Abstract
Background
We aimed to identify whether neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) are more useful predictors after initial intention to treat than at the time of diagnosis.
Methods
We collected the medical data of 533 patients. The results of the peripheral blood sampling before the primary treatments were labeled as initial cohort, and those obtained between 24 and 36 months after initial treatment were defined as the 2nd cohort. Delayed metastasis has been defined as distant metastasis 2 years after treatment, and survival outcome was estimated and compared across groups.
Results
Median follow-up duration was 74 months (24–162 months), and 53 patients experienced delayed metastasis. In univariate analysis, metastasis-free survival, patient age at diagnosis, tumor size, axillary lymph node metastasis, HER-2 status, initial NLR and PLR, and 2nd NLR and PLR were found to be significantly associated with delayed metastasis. However, in multivariate analysis, only the 2nd NLR and PLR were found to be significantly associated with delayed metastasis, excluding initial NLR and PLR. Metastasis-free survival was analyzed through the pattern changes of NLR or PLR. The results revealed that patients with continued low NLR and PLR values at pre- and post-treatment (low initial values and 2nd values) showed a significantly better prognosis than those with a change in value or continued high NLR and PLR.
Conclusions
We identified that patients with persistent high NLR and PLR after initial treatment have significant worse prognosis in terms of late metastasis. Therefore, these results suggest that NLR and PLR are more useful in predicting prognosis post-treatment.
Similar content being viewed by others
Background
Breast cancer is a common malignancy in women around the world, and despite the availability of optimal local and systemic therapies, a substantial number of women with breast cancer will develop systemic recurrence [1]. Indeed, the leading cause of breast cancer-related deaths is its metastatic spread, although the timing and distribution of breast cancer metastases vary considerably.
Previous studies have reported that there is a significant difference in the onset of recurrence depending on the hormone receptor status and hormonal therapy, wherein estrogen receptor-negative tumors are generally associated with early recurrence [2, 3]. The mechanisms that account for the wide variability in the propensity of breast cancer to metastasize are currently unknown. However, metastatic spread form a primary breast tumor can occur at an early, pre-symptomatic stage, and disseminated cells often settle in the bone marrow where they can lie dormant for years before becoming clinically evident [4].
In cancer patients, inflammatory cells and their mediators in the tumor microenvironment are considered to play an important role in cancer development and progression. A recent meta-analysis demonstrated that an elevated peripheral neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) at the baseline before the first treatment represent poor prognostic factors in breast cancer [5,6,7,8]. Inflammatory conditions can be migrated through treatments and lifestyle changes. In particular, chemotherapy affects various cells, including inflammatory and immune cells, and the subsequent recovery process may vary from patient to patient; these post-treatment changes may then affect the expression of disseminated metastatic cells [9].
Most previous studies have conducted primary tumor or blood tests before treatment; meanwhile, studies evaluating test results obtained after treatment as prognostic markers remain to be limited. The status of tumors or patients after treatment can also be useful surrogate markers of prognosis, for example, complete remission after neoadjuvant chemotherapy or Ki-67 level after preoperative endocrine therapy [10,11,12].
The primary aim of this study is to determine whether the NLR and PLR obtained after initial intention to treat could predict prognosis after 2 years in patients without evidence of early cancer recurrence or metastasis.
Methods
Study cohort
The data of female patients with primary breast cancer who diagnosed from January 2006 to December 2015 at a single institute were analyzed for this retrospective cohort study. All patients were recommended to undergo treatment with standard adjuvant therapy and post treatment surveillance according to the guidelines. The exclusion criteria were as follows: patients who were concurrently or previously diagnosed with other organs malignancies; patients who had M1 diseases on diagnosis; patients who had systemic autoimmune disease, such as systemic lupus or scleroderma; and patients who had incomplete data. The characteristics of study patients are presented in Table 1. Out of the 674 patients assessed, 533 patients were included in the final analysis; of these, 29 (4.3%) had disease recurrence or distant metastasis before 2 years, 51 (7.6%) were lost to follow-up within 2 years, and 61 (9.1%) had no blood test results between 24 and 36 months. This study protocol was received approval from the institutional review board and met the guidelines of the responsible governmental agencies (IRB No. GNUH 2020–04-020). Informed consent was waived based on the retrospective format of this study.
Data collection and statistical analysis
The NLR and PLR are defined as the absolute neutrophil count or absolute platelet count divided by the absolute lymphocyte count. Peripheral blood samplings were performed both at the initial work-up period before treatment and at routine follow-up. The results obtained before the primary treatments were labeled as the initial cohort; meanwhile the results derived between 24 and 36 months were defined as the 2nd cohort. Receiver operating characteristic (ROC) curve analysis was used to determine the cut-off value of the NLR and PLR. Non-parametric tests of the association of cohorts were compared with Mann-Whitney U test.
We reviewed the medical records, pathology reports, and follow-up data of the enrolled patients. Delayed metastasis was defined as metastasis 2 years after initial treatment, and metastasis-free survival (MFS) was defined as the time interval from the date of initial diagnosis to the date of distant metastasis or to the most recent follow-up date with no evidence of distant metastasis. To determine whether NLR and PLR are useful predictors of delayed metastasis, survival outcome was estimated using the Kaplan–Meier curve, and univariate analysis for comparing across groups was performed using the log-rank test. With regard to multivariate analysis, a Cox proportional hazards model was used to estimate the adjusted hazard ratio for significance. All analyses were carried out using SPSS (version 20.0; SPSS, Inc.), and p < 0.05 was assumed statistically significant.
Results
We reviewed the data of 533 patients (stage I; 219(41.1%), stage II; 237 (44.5%) and stage III; 77 (14.4%)) to identify the prognostic factors affecting delayed metastasis. The median follow-up duration was 74 months (range, 24–162 months), and 53 patients were found to experience delayed distant metastasis.
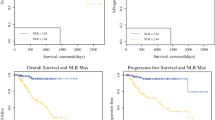
The mean values of the initial NLR and PLR were 2.11 and 145.75, respectively, and the mean values of the 2nd NLR and PLR were 1.72 and 118.55, respectively. The NLR and PLR values had a tendency to be lower in the 2nd group than in the initial group (Fig. 1a and b).
The average difference in value was analyzed according to delayed metastasis. Initial NLR and 2ndNLR were significantly higher in the metastasis group than in the no metastasis group. (initial NLR; no metastasis vs. metastasis [mean ± SD = 2.06 ± 1.17 vs. 2.40 ± 1.18] p = 0.016; and 2nd LNR; no metastasis vs. metastasis [mean ± SD = 1.65 ± 1.29 vs. 2.36 ± 3.12] p = 0.004). The continuous PLR value was also higher in the metastasis group than in the no metastasis group, bot statistically only 2nd PLR value as noted (initial PLR; no metastasis vs. metastasis [mean ± SD = 144.36 ± 54.40 vs. 157.34 ± 73.10] p = 0.363; and 2nd PLR; no metastasis vs. metastasis [mean ± SD = 116.22 ± 38.32 vs. 139.66 ± 56.73] p = 0.003) (Fig. 1c and d).
ROC curve analysis was also used to determine the optimal cutoff value of NLR and PLR for the initial and 2nd groups. The initial LNR cutoff value was 1.82 (area under the ROC curve [AUC], 0.601; 95% confidence interval [CI], 0.520–0.681) with 64.2% sensitivity and 52.1% specificity. The 2nd LNR cutoff value was 1.76 (AUC, 0.619; 95% CI, 0.540–0.711) with 50.9% sensitivity and 70.6% specificity. The initial PLR cut-off value was 204.27 (AUC, 0.534; 95% CI, 0.494–0.634) with 28.3% sensitivity and 87.7% specificity. The 2nd PNR cut-off value was 112.67 (AUC, 0.625; 95% CI, 0.540–0.711) with 69.8% sensitivity and 55.6% specificity.
The survival outcome was estimated using the Kaplan–Meier method, and the results were compared across groups using the log-rank test (Table 2). Patient age at diagnosis, tumor size, lymph node metastasis, HER-2 status, initial NLR and PLR, and 2nd NLR and PLR were found to be significantly associated with delayed metastasis.
Most of the patients included in the analysis were not subjected to HER-2 targeted therapy due to medical insurance problems in Korea at the time. Therefore, we performed two multivariate analyses, which included and excluded the HER-2 status (Table 3). The 2nd NLR and PLR were significantly associated with delayed metastasis; however, the initial NLR and PLR showed no prognostic significance.
We examined the effects of NLR and PLR changes after initial treatments, wherein the MFS was analyzed according to the change in NLR or PLR (Fig. 2a and b). Kaplan–Meier analysis revealed that patients with continued low NLR and PLR at the time of diagnosis and after treatment (low initial values and 2nd values) showed a significantly better MFS than patients with value changes or continued high NLR and PLR. In particular, patients with continued high 2nd NLR or PLR cutoff values had significantly poorer MFS than patients with continued low NLR or PLR cutoff values (Fig. 2c and d).
Discussion
This study demonstrated that patients with persistent high NLR and PLR after initial treatment have significantly worse prognosis with regard to late metastasis. In particular, we demonstrated that the NLR and PLR after initial treatment better reflect the prognosis than the NLR and PLR at the time of diagnosis. This result may explain the considerable differences in prognosis in breast cancer patients who have received the same standard treatment.
Tumor development, progression, and metastasis are affected by the host inflammation status and immune response in the tumor microenvironment [13,14,15,16]. Numerous studies have shown that lymphocytes play a critical role in tumor immune surveillance [16, 17], and are able to control tumor growth by their cytotoxic activity and induction of apoptosis [18]. Clinical data have shown that an increased density of tumor-infiltrating lymphocytes is associated with favorable prognosis in breast cancer [19, 20]. Meanwhile, neutrophils have been shown to inhibit the immune response by suppressing the cytolytic activity of immune cells, such as lymphocytes, activated T cells, and natural killer cells [21, 22]. Moreover, neutrophils and macrophages have been reported to secrete tumor growth-promoting factors, IL-6, IL-8, including vascular endothelial growth factor, and elastases, and thus likely contribute to a pro-tumor microenvironment [23,24,25,26]. Furthermore, platelets have been shown to secrete cellular growth factors, including transforming growth factor beta, platelet-derived growth factor, and vascular endothelial growth factor, which could stimulate tumor proliferation and angiogenesis [27,28,29]. Therefore, having high NLR and PLR, with a high neutrophil or platelet count and/or low lymphocyte count, can result in poor prognosis of multiple cancers.
A recent meta- analysis examining 100 studies demonstrated that a high NLR is associated with adverse survival in many solid tumors [5]. Similarly, in a meta-analysis of breast cancer, a high NLR was found to be associated with an adverse disease-free survival and overall survival, with a greater association with disease-specific outcome in estrogen receptor and HER-2 negative disease. Furthermore, the PLR in breast cancer highly correlated with clinicopathologic characteristics and was associated with poor prognosis [7].
With well-established prognostic factors, the estimation of risk development of a systemic disease following the treatment for breast cancer can be made possible. Known prognostic factors include histologic subtype of breast cancer, tumor grade, tumor size, involvement of skin or chest wall, extent of involvement of regional lymph nodes, hormone receptor status, and HER-2 status. However, due to the complex nature of breast cancer, the progression and prognosis according to time have been variable and difficult to predict adequately. Recently, a number of proven multigene array expression profiles, such as Oncotype Dx® and Pam-50 ror®, have yielded better predictive power of late recurrence; however, these tests are expensive and inaccessible to most patients [30,31,32].
In recent years, considerable effort and resources have been used in developing biomarkers, which can help to individual tailor therapy for cancer patients. A small number of patients have persistent poor clinical outcome irrespective of treatment with standard therapy; thus, finding a marker that predicts the prognosis of these patients remains a valuable research subject. Changes in blood inflammatory markers might be useful to predict the post-treatment prognosis and tailor the therapy after. Previous small studies have shown that chemotherapy can normalize an elevated NLR early after the initiation of treatment and that patients with a normalized NLR may have improved clinical outcome in advanced colorectal, urothelial, and biliary cancer [33,34,35]. Thus, it is considered that the prognostic role of the NLR might still be relevant for the evaluation of the early effects of systemic therapy. Further, in patients with metastatic breast cancer, high NLR was found to be factor related to low responsiveness to eriburin-based treatment [36]. Recently inflammatory markers were also reported as important prognostic markers not only in systemic therapy but also in immune therapy. In study, which perfromed in 90 patients who received immunotherapy based treatment regimens, elevated baseline and early increases in NLR and PLR values were strongly associated with poor clinical outcomes in advanced cancer patients [37].
In most cancer patients, a routine blood test is widely used as a traditional examination test at the time of diagnosis and follow-up periods. The results of our study confirmed that observing the process of continuous change, as well as the initial NLR or PLR, can also be an important indicator for predicting the prognosis of the patient. Indeed, a recent study demonstrated that patients with a high NLR approximately 5 years after the initial diagnosis had significantly worse breast cancer-free survival with late recurrence (HR, 1.448; p < 0.001). Furthermore, it was shown that the NLR obtained after the completion of primary treatment can predict later recurrence in breast cancer patients [38].
Our study has several limitations. First, the retrospective protocol of this study necessitates prospective validation of the prognostic effect. Second, this study analyzed the NLR and PLR values between 2 and 3 years, but further research is needed to determine whether the prognosis varies after this period, depending on the pattern of continuous change in long term. Third, we only analyzed our hospital data, which included a relatively small number of enrolled patients and had an insufficient follow-up period.
Conclusions
We showed that NLR and PLR follow-up values are important predictors of prognosis in breast cancer patients. NLR and PLR changes are easily accessible markers with a simple blood test follow-up, so they should be considered as potential prognostic biomarkers to be associated with others.
Availability of data and materials
All the data supporting our findings are contained within the manuscript.
Abbreviations
- NLR:
-
Neutrophil-to-lymphocyte ratio
- PLR:
-
Platelet-to-lymphocyte ratio
- ROC:
-
Receiver operating characteristic
- MFS:
-
Metastasis-free survival
- AUC:
-
Area under the ROC curve
References
Saphner T, Tormey DC, Gray R. Annual hazard rates of recurrence for breast cancer after primary therapy. J Clin Oncol. 1996;14:2738–46.
Park HS, Kim S, Kim K, Yoo H, Chae BJ, Bae JS, et al. Pattern of distant recurrence according to the molecular subtypes in Korean women with breast cancer. World J Surg Oncol. 2012;10:4.
Park YH, Lee S, Cho EY, Choi YL, Lee JE, Nam SJ, et al. Patterns of relapse and metastatic spread in HER2-overexpressing breast cancer according to estrogen receptor status. Cancer Chemother Pharmacol. 2010;66:507–16.
Schwartz RS, Erban JK. Timing of metastasis in breast Cancer. N Engl J Med. 2017;376:2486–8.
Templeton AJ, McNamara MG, Seruga B, Vera-Badillo FE, Aneja P, Ocana A, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106:dju124.
Ethier JL, Desautels D, Templeton A, Shah PS, Amir E. Prognostic role of neutrophil-to-lymphocyte ratio in breast cancer: a systematic review and meta-analysis. Breast Cancer Res. 2017;19:2.
Zhang M, Huang XZ, Song YX, Gao P, Sun JX, Wang ZN. High platelet-to-lymphocyte ratio predicts poor prognosis and clinicopathological characteristics in patients with breast cancer: a meta-analysis. Biomed Res Int. 2017;2017:9503025.
Wei B, Yao M, Xing C, Wang W, Yao J, Hong Y, et al. The neutrophil lymphocyte ratio is associated with breast cancer prognosis: an updated systematic review and meta-analysis. Onco Targets Ther. 2016;9:5567–75.
Bracci L, Schiavoni G, Sistigu A, Belardelli F. Immune-based mechanisms of cytotoxic chemotherapy: implications for the design of novel and rationale-based combined treatments against cancer. Cell Death Differ. 2014;21(1):15–25.
Ellis MJ, Suman VJ, Hoog J, Lin L, Snider J, Prat A, et al. Randomized phase II neoadjuvant comparison between letrozole, anastrozole, and exemestane for postmenopausal women with estrogen receptor-rich stage 2 to 3 breast cancer: clinical and biomarker outcomes and predictive value of the baseline PAM50-based intrinsic subtype--ACOSOG Z1031. J Clin Oncol. 2011;29:2342–9.
Liedtke C, Mazouni C, Hess KR, Andre F, Tordai A, Mejia JA, et al. Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J Clin Oncol. 2008;26:1275–81.
Carey LA, Dees EC, Sawyer L, Gatti L, Moore DT, Collichio F, et al. The triple negative paradox: primary tumor chemosensitivity of breast cancer subtypes. Clin Cancer Res. 2007;13:2329–34.
Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420:860–7.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–74.
DeNardo DG, Coussens LM. Inflammation and breast cancer. Balancing immune response: crosstalk between adaptive and innate immune cells during breast cancer progression. Breast Cancer Res. 2007;9:212.
Dunn GP, Old LJ, Schreiber RD. The immunobiology of cancer immunosurveillance and immunoediting. Immunity. 2004;21:137–48.
Seo AN, Lee HJ, Kim EJ, Kim HJ, Jang MH, Lee HE, et al. Tumour-infiltrating CD8+ lymphocytes as an independent predictive factor for pathological complete response to primary systemic therapy in breast cancer. Br J Cancer. 2013;109:2705–13.
Hiraoka K, Miyamoto M, Cho Y, Suzuoki M, Oshikiri T, Nakakubo Y, et al. Concurrent infiltration by CD8+ T cells and CD4+ T cells is a favourable prognostic factor in non-small-cell lung carcinoma. Br J Cancer. 2006;94:275–80.
Kotoula V, Chatzopoulos K, Lakis S, Alexopoulou Z, Timotheadou E, Zagouri F, et al. Tumors with high-density tumor infiltrating lymphocytes constitute a favorable entity in breast cancer: a pooled analysis of four prospective adjuvant trials. Oncotarget. 2016;7:5074–87.
Ibrahim EM, Al-Foheidi ME, Al-Mansour MM, Kazkaz GA. The prognostic value of tumor-infiltrating lymphocytes in triple-negative breast cancer: a meta-analysis. Breast Cancer Res Treat. 2014;148:467–76.
Petrie HT, Klassen LW, Kay HD. Inhibition of human cytotoxic T lymphocyte activity in vitro by autologous peripheral blood granulocytes. J Immunol. 1985;134:230–4.
El-Hag A, Clark RA. Immunosuppression by activated human neutrophils. Dependence on the myeloperoxidase system. J Immunol. 1987;139:2406–13.
Di Carlo E, Forni G, Musiani P. Neutrophils in the antitumoral immune response. Chem Immunol Allergy. 2003;83:182–203.
Jablonska E, Kiluk M, Markiewicz W, Piotrowski L, Grabowska Z, Jablonski J. TNF-alpha, IL-6 and their soluble receptor serum levels and secretion by neutrophils in cancer patients. Arch Immunol Ther Exp. 2001;49:63–9.
Schaider H, Oka M, Bogenrieder T, Nesbit M, Satyamoorthy K, Berking C, et al. Differential response of primary and metastatic melanomas to neutrophils attracted by IL-8. Int J Cancer. 2003;103:335–43.
Scapini P, Nesi L, Morini M, Tanghetti E, Belleri M, Noonan D, et al. Generation of biologically active angiostatin kringle 1-3 by activated human neutrophils. J Immunol. 2002;168:5798–804.
Egan K, Crowley D, Smyth P, O’Toole S, Spillane C, Martin C, et al. Platelet adhesion and degranulation induce pro-survival and pro-angiogenic signalling in ovarian cancer cells. PLoS One. 2011;6:e26125.
Kono SA, Heasley LE, Doebele RC, Camidge DR. Adding to the mix: fibroblast growth factor and platelet-derived growth factor receptor pathways as targets in non-small cell lung cancer. Curr Cancer Drug Targets. 2012;12:107–23.
Klinger MH, Jelkmann W. Role of blood platelets in infection and inflammation. J Interf Cytokine Res. 2002;22:913–22.
Sestak I, Cuzick J. Markers for the identification of late breast cancer recurrence. Breast Cancer Res. 2015;17:10.
Sestak I, Buus R, Cuzick J, Dubsky P, Kronenwett R, Denkert C, et al. Comparison of the performance of 6 prognostic signatures for estrogen receptor-positive breast Cancer: a secondary analysis of a randomized clinical trial. JAMA Oncol. 2018;4:545–53.
Sestak I. Risk stratification in early breast cancer in premenopausal and postmenopausal women: integrating genomic assays with clinicopathological features. Curr Opin Oncol. 2019;31:29–34.
Chua W, Charles KA, Baracos VE, Clarke SJ. Neutrophil/lymphocyte ratio predicts chemotherapy outcomes in patients with advanced colorectal cancer. Br J Cancer. 2011;104:1288–95.
Rossi L, Santoni M, Crabb SJ, Scarpi E, Burattini L, Chau C, et al. High neutrophil-to-lymphocyte ratio persistent during first-line chemotherapy predicts poor clinical outcome in patients with advanced urothelial cancer. Ann Surg Oncol. 2015;22:1377–84.
Cho KM, Park H, Oh DY, Kim TY, Lee KH, Han SW, et al. Neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and their dynamic changes during chemotherapy is useful to predict a more accurate prognosis of advanced biliary tract cancer. Oncotarget. 2017;8:2329–41.
Myojin M, Horimoto Y, Ito M, Kitano S, Ishizuka Y, Sasaki R, et al. Neutrophil-to-lymphocyte ratio and histological type might predict clinical responses to eriburin-based treatment in patients with metastatic breast cancer. Breast Cancer. 2020. https://doi.org/10.1007/s12282-020-01069-0.
Bilen MA, Martini DJ, Liu Y, Lewis C, Collins HH, Shabto JM, et al. The prognostic and predictive impact of inflammatory biomarkers in patients who have advanced-stage cancer treated with immunotherapy. Cancer. 2019;125(1):127–34.
Moon G, Noh H, Cho IJ, Lee JI, Han A. Prediction of late recurrence in patients with breast cancer: elevated neutrophil to lymphocyte ratio (NLR) at 5 years after diagnosis and late recurrence. Breast Cancer. 2020;27:54–61.
Acknowledgements
None.
Funding
This work was partly supported by grants from the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded (NRF-2019R1F1A1057175). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
All the authors have made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data. JYK and EJJ conceived of and organized the study and was primarily responsible for drafting the manuscript. JMK and HSL carried out collection of primary data and provided clinical input. JMK, HSL, JHP, TP and SHJ confirmed patients’ outcomes of recurrence and follow up results and guided statistical analysis. CYJ, YTJ and YJL participated in the study design and helped to draft the manuscript. As responding author, EJJ designed and coordinated the research and provided close guidance throughout the process. All authors read and approved the final manuscript. The authors have been involved in drafting the manuscript or revising it critically for important intellectual content and have all given final approval of the version to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Our study protocol, including the use of the institutional database was approved by the Institutional Review Board of Gyeongsang National University Hospital (IRB No. GNUH 2020–04-020) and all procedures were done in accordance with the Declaration of Helsinki. Informed consent was exempted due to the retrospective format of this study.
Consent for publication
Not applicable.
Competing interests
All authors declare that there is no actual or potential conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kim, JY., Jung, E.J., Kim, JM. et al. Dynamic changes of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio predicts breast cancer prognosis. BMC Cancer 20, 1206 (2020). https://doi.org/10.1186/s12885-020-07700-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-020-07700-9