians and healthcare providers to openly discuss clinical symptoms and encourage patients to voice their hesitations about anal cancer screening in order to normalize the concept of men’s anal health in an otherwise highly stigmatizing environment.
Availability of data and materials
In order to protect the clinic staff and the participants from stigma and criminalization of same sex behavior, the data have not been made publicly available. The data are available from the corresponding author on request.
Abbreviations
- HRA:
-
High resolution anoscopy
- MSM:
-
Men who have sex with men
- IQR:
-
Interquartile range
- CI:
-
Confidence interval
- HPV:
-
Human papillomavirus
- LSIL:
-
Low-grade squamous intraepithelial lesion
- HSIL:
-
High-grade squamous intraepithelial lesion
- P:
-
p-value
- Rs :
-
Spearman’s rank correlation coefficient
- STIs:
-
Sexually transmitted infections
- No:
-
Number
References
Dalla Pria A, Alfa-Wali M, Fox P, Holmes P, Weir J, Francis N, et al. High-resolution anoscopy screening of HIV-positive MSM: longitudinal results from a pilot study. AIDS. 2014;28:861–7.
Cachay E, Agmas W, Mathews C. Five-year cumulative incidence of invasive anal cancer among HIV-infected patients according to baseline anal cytology results: an inception cohort analysis. HIV Med. 2015;16:191–5.
Deshmukh AA, Suk R, Shiels MS, Sonawane K, Nyitray AG, Liu Y, et al. Recent trends in squamous cell carcinoma of the anus incidence and mortality in the United States, 2001-2015. J Natl Cancer Inst. 2019. https://doi.org/10.1093/jnci/djz219. [Epub ahead of print]
Leeds IL. Anal cancer and intraepithelial neoplasia screening: a review. World J Gastrointest Surg. 2016;8:41.
Jay N. Elements of an anal dysplasia screening program. J Assoc Nurses AIDS Care. 2011;22:465–77.
Hillman RJ, Cuming T, Darragh T, Nathan M, Berry-Lawthorn M, Goldstone S, et al. 2016 IANS international guidelines for practice standards in the detection of anal Cancer precursors. J Low Genit Tract Dis. 2016;20:283–91.
Chiao EY, Giordano TP, Palefsky JM, Tyring S, El Serag H. Screening HIV-infected individuals for anal cancer precursor lesions: a systematic review. Clin Infect Dis. 2006;43:223–33.
Aberg JA, Gallant JE, Ghanem KG, Emmanuel P, Zingman BS, Horberg MA. Primary care guidelines for the management of persons infected with HIV: 2013 update by the HIV medicine Association of the Infectious Diseases Society of America. Clin Infect Dis. 2014;58:1–10.
Berry JM, Palefsky JM, Welton ML. Anal cancer and its precursors in HIV-positive patients: perspectives and management. Surg Oncol Clin N Am. 2004;13:355–73.
Abbas A, Yang G, Fakih M. Management of anal cancer in 2010. Part 2: current treatment standards and future directions. Oncology (Williston Park). 2010;24:417–24.
Kwong JJ, Cook P, Bradley-Springer L. Improving anal cancer screening in an ambulatory HIV clinic: experience from a quality improvement initiative. AIDS Patient Care STDs. 2011;25:73–8.
Schofield AM, Sadler L, Nelson L, Gittins M, Desai M, Sargent A, et al. A prospective study of anal cancer screening in HIV-positive and negative MSM. Aids. 2016;30:1375–83.
De-Masi A, Davis E, Cuming T, Chindawi N, Pesola F, Cappello C, et al. The acceptability of high resolution anoscopy examination in patients attending a tertiary referral Centre. BMC Cancer. 2018;18:554.
Tinmouth J, Raboud J, Ali M, Malloch L, Su D, Sano M, et al. The psychological impact of being screened for anal cancer in HIV-infected men who have sex with men. Dis Colon Rectum. 2011;54:352–9.
Berry JM, Jay N, Cranston RD, Darragh TM, Holly EA, Welton ML, et al. Progression of anal high-grade squamous intraepithelial lesions to invasive anal cancer among HIV-infected men who have sex with men. Int J Cancer. 2014;134:1147–55.
de Pokomandy A, Rouleau D, Ghattas G, Trottier H, Vezina S, Cote P, et al. HAART and progression to high-grade anal intraepithelial neoplasia in men who have sex with men and are infected with HIV. Clin Infect Dis. 2011;52:1174–81.
Jemal A, Bray F, Forman D, O’Brien M, Ferlay J, Center M, et al. Cancer burden in Africa and opportunities for prevention. Cancer. 2012;118:4372–84.
Islami F, Ferlay J, Lortet-Tieulent J, Bray F, Jemal A. International trends in anal cancer incidence rates. Int J Epidemiol. 2017;46:924–38.
Rodriguez-Hart C, Musci R, Nowak RG, German D, Orazulike I, Ononaku U, et al. Sexual stigma patterns among Nigerian men who have sex with men and their link to HIV and sexually transmitted infection prevalence. AIDS Behav. 2018;22:1662–70.
Schwartz SR, Nowak RG, Orazulike I, Keshinro B, Ake J, Kennedy S, et al. The immediate eff ect of the Same-Sex Marriage Prohibition Act on stigma, discrimination, and engagement on HIV prevention and treatment services in men who have sex with men in Nigeria: analysis of prospective data from the TRUST cohort. Lancet HIV. 2015;2:e299–306.
Charurat ME, Emmanuel B, Akolo C, Keshinro B, Nowak RG, Kennedy S, et al. Uptake of treatment as prevention for HIV and continuum of care among HIV-positive men who have sex with men in Nigeria. J Acquir Immune Defic Syndr. 2015;68(Suppl 2):S114–23.
Baral SD, Ketende S, Schwartz S, Orazulike I, Ugoh K, Peel SA, et al. Evaluating respondent-driven sampling as an implementation tool for universal coverage of antiretroviral studies among men who have sex with men living with HIV. J Acquir Immune Defic Syndr. 2015;68(Suppl 2):S107–13.
Nowak RG, Ndembi N, Dauda W, Jibrin P, Bentzen SM, Nnaji CH, et al. Implementation of and Early Outcomes From Anal Cancer Screening at a Community-Engaged Health Care Facility Providing Care to Nigerian Men Who Have Sex With Men. J Glob Oncol. 2019;5:1–11.
Schoen RE, Weissfeld JL, Bowen NJ, Switzer G, Baum A. Patient satisfaction with screening flexible sigmoidoscopy. Arch Intern Med. 2000;160:1790–6.
Crowell TA, Keshinro B, Baral SD, Schwartz SR, Stahlman S, Nowak RG, et al. Stigma, access to healthcare, and HIV risks among men who sell sex to men in Nigeria. J Int AIDS Soc. 2017;20:21489.
Keshinro B, Crowell TA, Nowak RG, Adebajo S, Peel S, Gaydos CA, et al. High prevalence of HIV, chlamydia and gonorrhoea among men who have sex with men and transgender women attending trusted community centres in Abuja and Lagos, Nigeria. J Int AIDS Soc. 2016;19:21270. https://doi.org/10.7448/IAS.19.1.21270.
Koskan AM, LeBlanc N, Rosa-Cunha I. Exploring the perceptions of anal Cancer screening and behaviors among gay and bisexual men infected with HIV. Cancer Control. 2016;23:52–8.
Ong JJ, Chen M, Grulich A, Walker S, Temple-Smith M, Bradshaw C, et al. Exposing the gaps in awareness, knowledge and estimation of risk for anal cancer in men who have sex with men living with HIV: a cross-sectional survey in Australia. J Int AIDS Soc. 2015;18:19895.
De Vuyst H, Alemany L, Lacey C, Chibwesha CJ, Sahasrabuddhe V, Banura C, et al. The burden of human papillomavirus infections and related diseases in sub-saharan Africa. Vaccine. 2013;31(Suppl 5):F32–46.
Lekoane KMB, Kuupiel D, Mashamba-Thompson TP, Ginindza TG. Evidence on the prevalence, incidence, mortality and trends of human papilloma virus-associated cancers in sub-Saharan Africa: systematic scoping review. BMC Cancer. 2019;19:563.
Jedy-Agba EE, Dareng EO, Adebamowo SN, Odutola M, Oga EA, Igbinoba F, et al. The burden of HPV associated cancers in two regions in Nigeria 2012-2014. Cancer Epidemiol. 2016;45:91–7.
Acknowledgements
The authors would like to thank all research participants and study staff for their commitment to this study. We thank William A. Blattner for his mentorship and Lionhare Design for their graphic design support. The TRUST Study Group is constituted as follows: Principal Investigators: Manhattan Charurat (IHV, University of Maryland, Baltimore, MD, USA), Julie Ake (MHRP, Walter Reed Army Institute of Research, Silver Spring, MD, USA); Co-Investigators: Sylvia Adebajo, Stefan Baral, Erik Billings, Trevor Crowell, George Eluwa, Charlotte Gaydos, Sosthenes Ketende, Afoke Kokogho, Hongjie Liu, Jennifer Malia, Olumide Makanjuola, Nelson Michael, Nicaise Ndembi, Jean Njab, Rebecca Nowak, Oluwasolape Olawore, Zahra Parker, Sheila Peel, Habib Ramadhani, Merlin Robb, Cristina Rodriguez-Hart, Eric Sanders-Buell, Sodsai Tovanabutra, Erik Volz; Institutions: Institute of Human Virology at the University of Maryland School of Medicine (IHV-UMB), University of Maryland School of Public Health (UMD SPH), Johns Hopkins School of Public Health (JHSPH), Johns Hopkins University School of Medicine (JHUSOM), U.S. Military HIV Research Program (MHRP), Walter Reed Army Institute of Research (WRAIR), Henry M. Jackson Foundation for the Advancement of Military Medicine (HJF), Henry M. Jackson Foundation Medical Research International (HJFMRI), Institute of Human Virology Nigeria (IHVN), International Centre for Advocacy for the Right to Health (ICARH), The Initiative for Equal Rights (TIERS), Population Council (Pop Council) Nigeria, Imperial College London.
Prior presentation
Presented as a poster at the 22nd International AIDS Conference, Amsterdam, Netherlands, 23–27 July 2018.
Funding
Funding for this research was supported by the National Cancer Institute (NCI) [2P30CA134274-09S2, 5P30CA134274] and jointly with the Office of AIDS Research (OAR) [1K07CA225403]. NCI and OAR provided funding for developing the study; collecting, analyzing and interpreting the data; and writing of the manuscript. Additional support for the development and implementation of the parent cohort TRUST/RV368 within which this research was nested was provided by the National Institutes of Health (NIH) [R01 MH099001, R01 AI120913, R01 MH110358]; the Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc., and the U.S. Department of Defense [W81XWH-11-2-0174, W81XWH-18-2-0040]; Fogarty Epidemiology Research Training for Public Health Impact in Nigeria program [D43TW010051]; and the President’s Emergency Plan for AIDS Relief through a cooperative agreement between the Department of Health and Human Services/Centers for Disease Control and Prevention, Global AIDS Program, and the Institute for Human Virology-Nigeria [NU2GGH002099]. The content is solely the responsibility of the authors and should not be construed to represent the positions of the National Institutes of Health, U.S. Army, the Department of Defense, the Department of Health and Human Services, or other funders. The investigators have adhered to the policies for protection of human subjects as prescribed in AR-70.
Author information
Authors and Affiliations
Consortia
Contributions
This study was conceived and designed by RGN, CHN SDB, MEC, JMP and KJC in collaboration with the other authors. Data collection and management was facilitated by RGN, CHN, WD, OO, PJ, and NN. RGN, AM and SMB conducted the analysis with input from all authors. RGN, AM,TAC, and SMB drafted the manuscript and all authors provided critical review and editing. All authors have seen and approved the article and are accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The institutional review board at the Nigerian Federal Capital Territory Health Research Ethics Committee, the Clinical Research Committee at the University of Maryland Marlene and Stewart Greenebaum Comprehensive Cancer Center, and the Institutional Review Board at the University of Maryland Baltimore reviewed and approved the research protocol. All participants provided written informed consent prior to enrollment and all data was de-identified.
Consent for publication
Not applicable.
Competing interests
JMP has stock and ownership interests in Ubiome, Virion Therapeutics, VIR Biotechnology; has received honoraria from Janssen Pharmaceuticals, Vaccitech, Antiva Biosciences; has a consulting or advisory role for Antiva Biosciences, VIR Biotechnology, Vaccitech and Novan; receives research funding from Merck, Antiva Biosciences, VIR Biotechnology, CEL-SCI; and receives travel, accommodations and expenses from Merck, Vaccitech and Janssen. None of this relates to this specific work. All other authors have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Nowak, R.G., Nnaji, C.H., Dauda, W. et al. Satisfaction with high-resolution anoscopy for anal cancer screening among men who have sex with men: a cross-sectional survey in Abuja, Nigeria. BMC Cancer 20, 98 (2020). https://doi.org/10.1186/s12885-020-6567-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-020-6567-3